Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

PERIODONTAL SURGERY: ACCESS THERAPY • 525
The apically repositioned flap
In the 1950s and 1960s new surgical techniques for the
removal of soft and, when indicated, hard tissue peri-
odontal pockets were described in the literature. The
importance of maintaining
an adequate zone of attached
gingiva
after surgery was now emphasized. One of the
first authors to describe a technique for the preserva-
tion of the gingiva following surgery was
Nabers
(
1954). The surgical technique developed by Nabers
was originally denoted "repositioning of attached
gingiva" and was later modified by Ariaudo & Tyrrell
(
1957). In 1962
Friedman
proposed the term
apically
repositioned flap
to more appropriately describe the
surgical technique introduced by Nabers. Friedman
emphasized the fact that, at the end of the surgical
procedure, the entire complex of the soft tissues
(
gingiva and alveolar mucosa) rather than the gingiva
alone was displaced in an apical direction. Thus,
rather than excising the amount of gingiva which
would be in excess
after
osseous surgery (if per-
formed), the whole mucogingival complex was main-
tained and apically repositioned. This surgical tech-
nique was used on buccal surfaces in both maxillas
and mandibles and on lingual surfaces in the mandi-
ble, while an excisional technique had to be used on
the palatal aspect of maxillary teeth.
Technique
According to Friedman (1962) the technique should be
performed in the following way:
•
A reverse bevel incision is made using a scalpel with
a Bard-Parker blade (No. 12B or No. 15). How far
from the buccal/lingual gingival margin the inci-
sion should be made is dependent on the pocket
depth as well as the thickness and the width of the
gingiva (Fig. 25-17). If the gingiva preoperatively is
thin and only a narrow zone of keratinized tissue is
present, the incision should be made close to the
tooth. The beveling incision should be given a scal-
loped outline to ensure maximal interproximal cov-
erage of the alveolar bone, when the flap sub-
sequently is repositioned. Vertical releasing inci-
sions extending out into the alveolar mucosa (i.e.
past the mucogingival junction) are made at each of
the end points of the reverse incision, thereby mak
-
ing possible the apical repositioning of the flap.
•
A full thickness mucoperiosteal flap including buc-
cal/lingual gingiva and alveolar mucosa is raised
by
means of a mucoperiosteal elevator. The flap has
to
be elevated beyond the mucogingival line in
order to
later be able to reposition the soft tissue
apically.
The marginal collar of tissue, including
pocket
epithelium and granulation tissue, is re-
moved with
curettes (Fig. 25-18), and the exposed
root surfaces
are carefully scaled and planed.
•
The alveolar bone crest is recontoured with the
objective of recapturing the normal form of the
alveolar process but at a more apical level (Fig.
25-
19). The osseous surgery is performed using burs
and/or bone chisels.
•
Following careful adjustment, the buccal/lingual
flap is repositioned to the level of the newly recon-
toured alveolar bone crest and secured in this posi-
tion (Fig. 25-20). The incisional and excisional tech-
nique used means that it is not always possible to
obtain proper soft tissue coverage of the denuded
interproximal alveolar bone. A periodontal dressing
should therefore be applied to protect the exposed
bone and to retain the soft tissue at the level of the
bone crest (Fig. 25-21). After healing, an "adequate"
zone of gingiva is preserved and no residual pock-
ets should remain.
To handle periodontal pockets on the palatal aspect of
the teeth, Friedman described a modification of the
"
apically repositioned flap", which he termed the
bev-
eled flap.
Since there is no alveolar mucosa present on
the palatal aspect of the teeth, it is not possible to
reposition the flap in an apical direction.
•
In order to prepare the tissue at the gingival margin
to properly follow the outline of the alveolar bone
crest, a conventional mucoperiosteal flap is first
resected (Fig. 25-22).
•
The tooth surfaces are debrided and osseous recon-
touring is performed (Fig. 25-23).
•
The palatal flap is subsequently replaced and the
gingival margin is prepared and adjusted to the
alveolar bone crest by a secondary scalloped and
beveled incision (Fig. 25-24). The flap is secured in
this position with interproximal sutures (Fig. 25-25).
Among a number of suggested advantages of the
apically
repositioned flap
procedure, the following have
been emphasized:
•
Minimum pocket depth postoperatively.
•
If optimal soft tissue coverage of the alveolar bone
is obtained, the postsurgical bone loss is minimal.
•
The postoperative position of the gingival margin
may be controlled and the entire mucogingival
complex may be maintained.
