Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 36 RENAL COLIC AND SCROTAL PAIN258
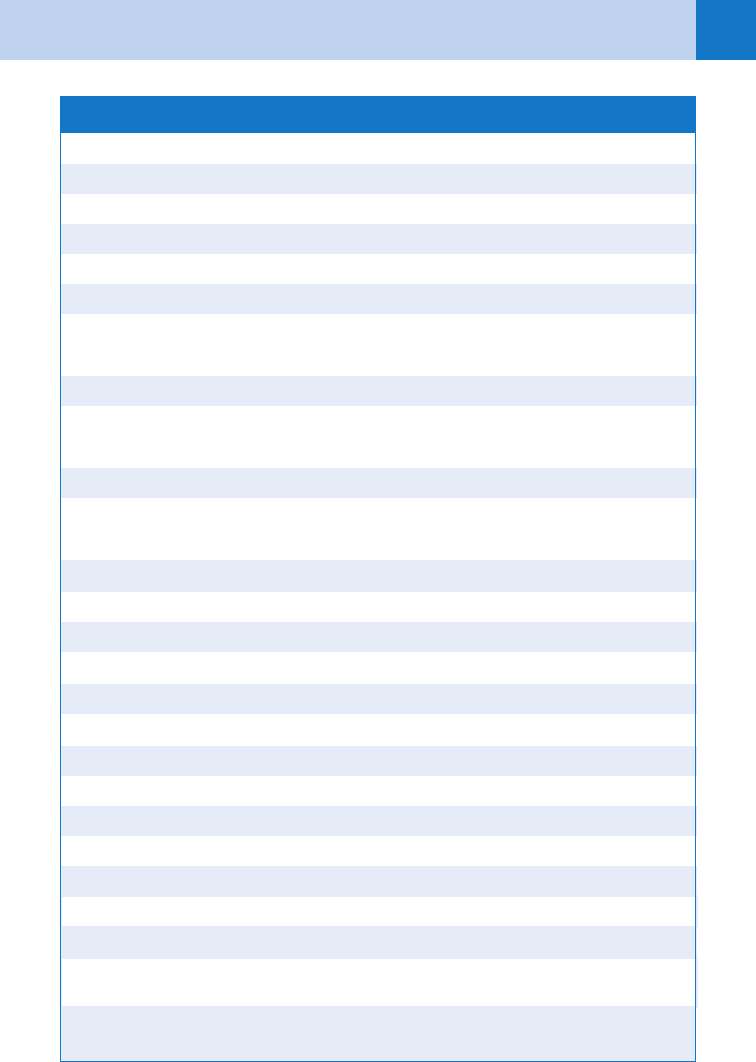
Opioid analgesics
Anileridine (Leritine) PO 50 mg q 4 h prn
Hydromorphone IV 1–2 mg q 2–4 h
IM 1–2 mg/kg q 2 h prn*
Meperidine (Demerol) IV 25–50 mg q 5–10 min prn
Morphine sulphate IV 3–5 mg q 5–10 min prn
IM 0.1–0.2 mg/kg q 3 h prn*
Oxycodone and acetaminophen
(Percocet)
PO 2 tabs q 4 h prn
Oxycodone and acetylsalicylic acid
(Percodan)
PO 2 tabs q 4 h prn
Antiemetics
Metoclopramide (Reglan) IV 10–20 mg q 15 min prn
Perphenazine (Trilafon) IM 5 mg q 6 h prn*
PO 4 mg q 6 h prn
Prochlorperazine (Compazine) IV 5–10 mg q 4 h prn
IM 5–10 mg q 6 h prn*
PO 5–10 mg q 4 h prn
Nonsteroidal analgesics
Diclofenac (Voltaren) 50- or 100-mg suppositories,
150 mg/day
Indomethacin 50- or 100-mg suppositories,
200 mg/day
Ketorolac (Toradol) IV 30 mg q 6 h
IM 30 mg q 6 h
IM, intramuscularly; IV, intravenously; PO, per os (by mouth); prn, as needed; q, every.
*Intramuscular route not recommended for ED management of acute, severe pain.
