Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

CHAPTER 14 • Intraductal Papilloma 157
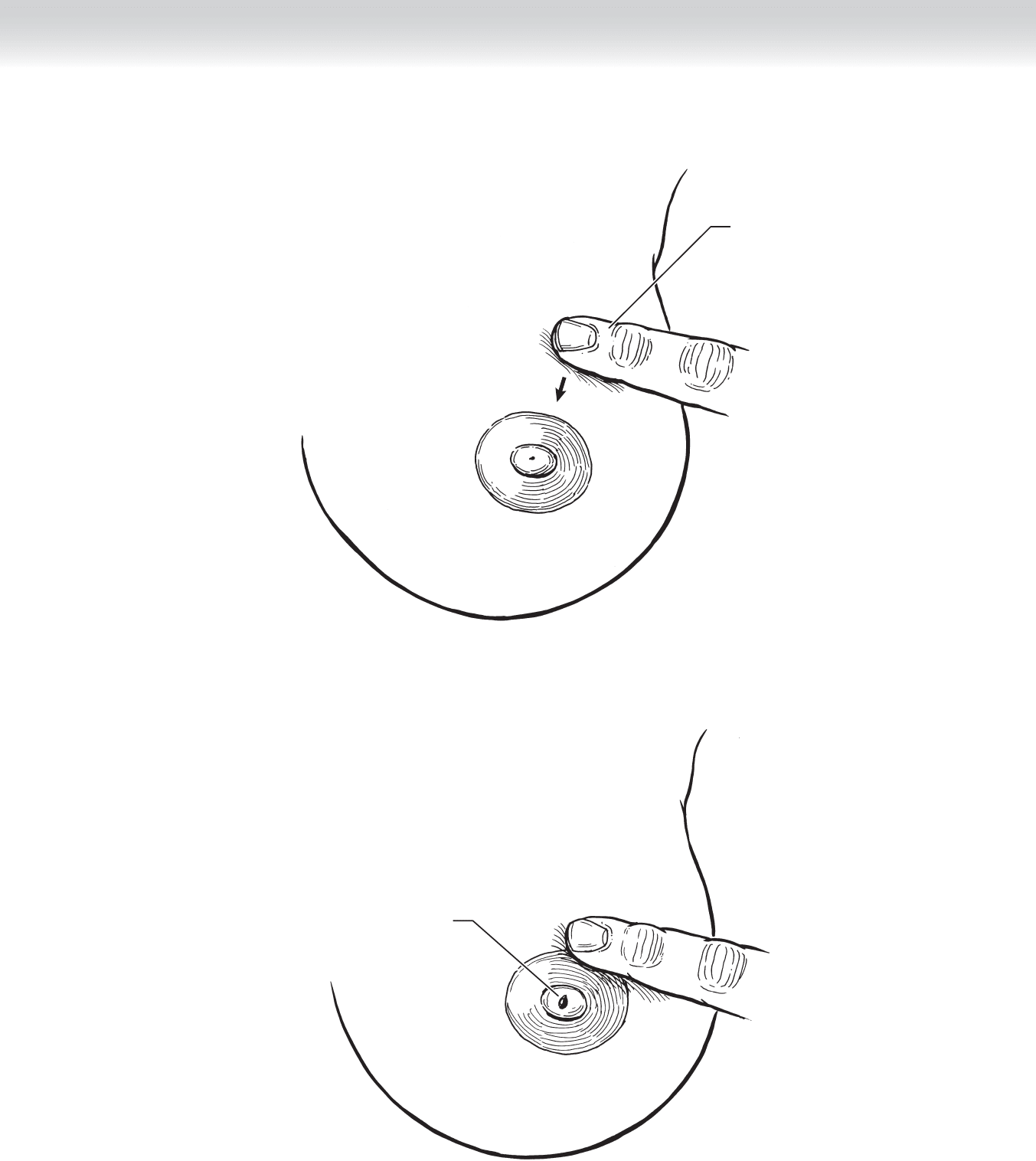
Milking duct
FIGURE 14 –2
Dab of blood
FIGURE 14 –3
158 Section II • The Breast
◆ If the involved duct cannot be identifi ed, single-digit compression in the area after the
areola is raised can be carried out to elicit discharge from the nipple, which is noted so
that the area of resection can be identifi ed (Figure 14-4).
