Environmental Encyclopedia
Подождите немного. Документ загружается.

Environmental Encyclopedia 3
Filtration
them to miss the fibers, but when the air stream bends to
go around the fibers the momentum, of the particles is too
much to let them remain with the stream, so that they are
“centrifuged out” onto the fibers (impaction). By electropho-
resis, still other particles may be attracted to the fibers by
electric charges of opposite sign on the particles and on the
fibers. Finally, particles may simply be larger than the space
between fibers, and be sifted out of the air in a process called
sieving.
Filters are also formed by a process in which polymers
such as cellulose esters are made into a film out of a solution
in an organic solvent containing water. As the solvent evapo-
rates, a point is reached at which the water separates out as
microscopic droplets, in which the polymer is not soluble.
The final result is a film of polymer full of microscopic holes
where the water droplets once were. Such filters can have
pore sizes from a small fraction of a micrometer to a few
micrometers. (One micrometer equals 0.00004 in) These
are called membrane filters.
Another form of membrane filter is formed from the
polymer called polycarbonate. A thin film of this material
is fastened to a surface of
uranium
metal and placed in a
nuclear reactor for a time. In the reactor, the uranium under-
goes
nuclear fission
, and gives off particles called fission
fragments, atoms of the elements formed when the uranium
atoms split. Every place that an atom from the fissioning
uranium passes through the film is disturbed on a molecular
scale. After removal from the reactor, if the polymer sheet
is soaked in alkali, the disturbed material is dissolved. The
amount of material dissolved is controlled by the temperature
of the solution and the amount of time the film is treated.
Since the fission fragments are very energetic, they travel in
straight lines, and so the holes left after the alkali treatment
are very straight and round. Again, pore sizes can be from
a small fraction of a micrometer to a few micrometers. These
filters are known by their trade name, Nuclepore.
In both types of membrane filters, the small pore size
increases the role of sieving in particle removal. Because of
their very simple structure, Nuclepore filters have been much
studied to understand
filtration
mechanisms, since they are
far easier to represent mathematically than a random ar-
rangement of fibers.
It was mentioned above that small particles are col-
lected because of their Brownian motion, while larger parti-
cles are removed by interception, impaction, and sieving.
Under many conditions, a particle of intermediate size may
pass through, too large for Brownian diffusion, and too small
for impaction, interception, or sieving. Hence many filters
may show a penetration maximum for particles of a few
tenths of a micrometer. For this reason, standard methods
of filter testing specify that the
aerosol
test for determining
the efficiency of filters should contain particles in that size
557
range. This phenomenon has also been used to select rela-
tively uniform particles of that size out of mixtures of
many sizes.
In circumstances where filter strength is of paramount
importance, such as in industrial filters where a large air
flow must pass through a relatively small filter area, filters
of woven cloth are used, made of materials ranging from
cotton to glass fiber and asbestos, these last for use when
very hot gases must be filtered. The woven fabric itself is
not a particularly good filter, but it retains enough particles
to form a particle cake on the surface, and that soon becomes
the filter. When the cake becomes thick enough to slow
airflow to an unacceptable degree, the air flow is interrupted
briefly, and the filters are shaken to dislodge the filter cake,
which falls into bins at the bottom of the filters. Then
filtration is resumed, allowing the cloth filters to be used
for months before being replaced. A familiar domestic exam-
ple is the bag of a home vacuum cleaner. Cement plants
and some electric
power plants
use dozens of cloth bags
up to several feet in diameter and more than ten feet (three
meters) in length to remove particles from their waste gases.
Otherwise poor filters can be made efficient by making
them thick. A glass tube can be partially plugged with a wad
of cotton or glass fiber, then nearly filled with crystals of
sugar or naphthalene and used as a filter; this is advantageous
since sugar can be dissolved in water, or naphthalene will
sublime away if gently heated, leaving behind the collected
particles. See also Baghouse; Electrostatic precipitation; Odor
control; Particulate
[James P. Lodge Jr.]
Filtration
A common technique for separating substances in two physi-
cal states. For example, a mixture of solid and liquid can be
separated into its components by passing the mixture
through a filter paper. Filtration has many environmental
applications. In water purification systems, impure water is
often passed through a charcoal filter to remove the solid
and gaseous contaminants that give water a disagreeable
odor, color, or taste. Trickling
filters
are used to remove
solid wastes in plants. Solid and liquid contaminants in waste
industrial gases can be removed by passing them through a
filter prior to
discharge
in a smokestack.
Fire
see
Prescribed burning; Wildfire

Environmental Encyclopedia 3
Fire ants
Fire ants
Two distinct
species
of fire ants (genus Solenopsis) from
South America have been introduced into the United States
this century. The South American black fire ant (S. richteri)
was first introduced into the United States in 1918. Its close
relative, the red fire ant (S. wagneri), was introduced in 1940,
probably escaping from a South American freighter docked
in Mobile, Alabama. Both species became established in the
southeastern United States, spreading into nine states from
Texas across to Florida and up into the Carolinas. It is
estimated that they have infested over 320 million acres (130
million ha) covering 13 states as well as Puerto Rico.
Successful
introduced species
are often more aggres-
sive than their native counterparts, and this is definitely true
of fire ants. They are very small, averaging 0.2 in (5 mm)
in length, but their aggressive, swarming behavior makes
them a threat to livestock and pets as well as humans. These
industrious, social insects build their nests in the ground—
the location is easily detected by the elevated earthen mounds
created from their excavations. The mounds are 18–36 in
(46–91 cm) in diameter and may be up to 36 in (91 cm)
high, although mounds are generally 6–10 in (15–25 cm)
high. Each nest contains as many as 25,000 workers, and
there may be over 100 nests on an acre of land.
If the nest is disturbed, fire ants swarm out of the
mound by the thousands and attack with swift ferocity.
As with other aspects of ant behavior, a chemical alarm
pheromone is released that triggers the sudden onslaught.