21. What are the basics of ED treatment of renal colic?
Hydration, analgesia, and antiemetics. Patients who have clinical dehydration secondary to
vomiting and decreased oral intake, as well as if radiocontrast media study is planned, should
receive intravenous fluid hydration. Various analgesics and antiemetics are available for rapid
control of symptoms (see Table 36-1). Intravenous pain control is the mainstay of ED
treatment. Analgesic treatment should not be delayed waiting for test results. Opiate
analgesics have long been the standard medication. Rectal or intravenous nonsteroidal
TABLE 36–1 ANALGESICS AND ANTIEMETICS FOR RENAL COLIC
Chapter 36 RENAL COLIC AND SCROTAL PAIN 259
anti-inflammatory drugs (NSAIDs), which inhibit renal prostaglandin synthesis, are effective
and may be given concurrently with opioids. A recent systematic review suggested that for the
management of acute renal colic, NSAIDs achieve slightly better pain relief, reduce need for
rescue analgesia, and produce much less vomiting than do opioids. Optimal ED pain control
involves the combined administration of NSAIDs and opioids (balanced analgesia).
22. Who requires hospitalization? Urology consultation?
Patients with high-grade obstruction, intractable pain or vomiting, associated urinary tract
infection, a solitary or transplanted kidney, and in whom the diagnosis is uncertain. Obtain
urologic consultation for patients with stones larger than 5 mm in diameter, urinary
extravasation, and renal insufficiency regardless of symptoms.
23. What advice should I give to patients being discharged from the ED?
Patients should be advised to drink plenty of fluids, strain their urine, and return to the ED if
they develop symptoms of infection or recurrent severe pain. Follow-up with a urologist within
a week should be recommended.
24. Which analgesics are recommended for outpatient pain control?
Gastrointestinal irritation limits the usefulness of oral NSAIDs in patients with renal colic;
however, rectal NSAIDs (diclofenac, indomethacin) may provide adequate analgesia. If
necessary, oral opioids can be combined with NSAIDs in patients with documented ureteral
calculi.
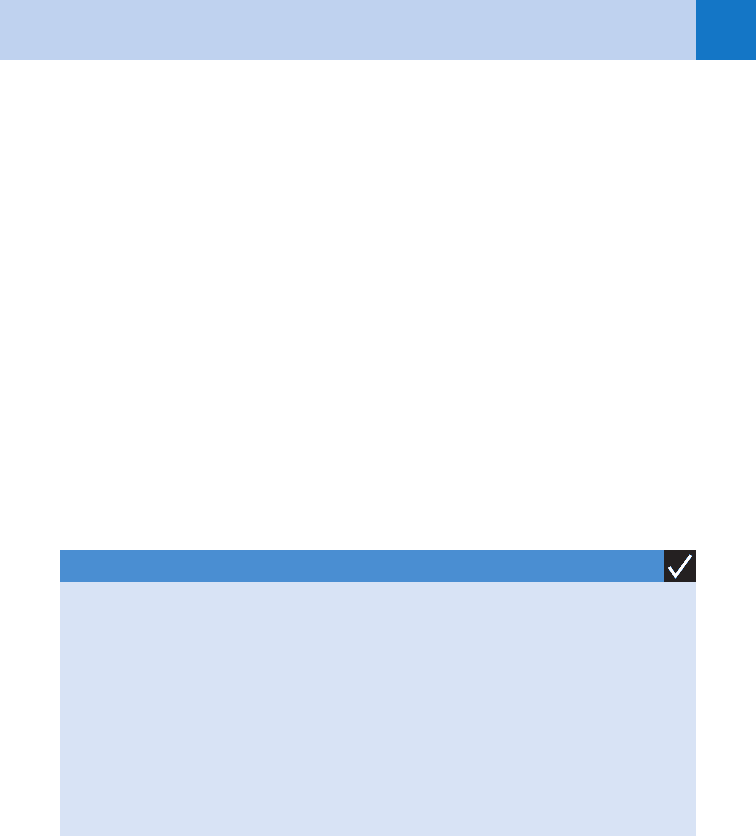
KEY POINTS: INDICATIONS FOR HOSPITALIZATION
1. Patients with high-grade obstruction
2. Intractable pain or vomiting
3. Associated urinary tract infection
4. Solitary or transplanted kidney
5. Patients in whom the diagnosis is uncertain
6. Stones larger than 5 mm in diameter
7. Urinary extravasation
8. Renal insufficiency regardless of symptoms
25. Why should patients be given a urine strainer on discharge?
If the stone can be analyzed, the patient can then receive follow-up counseling on dietary
modification or medications that may reduce the risk of recurrence.