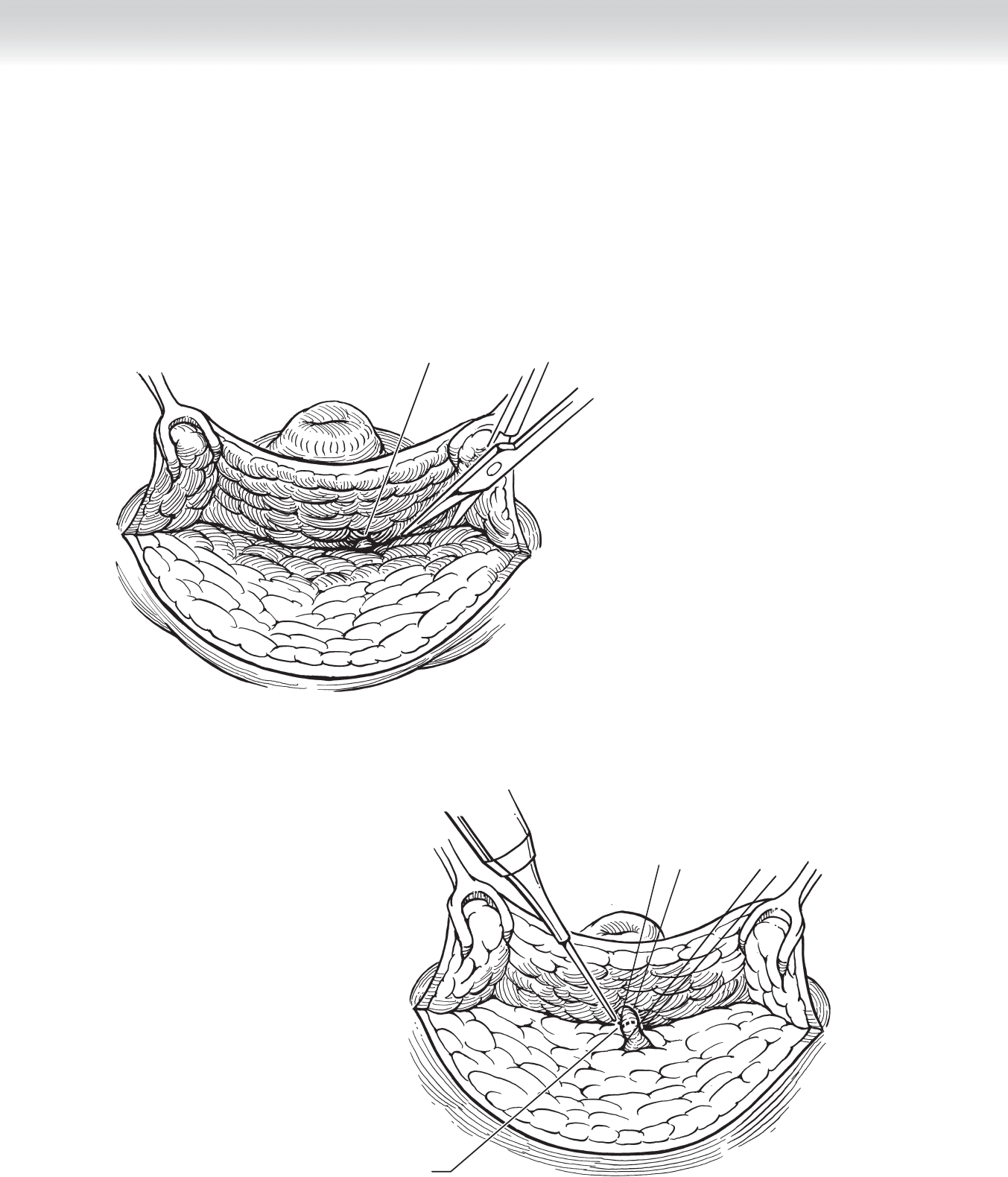
◆ Once the duct is isolated below the nipple, it is dissected free from the surrounding tissue,
ligated, and divided just below the nipple (Figures 14-5 and 14-6).
