Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

PERIODONTAL SURGERY: ACCESS THERAPY • 535
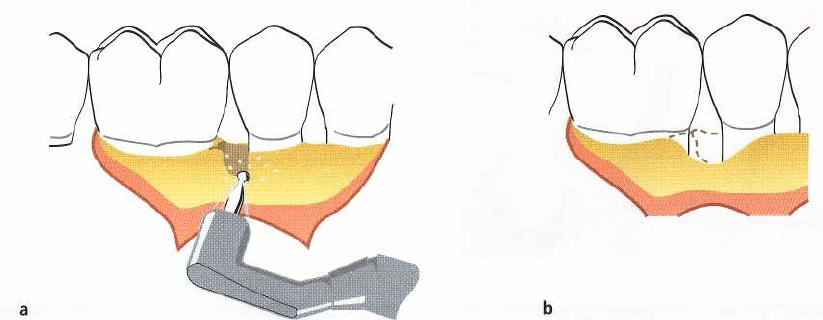
Fig. 25-41.
Ostectomy.
(a) A combined one- and two-wall osseous defect on the distal aspect of a mandibular premo
-
lar has been exposed following reflection of mucoperiosteal flaps. Since esthetics is not a critical factor to consider
in the posterior tooth region of the mandible, the bone walls are reduced to a level close to the base of the defect us
ing rotating round burs under continuous saline irrigation. (b) The osseous recontouring completed. Note that
some supporting bone has to be removed from the buccal and lingual aspect of both the second premolar and the
first molar in order to provide a hard tissue topography which allows a close adaptation of the covering soft tissue
flap.
GENERAL GUIDELINES FOR
PERIODONTAL SURGERY
Objectives of surgical treatment
Traditionally,
pocket elimination
has been a main objec
-
tive of periodontal therapy. The removal of the pocket
by surgical means served two purposes: (1) the pocket,
which established an environment conducive to pro-
gression of periodontal disease, was eliminated and
(
2) the root surface was made accessible for scaling
and, after healing, for self-performed toothcleaning.
While these objectives cannot be entirely discarded
today, the necessity for pocket elimination in peri-
odontal therapy has been challenged. During recent
years our understanding of the biology of the perio-
dontium, the pathogenesis of periodontal disease and
the healing capacity of the periodontium has mark-
edly increased. This new information has thus formed
the basis for a more differentiated understanding of
the role played by periodontal surgery in the preser-
vation of teeth.
In the past,
increased pocket depth
was the main
indication for periodontal surgery. However, pocket
depth is no longer as unequivocal a concept as it used
to be. The
probeable depth,
i.e. the distance from the
gingival margin to the point where further periodon-
tal probe penetration is stopped by tissue resistance,
may only rarely correspond to the "true" depth of the
pocket (see Chapter 18). Furthermore, regardless of
the accuracy with which pockets can be measured,
there is no established correlation between probeable
pocket depth and the presence or absence of active
disease. This means that symptoms other than in-
creased probing depth should be present to justify
surgical therapy. These include clinical signs of in-
flammation, especially exudation and bleeding on
probing (to the bottom of the pockets), as well as
aberrations of gingival morphology. Finally, the fact
that proper plaque control, maintained by the patient,
is a decisive factor for a good prognosis (Rosling et al.
1976a, Nyman et al. 1977, Axelsson & Lindhe 1981)
must be considered prior to the initiation of surgery.
In conclusion, the main objective of periodontal
surgery is to contribute to the long-term preservation
of the periodontium by facilitating plaque removal
and plaque control, and periodontal surgery can serve
this purpose by:
•
creating accessibility for proper professional scaling
and root planing
•
establishing a gingival morphology which facili-
tates the patient's self-performed plaque control.
In addition to this, periodontal surgery may aim at:
•
regeneration of periodontal attachment lost due to
destructive disease. (New attachment procedures in
periodontal therapy are discussed in Chapter 28.)
Indications for surgical treatment
Impaired access for scaling and root planing
Scaling and root planing are methods of therapy
which are difficult to master. The difficulties in accom
-
plishing proper debridement increase with (1) increas
-
ing depth of the periodontal pockets, (2) increasing

536 • CHAPTER 25
Fig.
25-42.
Evaluation following non-surgical instru-
mentation reveals persistent signs of inflammation,
bleeding following pocket probing and probing depth
6 mm. Flap elevation to expose the root surface for
proper cleaning should be considered.
Fig.
25-43.
Examples of gingival aberrations, (a) gingival enlargement and (b) proximal soft tissue crater, which fa
vor plaque retention and thereby impede the patient's plaque control.
width of the tooth surfaces,
(3)
the presence of root
fissures, root concavities, furcations, and defective
margins of dental restorations in the subgingival area.
Provided a correct technique and suitable instru-
ments are used, it is usually possible to properly de-
bride pockets up to 5 mm deep (Waerhaug
1978,
Caf-
fesse et al.
1986).
However, this
5
mm limit cannot be
used as a universal rule-of-thumb. Reduced accessi-
bility and the presence of one or several of the above-
mentioned impeding conditions may prevent proper
debridement of shallow pockets, whereas at sites with
good accessibility and favorable root morphology,
proper debridement can be accomplished even in
deeper pockets (Badersten et al.
1981,
Lindhe et al.
1982).
It is often difficult to ascertain by clinical means
whether subgingival instrumentation has been prop-
erly performed. Following scaling, the root surface
should be smooth – roughness will often indicate the
presence of remaining subgingival calculus. It is also
important to monitor carefully the gingival reaction to
subgingival debridement. If inflammation persists
and
if bleeding is elicited by gentle probing in the
subgingival area, the presence of subgingival deposits
should be suspected (Fig.
25-42).