26. When should patients return to the ED?
Patients should be instructed to seek medical care immediately if they have continued or
increasing pain, nausea and vomiting, fever or chills, or any other new symptoms.
27. What medical alternatives to active stone removal are available?
In patients with ureteral stones ,10 mm and whose symptoms are controlled with
medications, observation with periodic evaluation is an option. For such patients, appropriate
medical therapy can be offered. In such patients, calcium channel blocker or a-blocker
therapy can be used. With some data suggesting faster passage with tamsulosin, treatment
can be initiated for four weeks.
Chapter 36 RENAL COLIC AND SCROTAL PAIN260
28. What is the differential diagnosis in a patient presenting with an acutely
painful scrotum?
The differential diagnosis of acute scrotal pain includes testicular torsion, torsion of the
testicular or epididymal appendages, epididymitis, orchitis, scrotal hernia, testicular tumor,
renal colic, Henoch-Schönlein purpura, and Fournier’s gangrene. Although not life-threatening,
testicular torsion is a significant cause of morbidity and sterility in the male. Thus, any case of
an acute scrotum should be considered testicular torsion until proven otherwise.
29. What is testicular torsion?
Testicular torsion results from maldevelopment of the normal fixation that occurs between the
enveloping tunica vaginalis and the posterior scrotal wall. This maldevelopment then allows
the testis and the epididymis to hang freely in the scrotum (the so-called bell-clapper
deformity), allowing the testis to rotate on the spermatic cord. The degree of testicular
ischemia is dependent on the number of rotations of the cord.
30. When is testicular torsion most likely to occur?
The annual incidence of testicular torsion is estimated to be 1 in 400 for males younger than
the age of 25. Testicular torsion has a bimodal distribution, with peak incidence in the neonate
within the first few days of life and in preadolescence.
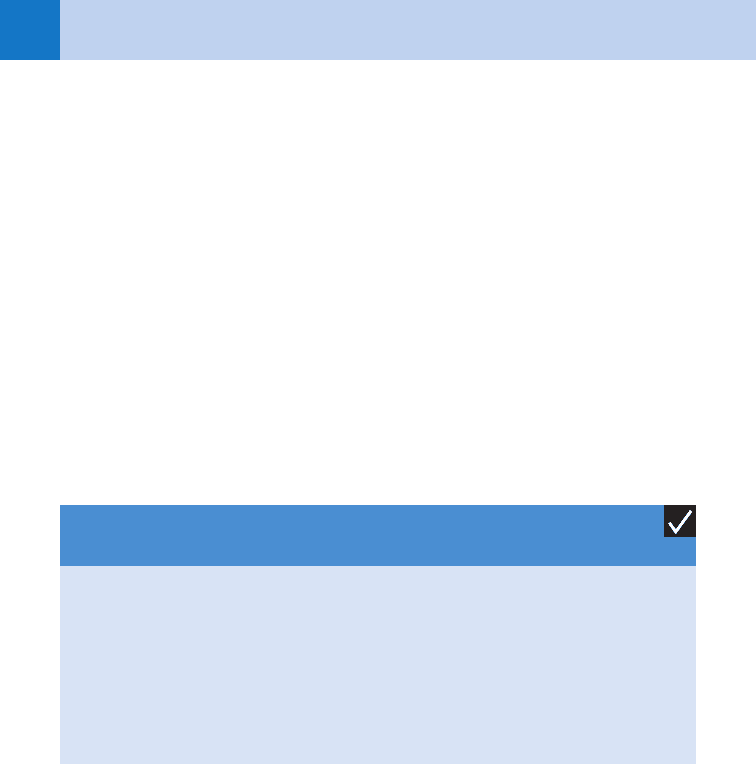
KEY POINTS: SIX DIFFERENTIAL DIAGNOSES OF ACUTE
SCROTUM
1. Testicular torsion
2. Torsion of the testicular or epididymal appendages
3. Epididymo-orchitis
4. Scrotal hernia
5. Testicular tumor
6. Fournier’s gangrene
31. What history is suggestive of testicular torsion?
Usually, there is a history of trauma or strenuous event before the onset of scrotal pain in
testicular torsion. One study reported sudden onset of scrotal pain to be present in 90% of
patients with testicular torsion, compared with 58% of patients with epididymitis and 78% of
patients with normal scrotum. Fever was present in 10% of patients with testicular torsion
compared with 32% of patients with epididymitis.