Involved duct
Duct is ligated
and transected
FIGURE 14 –4
FIGURE 14 –5
CHAPTER 14 • Intraductal Papilloma 159
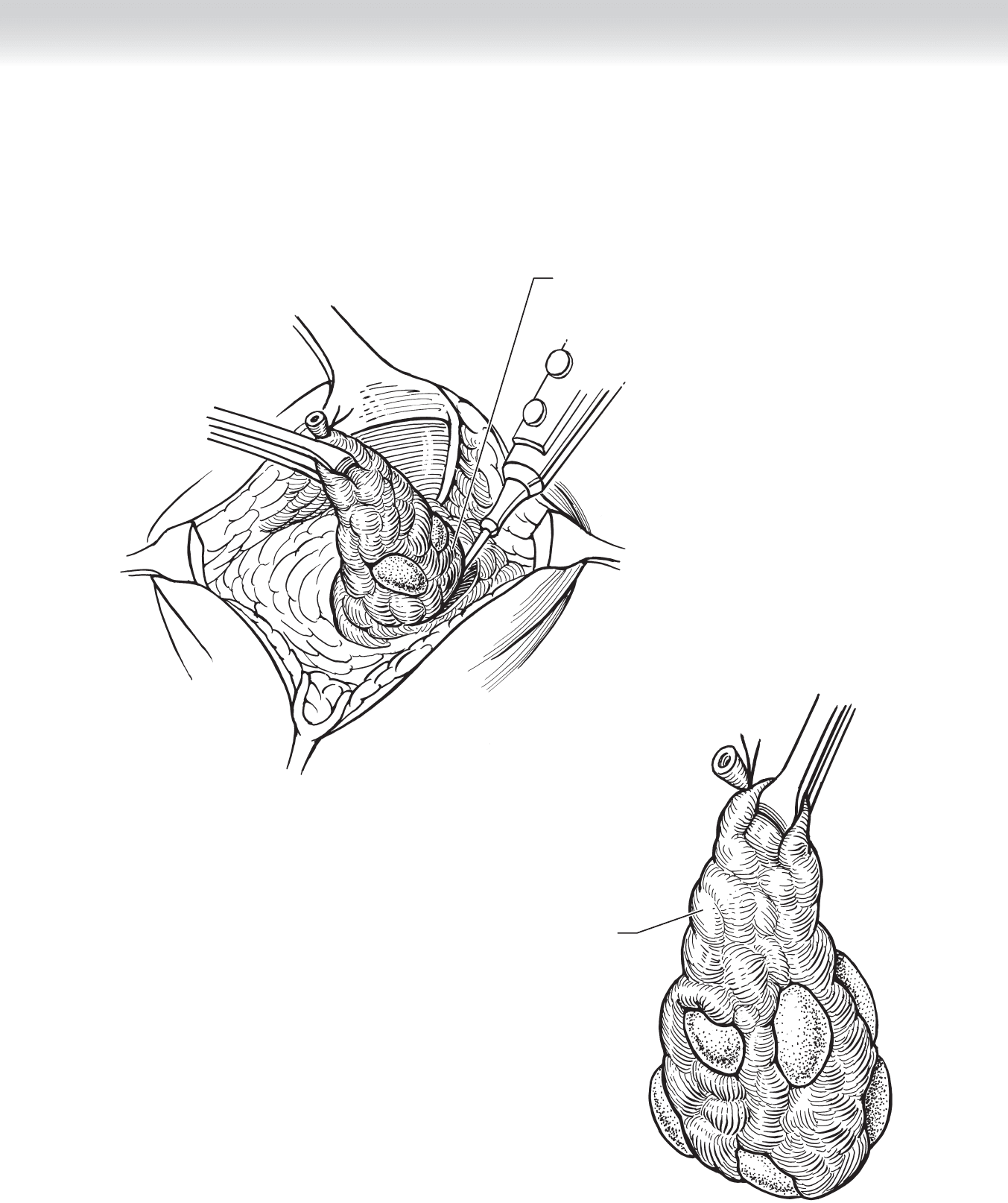
◆ The segment drained by the duct is then excised by sharp dissection (Figure 14-7). (I prefer
cautery. Although the illustration shows specimen grasped with forceps, I have come to prefer
use of a traction suture placed in a fi gure-of-eight fashion to avoid clamp dislodgment with
tearing breast tissue).
Isolated duct
under traction
and further
dissection
FIGURE 14 –6
Duct and surrounding
tissue removed
FIGURE 14 –7

160 Section II • The Breast
◆ After the specimen is excised, the wound is irrigated. I use hydrogen peroxide because it
helps localize any bleeding. Direct cautery through the foam of the peroxide can be car-
ried out.
3. CLOSURE
◆ The breast tissue is not closed. After hemostasis is secured, the incision is closed with
running subcuticular absorbable sutures and a clear plastic dressing is applied.
STEP 4: POSTOPERATIVE CARE
◆ I recommend that all patients who are going to have partial mastectomy for benign or
malignant conditions wear a new sport or jogging bra after the procedure, because it gives
good, nonrigid support to the breast.
◆ An ice pack is often helpful to relieve localized pain, and one or two doses of nonopioid anal-
gesic is usually all that is required. The dressing can be removed in the bath 24 to 36 hours
after the operation, and no further dressing needs to be used.
STEP 5: PEARLS AND PITFALLS
◆ The most important determination to be made is that pathologic nipple discharge is pres-
ent and that resection will be required. Every patient must have a preoperative mammog-
raphy, but there is no need for ductography or for cannulation of the ductal opening at the
time of operation.
◆ The duct can be identifi ed with digital compression after the incision is made, or often the
duct can be visualized and seen to be dilated, containing the dark fl uid.

162
STEP 1: SURGICAL ANATOMY
◆ A comprehensive understanding of the anatomy of the esophagus is critical before under-
taking surgical procedures on the esophagus.