If such symptoms are
not resolved by repeated subgingival instrumenta-
tion, surgical treatment should be performed to ex-
pose the root surfaces for proper cleaning.
Impaired
access for self-performed
plaque control
The level of plaque control which can be maintained
by the patient is determined not only by his/her inter
-
est and dexterity but also, to some extent, by the
morphology of the dentogingival area.
The patient's responsibility in a plaque control pro-
gram must obviously include the cleansing of the
supragingival tooth surfaces and the marginal part of
the gingival sulcus. This means that the tooth area
coronal to the gingival margin and at the entrance to
the gingival sulcus should be the target for the pa-
tient's home care efforts.
Pronounced gingival hyperplasia and gingival cra-
ters (Fig.
25-43) are examples of morphologic aberra-
tions which may impede proper home care. Likewise,
the presence of restorations with defective marginal
fit
or adverse contour and surface characteristics at the
gingival margin may seriously compromise plaque
removal.
By the professional treatment of periodontal dis-
ease, the dentist prepares the dentition in such a way
that home care can be effectively managed. At the
completion of treatment, the following objectives
should have been met:
•
no sub or supragingival dental deposits
•
no pathologic pockets (no bleeding on probing to
the bottom of the pockets)
PERIODONTAL SURGERY: ACCESS THERAPY • 537
•
no plaque-retaining aberrations of gingival mor-
phology
•
no plaque-retaining parts of restorations in
relation
to the gingival margin
These requirements lead to the following indications
for periodontal surgery:
•
accessibility for proper scaling and root planing
•
establishment of a morphology of the dento-gingi-
val area conducive to plaque control
•
pocket depth reduction
•
correction of gross gingival aberrations
•
shift of the gingival margin to a position apical to
plaque-retaining restorations
•
facilitate proper restorative therapy
Contraindications for periodontal surgery
Patient cooperation
Since optimal postoperative plaque control is decisive
for the success of periodontal treatment (Axelsson &
Lindhe 1981), a patient who fails to cooperate during
the cause-related phase of therapy should not be ex-
posed to surgical treatment.
Even though short-term postoperative plaque con
-
trol entails frequent professional treatments, the long
-
term responsibility for maintaining good oral hygiene
must rest with the patient. Theoretically, even the
poorest oral hygiene performance by a patient may be
compensated for by frequent recall visits for suppor-
tive therapy (e.g. once a week), but it is unrealistic to
consider larger groups of patients being maintained
in this manner. A typical recall schedule for periodon
-
tal patients involves professional consultations for
supportive periodontal therapy once every 3-6
months. Patients who cannot maintain satisfactory
oral hygiene over such a period should normally be
considered unsuited for periodontal surgery.
Cardiovascular disease
Arterial hypertension
does not normally preclude peri-
odontal surgery. The patient's medical history should
be checked for previous untoward reactions to local
anesthesia. Local anesthetics free from or low in ad-
renaline may be used and an aspirating syringe
should be adopted to safeguard against intravascular
injection.
Angina pectoris
does not normally preclude periodon-
tal surgery. The drugs used and the number of epi-
sodes of angina may indicate the severity of the dis-
ease. Premedication with sedatives and the use of local
anesthesia low in adrenaline are often recommended.
Safeguards should be adopted against intravascular
injection.
Myocardial infarction patients
should not be subjected
to periodontal surgery within 6 months following
hospitalization, and thereafter only in cooperation
with the physician responsible for the patient.
Anticoagulant treatment
implies increased propensity for
bleeding. Periodontal surgery should be sched
uled
first after consultation with the patient's physi
cian to
determine whether modification of the antico
agulant
therapy is indicated. In patients on moderate
levels
of anticoagulation and only requiring minor
surgical
treatment no alteration of their anticoagulant
therapy
may be required. To keep the prothrombin
time
within a safety level for hemorrhage control dur
ing
surgery in patients with higher levels of antico-
agulation, adjustments of the anticoagulant drug ther
-
apy usually need to be initiated 2-3 days prior to the
dental appointment. Anticoagulation may be safely
resumed immediately after the periodontal surgical
procedure since several days are needed for full anti-
coagulation to return. Aspirin and other non-steroidal
anti-inflammatory drugs should not be used for post-
operative pain control since they increase bleeding
tendency. Furthermore, tetracyclines are contraindi-
cated in patients on anticoagulant drugs due to inter-
ference with prothrombin formation (Fay & O'Neil
1984).
Rheumatic endocarditis, congenital heart lesions and
heart/vascular implants
involve risk for transmission of
bacteria to heart tissues and heart implants during the
transient bacteremia that follows manipulation of in-
fected periodontal pockets. Surgical treatment (in-
cluding tooth extractions) of patients with these con-
ditions, as well as of patients at risk of hematogenous
prosthetic joint infection (for the first 2 years following
joint placement) (American Dental Association and
American Academy of Orthopedic Surgeons 1997),
should be preceded by antiseptic mouthrinsing (0.2 %
chlorhexidine) and prescription and administration of
an appropriate antibiotic in a high dose. According to
the recommendations by the American Heart Associa
-
tion (Dajani et al. 1997), 2 g of amoxicillin adminis-
tered 1 hour before the treatment is an adequate regi-
men. In case the patient is allergic to penicillin, clin-
damycin (600 mg) is recommended as an alternative.
No second doses are recommended for any of the
above dosing regimens. Tetracyclines and erythromy-
cin are not recommended for prophylactic cardiovas-
cular antibiotic coverage.
Organ
transplantation
In organ transplantation, medications are used to pre
-
vent transplant rejection. The drug of choice today is
cyclosporin A, a potent immunosuppressant drug.