32. What clinical features are suggestive of testicular torsion?
In testicular torsion, the affected testis usually is firm, tender, and aligned in a horizontal
rather than a vertical axis. The presence of the cremasteric reflex appears to be one of the
most helpful signs in ruling out testicular torsion with 96% negative predictive value. It is
elicited by gently stroking the inner aspect of the involved thigh and observing more than
0.5 cm of elevation in the affected testis.
33. What is the proper management of testicular torsion?
The proper management of a suspected testicular torsion is immediate urologic consultation
and surgical exploration. If surgical consultation is not immediately available, manual
detorsion should be attempted.
Chapter 36 RENAL COLIC AND SCROTAL PAIN 261
34. How is manual detorsion performed?
This procedure is best done by standing at the foot or right side of the patient’s bed. The
torsed testis is detorsed in fashion similar to opening a book. The patient’s right testis is
rotated counterclockwise, and the left testis is rotated clockwise. A testis viability rate of
100%, 70%, and 20% for 6, 6–12, and 12–24 hours of symptoms, respectively, has been
reported.
35. Is imaging testing helpful to confirm the diagnosis of testicular torsion?
Testicular torsion is mainly a clinical diagnosis. If it is suspected, immediate urologic
evaluation is mandatory and should precede any further testing because time is critical.
However, imaging tests could be helpful adjuncts to the work-up of the acute scrotum when
the diagnosis is unclear.
36. What are the diagnostic imaging tests that can be used to evaluate the acute
scrotum?
Doppler ultrasound and radionucleotide scintigraphy are the two imaging tests that can be
used to evaluate the acute scrotum. Both measure the blood flow to the testis; Doppler
ultrasound carries a sensitivity of 86% and 97% accuracy, whereas radionucleotide
scintigraphy has 80% sensitivity and 97% specificity.
37. How is testicular torsion treated surgically?
The involved testis must be detorsed and then checked for viability. If it is viable, it is fixed
(orchiopexy). Because approximately 40% of patients have a bell-clapper deformity of the
contralateral testis, the unaffected testis should be fixed to prevent recurrence.
38. What are testis and epididymal appendix?
The appendix testis is a Müllerian duct remnant that is attached to the superior pole of the
testicle and rests in the groove between the testis and epididymis. The appendix epididymis is
a Wolffian duct remnant that is attached to the head of the epididymis.
39. What are clinical features of torsion of testis and epididymal appendix?
Both torsion of testis and epididymal appendix result in unilateral pain. The pain of
epididymal appendix torsion typically is more gradual in onset and is usually not quite as
severe as that associated with true testicular torsion. The most important aspect of the
physical examination is pain and tenderness localized to the involved appendix. However, late
in its course, generalized scrotal swelling and tenderness may be encountered, making it
difficult to differentiate from testicular torsion. The classic blue dot sign (visualization of the
ischemic or necrotic appendix testis through the scrotal wall on the superior aspect of the
testicle) is pathognomonic for appendix testis torsion, but it is also relatively uncommon.
40. How is torsion of testis or epididymal appendix treated?
Torsion of epididymal and testicular appendix are self-resolving, benign processes. Rest,
scrotal elevation, and analgesia are the mainstays of treatment. Resolution of the swelling and
pain should be expected within 1 week.
41. What is epididymitis?
Epididymitis arises from swelling and pain of the epididymis. It usually occurs secondary to
infection or inflammation from the urethra or bladder. Patients with epididymitis present with
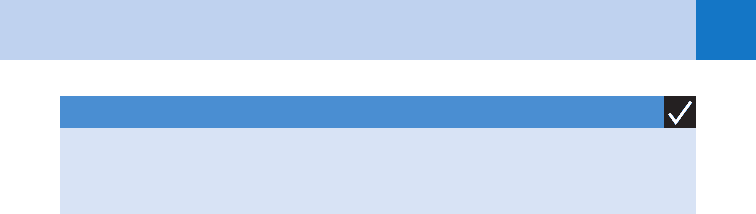
KEY POINTS: PROPER MANAGEMENT OF TESTICULAR TORSION
1. Emergent urologic consultation
2. Attempt at manual detorsion

Chapter 36 RENAL COLIC AND SCROTAL PAIN262
increasing, dull, unilateral scrotal pain during a period of hours to days. Possible associated
symptoms include fever, urethral discharge, hydrocele, erythema of the scrotum, and palpable
swelling of the epididymis. Involvement of the ipsilateral testis is common, producing
epididymitis-orchitis.
