Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

248
LIVER AND BILIARY TRACT DISEASE
CHAPTER 35
Elan S. Levy, MD, and Kaushal H. Shah, MD
1. What are the common manifestations of biliary disease?
Cholelithiasis is the presence of gallstones in the gallbladder without evidence of
infection. Among adults, 8% of men and 17% of women have gallstones, and the
incidence increases with age with an incidence as high as 27% in the elderly.
n
Biliary colic is right upper quadrant or epigastric pain sometimes radiating to the
right shoulder or scapula. It usually lasts less than 6 hours, is persistent, not colicky,
occurs after a fatty meal, and is thought to be due to transient obstruction of the
cystic duct by a gallstone.
n
Of patients with colic, 30% progress to cholecystitis, a bacterial overgrowth and
inflammation of the gallbladder caused by obstruction of the cystic duct by a stone.
The pain with cholecystitis is similar to biliary colic but persists beyond 6 hours, is
accompanied by a Murphy’s sign, and can be present with or without fever and chills
n
Choledocholithiasis occurs when a gallstone lodges in the common bile duct (CBD)
and can cause cholecystitis or pancreatitis (if the ampulla of Vater is obstructed)
or both.
n
Ascending cholangitis is a severe infection of the biliary tract from complete biliary
obstruction (most commonly the CBD) in the presence of a bacterial infection. It
presents as right upper quadrant pain, fever and chills, and jaundice (Charcot’s triad),
although only 25% of patients have all three. It may include shock and mental status
changes (Reynold’s pentad), more commonly seen with gangrenous or
emphysematous cholecystitis
n
Emphysematous cholecystitis is caused by complete cystic duct obstruction with
subsequent abscess formation in the gallbladder wall by gas-forming bacteria. It is
seen with vascular insufficiency, severe burns, and trauma. It is more frequent in men
and diabetic patients and often is accompanied by sepsis.
2. Do all gallstones produce pain? Does a lack of stones preclude
cholecystitis?
Of patients with gallstones, 80% are asymptomatic. Of asymptomatic patients, 15% to
30% develop symptoms within 15 years. Although 90% to 95% of cholecystitis cases
are in the setting of gallstones, 5% to 10% are not secondary to cholelithiasis and
are termed acalculous cholecystitis. It is a difficult diagnosis because it is often a
complication of another process such as diabetes, burns, multisystem trauma, AIDS,
or sepsis.
3. What is Murphy’s sign?
The sign is named after a prominent Chicago surgeon, John B. Murphy (1857–1916).
The patient is asked to take a deep breath while the examiner applies pressure over the
area of the gallbladder. If the gallbladder is inflamed, the descending diaphragm forces it
against the examiner’s fingertips, causing pain and often a sudden halt to the inspiration.
A sonographic Murphy’s sign uses the ultrasound probe instead of the examiner’s
fingers and is positive when the site of maximal tenderness localizes to the gallbladder.
The finding is 97% sensitive for acute cholecystitis.
Chapter 35 LIVER AND BILIARY TRACT DISEASE 249
4. Can a plain radiograph of the abdomen aid diagnosis?
Maybe. However, ultrasound is the preferred first-line diagnostic test. Only 10% to 20% of
gallstones contain sufficient calcium to be radiopaque. Air can be seen in the biliary tree or the
gallbladder wall when infection is due to gas-forming bacteria or there is a biliary-intestinal
fistula.
5. What is the gold standard for diagnosing cholecystitis?
Although ultrasound is the test of choice in the ED, a hepatobiliary iminodiacetic acid (HIDA)
scan is the gold standard with 95% accuracy if the gallbladder does not fill with radioisotope
within 4 hours after injection.
6. Is an elevated temperature or white blood cell count necessary for diagnosis?
No, they are not helpful for diagnosis, as is seen in one study in which 71% of patients with
acute nongangrenous cholecystitis were afebrile, and 32% had normal white blood cell count.
Past the age of 60, the typical signs and symptoms may not be present. The sensitivity of the
Murphy’s sign decreases to 48% with age older than 60.