The adverse effects seen following cyclosporin A treat-
ment include an increased risk for gingival enlarge-
ment as well as hypertension. In addition, hyperten-
sion seen in renal transplant recipients is often treated
with calcium channel blockers. These antihyperten-
sive agents have also been associated with gingival
enlargement. As in patients on phenytoin therapy,
53
8
• CHAPTER 25
gingival enlargement in patients on cyclosporin A
therapy or on antihypertensive therapy with calcium
blockers may be corrected by means of periodontal
surgery. However, due to the strong propensity for
recurrence, the use of intensified conservative peri-
odontal therapy to prevent gingival enlargement in
susceptible patients should be encouraged.
Prophylactic antibiotics are recommended in trans
-
plant patients taking immunosuppressive drugs, and
the patient's physician should be consulted before any
periodontal therapy is performed. In addition, anti-
septic mouthrinsing (0.2% chlorhexidine) should pre
-
cede the surgical treatment.
Blood disorders
If the medical history includes blood disorders, the
exact nature of these should be ascertained.
Patients suffering from
acute leukemias, agranulocy-
tosis
and
lymphogranulomatosis
must
not
be subjected
to periodontal surgery.
Anemias
in mild and compensated forms do not
preclude surgical treatment. More severe and less
compensated forms may entail lowered resistance to
infection and increased propensity for bleeding. In
such cases, periodontal surgery should only be per-
formed after consultation with the patient's physician.
Hormonal disorders
Diabetes mellitus
entails lowered resistance to infec-
tion, propensity for delayed wound healing and pre-
disposition for arteriosclerosis. Well compensated pa
-
tients may be subjected to periodontal surgery pro-
vided precautions are taken not to disturb dietary and
insulin routines.
Adrenal function
may be impeded in patients receiving
large doses of corticosteroids over an extended period.
These conditions involve reduced resistance to physi
-
cal and mental stress, and the doses of corticosteroid
may have to be altered during the period of periodon
-
tal surgery. The patient's physician should be con-
sulted.
Neurologic disorders
Multiple sclerosis and Parkinson's disease
may in severe
cases make ambulatory periodontal surgery impossi-
ble. Paresis, impaired muscular function, tremor, and
uncontrollable reflexes may necessitate treatment un
-
der general anesthesia.
Epilepsy is
often treated with
phenytoin
which, in ap-
proximately 50%) of cases, may mediate the formation
of gingival enlargement. These patients may, without
special restrictions, be subjected to periodontal sur-
gery for correction of the enlargement. There is, how-
ever, a strong propensity for recurrence of the enlarge
ment, which in many cases can be countered by
inten
sifying the plaque control.
Smoking
Although smoking negatively affects wound healing
(
Siana et al. 1989), it may not be considered a contra-
indication for surgical periodontal treatment. The cli-
nician should be aware, however, that less resolution
of probing pocket depth and smaller improvement in
clinical attachment may be observed in smokers than
in non-smokers (Preben & Bergstrom 1990, Ah et al.
1994, Scabbia et al. 2001).
Local anesthesia in periodontal surgery
Traditional views of pain and discomfort as an inevi-
table consequence of dental procedures, in particular
surgical procedures (including scaling and root plan-
ing) and extractions, are no longer accepted by pa-
tients. Pain management is an ethical obligation and
will improve patient satisfaction in general (e.g. in-
creased confidence and improved cooperation) as
well
as patient recovery and short-term functioning
after
oral/periodontal surgical procedures.
In order to prevent pain during the performance of
a periodontal surgical procedure, the entire area of the
dentition scheduled for surgery, the teeth as well as the
periodontal tissues, requires proper local anesthesia.
Mechanism of action
Local anesthesia is defined as a loss of feeling or
sensation that is confined to a certain area of the body.
All local anesthetics have a common mechanism of
action. To produce their effect they block the genera-
tion and propagation of impulses along nerve fibers.
Such impulses are transmitted by the rapid depolari-
zation and repolarization within the nerve axons.
These changes in polarity are due to the passage of
sodium and potassium ions across the nerve mem-
brane through ionic channels within the membrane.
Local anesthetics prevent the inward movement of
sodium ions which initiate depolarization and as a
consequence the nerve fiber cannot propagate any
impulse. The potassium efflux, on the other hand, is
influenced very little and there is no change in the
resting potential. The mechanisms behind the activity
of the local anesthetics are not fully understood, but
the most plausible theory is that the lipid-soluble free
base form of the local anesthetic, which is the form that
penetrates biologic membranes most easily, pene-
trates the connective tissue to reach the axons and
diffuses across the lipid membrane into the axon.
Inside the axon the drug interacts with specific recep-
tor sites on or within the sodium channels to exert an
inhibitory effect on sodium influx and, consequently,
on impulse conduction.
Dental local anesthetics
Anesthetics from the chemical group amino-amides,
for example lidocaine, mepivacaine, prilocaine and
articaine, are more potent and significantly less aller-
genic than amino-esters (e.g. procaine and tetracaine)
PERIODONTAL SURGERY: ACCESS THERAPY • 539
and have therefore replaced esters as the "gold stan-
dard" for dental local anesthetics.
Due to the specific need for bone penetration, den-
tal local anesthetics contain high concentrations of the
active agent. Although most amide local anesthetics
may cause local vasoconstriction in low concentra-
tions, the clinically used concentrations in dental so-
lutions will cause an increase in the local blood flow.
Significant clinical effects of this induced vasodilation
are an increased rate of absorption, thus decreasing
the duration of anesthesia. Major benefits can there-
fore be obtained by adding relatively high concentra-
tions of vasoconstrictors (e.g. epinephrine > 1:200 000
or > 5 mg/ml) to dental local anesthetic solutions; the
duration is considerably prolonged, the depth of an-
esthesia may be enhanced and the peak concentra-
tions of the local anesthetic in blood can be reduced.