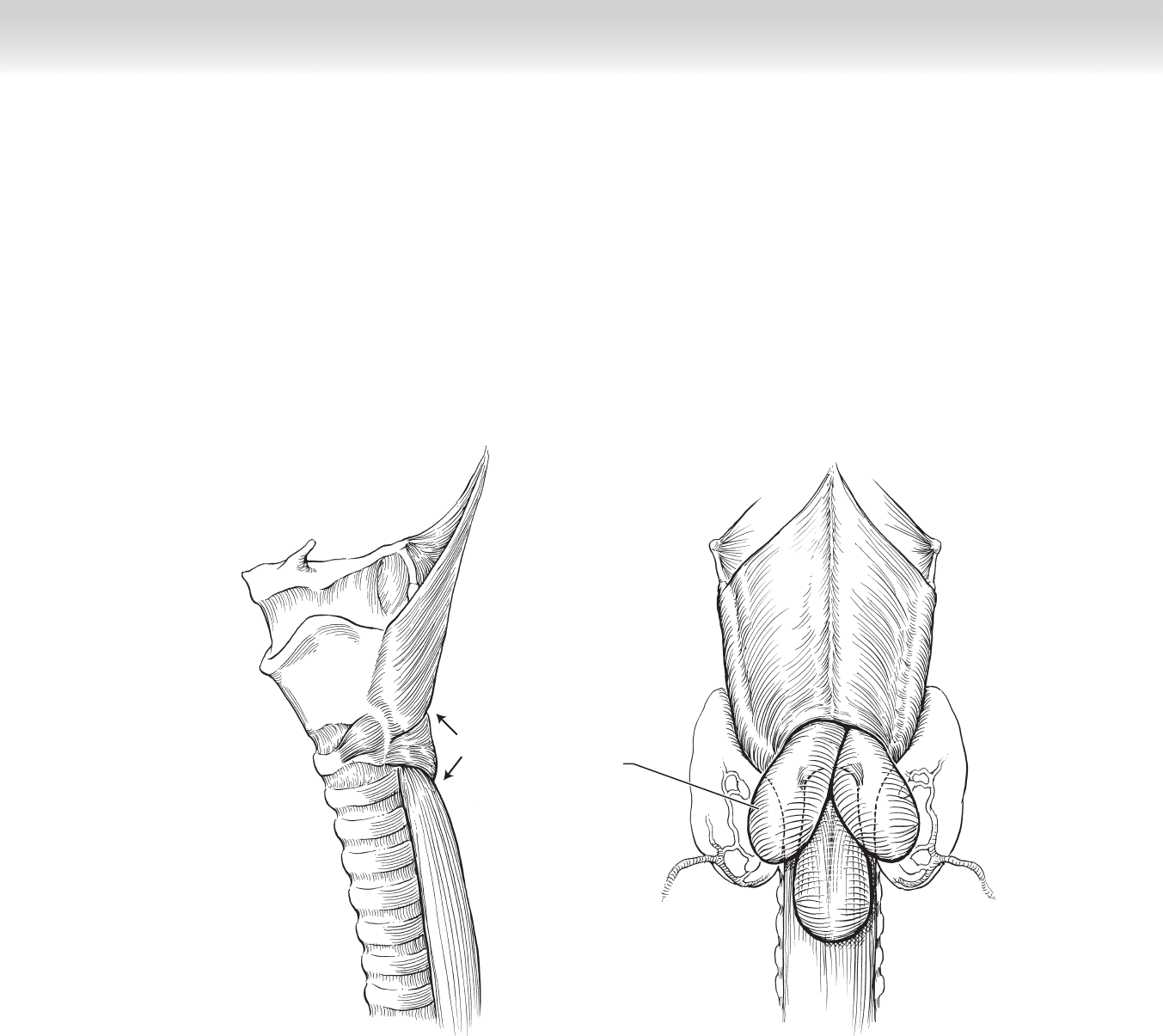
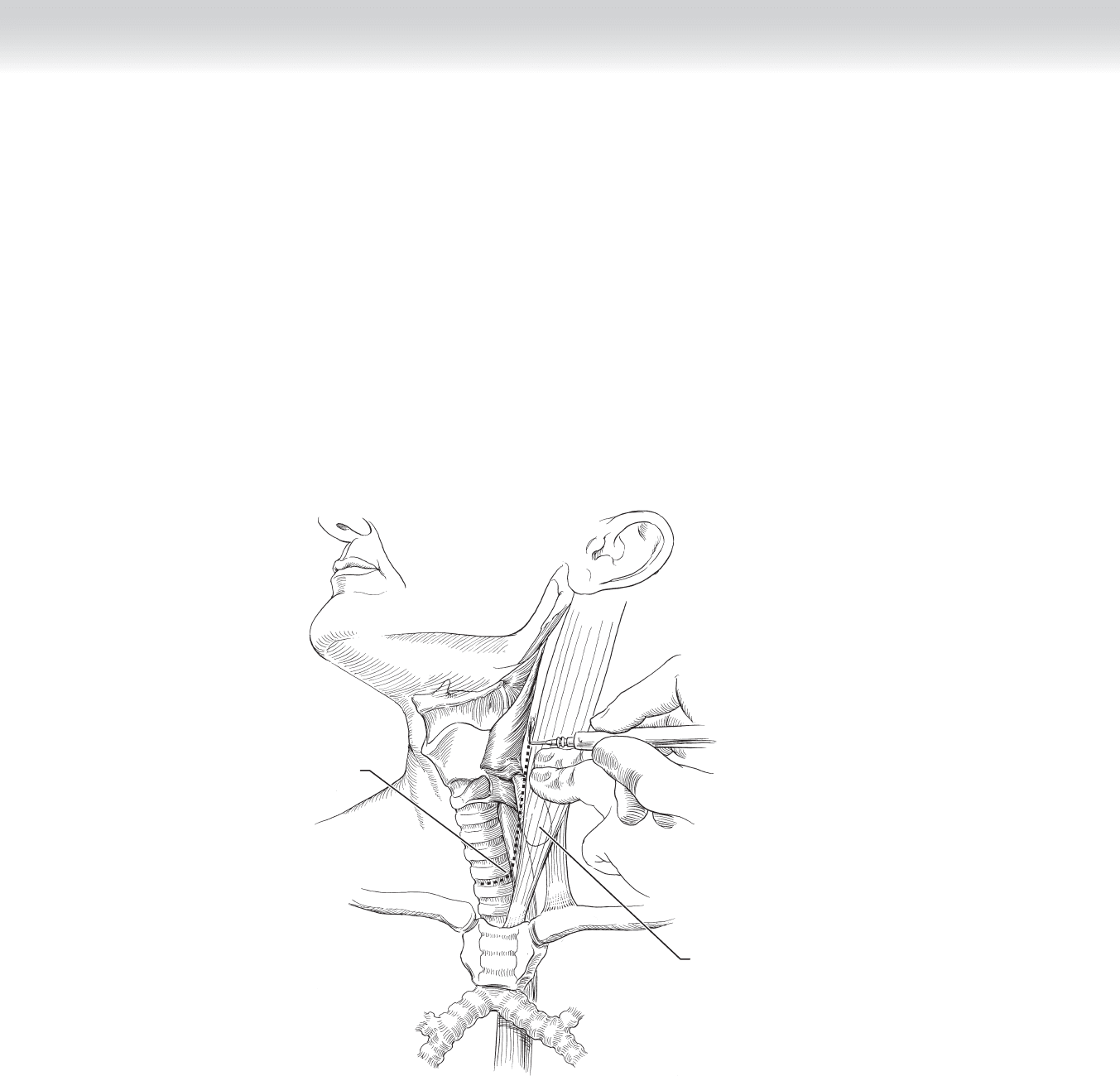
◆ Figure 15-1 demonstrates key anatomic structures that must be considered in surgical
correction of Zenker’s diverticula.
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ Pharyngoesophageal (Zenker’s) diverticula, the most common diverticula of the esophagus,
occur during the fi fth to eighth decades of life. They are classifi ed as pulsion diverticula and
consist of mucosal and submucosal esophageal layers. Zenker’s diverticula are believed to
result from either an uncoordinated relaxation or incomplete relaxation of the upper esoph-
ageal sphincter (cricopharyngeal muscle) during swallowing, resulting in higher than nor-
mal bolus pressures in the lower pharynx. This leads to herniation of the esophageal
mucosa between the oblique fi bers of the inferior constrictor muscle (superiorly) and the
transverse fi bers of the cricopharyngeal muscle (inferiorly) (see Figure 15-1). Small divertic-
ula rarely produce symptoms. However, progressive enlargement of the diverticula leads to
pronounced symptoms. Upper esophageal dysphagia, foul breath, and spontaneous
regurgitation of undigested food material are characteristically seen. Rarely is a palpable
mass encountered. Late manifestations include weight loss, hoarseness, and pulmonary
abscess. Any symptomatic Zenker’s diverticulum should be corrected.
◆ Barium esophagram is obtained to confi rm the presence of a pharyngoesophageal diverticu-
lum and localize it to the left or right side to assist in planning the surgical approach.
◆ Anesthetic approach is dictated by the comorbidities of the patient and by surgeon prefer-
ence. The procedure can be performed satisfactorily under a regional cervical block or a
general anesthetic.
CHAPTER
15
Zenker’s Diverticula
David B. Loran and Joseph B. Zwischenberger
CHAPTER 15 • Zenker’s Diverticula 163
◆ The patient is placed supine on the operating room table, with the head slightly extended
and turned away from the side of the incision. Some surgeons prefer to have the patient
semirecumbent or seated.
◆ Betadine preparation of the skin should be applied to cover the entire neck and upper
chest. This should include the area from the mastoid process to the spinous processes pos-
teriorly, along the angle of the mandible anteriorly, and to the level of the nipples inferiorly.