42. List the most common causes of epididymitis.
The most common causes of epididymitis in males older than 35 years are gram-negative
organisms such as Escherichia coli, Klebsiella, and Pseudomonas species. Among sexually
active men younger than 35 years, epididymitis is often caused by Chlamydia trachomatis or
Neisseria gonorrhoeae. E. coli infection also may occur in men who are insertive partners
during anal intercourse.
43. What is the treatment for epididymitis?
Admission should be considered for any febrile, toxic-appearing patient with epididymitis or
when testicular or epididymal abscess should be excluded. In-patient therapy includes bed
rest, analgesia, scrotal elevation (performed by taping a towel under the scrotum and over the
proximal anterior thighs in the supine position), NSAIDs, and parenteral antibiotics based on
presumed etiology.
When sexually transmitted disease is suspected to be the cause of epididymitis, or in males
younger than 35 years, urethral culture should be taken for Chlamydia and gonorrhea, followed
by empirical treatment with ceftriaxone 250 mg intramuscularly once, plus doxycycline 100 mg
orally twice a day for 10 days or ofloxacin 300 mg orally twice a day for 10 days. When gram-
negative bacilli are suspected to be the cause for epididymitis, or in males older than
35 years, treatment includes ciprofloxacin 500 mg orally twice a day or levofloxacin 750 mg
once a day for 10 to 14 days.
Treatment in all patients should also include bed rest, analgesia, and scrotal elevation.
Follow up with a urologist within 5 to 7 days is recommended.
44. What is Fournier’s gangrene?
Fournier’s gangrene, a surgical emergency, is a life-threatening disease characterized by
necrotizing fasciitis of the perineal and genital region. It is generally the result of a
polymicrobial infection from bacteria that are normally present in the perianal area. The
diagnosis and treatment of Fournier’s gangrene are similar to those of necrotizing fasciitis.
Diabetes mellitus, alcohol abuse, and local trauma are known risk factors. Empirical broad-
spectrum antibiotics with early aggressive surgical debridement are the mainstays of therapy.
Reexploration is commonly needed, and some patients require diverting colostomies or
orchiectomies.
BIBLIOGRAPHY
1. Dorga V, Bhatt S: Acute painful scrotum. Radiol Clin North Am 42:49–63, 2004.
2. Eray O: The efficacy of urinalysis, plain films, and spiral CT in ED patients with suspected renal colic. Am J
Emerg Med 21:152–154, 2003.
3. Holdgate A, Pollock T: Systematic review of the relative efficacy of non-steroidal anti-inflammatory drugs and
opioids in the treatment of acute renal colic. BMJ 328:1401–1406, 2004.
4. McCollough M, Sharieff G: Abdominal surgical emergencies in infants and young children. Emerg Med Clin
North Am 21:909–935, 2003.
5. Noble VE: Renal ultrasound. Emerg Med Clin North Am 22:641–659, 2004.
6. Preminger GM, Tiselius HG, Assimos DG, et al: 2007. guideline for the management of ureteral calculi. J Urol
2007; 178:2418.
7. Schneider R: Male genital problems. In Tintinalli JE, Kelen GD, Stapczynski JS, editors: Emergency medicine:
a comprehensive study guide, ed 6, New York, 2004, McGraw-Hill, pp 613–620.
8. Teichman, JMH: Acute renal colic from ureteral calculus. N Engl J Med 350:684–693, 2004.
Chapter 36 RENAL COLIC AND SCROTAL PAIN 263
9. Van Glabeke E, Khairouni A, Larroquet M, et al: Acute scrotal pain in children: results of 543 surgical
explorations. Pediatr Surg Int 15:353–357, 1999.
10. Workowski KA, Berman SM: Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep
55:1, 2006.
11. Worster A, Preyra I, Weaver B, et al: The accuracy of noncontrast helical computed tomography versus
intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med
40:280–286, 2002.
264
ACUTE URINARY RETENTION
CHAPTER 37
John P. Marshall, MD
1. What is acute urinary retention (AUR)?
A painful inability to urinate. AUR is most commonly the result of bladder outlet
obstruction, but it also may result from neurogenic, pharmacologic, or other causes of
detrusor muscle dysfunction. Urine is produced normally but is retained in the bladder,
which then becomes distended and uncomfortable.