Furthermore, in periodontal surgery, incorporation of
adrenergic vasoconstrictors into the local anesthetic is
of considerable value in keeping bleeding to a mini-
mum during surgery (avoiding considerable blood
loss, making it possible to visualize the surgical site
and thus with intact surgical quality shorten the time
spent on the procedure). As a matter of fact, the use of
a dental local anesthetic without a vasoconstrictor
during a periodontal surgical procedure is counter-
productive because the vasodilating properties of
such a local anesthetic will increase the bleeding in the
area of surgery.
Vasoconstrictors and local
hemostasis
Epinephrine is the vasoconstrictor of choice for local
hemostasis and is most commonly used in a concen-
tration of 1:80 000 (12.5 mg/ml). However, 1:100 000
epinephrine also provides excellent hemostasis and
most periodontists are unable to detect a clinical dif-
ference between the two concentrations. It therefore
seems prudent to use the least concentrated form of
epinephrine that provides clinically effective hemo-
stasis (i.e. the 1:100 000 concentration).
Although the cardiovascular effects of the usually
small amounts of epinephrine used during a peri-
odontal surgical procedure are of little practical con-
cern in most individuals, accidental intravascular in-
jections, unusual patient sensitivity and unantici-
pated drug interactions (or excessive doses) can result
in potentially serious outcomes. It must also be under
-
stood that the use of epinephrine for hemostasis dur-
ing periodontal surgery has some potential draw-
backs. Epinephrine will produce a rebound vasodila-
tion after the vasoconstriction has worn off, leading to
increased risk for bleeding in the immediate postop-
erative period. There is a greater potential for such
undesirable delayed hemorrhage following the use of
1:80.000 epinephrine than after the use 1:100 000.
Postoperative pain may increase and wound heal-
ing may be delayed when adrenergic vasoconstrictors
are used because of local ischemia with subsequent
tissue acidosis and accumulation of inflammatory me
-
diators. Furthermore, the possibility of an ischemic
necrosis of surgical flaps infiltrated with an adrenergic
vasoconstrictor (especially if norepinephrine is used
instead of epinephrine) cannot be discounted. For
these reasons as well as because of the possibility of
systemic reactions alluded to above, dental local an-
esthetics containing adrenergic vasoconstrictors for
hemostasis should be infiltrated
only
as needed and
not
merely from habit.
Felypressin, another commonly used vasoconstric-
tor, appears to act preferentially on the venous side of
the microcirculation and is not very active in constrict
-
ing the arteriolar circulation. Felypressin is therefore
not nearly as effective as adrenergic vasoconstrictors
in limiting hemorrhage during a surgical procedure.
Individual variability in response to dental local
anesthetics
Although it is possible for the periodontist to choose
from a broad spectrum of dental local anesthetics to
achieve the expected clinical action, there are a num-
ber of other factors (i.e. not related to the drug) that
can affect the drug action in a single patient.
During clinical conditions the variability in re-
sponse to dental local anesthetics administered can be
expected to be great, for example with regard to depth
and duration of anesthesia. The reason for the great
variation has not been adequately explained but has
to be accepted as it may have significant implications
in periodontal surgical procedures. A list of possible
factors that may cause anesthetic failures include:
•
Accuracy in administration of the drug
•
Anatomic variation between patients (e.g. in elderly
patients with bone resorption)
•
Status of the tissues at the site of injection (
vascular
ity, inflammation)
•
General condition of patient
•
Psychologic factors
Inaccuracy in administration is a major factor causing
anesthetic failures. Although not particularly signifi-
cant in infiltration anesthesia, the mandibular block is
a prime example of a technique in which duration of
anesthesia is greatly influenced by accuracy of injec-
tion.
The general condition of the patient as well as
psychologic factors may also affect the anticipated
duration of action. Infection, stress or pain will usually
lead to decreased duration of anesthesia, while an
increase in the patient's own defense mechanisms
against pain perception by, for example, release of
endogenous endorphins, may provide improved
depth and/or duration of anesthesia.
Techniques for anesthesia in periodontal surgery
Injections of dental local anesthetics prior to a peri-
odontal surgical procedure may be routine for the
dentist, but are often a most unpleasant experience for
the patient. Reassurance and psychologic support are
essential and will increase the patient's confidence in
540 • CHAPTER 25
his dentist. To create a relaxed atmosphere and to
decrease the patient's fear of an unusual situation is
of course also a useful way of increasing the patient's
own defense mechanisms against pain perception
(e.
g. release of endogenous endorphins).
Anesthesia for periodontal surgery is obtained by
nerve block and/or by local infiltration. In cases of
flap surgery, complete anesthesia must be attained
before commencing the operation, as it may be diffi-
cult to supplement the anesthesia after the bone sur-
face has been exposed. In addition, the pain elicited
by needle insertion can be significantly reduced if the
mucosa at the puncture site is anesthetized in advance
by the use of a suitable topical ointment or spray.
Local infiltration may have a greatly decreased rate
of success in areas where inflammation, in spite of
optimal conservative periodontal therapy and good
oral hygiene, remains in the periodontal tissues. The
suggested reason for this is that tissue pH tends to be
low in inflamed areas and anesthetic solutions are less
potent at low pH because there is a greater proportion
of charged cation molecules than of the uncharged
base molecules. Because of this, diffusion of the local
anesthetic into the axoplasm is slower, with sub-
sequent delayed onset and decreased efficacy. An-
other more recent hypothesis suggests that NGF
(
Nerve Growth Factor) released during tissue inflam-
mation will induce sprouting or proliferation of sen-
sory nerve endings, expressing a different (sub-)type
of sodium channel than in normal tissues. The dental
local anesthetics used at present may not be selective
enough for proper interaction with these sodium
channel subtypes to induce anticipated anesthesia.