The sacrifice of periodontal tissues by bone resection
and the subsequent exposure of root surfaces (which
may cause esthetic and root hypersensitivity prob-
lems) were regarded as the main disadvantages of this
technique.
526 • CHAPTER 25
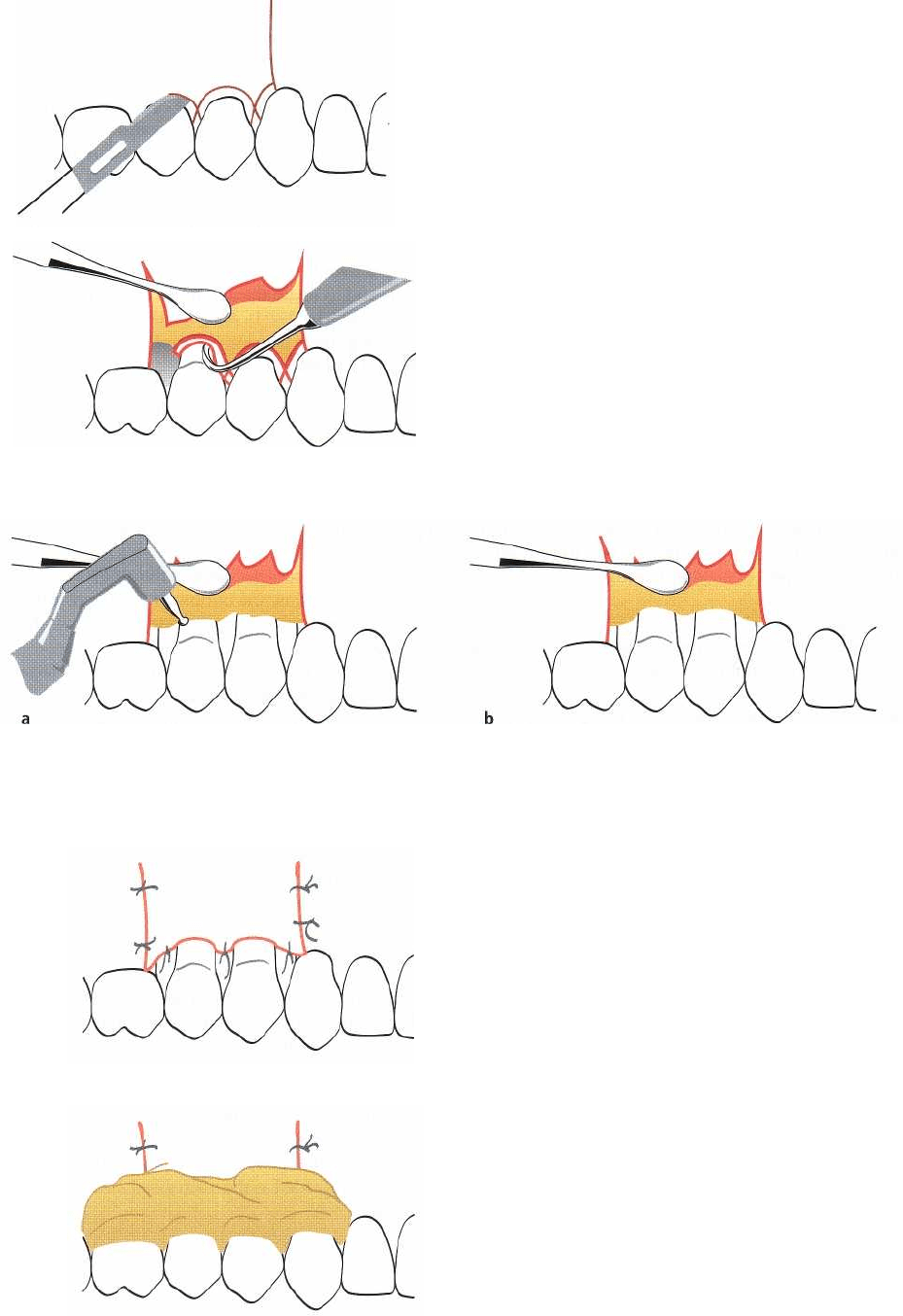
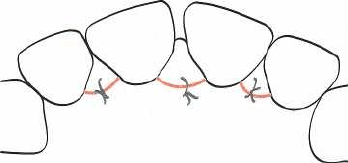
Fig. 25-17.