Each ant in the swarm uses its powerful jaws to bite and latch
onto whatever disturbed the nest, while using the stinger on
the tip of its abdomen to sting the victim repeatedly. The
intruder may receive thousands of stings within a few
seconds.
The toxin produced by the fire ant is extremely potent,
and it immediately causes an intense burning pain that may
continue for several minutes. After the pain subsides, the
site of each sting develops a small bump which expands and
becomes a tiny, fluid-filled blister. Each blister flattens out
several hours later and fills with pus. These swollen pustules
may persist for several days before they are absorbed and
replaced by scar tissue. Fire ants obviously pose a problem
for humans. Some people may become sensitized to fire ant
venom, have a generalized systematic reaction, and go into
anaphylactic shock. Fire-ant induced deaths have been re-
ported. Because these species prefer open, grassy yards or
fields, pets and livestock may fall prey to fire ant attacks
as well.
Attempts to eradicate this
pest
involved the use of
several different generalized pesticides, as well as the wide-
spread use of
gasoline
either to burn the nest and its inhabit-
ants or to kill the ants with strong toxic vapors. Another
558
approach involved the use of specialized crystalline pesticides
which were spread on or around the nest mound. The work-
ers collected them and took them deep into the nest, where
they were fed to the queen and other members of the colony,
killing the inhabitants from within. A more recent method
involves the release of a natural predator of the fire ant, the
“phorid” fly. The fly releases an egg into the fire ant. The
larva then eats the ant’s brain while releasing an
enzyme
.
The enzyme systematically destroys the joints causing the
ant’s head to fall off. The flies were released in 11 states as
of 2001 and seem to be slowly inhibiting the growth of the
fire ant population. As effective as some of these methods
are, fire ants are probably too numerous and well established
to be completely eradicated in North America.
[Eugene C. Beckham]
R
ESOURCES
B
OOKS
Holldobler, B. The Ants. Cambridge: Harvard University Press, 1990.
Taber, Stephen Welton. Fire Ants. Texas A&M University Press, 2000.
P
ERIODICALS
Vergano, Dan. “Decapitator Flies will Fight Fire Ants.” USA Today, No-
vember 20, 2000.
O
THER
“Imported Fire Ant.” NAPIS Page for BioControl Host. April 2001 [cited
May 2002]. <http://www.ceris.purdue.edu/napis/pests/ifa/ifabc.html>.
“Invasive Species and Pest Management: Imported Fire Ant.” Animal and
Plant Health Inspection Service. May 2002 [cited May 2002]. <http://
www.aphis.usda.gov>.
First World
The world’s more wealthy, politically powerful, and industri-
ally developed countries are unofficially, but commonly, des-
ignated as the First World. The term differentiates the pow-
erful, capitalist states of Western Europe and North America
and Japan from the (formerly) communist states (
Second
World
) and from the nonaligned, developing countries
(
Third World
) in world systems theory. In common usage,
First World refers mainly to a level of economic strength.
The level of industrial development of the First World,
characterized by an extensive infrastructure, mechanized
production, efficient and fast transport networks, and perva-
sive use of high technology, consumes huge amounts of
natural resources
and requires an educated and skilled
work force. However, such a system is usually highly profit-
able. Often depending upon raw materials imported from
poorer countries (wood, metal ores,
petroleum
, food, and
so on), First World countries efficiently produce goods that
less developed countries
desire but cannot produce them-
selves, including computers, airplanes, optical equipment,

Environmental Encyclopedia 3
Fish kills
and military hardware. Generally, high domestic and inter-
national demand for such specialized goods keeps First
World countries wealthy, allowing them to maintain a high
standard of material consumption, education, and health
care for their citizens.
Fish and Wildlife Service
The United States Fish & Wildlife Service based in Wash-
ington, D.C., is charged with conserving, protecting, and
enhancing fish,
wildlife
, and their habitats for the benefit
of the American people. As a division of the
U.S. Depart-
ment of the Interior
, the Service’s primary responsibilities
are for the protection of migratory birds,
endangered spe-
cies
, freshwater and anadromous (saltwater
species
that
spawn in freshwater rivers and streams) fisheries, and certain
marine mammals.
In addition to its Washington, D.C., headquarters,
the Service maintains seven regional offices and a number
of field units. Those include national wildlife refuges, na-
tional fish hatcheries, research laboratories, and a nationwide
network of law enforcement agents.
The Service manages 530 refuges that provide habitats
for migratory birds, endangered species, and other wildlife.
It sets migratory bird
hunting
regulations, and leads an
effort to protect and restore endangered and threatened ani-
mals and plants in the United States and other countries.
Service scientists assess the effects of contaminants on
wildlife and habitats. Its geographers and cartographers work
with other scientists to map
wetlands
and carry out pro-
grams to slow wetland loss, or preserve and enhance these
habitats. Restoring fisheries that have been depleted by
over-
fishing
,
pollution
, or other
habitat
damage is a major pro-
gram of the Service. Efforts are underway to help four impor-
tant species: lake trout in the upper
Great Lakes
; striped
bass in both the
Chesapeake Bay
and Gulf Coast; Atlantic
salmon
in New England; and salmonid species of the Pacific
Northwest.
Fish and Wildlife biologists working with scientists
from other federal and state agencies, universities, and pri-
vate organizations develop recovery plans for endangered and
threatened species. Among its successes are the
American
alligator
, no longer considered endangered in some areas,
and a steadily increasing
bald eagle
population.
Internationally, the Service cooperates with 40 wildlife
research and
wildlife management
programs, and provides
technical assistance to many other countries. Its 200 special
agents and inspectors help enforce wildlife laws and treaty
obligations. They investigate cases ranging from individual
migratory bird hunting violations to large-scale
poaching
and commercial trade in protected wildlife.
559
It its “Vision for the Future” statement, the Fish and
Wildlife Service states its mission to “provide leadership to
achieving a national net gain of fish and wildlife and the
natural systems which support them.” Into the twenty-first
century, this vision statement calls for new
conservation
compacts with all citizens to increase the value of the United
States wildlife holdings in number and
biodiversity
, and
to provide increased opportunities for the public to use,
associate with, learn about and enjoy America’s wildlife
wealth.