Local anesthesia in the mandible
As a rule, analgesia of the teeth and the soft and hard
tissues of the mandible should be obtained by a
mandibular block and/or a mental block. In the ante
-
rior region of the mandible, canines and incisors can
often be anesthetized by infiltration, but there are
often anastomoses over the midline. These anasto-
moses must be anesthetized by bilateral infiltration,
or by bilateral mental blocks. The buccal soft tissues
of the mandible are anesthetized by local infiltration
or by blocking the buccal nerve. Local infiltration,
performed as a series of injections in the buccal fold of
the treatment area, has of course the added advantage
of providing a local ischemic effect if a suitable anes-
thetic is used.
The lingual periodontal tissues must also be anes-
thetized. This is accomplished by blocking the lingual
nerve and/or by infiltration in the floor of the mouth
close to the site of operation. If necessary to obtain
proper ischemia, and only then, supplementary injec-
tions may be made in the interdental papillae (in-
traseptal injections).
Local anesthesia in the maxilla
Local anesthesia of the teeth and buccal periodontal
tissues of the maxilla can easily be obtained by injec-
tions in the mucogingival fold of the treatment area. If
larger areas of the maxillary dentition are scheduled
for surgery, repeated injections (in the mucogingival
fold) have to be performed, e.g. at the central incisor,
canine, second premolar and second molar. In the
posterior maxillary region a tuberosity injection can
be used to block the superior alveolar branches of the
maxillary nerve. However, because of the vicinity to
the pterygoid venous plexus, this type of block anes-
thesia is not recommended due to the risk of intrave-
nous injection and/or hematoma formation.
The palatal nerves are most easily anesthetized by
injections made at right angles to the mucosa and
placed around 10 mm apical to the gingival margin
adjacent to teeth included in the operation. In cases of
advanced bone loss, the pain produced by injecting
into the non-resilient palatal mucosa can be mini-
mized if the injections are performed from the buccal
aspect, i.e. through the interdental gingiva. Sometimes
blocks of the nasopalatine nerves and/or the greater
palatine nerves can be applied. Especially for peri-
odontal surgery involving molars, supplementary
blocking of the greater palatine nerve should be con-
sidered.
Instruments used in periodontal surgery
General considerations
Surgical procedures used in periodontal therapy often
involve the following measures (instruments):
•
Incision and excision (periodontal knives)
•
Deflection and readaptation of mucosal flaps (pe-
riosteal elevators)
•
Removal of adherent fibrous and granulomatous
tissue (soft tissue rongeurs and tissue scissors)
•
Scaling and root planing (scalers and curettes)
•
Removal of bone tissue (bone rongeurs, chisels and
files)
•
Root sectioning (burs)
•
Suturing (sutures and needle holders, suture scis-
sors)
•
Application of wound dressing (plastic instru
ments)
The set of instruments used for the various periodon-
tal surgical procedures should have a comparatively
simple design. As a general rule, the number and
varieties of instruments should be kept to a minimum.
In addition to particular instruments used for peri-
odontal treatment modalities, equipment and instru-
ments generally used in oral surgery are often needed.
Within each category of surgical instruments used
for periodontal therapy there are usually several
PERIODONTAL SURGERY: ACCESS THERAPY • 541
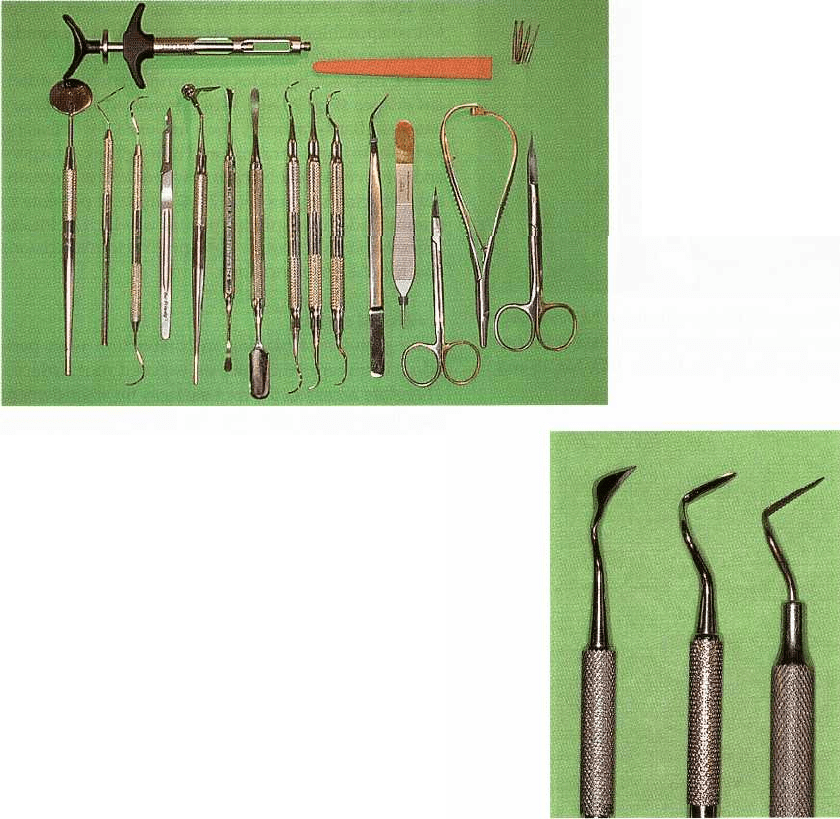
Fig. 25-44. Set of instruments used
for periodontal surgery and in-
cluded in a standard tray.
brands available, varying in form and quality, leaving
ample room for individual preferences.
The instruments should be stored in sterile "ready
-
to-use" packs or trays. Handling, storing and labeling
of surgical instruments and equipment must be man
-
aged in such a way that interchanging of sterile and
non-sterile items is prevented.