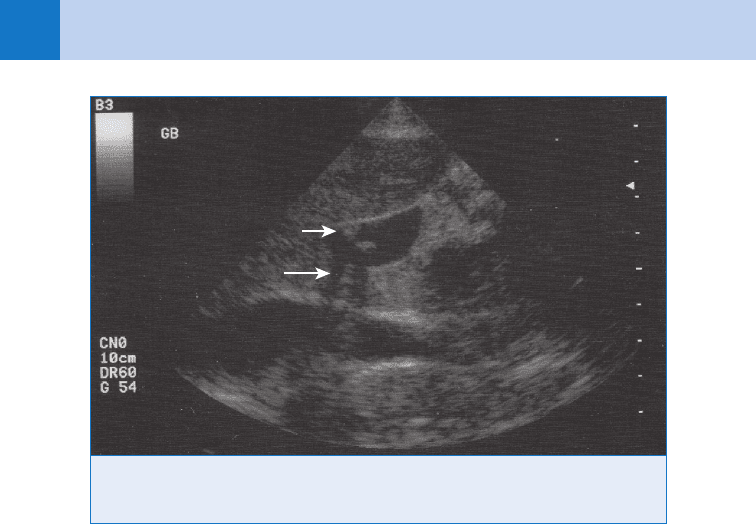
7. Describe the ultrasound findings in cholecystitis.
Gallstones as small as 2 mm can be detected directly, or sometimes their presence can be
inferred by interference with transmission of ultrasound waves (acoustic shadowing)
(Fig. 35-1). Other helpful findings include a thickened gallbladder wall (.3 mm), fluid
collections around the gallbladder (pericholecystic fluid), and common ductal dilation
(.6 mm). The ultrasound is 94% sensitive and 78% specific for identifying cholecystitis
KEY POINTS: ULTRASOUND FINDINGS OF CHOLECYSTITIS
1. Presence of gallstones
2. Gallbladder wall thickening .3 mm
3. Pericholecystic fluid
4. CBD dilatation .6 mm
8. When should elective surgery be considered in patients with asymptomatic
cholelithiasis?
Cholecystectomy should be considered in diabetics, patients with a porcelain gallbladder, and
patients with a history of biliary pancreatitis.
n
Diabetics have increased morbidity and mortality when urgent cholecystectomy is done in
the setting of cholecystitis.
n
Calcified or porcelain gallbladders have a 22% association with carcinoma.
n
The risks of pancreatitis may outweigh the risks of elective cholecystectomy.
9. What are Courvoisier’s law, Klatskin’s tumor, and Fitz-Hugh-Curtis syndrome?
n
Courvoisier’s law states that a palpable gallbladder in the setting of painless jaundice is
likely to represent obstruction of the CBD by a malignancy, usually carcinoma of the
pancreatic head.
n
Klatskin’s tumor is a malignant tumor located where the hepatic ducts form the common
duct.
n
Fitz-Hugh-Curtis syndrome is caused by pelvic inflammatory disease extending up the right
paracolic gutter, causing inflammation of the capsule of the liver (perihepatitis), and can
lead to adhesions between the liver and abdominal wall.
Chapter 35 LIVER AND BILIARY TRACT DISEASE250
10. What is a porcelain gallbladder?
A gallbladder with calcified walls. This is an important finding because 22% are associated
with carcinoma, and it is an indication for cholecystectomy in asymptomatic patients. There is
a higher incidence in women and American Indians, especially members of the Pima tribe.
11. Are all gallstones created equal?
No. The most common are cholesterol stones and usually are found in the stereotypical,
female, fat, forty, fertile patient. Patients of Asian descent, those with parasitic infections
(Ascaris lumbricoides), chronic liver/biliary disease, or chronic hemolysis states (i.e., sickle
cell, spherocytosis) are more likely to have pigment stones.
12. What is endoscopic retrograde cholangiopancreatography (ERCP)? What is
the most common complication that presents to the ED after an ERCP
procedure?