[Linda Rehkopf]
R
ESOURCES
O
THER
U.S. Fish and Wildlife Service. Vision for the Future. Washington, DC:
U.S. Government Printing Office, 1991.
O
RGANIZATIONS
U.S. Fish and Wildlife Service, Email: contact@fws.gov, <http://
www.fws.gov>
Fish farming
see
Blue revolution (fish farming)
Fish kills
Fishing has long been a major provider of food and livelihood
to people throughout the world. In the United States, 50
million people enjoy fishing as an outdoor recreation—38
million in fresh water and 12 million in salt water. Com-
bined, they spend over $315 million annually on this sport.
It is no surprise, then, that public attitude towards factors
that influence fishing is strong.
The
Environmental Protection Agency
(EPA) is
charged with overseeing the quality of the nation’s water-
ways. In 1977 they received information on 503 separate
incidents in which 16.5 million fish were killed. In 1974, a
record 47 million fish were killed in the Black River near
Essex, Maryland, by a
discharge
from a sewage plant.
Fish kills can result from natural as well as human
causes. Natural causes include sudden changes in tempera-
ture, oxygen depletion, toxic gases, epidemics of viruses and
bacteria, infestations of
parasites
, toxic algal blooms, light-
ning,
fungi
, and other similar factors. Human influences
that lead to fish kills include
acid rain
, sewage
effluent
,
and toxic spills.
In a 10-year study of the causes of 409 documented
fish kills totaling 3.6 million fish in the state of Missouri,
Environmental Encyclopedia 3
Fish kills
S. M. Czarnezki determined the percentage contributions
as: 26% municipal-related (sewage effluent), 17% from ag-
ricultural activities, 11% from industrial operations, 8% by
transportation
accidents, 7% each by oxygen depletions,
nonindustrial operations, and mining, 4% by disease, 3% by
“other” factors, and 10% as undetermined.
Fish kills may occur quite rapidly, even within minutes
of a major toxic spill. Usually, however, the process takes
days or even months, especially in natural causes. Experi-
enced fishery biologists usually need a wide variety of physi-
cal, chemical, and biological tests of the
habitat
and fish
to determine the exact causative agent or agents. The investi-
gative procedure is often complex and may require a lot
of time.
Species
of fish vary in their susceptibility to the differ-
ent factors that contribute to die-offs. Some species are
sensitive to almost any disturbance, while other fish are
tolerant of changes. As discussed below, predatory fish at
the top of the
food chain/web
are typically the first fish
affected by toxic substances that accumulate slowly in the
water.
The most common contributor to fish kills by natural
causes is oxygen depletion, which occurs when the amount of
oxygen utilized by
respiration
,
decomposition
, and other
processes exceeds oxygen input from the
atmosphere
and
photosynthesis
. Oxygen is more soluble in cold than warm
water. Summer fish kills occur when lakes are thermally
stratified. If the lake is eutrophic (highly productive), dead
plant and animal matter that settles to the bottom undergoes
decomposition, utilizing oxygen. Under windless conditions,
more oxygen will be used than is gained, and animals like
fish and
zooplankton
often die from suffocation.
Winter fish kills can also occur. Algae can photosyn-
thesize even when the lake is covered with ice because sun-
light can penetrate through the ice. However, if heavy snow-
fall accumulates on top of the ice, light may not reach the
underlying water, and the
phytoplankton
die and sink to
the bottom.
Decomposers
and respiring organisms again
use up the remaining oxygen and the animals eventually die.
When the ice melts in the spring, dead fish are found floating
on the surface. This is a fairly common occurrence in many
lakes in Michigan, Wisconsin, Minnesota, and surrounding
states. For example, dead alewives (Alosa pseudoharengus)
often wash up on the southwestern shore of Lake Michigan
near Chicago during spring thaws following harsh winters.
In summer and winter, artificial
aeration
can help
prevent fish kills. The addition of oxygen through aeration
and mixing is one of the easiest and cheapest methods of
dealing with low oxygen levels. In intensive
aquaculture
ponds, massive fish deaths from oxygen depletion are a con-
stant threat. Oxygen sensors are often installed to detect low
560
oxygen levels and trigger the release of pure oxygen gas from
nearby cylinders.
Natural fish kills can also result from the release of
toxic gases. In 1986, 1,700 villagers living on the shore
of Lake Nyos, Cameroon, mysteriously died. A group of
scientists sent to investigate determined that they died of
asphyxiation. Evidently a
landslide
caused the trapped
car-
bon
dioxide-rich bottom waters to rapidly rise to the surface
much like a popped champagne bottle. The poisonous gas
killed everyone in its downwind path. Fish in the upper
oxygenated waters of the lake were also killed as the
carbon
dioxide
passed through.
Hydrogen
sulfide (H
2
S), a foul-smelling gas naturally
produced in the oxygen-deficient sediments of eutrophic
lakes, can also cause fish deaths. Even in oxygenated waters,
high H
2
S levels can cause a condition in fish called “brown
blood.” The brown color of the blood is caused by the forma-
tion of sulfhemoglobin, which inhibits the blood’s oxygen-
carrying capacity. Some fish survive, but sensitive fish such
as trout usually die.
Fish kills can also result from toxic algal blooms. Some
bluegreen algae in lakes and dinoflagellates in the ocean
release
toxins
that can kill fish and other vertebrates, includ-
ing humans. For example, dense blooms of bluegreen algae
such as Anabaena, Aphanizomenon, and Microcystis have
caused fish kills in many farm ponds during the summer.
Fish die not only from the toxins but also from asphyxiation
resulting from decomposition of the mass of algae that also
die due to lack of sunlight in the densely-populated lake
water. In marine waters, toxic dinoflagellate blooms called
red tides are notorious for causing massive fish kills. For
example, blooms of Gymnodinium or Gonyaulax periodically
kill fish along the East and Gulf Coasts of the United States.