It is also important that the instruments are kept in
good working condition. The maintenance routine
should ensure that scalers, curettes, knives with fixed
blades, etc., are sharp and that the hinges of scissors,
rongeurs and needle holders are properly lubricated.
Spare instruments (sterile) should always be available
to replace instruments found to be defective or acci-
dentally contaminated.
The instrument tray
Instrument trays for periodontal surgery may be ar-
ranged in several ways. Different trays can be used for
different procedures or a standard tray can be used for
all procedures supplemented with the particular in-
struments that are needed for a specific procedure.
A commonly used standard tray combines the basic
set of instruments used in oral surgery and a few
periodontal instruments. The instruments listed be-
low are often found on such a standard tray (Fig.
25-
44):
•
Mouth mirrors
•
Graduated periodontal probe/Explorer
•
Handles for disposable surgical blades (e.g. Bard-
Parker handle)
•
Mucoperiosteal elevator and tissue retractor
•
Scalers and curettes
•
Cotton pliers
•
Tissue pliers
(ad modum
Ewald)
•
Tissue scissors
•
Needle holder
•
Suture scissors
•
Plastic instrument
•
Hemostat
•
Burs
Fig. 25-45. Examples of gingivectomy knifes with fixed
blades. From left to right: Kirkland
15
/16,
Orban
1
/2,
and
Waerhaug
1
/2.
Additional equipment may include:
•
Syringe for local anesthesia
•
Syringe for irrigation
•
Aspirator tip
•
Physiologic saline
•
Drapings for the patient
•
Surgical gloves, surgical mask, surgeon's hood
Surgical instruments
Knives
Knives are available with fixed or replaceable blades.
The advantage of the fixed blade versions is that the
blade can be given any desired shape and orientation
in relation to the handle. A disadvantage is that such
instruments need frequent resharpening. Fig. 25-45
shows examples of knives with fixed blades.
New disposable blades are always sharp. They can
be rapidly replaced if found defective. The cutting
edge of the blades normally follows the long axis of
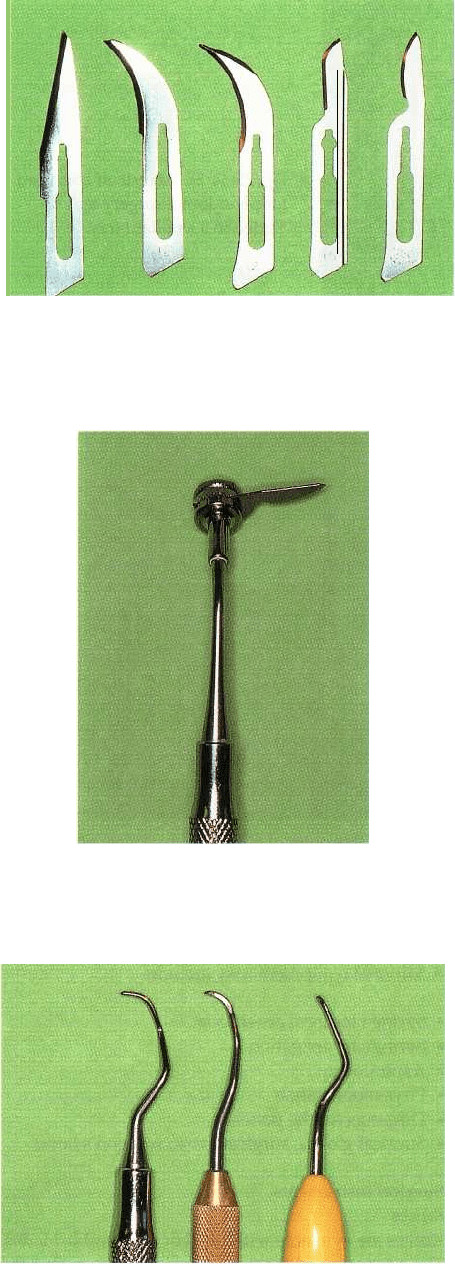
542 • CHAPTER 25
Fig. 25-46. Disposable blades which can be mounted in
various types of handles. The shape of the blades are
from left to right: No. 11, No. 12, No. 12D, No. 15 and
No. 15C.
Fig. 25-47. A universal360° handle for disposable
blades, which allows the mounting of the blade in any
angulated position of choice.
Fig. 25-48. Examples of double-ended sickle scalers and
curettes useful for root debridement in conjunction
with periodontal surgery. From left to right: Curette SG
215/16C Syntette, Sickle 215-216 Syntette and mini-cu
rette SG 215 / 16MC.
the handle, which limits their use. However, knives
with disposable blades fitted at an angle to the handle
are also available.
The disposable blades are manufactured in differ-
ent shapes (Fig. 25-46). When mounted in ordinary
handles (Bard-Parker
®
), they are used for releasing
incisions in flap operations and mucogingival surgery
and for reverse bevel incisions where access is obtain-
able. Special handles (Fig. 25-47) make it possible to
mount blades in angulated positions, which facilitates
the use of such knives for both gingivectomy excisions
and reverse bevel incisions.
Scalers and curettes
Scaling and root planing in conjunction with peri-
odontal surgery take place on exposed root surfaces.
Therefore access to the root surfaces for debridement
may be obtained also with the use of comparatively
sturdy instruments (Fig. 25-48). Tungsten carbide cu-
rettes and scalers with durable cutting edges are often
used when "access" is not a problem. Rotating fine-
grained diamond stones (Fig. 25-49) may be used
within infrabony pockets, root concavities and en-
trances to furcations.
Instruments for bone removal
Sharp bone chisels or bone rongeurs (Fig. 25-50) cause
the least tissue damage and should be employed
whenever access permits. With reduced access, surgi-
cal burs or files may be used. The burs should operate
at low speed and ample rinsing with sterile physi-
ologic saline should ensure cooling and removal of
tissue remnants.