ERCP is a procedure that examines the pancreatic and bile ducts for disease or irregularities
with the ability of removing lodged stones and opening narrowed ducts with stents. The most
common serious complication is pancreatitis, which occurs in approximately 1% of cases.
13. What are liver function tests?
Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are markers of acute
liver injury and have no correlation with liver function. Liver function is analyzed best by
measuring factors affected by hepatic protein synthesis. Acute liver failure results in a
decrease in vitamin K-dependent coagulation factors (except factor VIII), leading to a
prolonged prothrombin time. The liver also synthesizes albumin, although its longer half-life
makes it a better marker of subacute or chronic liver disease.
14. What is the difference between conjugated and unconjugated bilirubinemia?
Bilirubin is a breakdown product of hemoglobin and heme-related proteins. In its unconjugated,
hydrophobic form, it is unable to be excreted into bile, although it can traverse the blood-brain
barrier and placenta. Bilirubin is conjugated in the liver with glucuronic acid, making it more
water soluble for excretion into the bile. A predominance of unconjugated bilirubin occurs when
Figure 35-1. Ultrasound image reveals an anechoic gallbladder containing two echogenic
stones, which are creating acoustic shadowing inferiorly. The short arrow is pointed to the gall-
stones within the gallbladder, and the long arrow points to the shadowing effect of the stones.
Chapter 35 LIVER AND BILIARY TRACT DISEASE 251
KEY POINTS: CRITERIA FOR ADMISSION IN PATIENT
WITH HEPATITIS
1. Coagulopathy, international normalized ratio (INR) .3
2. Active bleeding
3. Encephalopathy
4. Unable to tolerate intake by mouth
5. Social issues that make follow up care and compliance problematic
there is overproduction (hemolysis) or decreased conjugation (decreased intrinsic metabolic
activity of the liver by acute or chronic injury). A primarily conjugated bilirubinemia results from
reflux into the plasma from impaired excretion, secondary to biliary obstruction from
cholestasis, gallstones, tumors, or strictures.
15. State the major causes of acute hepatitis.
Viruses such as hepatitis A through E viruses, Epstein-Barr virus, herpes simplex virus (HSV),
Coxsackie, and cytomegalovirus. It also can result from exposure to toxins such as ethanol,
Amanita phalloides mushrooms, carbon tetrachloride, acetaminophen, halothane, and
chlorpromazine.
16. What are the risk factors for viral hepatitis? Which can result in a carrier
state?
Hepatitis B and C are transmitted via blood and body fluid exposures: sexual intercourse,
intravenous drug abuse, blood transfusions, tattoos or body piercings, hemodialysis, and
needle sticks. Hepatitis A and E are transmitted via fecal/oral exposure (i.e., foreign travel, raw
seafood ingestion, poor hygiene or sewage management, and close contact with a person
infected with hepatitis). Hepatitis A and E are often self-limited, whereas hepatitis B and C can
result in a carrier state and progress to chronic hepatitis.
17. What is the most common form of liver disease in the United States?
Alcoholic hepatitis. It is most often diagnosed by history, but the following are highly
suggestive associated findings: spider angiomas, gynecomastia, palmar erythema, ascites,
and an elevated AST and ALT in a ratio of greater than 2:1.
18. Which patients with hepatitis should be admitted?
19. What is the initial treatment of hepatic encephalopathy? What is asterixis?
n
Hepatic encephalopathy is the accumulation of nitrogenous waste products normally
metabolized by the liver. It comprises a spectrum of clinical presentations ranging from
lethargy to coma. In addition to supportive care, lactulose, neomycin, and a low-protein
diet are the mainstays of treatment. Lactulose reduces ammonia absorption by increasing
gastrointestinal (GI) motility and by trapping ammonia as ammonium in the stool via fecal
acidification in the form of lactic acid; neomycin is an aminoglycoside that reduces the
bacteria that produces ammonia.
n
Asterixis is a clinical manifestation of moderate hepatic encephalopathy in which the hands
flap (low-amplitude alternating flexion and extension) when the arms are held straight and
the wrists are held in extension.