Die-offs of
salmon
in aquaculture pens along the southwest-
ern shoreline of Norway have been blamed on these organ-
isms. Millions of dollars can be lost if the fish are not moved
to clear waters. Saxitoxin, the toxic chemical produced by
Gonyaulax, is 50 times more lethal than strychnine or curare.
Pathogens and parasites can also contribute to fish
kills. Usually the effect is more secondary than direct. Fish
weakened by parasites or infections of bacteria or viruses
usually are unable to adapt to and survive changes in water
temperature and chemistry. Under stressful conditions of
over-crowding and malnourishment, gizzard shad often die
from minor infestations of the normally harmless bacterium
Aeromonas hydrophila. In the same way, fungal infections
such as Ichthyophonus hoferia can contribute to fish kills.
Most fresh water aquarium keepers are familiar with the
threat of “ick” for their fish. The telltale white spots under
the epithelium of the fins, body, and gills are caused by the
protozoan parasite Ichthyophthirius multifiliis.

Environmental Encyclopedia 3
Fisheries and Oceans Canada
Changes in
pH
of lakes resulting from
acid
rain are
a modern example of how humans can cause fish kills.
Atmo-
spheric pollutants
such as
nitrogen
dioxide and
sulfur
dioxide
released from automobiles and industries mix with
water vapor and cause the rainwater to be more acid than
normal (>pH 6.5). Nonprotected lakes downwind that re-
ceive this rainfall increase in acidity, and sensitive fish even-
tually die. Most of the once-productive trout streams and
lakes in the southern half of Norway are now devoid of these
prized fish. Sweden has combatted this problem by adding
enormous quantities of lime to their affected lakes in the
hope of neutralizing the acid’s effects.
Sewage treatment
plants add varying amounts of
treated effluent to streams and lakes. Sometimes during
heavy rainfall raw sewage escapes the treatment process and
pollutes the aquatic
environment
. The greater the organic
matter that comprises the effluent, the more decomposition
occurs, resulting in oxygen usage. Scientists call this the
biological or
biochemical oxygen demand
(BOD), the
quantity of oxygen required by bacteria to oxidize the
or-
ganic waste
aerobically to carbon dioxide and water. It is
measured by placing a sample of the
wastewater
in a glass-
stoppered bottle for five days at 71 degrees Fahrenheit (20
degrees Celsius) and determining the amount of oxygen
consumed during this time. Domestic sewage typically has
a BOD of about 200 milligrams per liter, or 200
parts per
million
(ppm); rates for industrial waste may reach several
thousand milligrams per liter. Reports of fish kills in indus-
trialized countries have greatly increased in recent years.
Sewage effluent not only kills fish; it can also create a barrier
to fish migrating upstream because of the low oxygen levels.
For example, coho salmon will not pass through water with
oxygen levels below 5 ppm. Oxygen depletion is often more
detrimental to fish than thermal shock.
Toxic
chemical spills
, whether via sewage treatment
plants or other sources, are the major cause of fish kills.
Sudden discharges of large quantities of highly toxic
substances usually cause massive death of most aquatic
life. If they enter the
ecosystem
at sublethal levels over
a long time, the effects are more subtle. Large predatory
or omnivorous fish are typically the first ones affected.
This is because toxic
chemicals
like methyl
mercury
,
DDT, PCBs, and other organic pollutants have an affinity
for fatty tissue and progressively accumulate in organisms
up the food chain. This is called the principle of
biomagni-
fication
. Unfortunately for human consumers, these fish
do not usually die right away, so people who eat a lot
of tainted fish become sick and possibly die. Such is the case
for
Minamata disease
, named for the first documented
connection between the death of fishermen and methyl
mercury contamination.
[John Korstad]
561
R
ESOURCES
B
OOKS
Czarnezki, J. M. A Summary of Fish Kill Investigations in Missouri, 1970–
1979. Columbia, MO: Missouri Dept. of Conservation, 1983.
Ehrlich, P. R., A. H. Ehrlich, and J. P. Holdren. Ecoscience: Population,
Resources, Environment. San Francisco: W. H. Freeman, 1977.
Goldman, C. R., and A. J. Horne. Limnology. New York: McGraw-
Hill, 1983.
Hill, D. M. “Fish Kill Investigation Procedures.” In Fisheries Techniques,
edited by L. A. Nielson and D. L. Johnson. Bethesda, MD: American
Fisheries Society, 1983.
Meyer, F. P., and L. A. Barclay, eds. Field Manual for the Investigation of
Fish Kills. Washington, DC: U.S. Fish and Wildlife Service, 1990.
Moyle, P. B., and J. J. Cech Jr. Fishes: An Introduction to Ichthyology. 2nd
ed. New York: Prentice-Hall, 1988.
P
ERIODICALS
Keup, L. E. “How to ’Read’ A Fish Kill.” Water and Sewage Works 12
(1974): 48–51.
Fish nets
see
Drift nets; Gill nets
Fisheries and Oceans Canada
The Department of Fisheries and Oceans (DFO) in Canada
was created by the Department of Fisheries and Oceans Act
on April 2, 1979. This act formed a separate government
department from the Fisheries and Marine Service of the
former Department of Fisheries and the Environment. The
new department was needed, in part, because of increased
interest in the management of Canada’s oceanic resources,
and also because of the mandate resulting from the unilateral
declaration of the 200-nautical-mi Exclusive Economic
Zones in 1977.
At its inception, the DFO assumed responsibility for
seacoast and inland fisheries, fishing and recreational vessel
harbors, hydrography and ocean science, and the coordina-
tion of policy and programs for Canada’s oceans. Four main
organizational units were created: Atlantic Fisheries, Pacific
and Freshwater Fisheries, Economic Development and Mar-
keting, and Ocean and Aquatic Science. Among the activi-
ties included in the department’s original mandate were:
comprehensive husbandry of fish stocks and protection of
habitat
; “best use” of fish stocks for optimal socioeconomic
benefits; adequate hydrographic surveys; the acquisition of
sufficient knowledge for defense,
transportation
, energy
development and fisheries, with provision of such informa-
tion to users; and continued development and maintenance
of a national system of harbors.