A
Weak areas
MC
Various
locations
for
diverticula
12
3
B
FIGURE 15–1
164 Section III • The Esophagus
STEP 3: OPERATIVE STEPS
1. INCISION
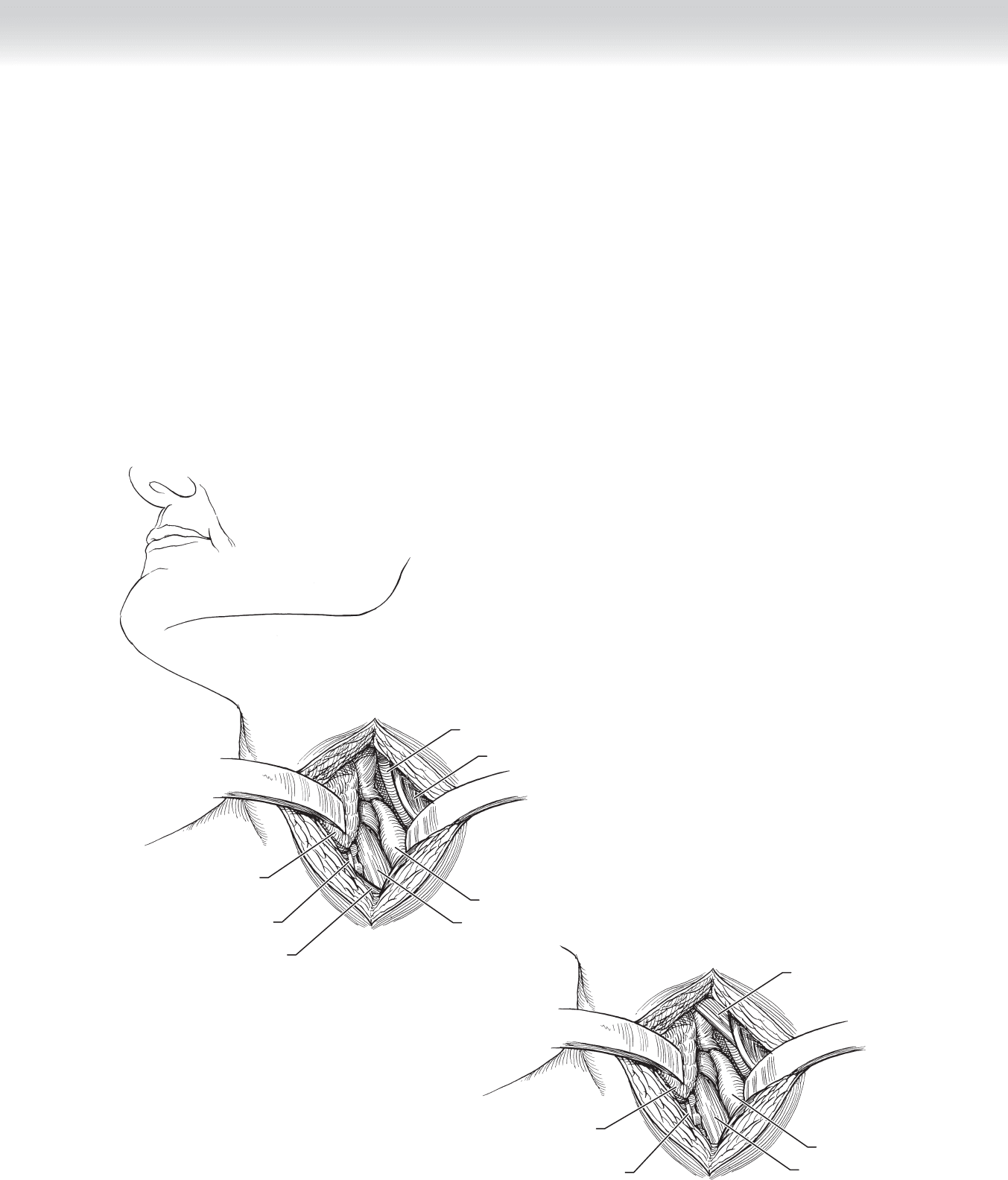
◆ Almost all diverticula are best approached through the left side of the neck. Various
incisions can be used based on surgeon preference and patient anatomy. Most surgeons use an
incision along the anterior border of the sternocleidomastoid muscle, from the level of the
hyoid bone to 1 cm above the clavicle. Alternatively, a transverse cervical incision can be used
within a prominent cervical fold centered over the middle third of the sternocleidomastoid
muscle (Figure 15-2).