Chapter 35 LIVER AND BILIARY TRACT DISEASE252
20. What are complications of chronic liver disease to watch for in the ED?
The most common complication of cirrhotic ascites is spontaneous bacterial peritonitis
(SBP), which can present with any of the following: fever, abdominal pain, or mental status
changes. Paracentesis is diagnostic if it shows white blood cell count greater than 1000 cells/
mm
3
, neutrophils greater than 250 cells/mm
3
, or a positive Gram stain or culture. Portal
hypertension causes the development of esophageal varices, which can lead to massive
GI bleeding. Management should focus on resuscitation, local control (balloon tamponade or
endoscopic ligation/sclerotherapy), and reduction of portal pressure (vasopressin plus
nitroglycerin, somatostatin/octreotide, and if necessary, emergent transjugular intrahepatic
portosystemic shunt). Patients with chronic liver disease are at greatly increased risk of
bleeding because of deficits of the coagulation cascade proteins, platelet abnormalities, and
increased fibrinolysis. Renal failure in cirrhotic patients with structurally normal kidneys
represents the hepatorenal syndrome. One study showed 38% 1-year survival in patients
with the hepatorenal syndrome.
KEY POINTS: PERITONEAL FLUID CRITERIA FOR SBP
1. White blood cell count . 1000 cells/mm
3
2. Neutrophil count . 250 cells/mm
3
3. Positive Gram stain
4. Positive culture result (gold standard)
KEY POINTS: TREATMENT OF HEPATIC ENCEPHALOPATHY
1. Supportive care
2. Lactulose, 15–30 mL PO every 6–8 hours
3. Neomycin, 0.5 gm PO every 4–6 hours
4. Low-protein diet
21. Are there any special issues to watch for in the postliver-transplant patient?
Transplant rejection is common and manifests as fever, pain, and elevated transaminases and
bilirubin. This can be treated with high-dose steroids and increased immunosuppressive
medication. Other causes of transplant dysfunction include biliary strictures, recurrence of
viral hepatitis, and vascular thrombosis. Immunosuppressive therapy can cause
nephrotoxicity, neurotoxicity, and hypertension. As with other immunosuppressed patients,
opportunistic infections, such as cytomegalovirus, Epstein-Barr virus, mycobacteria, and
Pneumocystis, and fungal infection should be considered.
WEBSITES
Hepatitis B: www.hepb.org/
Hepatitis C: http://hepatitis-central.com/
Chapter 35 LIVER AND BILIARY TRACT DISEASE 253
BIBLIOGRAPHY
1. Feldman M, editor: Sleisenger and Fordtran’s gastrointestinal and liver disease, ed 7, Philadelphia, 2002, W. B.
Saunders, pp 1065–1090.
2. Gruber PJ, Silverman RA, Gottesfeld S, et al: Presence of fever and leukocytosis in acute cholecystis. Ann
Emerg Med 28:273–277, 1996.
3. Guss DA. Liver and biliary tract. In Marx J, Hockenberger R, Walls R, editors: Rosen’s emergency medicine
concepts and clinical practice, ed 5, St. Louis, 2002, Mosby, pp 1258–1260.
4. Lum DF, Leung JW: Bacterial cholangitis. Curr Treat Opt Gastroenterol 4:139–146, 2003.
5. Shah K, Wolfe R: Hepatobiliary ultrasound. Emerg Med Clin North Am 22:661–673, 2004.
6. Sheth S, Bedford A, Chopra S: Primary gallbladder cancer: recognition of risk factors and the role of
prophylactic cholecystectomy. Am J Gastroenterol 95:1402–1410, 2000.
7. Tintinalli JE, Kelen GD, Stapczynski JS: Emergency medicine, ed 6, New York, 2004, McGraw-Hill Companies,
pp 561–564.
8. Yusoff IF, Barkun JS, Barkun AN: Diagnosis and management of cholecystitis and cholangitis. Gastroenterol
Clin North Am 32:1152–1153, 2003.