Since its inception, the department’s mandate has
changed in minor ways, to include new terminology such as
“sustainability” and to include Canada’s “ecological inter-

Environmental Encyclopedia 3
Floatable debris
ests.” Recently, attention has been given to support those
who make their living or benefit from the sea. This constitu-
ency includes the public first, but the DFO also directs
its efforts toward commercial fishers, fish plant workers,
importers, aquaculturists, recreational fishers, native fishers,
and the ocean manufacturing and service sectors. There are
now six DFO divisions: Science, Atlantic Fisheries, Pacific
Fisheries, Inspection Services, International, and Corporate
Policy and Support administered through six regional offices.
A primary focus of DFO’s current work is the failing
cod and groundfish stocks in the Atlantic; the department
has commissioned two major inquiries in recent years to
investigate those problems. In addition, the DFO has in-
creased regulation of foreign fleets, and works to manage
straddling stocks in the Atlantic
Exclusive Economic Zone
through the North Atlantic Fisheries Organization, the Pa-
cific drift nets fisheries, recreational fishing and
aquaculture
development. In 1992, management problems in the major
fisheries arose on both the Pacific and Atlantic coasts. Amer-
ican fisheries managers reneged on quotas established
through the Pacific
Salmon
Treaty, northern cod stocks in
Newfoundland virtually failed, and the Aboriginal Fishing
Strategy was adopted as part of a land claim settlement on
the Pacific coast.
There are several major problems associated with
ocean resource and environment management in Canada—
problems that the DFO has neither the resources, the legisla-
tive infrastructure, nor the political will to address. One
result of this has been the steady decline of commercial fish
stocks, highlighted by the virtual collapse of Atlantic cod
(Gadus callarias), which is Canada’s, and perhaps, the Atlan-
tic’s most historically significant fishery. A second result has
been an increased need to secure international agreements
with Canada’s ocean neighbors. A third result of social sig-
nificance is the perception that fisheries have been used in
a political sense in cases of regional economic incentives
and land claims settlements. See also Commercial fishing;
Department of Fisheries and Oceans (DFO), Canada
[David A. Duffus]
Fishing
see
Commercial fishing; Drift nets; Gill
nets
Fission
see
Nuclear fission
562
Floatable debris
Floatable debris is buoyant
solid waste
that pollutes water-
ways. Sources include boats and shipping vessels, storm water
discharge
, sewer systems, industrial activities, offshore drill-
ing, recreational beaches, and landfills. Even waste dumped
far from a water source can end up as floatable debris when
flooding
, high winds, or other weather conditions transport
it into rivers and streams.
According to the U.S.
Environmental Protection
Agency
(EPA), floatable debris is responsible for the death
of over 100,000 marine mammals and one million seabirds
annually.
Seals
,
sea lions
,
manatees
,
sea turtles
, and
other marine creatures often mistake debris for food, eating
objects that block their intestinal tract or cause internal
injury. They can also become entangled in lost fishing nets
and line, six-pack rings, or other objects.
Fishing nets lost at sea catch tons of fish that simply
decompose, a phenomenon known as “ghost fishing.” Often,
seabirds are ensnared in these nets when they try to eat
the fish.
Lost nets and other entrapping debris are also a danger
for humans who swim, snorkel, or scuba dive. And biomedi-
cal waste and sewage can spread disease in recreational wa-
ters. Floatable debris takes a significant financial toll as well.
It damages boats, deters tourism, and negatively impacts the
fishing industry.
[Paula Anne Ford-Martin]
R
ESOURCES
B
OOKS
Coe, James, and Donald Rogers, eds. Marine Debris: Sources, Impacts, and
Solutions New York: Springer-Verlag, 1996.
P
ERIODICALS
Miller, John. “Solving the Mysteries of Ocean-borne Trash.” U.S. News &
World Report 126, no.14 (April 1999): 48.
O
THER
U.S. Environmental Protection Agency, Office of Water, Oceans and
Coastal Protection Division. Assessing and Monitoring Floatable Debris—
Draft. [cited May 11, 2002]. <http://www.epa.gov/owow/oceans/debris/
floatingdebris>.
U.S. Environmental Protection Agency, Office of Water, Oceans and
Coastal Protection Division. Turning the Tide on Trash: A Marine Debris
Curriculum [cited May 2002]. <http://www.epa.gov/owow/OCPD/Ma-
rine/contents.htm>.
O
RGANIZATIONS
The Center for Marine Conservation, 1725 DeSales Street, N.W., Suite
600, Washington, DC USA 20036 (202) 429-5609, Fax: (202) 872-0619,
Email: cmc@dccmc.org, http://www.cmc-ocean.org

Environmental Encyclopedia 3
Flooding
Flooding in Texas caused by Hurricane Beulah in 1967. (National Oceanic and Atmospheric Administration.)
Flooding
Technically, flooding occurs when the water level in any
stream, river, bay, or lake rises above bank full. Bays may
flood as the result of a tsunami or tidal wave induced by an
earthquake
or volcanic eruption; or as a result of a tidal
storm surge caused by a
hurricane
or tropical storm moving
inland. Streams, rivers and lakes may be flooded by high
amounts of surface
runoff
resulting from widespread precip-
itation or rapid snow melt. On a smaller scale, flash floods
due to extremely heavy precipitation occurring over a short
period of time can flood streams, creeks, and low lying areas
in a matter of a few hours. Thus, there are various temporal
and spatial scales of flooding. Historical evidence suggests
that flooding causes greater loss of life and property than
any other natural disaster. The magnitude, seasonality, fre-
quency, velocity, and load are all properties of flooding which
are studied by meteorologists, climatologists, and hydrolo-
gists.