2. Is there chronic urinary retention?
Yes. It generally represents prolonged retention. The hallmarks of chronic urinary
retention are (a) the absence of pain and (b) overflow incontinence. It most frequently
occurs in mentally debilitated or neurologically compromised patients.
3. What is the most common cause of AUR? Who gets it?
Obstruction of the lower urinary tract (bladder and urethra) is the most common
cause encountered in the ED. In general, AUR is a disease of older men, although it is
occasionally encountered in women. The usual site of obstruction is the prostate gland,
but lesions of the urethra or penis also may cause retention. Patients with indwelling
catheters (suprapubic or Foley) are at risk for episodes of retention because of
obstruction or dysfunction of these drainage systems.
4. How does benign prostatic hypertrophy (BPH) cause AUR?
BPH with bladder neck obstruction is the most common cause of AUR. Of men older
than age 60, 50% have histologic evidence of BPH. As the prostate hypertrophies, urine
outflow is obstructed by enlargement of the median lobe of the gland impinging on the
internal urethral lumen. The typical patient with BPH gives a progressive history
suggestive of urinary outlet obstruction. Symptoms such as hesitancy, diminished
stream quality, dribbling, nocturia, and the sensation of incomplete bladder emptying
may precede the episode of acute retention. New medications or increased fluid loads
may precipitate an acute episode of retention in these patients.
5. List the other causes of AUR.
n
Obstructive: BPH, prostate carcinoma, prostatitis, urethral stricture, posterior urethral
valves, phimosis, paraphimosis, balanitis, meatal stenosis, calculi, blood clots,
circumcision, urethral foreign body, constricting penile ring, and clogged or crimped
Foley catheter
n
Neurogenic: Spinal cord injuries, herniated lumbosacral disks (cauda equina
syndrome), central nervous system (CNS) tumors, stroke, diabetes, multiple
sclerosis, encephalitis, tabes dorsalis, syringomyelia, herpes simplex, herpes zoster,
and alcohol withdrawal
n
Pharmacologic: Anticholinergics, antihistamines, antidepressants, antispasmodics,
narcotics, sympathomimetics, antipsychotics, and antiparkinsonian agents (see
Question 14)
n
Psychogenic: Diagnosis of exclusion
Chapter 37 ACUTE URINARY RETENTION 265
6. What are the important features in the history and physical examination?
When taking the history, any previous prostate or urethral conditions should be elicited.
Patients often have a history of chronic voiding hesitancy, a decreased force to the urinary
stream, a feeling of incomplete bladder emptying, or nocturia. Information about neurologic
symptoms, trauma, previous instrumentation, back pain, and current medication is essential.
On physical examination, the distended bladder often is palpable above the pubic rim and
indicates at least 150 mL of urine in the bladder. The penis or vulva, and particularly the
urethra should be examined carefully for any signs of stricture, which may be evident on
palpation. A rectal examination is essential and often provides clues to the diagnosis of BPH,
prostate carcinoma, or prostatitis. A careful neurologic examination, including rectal tone and
perineal sensation, is vital in any patient suspected of having a neurologic lesion.
7. Are there any red flags in the history and physical examination that might
indicate a more serious, potentially surgical, cause?
Yes. New urinary symptoms, particularly obstruction, in patients with a history of trauma or
back pain should alert the examiner to the possibility of spinal cord compression resulting
from disk herniation, fracture, epidural hematoma, epidural abscess, or tumor. Be especially
suspicious if there is no prior history of bladder, prostate, or urethral disorders.
8. How do I treat AUR?
Catheterization and bladder decompression using a Foley catheter.
9. What if I can’t pass a Foley catheter?
Occasionally, simple passage of a 16- or 18-French Foley catheter cannot be accomplished. One
trick that often helps is to fill a 30-mL syringe with lidocaine (Xylocaine) jelly and inject it into the
urethral meatus. Still no luck? Try an 18- or 20-French coudé catheter. The coudé-tipped catheter
has a gentle upward curve in the distal 3 cm that may be helpful in pointing the catheter up and
over the enlarged prostatic lobe. Never force a catheter through an area of significant resistance
because this can cause urethral perforation, false lumens, and subsequent stricture formation.