Diverticulum
Skin incision
FIGURE 15–2
CHAPTER 15 • Zenker’s Diverticula 165
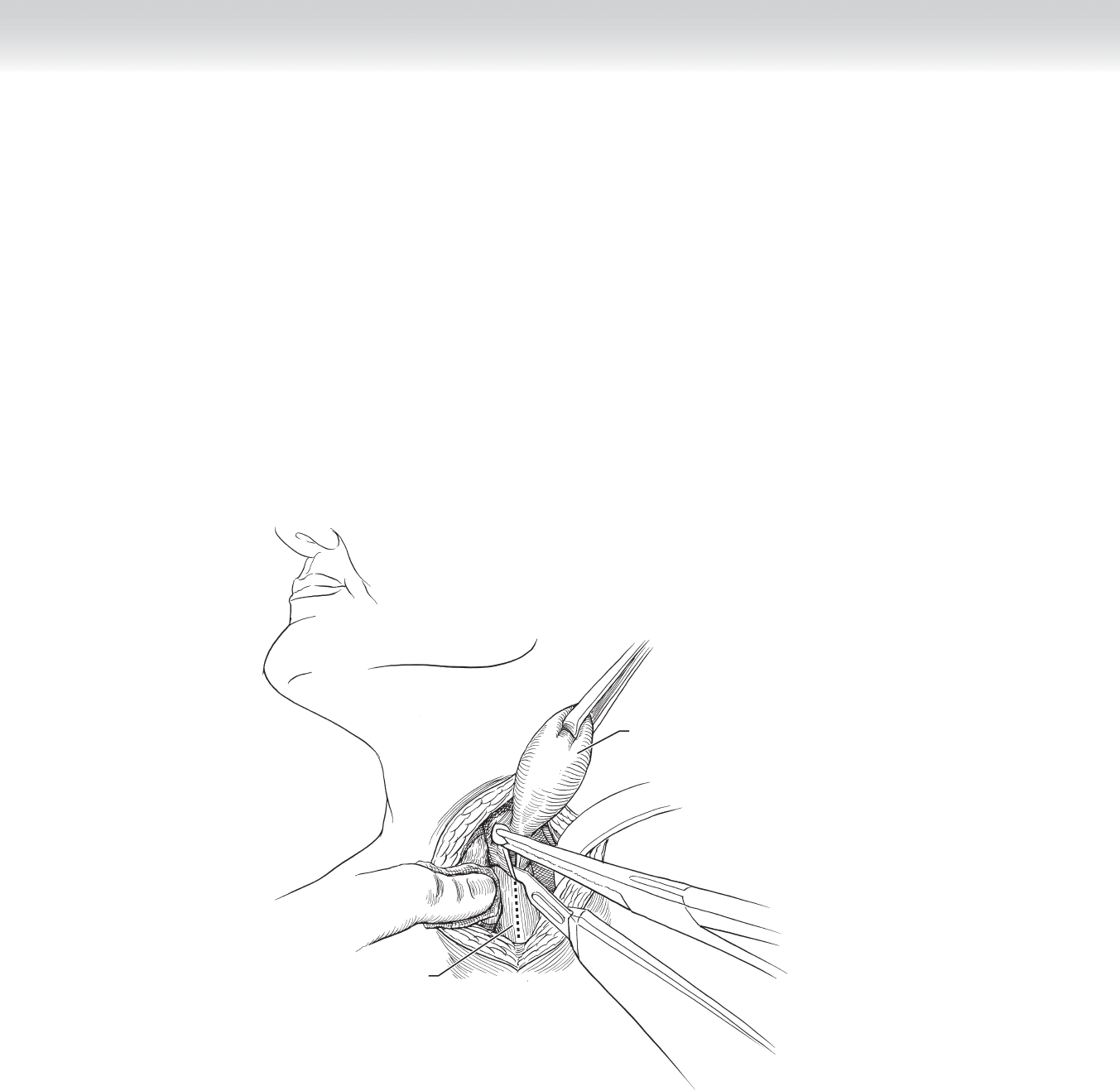
Esophagus
Diverticulum
Sternocleidomastoid
muscle
Carotid artery
Thyroid gland
Left recurrent
laryngeal nerve
Omohyoid muscle
A
Esophagus
Diverticulum
Omohyoid muscle
Thyroid gland
Left recurrent
laryngeal nerve
B
FIGURE 15–3
2. DISSECTION
◆ The incision is carried through the platysma to expose the deep cervical fascia. The sterno-
cleidomastoid muscle and carotid sheath are retracted laterally to expose the retroesopha-
geal space. Sometimes ligation of the middle thyroid vein is needed to adequately retract
the thyroid gland and larynx medially. Care should be taken to avoid excessive retraction
on the thyroid so that the recurrent laryngeal nerve, which courses superiorly in the tra-
cheoesophageal groove, is not injured.
◆ The omohyoid muscle, which can be divided, is retracted superiorly to complete exposure
of the area and should bring into view the diverticulum as it emerges superior to the crico-
pharyngeal muscle (Figure 15-3).