255
RENAL COLIC AND SCROTAL PAIN
CHAPTER 36
Christopher M.B. Fernandes, MD
VIII. GENITOURINARY TRACT
1. What are the most common forms of renal stones?
Calcium stones account for 80% of all renal stones: Two thirds are calcium oxalate, and
the remainder are calcium phosphate. Struvite (magnesium ammonium phosphate), uric
acid, and cystine account for 20% of renal stones.
2. List factors that predispose to stone formation.
Calcium stones
n
Chronic dehydration
n
Antacid use
n
Hypercalciuria
n
Hyperoxaluria
n
Acid urine
n
Ingestion of vitamins A, C, and D
Struvite stones: chronic infection by urea-splitting organisms
Cystine stones: cystinuria
3. What lethal conditions are sometimes misdiagnosed as renal colic?
Aortic and iliac aneurysms. A careful search for bruits and pulsatile masses is
mandatory when renal colic is suspected.
4. What clinical features help distinguish renal colic from other causes of
abdominal pain?
Renal colic usually begins abruptly, causing terrible pain in the flank, costovertebral
angle, lateral abdomen, and genitals. Patients often are profoundly distressed, more so
than patients with other abdominal pathologies. Pallor, diaphoresis, restlessness, and
nausea are prominent. Renal colic causes flank tenderness, but in contrast to other
causes of lateralized abdominal pain (e.g., appendicitis, diverticulitis, cholelithiasis,
and ectopic pregnancy), it produces little or no abdominal tenderness.
5. In which patients would imaging be absolutely indicated to confirm the
diagnosis of renal colic?
n
Patients with a first episode of renal colic
n
Patients in whom the diagnosis is unclear
n
Patients in whom a proximal urinary tract infection, in addition to a calculus, is
suspected
n
Elderly patients
6. What is the role of the abdominal flat plate in diagnosing renal colic?
The abdominal flat plate, or kidneys-ureter-bladder (KUB), is less sensitive and less
specific than the clinical examination and, by itself, has no role in the work-up of
suspected renal colic. If a stone is diagnosed on ultrasound, it may be appropriate to
view the stone on a plain film. Subsequent radiographs may be helpful to document
stone progression.
Chapter 36 RENAL COLIC AND SCROTAL PAIN256
7. Has helical computed tomography (CT) supplanted the intravenous pyelogram
(IVP) as the diagnostic test of choice? Why or why not?
Helical noncontrast CT has replaced IVP as the preferred diagnostic test. The IVP pinpoints
stone size and location, clarifies the degree of obstruction, and shows ongoing renal function.
Helical CT has been shown to be 97% sensitive and 96% specific in diagnosing renal stones.
Used for this purpose, helical CT does not require intravenous contrast material and is faster
than IVP—requiring only 1 to 2 minutes of scanner time to complete a study. Even though
helical CT provides no information about renal function, this can be ascertained by a urinalysis
and serum creatinine. The marginal cost is less, and it can identify other important causes of
flank pain.
8. Is pregnancy a contraindication to IVP?
Ultrasound is the investigation of choice in pregnant patients, but if ultrasound is
nondiagnostic, a limited IVP (scout film and 20-minutes postinjection film, preferably coned to
the area of concern) is appropriate because the risk of radiation from CT KUB is greater than
the limited exposure of plain film radiography with this limited IVP.
9. What IVP findings suggest a renal stone?
Typical findings include a delayed, intense, and often prolonged nephrogram on the involved
side, delayed filling and dilation of the affected collecting system (hydroureter and
hydronephrosis), and an uninterrupted column of dye extending from the kidney to the
calculus. An unobstructed ureter, because it is peristaltic, does not normally appear opacified
with contrast in its entirety.
10. Why is the postvoid film important? What other special views are helpful?
Contrast in the bladder obscures the distal ureter. The postvoid film provides optimal
visualization of the distal ureter and the ureterovesical junction. The postvoid film also shows
whether the bladder is emptying completely. Oblique views help to confirm that a visualized
stone is in, rather than overlying, the ureter. Prone films often provide a better view of the
ureter than do standard supine films.