10. Is bigger better?
A loaded question. If you are unable to pass a 16-French (standard adult) catheter, it is generally
recommended to move up in size to an 18- or 20-French Foley catheter. Usually, the stiffness and
larger bulk of the bigger catheter are more successful in passing through the bladder neck than a
smaller, more flexible catheter. Remember, never force a catheter through significant resistance.
11. What if nothing is working?
If you still cannot pass a catheter, the obstruction may be more severe than anticipated, or a
stricture may be present. One clue to the presence of a stricture in adult males is that the
obstruction occurs less than 16 cm from the external meatus of the urethra. If this is the case,
an attempt may be made using a pediatric-sized urinary catheter. If this fails, more
sophisticated instrumentation may be required, such as filiforms and followers or catheter
guides. These techniques should be done only by a urologist or practitioner with extensive
training in their use. If AUR cannot be relieved by transurethral bladder catheterization,
placement of a suprapubic catheter may be necessary.
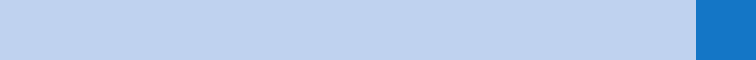
12. What is suprapubic catheterization? How is it done?
A procedure used to pass a urinary catheter directly into the bladder through the lower anterior
abdominal wall (see Fig. 37-1). It is indicated when bladder drainage is necessary and other
methods have failed or when urethral damage from trauma is suspected. The procedure is done
under sterile conditions with local anesthesia. The presence of a distended bladder is confirmed
by ultrasound or percussion. A small midline incision is made 2 cm above the symphysis pubis.
Depending on the technique, either a needle or a trocar is used to penetrate the bladder through
the incision. When urine is aspirated, a catheter is advanced over the cannula.
Chapter 37 ACUTE URINARY RETENTION266
KEY POINTS: TREATMENT OPTIONS FOR AUR
1. Foley catheter placement
2. Coudé catheter placement
3. Filiforms and followers
4. Suprapubic catheterization
13. What diagnostic studies are useful in the evaluation of AUR?
Bedside ultrasonography can be helpful during the initial evaluation, and, if needed, can
facilitate suprapubic aspiration. Always check a urinalysis with microscopic examination and
urine culture. It is generally recommended to check blood urea nitrogen and creatinine levels
to evaluate renal function, especially in cases of suspected chronic retention.
14. Which medications may cause AUR?
Table 37-1 presents the broad categories, as well as some specific medications that can
cause AUR.
Figure 37-1. Suprapubic catheterization. (From Roberts J, Hedges J: Clinical procedures in emergency
medicine, Philadelphia, 2000, W. B. Saunders.)
A B
C D
Chapter 37 ACUTE URINARY RETENTION 267
MDMA, 3,4-methylenedioxymethamphetamine.
Sympathomimetics (Alpha-Adrenergic) Antipsychotics
Ephedrine Haloperidol
Pseudoephedrine (Sudafed, Actifed) Chlorpromazine (Thorazine)
Phenylephrine hydrochloride (Neo-Synephrine) Prochlorperazine (Compazine)
Phenylpropanolamine hydrochloride (Contac) Risperidone (Risperdal)
Amphetamine Clozapine (Clozaril)
Cocaine Quetiapine (Seroquel)
Sympathomimetics (Beta-Adrenergic) Antihypertensives
Isoproterenol Nifedipine (Procardia)
Terbutaline Hydralazine
Antidepressants Nicardipine
Tricyclic Muscle Relaxants
Fluoxetine (Prozac) Diazepam (Valium)
Antidysrhythmics Cyclobenzaprine (Flexeril)
Quinidine Narcotics
Disopyramide (Norpace) Morphine sulfate
Procainamide Codeine
Anticholinergics Meperidine (Demerol)
Antihistamines Hydromorphone hydrochloride (Dilaudid)
Antiparkinsonian Agents Miscellaneous
Benztropine (Cogentin) Indomethacin
Amantadine (Symmetrel) Metoclopramide (Reglan)
Levodopa (Sinemet) Carbamazepine (Tegretol)
Trihexyphenidyl (Artane) Mercurial diuretics
Hormonal Agents Dopamine
Progesterone Vincristine
Estrogen MDMA
Testosterone Cannabis
TABLE 37–1. MEDICATIONS THAT CAN CAUSE ACUTE URINARY RETENTION