Instruments for handling flaps
The proper healing of the periodontal wound is criti-
cal for the success of the operation. It is therefore
important that the manipulations of the soft tissue
flaps are performed with the minimum of tissue dam-
age. Care should be exercised in the use of periosteal
elevators when flaps are deflected and retracted for
optimal visibility. Surgical pliers and tissue retractors
which pierce the tissues should not be used in the
marginal area of the flaps. Needle holders with small
beaks and atraumatic sutures should be used.
Additional equipment
Hemorrhage is rarely a problem in periodontal sur-
gery. The characteristic oozing type of bleeding can
normally be controlled by a pressure pack (sterile
gauze moistened with saline). Bleeding from small
vessels can be stopped by clamping and tying using a
hemostat and resorbable sutures. If the vessel is sur-
rounded by bone, bleeding may be stopped by crush-
ing the nutrient canal in which the vessel runs with a
blunt instrument.
Sterile physiologic saline is used for rinsing and
moistening the field of operation and for cooling when
burs are employed. The saline solution may be kept in
a sterile metal cup on the instrument tray and may be
PERIODONTAL SURGERY: ACCESS THERAPY • 543
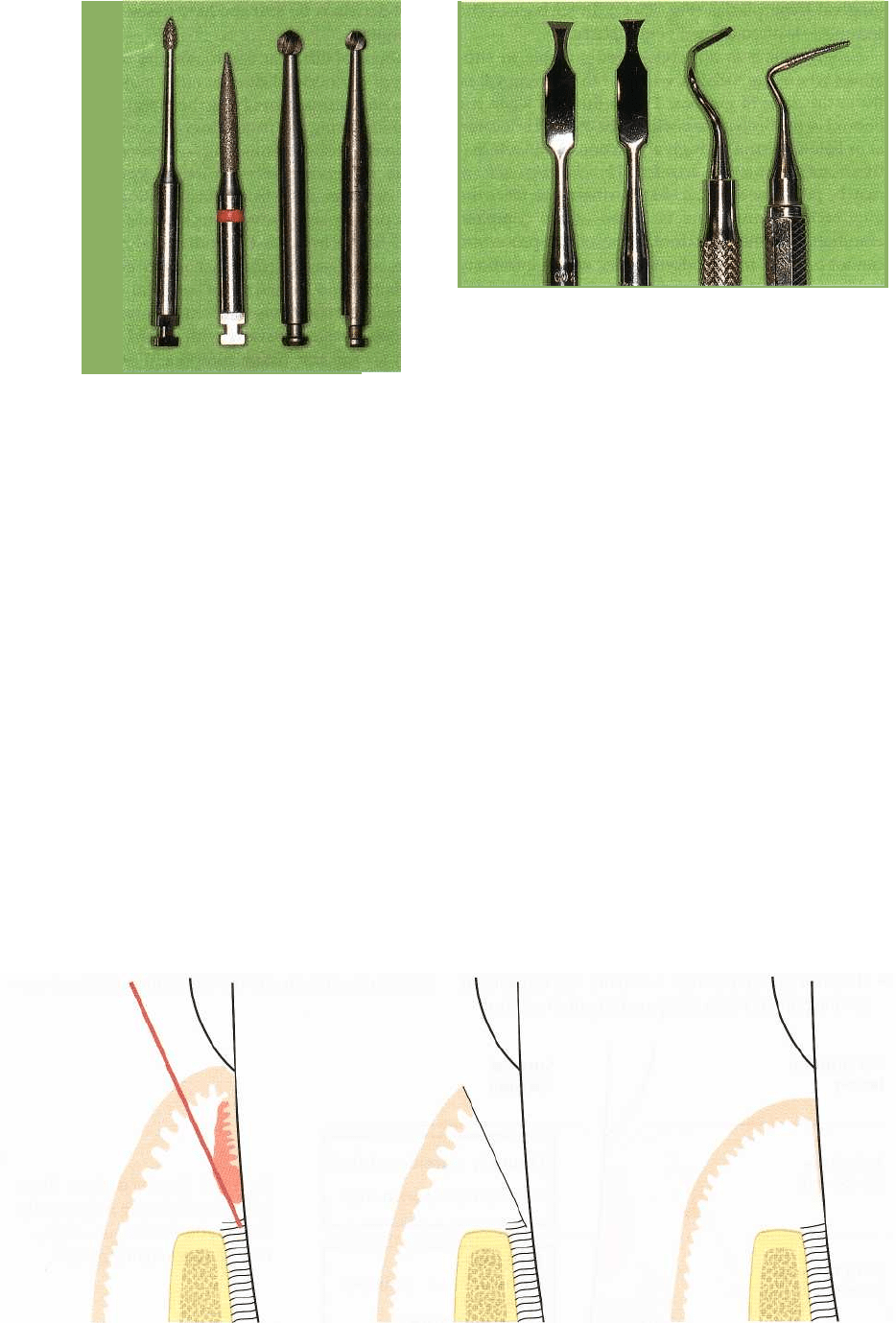
Fig.
25-49. A
set of burs which may be useful in peri
-
odontal surgery. The rotating fine-grained diamond
stones may be used for debridement of infrabony de
fects. The round burs are used for bone
recontouring.
applied to the wound by means of a sterile disposable
plastic syringe and a needle with rounded tip.
Visibility in the field of operation is secured by
using effective suction. The lumen of the aspirator tip
should have a smaller diameter than the rest of the
tube, in order to prevent clogging.
The patient's head may be covered by autoclaved
cotton drapings or sterile disposable plastic /paper
drapings. The surgeon and all assistants should wear
sterile surgical gloves, surgical mask and surgeon's
hood.