KEY POINTS: MOST COMMON FORMS OF RENAL STONES
1. Calcium stones (80%)
• Calcium oxalate: two thirds
• Calcium phosphate: one third
2. Struvite, uric acid, and cystine (20%)
11. What if the ureter is not visualized on the standard IVP?
In high-grade ureteral obstruction, contrast material may not reach the distal ureter for many
hours. If the ureter cannot be visualized at 1 hour, take a 2-hour film. If this fails, take a
4-hour film. The interval between films should be doubled until adequate visualization is
achieved. It is important not to abandon the IVP until contrast material reaches the calculus.
12. Name the most common sites of ureteral stone impaction.
The ureteropelvic junction, the pelvic brim (where the ureter crosses the iliac vessels), and the
ureterovesical junction (the most narrow point in the ureter).
13. Can the likelihood of spontaneous passage be predicted based on the size
and location of the stone?
Stones reaching the distal ureter are more likely to pass than those impacting proximally.
Stones 2 to 4 mm pass 95% of the time; stones 4 to 6 mm pass 50% of the time, and stones

Chapter 36 RENAL COLIC AND SCROTAL PAIN 257
greater than 6 mm pass 10% of the time. When estimating stone size, remember that the
X-ray image is magnified; the actual size is 80% of what is measured on the films.
14. What if the imaging study is normal, but the patient still appears to have renal
colic?
Re-examine the patient carefully to ensure that you have not missed another cause of
abdominal pain and that the patient is not developing a condition requiring surgery. If the
physical examination is still compatible with renal colic, treat the patient, not the test result.
Occasional false-negative results occur with all tests, and imaging modalities may miss small
stones, but this may not be clinically relevant because small stones are unlikely to require
specific therapy. Persistent severe flank pain can be caused by a leaking abdominal aortic
aneurysm (AAA).
15. Isn’t an ultrasound just as accurate as helical CT or an IVP?
Ultrasound is safe and noninvasive but is more prone to false-negative results than the other
studies. Ultrasound is sensitive for stones in the bladder and renal pelvis but often fails to
visualize those in the mid and distal ureter—the most common sites for stone impaction.
When ultrasound fails to identify a stone, however, it may show dilation of the renal collecting
system, providing evidence of ureteral obstruction.
16. List secondary signs of ureteral obstruction shown on helical CT.
n
Unilateral obstruction
n
Stranding of perinephric fat
n
Hydronephrosis
n
Nephromegaly
17. What is the soft tissue rim sign on helical CT? How is it useful?
This sign shows soft-tissue attenuation around a ureteral calculus and helps differentiate a
calculus from a phlebolith.
18. What other tests are useful in the ED in patients with renal calculi?
Urine dipsticks are sensitive for microscopic hematuria, which is present in 80% of patients
with renal colic. Urinalysis is recommended to rule out pyuria and bacteriuria. Urine culture
is indicated if symptoms, signs, or urinalysis findings suggest infection. Determination of
blood urea nitrogen (BUN), creatinine, and electrolyte levels is helpful if the patient has been
vomiting or if presence of an underlying renal disease is suspected. There is usually no need
for a more extensive metabolic work-up in the ED.
19. Why is coexistent infection a major problem?
Bacteria in an obstructed collecting system can cause abscess formation, renal destruction,
bacteremia and sepsis. The presence of infection in an obstructed ureter mandates immediate
consultation with a urologist and high-dose intravenous antibiotics.
20. Has lithotripsy supplanted percutaneous and open surgical methods of
stone removal?
Not always. Optimal therapy depends on the size, type, and location of the stone. Uretero-
scopic techniques probably are still preferable for lower ureteral stones. Extracorporeal
shock wave lithotripsy (ESWL) is optimal for stones 2 cm in size, particularly those in the
renal pelvis. Percutaneous stone removal techniques are indicated for larger stones, when
there is obstructive uropathy, and when less invasive techniques have failed. For some
stones, a combination of ESWL followed by percutaneous instrumentation is optimal.
Some large stones still require open surgery. The method of removal is best determined
by a urologist. Of note, newer technologies for treatment have led to an increased
frequency of procedural interventions, with an overall cost increase attributable to
stones compared to the pre-ESWL era.