Spring and winter floods occur with some frequency
primarily in the mid-latitude regions of the earth, and partic-
ularly where continental
climate
is the norm. Five climatic
563
features contribute to the spring and winter flooding poten-
tial of any individual year or region: 1) heavy winter snow
cover; 2) saturated soils or soils at least near their
field
capacity
for storing water; 3) rapid melting of the winter’s
snow pack; 4) frozen
soil
conditions which limit
infiltration
;
and 5) somewhat heavy rains, usually from large scale cy-
clonic storms. Any combination of three of these five climatic
features usually leads to some type of flooding. This type of
flooding can cause hundreds of millions of dollars in property
damage, but it can usually be predicted well in advance,
allowing for evacuation and other protective action to be
taken (sandbagging, for instance). In some situations flood
control measures such as stream or channel diversions,
dams
, and levees can greatly reduce the risk of flooding.
This is more often done in
floodplain
areas with histories
of very damaging floods. In addition,
land use
regulations,
encroachment statutes and building codes are often intended
to protect the public from the risk of flooding.
Flash flooding is generally caused by violent weather,
such as severe thunderstorms and hurricanes. This type of
flooding more frequently occurs during the warm season
when convective thunderstorms develop more frequently.

Environmental Encyclopedia 3
Floodplain
Rainfall intensity is so great that the
carrying capacity
of
streams and channels is rapidly exceeded, usually within
hours, resulting in sometimes life-threatening flooding. It
is estimated that the average death toll in the United States
exceeds 200 per year as a result of flash flooding. Many
government weather services provide the public with flash
flood watches and warnings to prevent loss of life. Many
flash floods occur as the result of afternoon and evening
thundershowers which produce rainfall intensities ranging
from a few tenths of an inch per hour to several inches per
hour. In some highly developed urban areas, the risk of flash
flooding has increased over time as the native vegetation
and soils have been replaced by buildings and pavement
which produce much higher amounts of surface runoff. In
addition, the increased usage of parks and recreational facili-
ties which lie along stream and river channels has exposed
the public to greater risk. See also Urban runoff
[Mark W. Seeley]
R
ESOURCES
B
OOKS
Battan, L. J. Weather In Your Life. San Francisco: W. H. Freeman, 1983.
Critchfield, H. J. General Climatology. 4th ed. Englewood Cliffs, NJ: Pren-
tice-Hall, 1983.
Floodplain
An area that has been built up by stream deposition, generally
represented by the main
drainage
channel of a
watershed
,
is called a floodplain. This area, usually relatively flat with
respect to the surrounding landscape, is subject to periodic
flooding
, with
return periods ranging from one year to 100 years.
Floodplains vary widely in size, depending on the area of
the drainage basin with which they are associated. The soils
in floodplains are often dark and fertile, representing material
lost the to erosive forces of heavy precipitation and
runoff
.
These soils are often farmed, though subject to the risk of
periodic crop losses due to flooding. In some areas, flood-
plains are protected by flood control measures such as reser-
voirs and levees and are used for farming or residential devel-
opment. In other areas, land-use regulations, encroachment
statutes and local building codes often prevent development
on floodplains.
Flora
All forms of plant life that live in a particular geographic
region at a particular time in history. A number of factors
determine the flora in any particular area, including tempera-
ture, sunlight,
soil
, water, and evolutionary history. The
564
flora in any given area is a major factor in determining the
type of
fauna
found in the area. Scientists have divided the
earth’s surface into a number of regions inhabited by distinct
flora. Among these regions are the African-Indian
desert
,
western African
rain forest
, Pacific North American region,
Arctic and Sub-arctic region, and the Amazon.
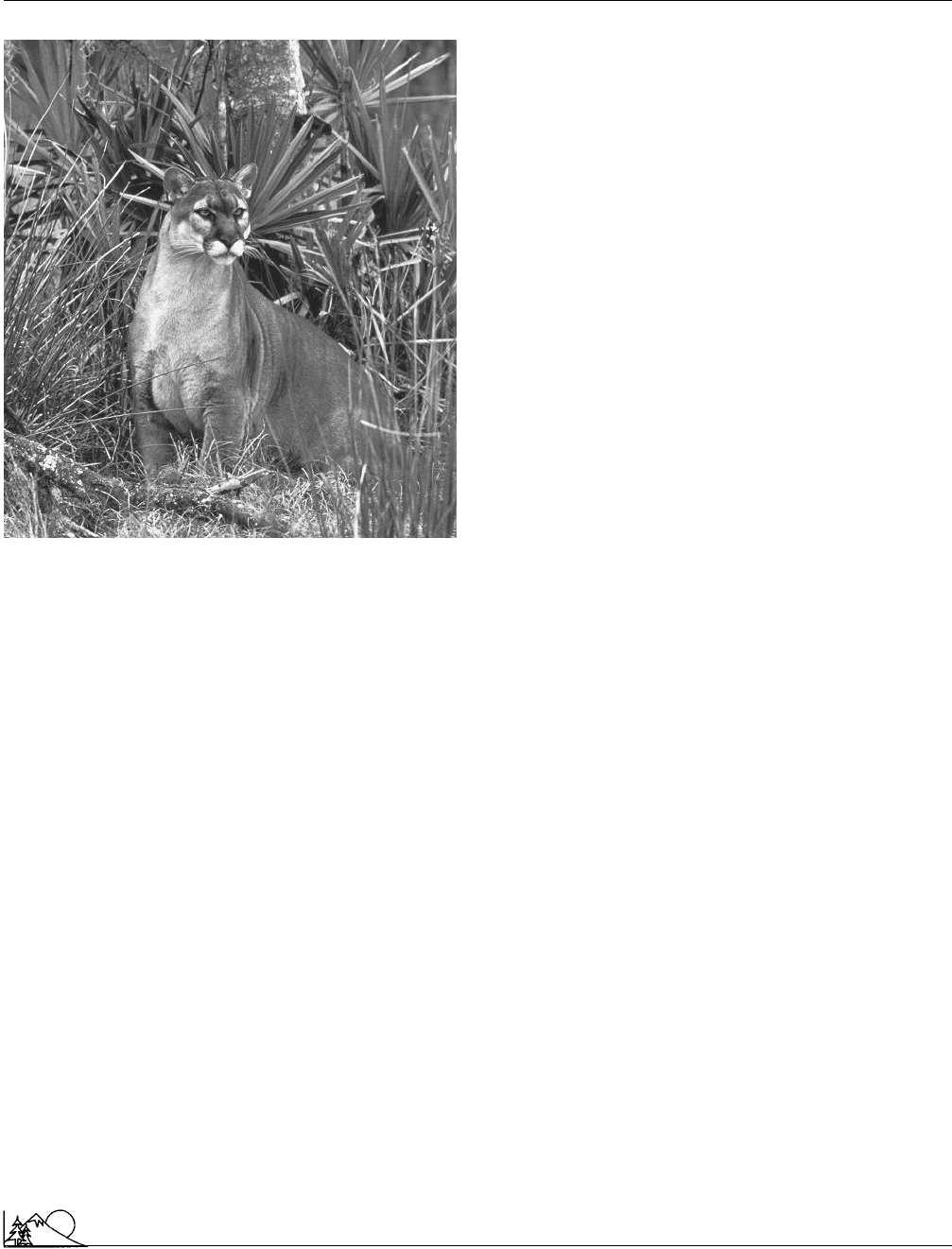
Florida panther
The Florida panther (Felis concolor coryi), a subspecies of the
mountain lion, is a member of the cat family, Felidae, and
is severely threatened with
extinction
. Listed as endangered,
the Florida panther population currently numbers between
30 and 50 individuals. Its former range probably extended
from western Louisiana and Arkansas eastward through
Mississippi, Alabama, Georgia, and southwestern South
Carolina to the southern tip of Florida. Today the Florida
panther’s range consists of the Everglades-Big Cypress
Swamp area. The preferred
habitat