Selection of surgical technique
Many of the technical problems experienced in peri-
odontal surgery stem from the difficulties in assessing
accurately the degree and type of breakdown that has
occurred prior to surgery. Furthermore, at the time of
Fig.
25-50. Examples of instruments used for bone re
-
contouring. From left to right: Bone chisels Ochsenbein
no. 1 and
2
(Kirkland 13K/13KL), Bone chisel Ochsen
-
bein no. 3 and Schluger curved file no.
9/10.
surgery, previously undiagnosed defects may be rec-
ognized or some defects may have a more complex
outline than initially anticipated. Since each of the
surgical procedures described above is designed to
deal with a specific situation or to meet a certain
objective, it must be understood that in most patients
no single standardized technique alone can be applied
when periodontal surgery is undertaken. Therefore,
in each surgical field, different techniques are often
used and combined in such a way that the overall
objectives of the surgical part of the periodontal ther-
apy are met. As a general rule, surgical modalities of
therapy which preserve or induce the formation of
periodontal tissue should be preferred over those
which resect or eliminate tissue.
General indications for various surgical techniques
Gingivectomy
The obvious indication for gingivectomy is the pres-
ence of deep supra-alveolar pockets. In addition, the
gingivectomy technique can be used to reshape abnor
-
mal gingival contours such as gingival craters and
Fig.
25-51.
Internal beveled gingivectomy.
Schematic illustration of the incision technique in case of the presence of
only a minimal zone of gingiva.
544 • CHAPTER 25
gingival hyperplasias (Fig. 25-43). In such cases the
technique is often termed
gingivoplasty.
Gingivectomy is not considered suitable in situ-
ations where the incision will lead to the removal of
the entire zone of gingiva. This is the case when the
bottom of the probeable pocket to be excised is located
at or below the mucogingival junction. As an alterna-
tive in such a situation, an
internal beveled gingivectomy
may be performed (Fig. 25-51). Furthermore, since the
gingivectomy procedure is aimed at the complete
elimination of the periodontal pocket, the procedure
cannot be used in periodontal sites where infrabony
lesions or bony craters are present.
These limitations, combined with the development
in recent years of surgical methods which have a
broader field of application, have led to less frequent
use of gingivectomy in the treatment of periodontal
disease.
Flap operation with or without osseous surgery
Flap operations can be used in all cases where surgical
treatment of periodontal disease is indicated. Flap
procedures are particularly useful at sites where pock
-
ets extend beyond the mucogingival border and/or
where treatment of bony lesions and furcation in-
volvements is required.
The advantages of flap operations include:
•
existing gingiva is preserved
•
the marginal alveolar bone is exposed whereby the
morphology of bony defects can be identified and
the proper treatment rendered
•
furcation areas are exposed, the degree of involve-
ment and the "tooth-bone" relationship can be iden
-
tified
•
the flap can be repositioned at its original level or
shifted apically, thereby making it possible to adjust
the gingival margin to the local conditions
•
the flap procedure preserves the oral epithelium
and often makes the use of surgical dressing super
-
fluous
•
the postoperative period is usually less unpleasant
for the patient when compared to gingivectomy.
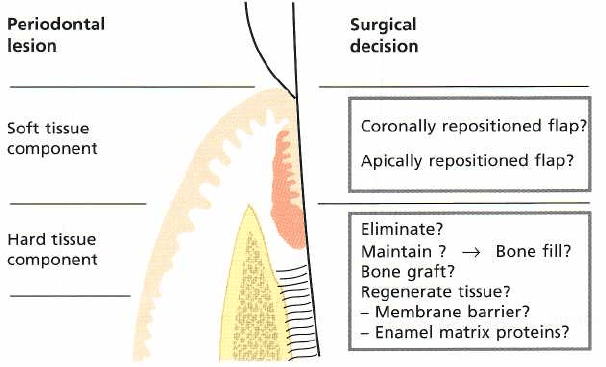
Treatment decisions for soft and hard tissue pockets
in flap surgery
Classifications of different flap modalities used in the
treatment of periodontal disease often make distinc-
tions between methods involving the marginal tissues
and those involving the mucogingival area and, fur-
ther, between tissue eliminating/resective varieties
and tissue preserving/reconstructive types (access
flaps for debridement). Such classifications appear
less than precise since several techniques are often
combined in the treatment of individual cases, and
since there is no clear-cut relationship between disease
characteristics and selection of surgical methods.
From a didactic point of view it seems more appropri-
ate to discuss surgical therapy with regard to how to
deal with (1) the soft tissue component and (2) the
hard tissue component of the periodontal pocket at a
specific tooth site (Fig. 25-52).
Soft
tissue pockets
The description of the various flap procedures reveals
that, depending on the surgical technique used, the
soft tissue flap should either be apically positioned at
the level of the bone crest (original Widman flap,
Neumann flap and apically repositioned flap) or
maintained in a coronal position (Kirkland flap, modi
-
fied Widman flap and papilla perservation flap) at the
completion of the surgical intervention. The mainte-
nance of the presurgical soft tissue height is of impor
-
tance from an esthetic point of view, particularly in the
anterior tooth region. However, long-term results
from clinical trials have shown that major differences
in the final position of the soft tissue margin are not
evident between surgical procedures involving coro-
nal and apical positioning of the flap margin. The
reported difference in final positioning of the gingival
margin between surgical techniques is attributed to
osseous recontouring (Townsend-Olsen et al. 1985,
Lindhe et al. 1987, Kaldahl et al. 1996, Becker et al.
2001). In many patients, however, it may be of signifi
-
cance to position the flap coronally in the anterior
tooth region in order to give the patient a prolonged
period of adaptation to the inevitable soft tissue reces
-
Fig. 25-52.
Surgical decisions.
Treat
ment decisions with respect to
the
soft and the hard tissue
compo
nent of a periodontal
pocket.