166 Section III • The Esophagus
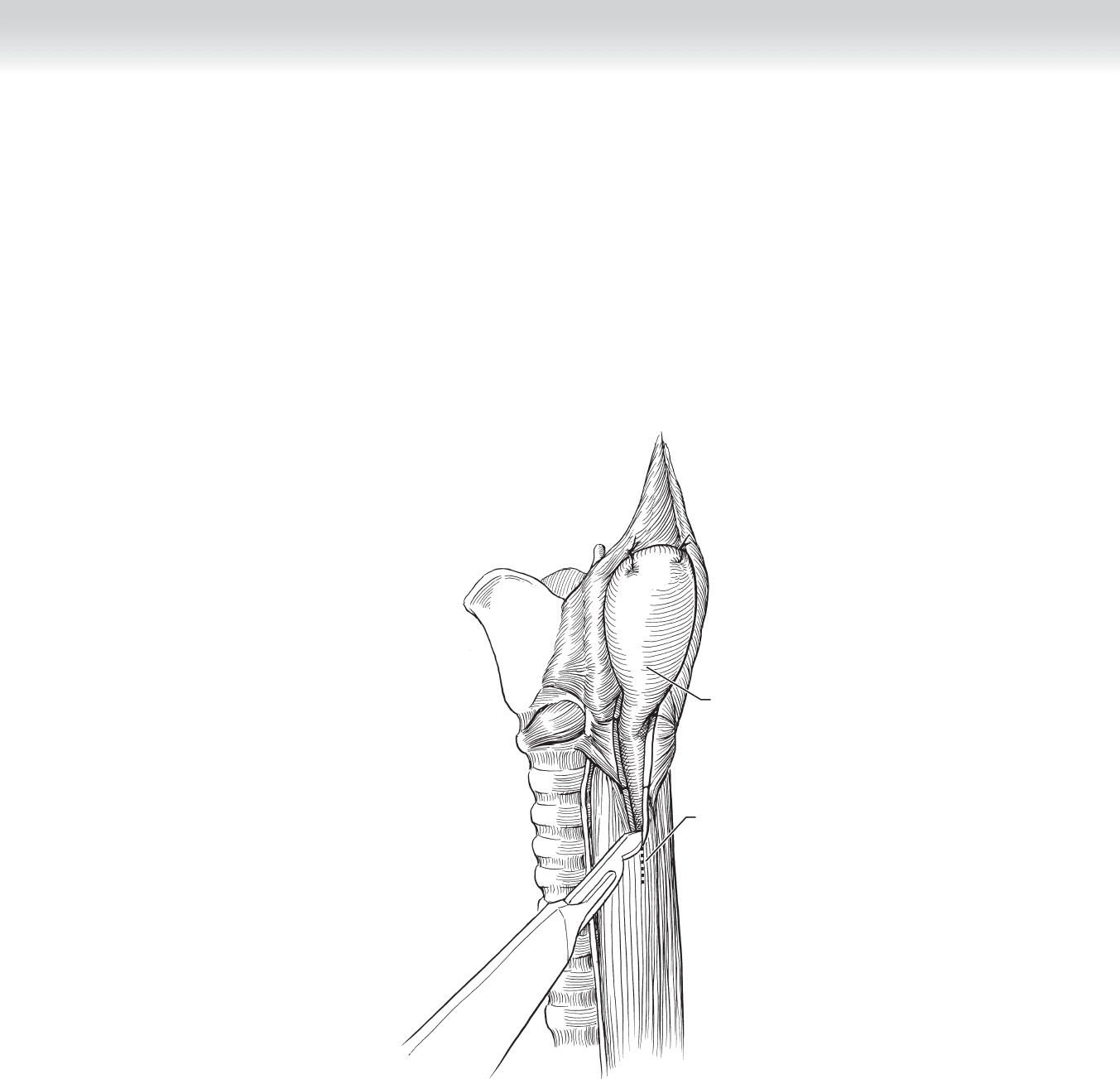
◆ The diverticulum is grasped with an Allis or Babcock clamp and dissected free from the
surrounding fi broadipose tissue to adequately expose the neck. A 36F to 40F bougie is
placed into the pharynx by the anesthesiologist to help prevent narrowing of the esophagus
with diverticulectomy and to facilitate dissection. A myotomy is performed with a no. 15
blade scalpel or Bovie electrocautery unit on low settings between a dissecting hemostat
from the base of the diverticula through the entire length of the transverse cricopharyngeal
muscle fi bers and extended onto the longitudinal muscle fi bers of the upper esophagus over
a total length of 8 to 10 cm (Figure 15-4).
Diverticulum
Thyroid gland
FIGURE 15–4
CHAPTER 15 • Zenker’s Diverticula 167
◆ The base of the diverticulum is now easily seen. Diverticula that measure less than 2 cm
long usually do not require resection, and the mucosa will retract once the myotomy is per-
formed. Those diverticula larger than 2 cm will require resection or “pex.” Many surgeons
prefer to tack, or pex, the pouch cephalad on the pharynx (Figure 15-5).
Incision
Diverticulum
FIGURE 15–5