for this large cat is
subtropical forests comprised of dense stands of trees, vines,
and shrubs, typically in low, swampy areas.
Several factors have contributed to the decline of the
Florida panther. Historically the most significant factors
have been habitat loss and persecution by humans.
Land
use
patterns have altered the
environment
throughout the
former range of the Florida panther.
With shifts to cattle ranching and agriculture, lands
were drained and developed, and with the altered vegetation
patterns came a change in the prey base for this top carnivore.
The main prey item of the Florida panther is white-tailed deer
(Odocoileus virginianus). Formerly, the spring and summer
rains kept the area wet, and then, as it dried out, fires would
renew the grassy meadows at the forest edges, creating an ideal
habitat for the deer. With development and increased deer
hunting
by humans, the panther’s prey base declined and so
did the number of panthers. Prior to the 1950s, Florida had
a bounty on Florida panthers because the animal was consid-
ered a “threat” to humans and livestock. During the 1950s,
state law protected the dwindling population of panthers. In
1967 the Florida panther was listed by the U. S.
Fish and
Wildlife Service
as an
endangered species
.
Land development is still moving southward in Flor-
ida. With the annual influx of new residents, fruit orchards
being moved south due to recent freezes, and continued
draining and clearing of land, panther habitat continues to
be destroyed. The Florida panther is forced into areas that
are not good habitat for white-tailed deer, and the panthers
are catching armadillos and raccoons for food. The panthers
then become underweight and anemic due to poor nutrition.
Environmental Encyclopedia 3
Flu pandemic
A Florida panther (
Felis concolor coryi
). (Photo-
graph by Tom and Pat Leeson. Photo Researchers Inc.
Reproduced by permission.)
Development contributes to the Florida panther’s de-
cline in other ways, too. Its range is currently split in half
by the east-west highway known as Alligator Alley. During
peak seasons, over 30,000 vehicles traverse this stretch of
highway daily, and, since 1972, 44 panthers have been killed
by cars, the largest single cause of death for these cats in
recent decades.
Biology is also working against the Florida panther.
Because of the extremely small population size,
inbreeding
of panthers has yielded increased reproductive failures, due
to deformed or infertile sperm. The spread of feline distem-
per
virus
also is a concern to
wildlife
biologists. All these
factors have led officials to develop a recovery plan that
includes a captive breeding program using a small number
of injured animals, as well as a mark and recapture program,
using radio collars, to
inoculate
against disease and track
young panthers with hopes of saving this valuable part of
the biota of south Florida’s
Everglades ecosystem
.
[Eugene C. Beckham]
R
ESOURCES
B
OOKS
Belden, R. “The Florida Panther.” Audubon Wildlife Report 1988/1989. San
Diego: Academic Press, 1988.
565
Fergus, Charles. Swamp Screamer: At Large with the Florida Panther. New
York: North Point Press, 1996.
Miller, S. D., and D. D. Everett, eds. Cats of the World: Biology, Conservation,
and Management. Washington, DC: National Wildlife Federation, 1986.
O
THER
Florida Panther Net. [cited May 2002]. <http://www.panther.state.fl.us>.
Florida Panther Society. [cited May 2002]. <http://www.atlantic.net/~oldfla/
panther/panther.html>.
Flotation
An operation in which submerged materials are floated, by
means of air bubbles, to the surface of a water and removed.
Bubbles are generated through a system called dissolved air
flotation (DAF), which is capable of producing clouds of
very fine, very small bubbles. A large number of small-sized
bubbles is generally most efficient for removing material
from water.
This process is commonly used in
wastewater
treat-
ment and by industries, but not in
water treatment
. For
example, the mining industry uses flotation to concentrate
fine ore particles, and flotation has been used to concentrate
uranium
from sea water. It is commonly used to thicken
the sludges and to remove grease and oil at wastewater
treatment plants. The textile industry often uses flotation
to treat process waters resulting from dyeing operations.
Flotation might also be used to remove surfactants. Materials
that are denser than water or that dissolve well in water
are poor candidates for flotation. Flotation should not be
confused with foam separation, a process in which surfac-
tants are added to create a foam that affects the removal or
concentration of some other material.
Flu pandemic
The influenza outbreak of 1918–1919 carried off between
20 to 40 million people worldwide. The Spanish flu outbreak
differed significantly from other influenza (flu) epidemics.
It was much more lethal, and it killed a high proportion of
otherwise healthy adults. Most flu outbreaks kill only the
very young, the elderly, and people with weakened immune
systems. Scientists and public health officials have been try-
ing to learn more about Spanish flu in the hopes of pre-
venting a similar outbreak.
The Spanish flu
virus
caused one of the worst pan-
demic of an infectious disease ever recorded. And while the
threat of many infectious diseases, including tuberculosis and
smallpox, have been contained by antibiotics and vaccination
programs, influenza remains a difficult disease. There are
worldwide outbreaks of influenza every year, and the flu
typically reaches pandemic proportions (lethally afflicting an

Environmental Encyclopedia 3
Flu pandemic
unusually high portion of the population) every 10–40 years.
The last influenza pandemic was the Hong Kong flu of
1968–69, which caused 700,000 deaths worldwide, and
killed 33,000 Americans. The influenza virus is highly muta-
ble, so each year’s flu outbreak presents the human body
with a slightly different virus. Because of this, people do not
build an immunity to influenza. Vaccines are successful in
protecting people against influenza, but vaccine manufactur-
ers must prepare a new batch each year, based on their
best supposition of which particular virus will spread. Most
influenza viruses originate in China, and doctors, scientists,
and public health officials closely monitor flu cases there
in order to make the appropriate vaccine. The two main
organizations tracking influenza are the Centers for Disease
Control (CDC) and the World Health Organization
(WHO). The CDC and other government agencies have
been preparing for a flu pandemic on the level of Spanish
flu since the early 1990s.
Spanish flu did not originate in Spain, but presumably
in Kansas, where the first case was recorded in March, 1918,
at the army base Camp Funston. It quickly spread across
the United States, and then to Europe with American sol-
diers who were fighting in the last months of World War
I. Infected ships brought the outbreak to India, New
Zealand, and Alaska. Spanish flu killed quickly. People often
died within 48 hours of first feeling symptoms. The disease
afflicted the lungs, and caused the tiny air sacs, called alveoli,
to fill with fluid. Victims were soon starved of oxygen, and
sometimes effectively drowned on the fluid clogging their
lungs. Children and old people recovered from the Spanish
flu at a much higher rate than young adults. In the United
States, the death rate from Spanish flu was several times
higher for men aged 25–29 than for men in their seventies.
Social conditions at the time probably contributed to
the remarkable power of the disease. The flu struck just at
the end of World War I, when thousands of soldiers were
moving from America to Europe and across that continent.
In a peaceful time, sick people may have gone home to bed,
and thus passed the disease only to their immediate family.
But in 1918, men with the virus were packed in already
crowded hospitals and troop ships. The unrest and devasta-
tion left by the war probably hastened the spread of Spanish
flu. So it is possible that if a similarly virulent virus were to
arise again soon, it would not be quite as destructive.
Researchers are concerned about a return of Spanish
flu because little is known about what made it so virulent.
The flu virus was not isolated until 1933, and since then,
there have been several efforts to collect and study the 1918
virus by exhuming graves in Alaska and Norway, where
bodies were preserved in permanently frozen ground. In
1997, a Canadian researcher, Kirsty Duncan, was able to
extract tissue samples from the corpses of seven miners who
566
had died of Spanish flu in October 1918 and were buried
in frozen ground on a tiny island off Norway. Duncan’s
work allowed scientists at several laboratories around the
world to do genetic work on the Spanish flu virus. But by
2002, there was still no conclusive agreement on what was
so different about the 1918 virus.
The influenza virus is believed to originate in migratory
water fowl, particularly ducks. Ducks carry influenza viruses
without becoming ill. They excrete the virus in their feces.
When their feces collect in water, other animals can become
infected. Domestic turkeys and chickens can easily become
infected with influenza virus borne by wild ducks. But most
avian (bird-borne) influenza does not pass to humans, or if
it does, is not particularly virulent. But other mammals too
can pick up influenza from either wild birds or domestic fowl.
Whales
,
seals
, ferrets, horses, and pigs are all susceptible to
bird-borne viruses. When the virus moves between
species
,
it may mutate. Human influenza viruses most likely pass
from ducks to pigs to humans. The 1918 virus may have
been a particularly unusual combination of avian and swine
virus, to which humans were unusually vulnerable.
Enacting controls on pig and poultry farms may be
an important way to prevent the rise of a new influenza
pandemic. Some influenza researchers recommend that pigs
and domestic ducks and chickens not be raised together.
Separating pigs and fowl at live markets may also be a sensible
precaution. With the concentration of poultry and pigs at
huge “factory” farms, it is important for farmers, veterinari-
ans, and public health officials to monitor for influenza. A flu
outbreak among chickens in Hong Kong in 1997 eventually
killed six people, but the epidemic was stopped by the quick
slaughter of millions of chickens in the area. Any action to
control flu of course must be an international effort, since
the virus moves rapidly without respect to national borders.
[Angela Woodward]
R
ESOURCES
P
ERIODICALS
Gladwell, Malcolm. “The Dead Zone.” New Yorker (September 29, 1997):
52–65.
Henderson, C. W. “Spanish Flu Victims Hold Clues to Fight Virus.”
Vaccine Weekly (November 29, 1999/December 6, 1999): 10.
Koehler, Christopher S. W. “Zeroing in on Zoonoses.” Modern Drug Dis-
covery 8, no. 4 (August 2001): 44–50.
Lauteret, Ronald L. “A Short History of a Tragedy” Alaska (November
1999): 21–23.
Pickrell, John. “Killer Flu with a Human-Pig Pedigree?” Science 292 (May
11, 2001): 1041.
Shalala, Donna E. “Collaboration in the Fight Against Infectious Diseases.”
Emerging Infectious Diseases 4, no. 3 (July/September 1998): 354.
Webster, Robert G. “Influenza: An Emerging Disease.” Emerging Infectious
Diseases 4, no. 3 (July-September 1998).