Apically
repositioned
flap.
Following a vertical
releasing incision, the reverse bevel incision is made
through the gingiva and the periosteum to separate the
inflamed tissue adjacent to the tooth from the flap.
Fig. 25-18.
Apically
repositioned
flap.
A mucoperiosteal
flap is raised and the tissue collar remaining around
the teeth, including the pocket epithelium and the in-
flamed connective tissue, is removed with a currette.
Fig. 25-19.
Apically
repositioned
flap.
Osseous surgery is performed with the use of a rotating bur (a) to recapture the
physiologic contour of the alveolar bone (b).
Fig. 25-20.
Apically repositioned flap.
The flaps are reposi-
tioned in an apical direction to the level of the recon-
toured alveolar bone crest and retained in this position
by sutures.
Fig. 25-21.
Apically
repositioned
flap.
A periodontal dress-
ing is placed over the surgical area to ensure that the
flaps remain in the correct position during healing.
PERIODONTAL SURGERY: ACCESS THERAPY • 527
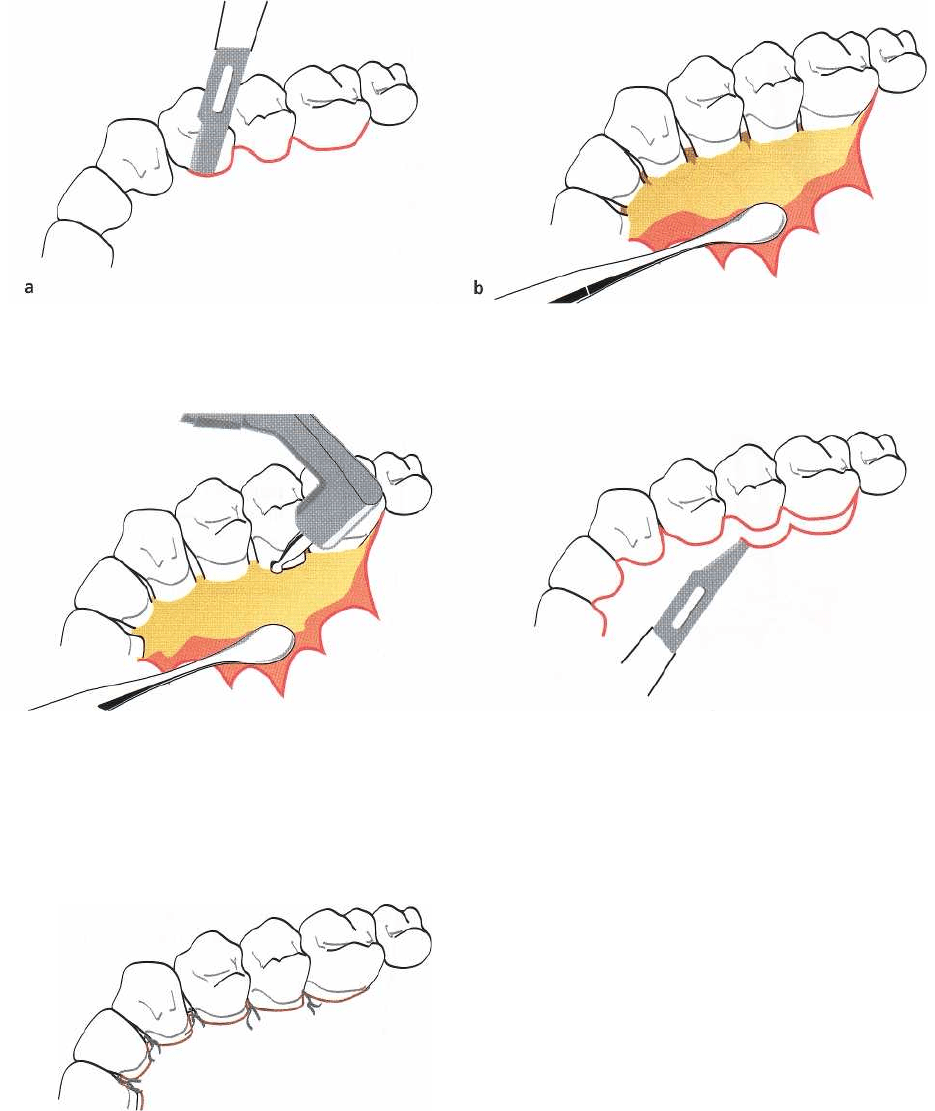
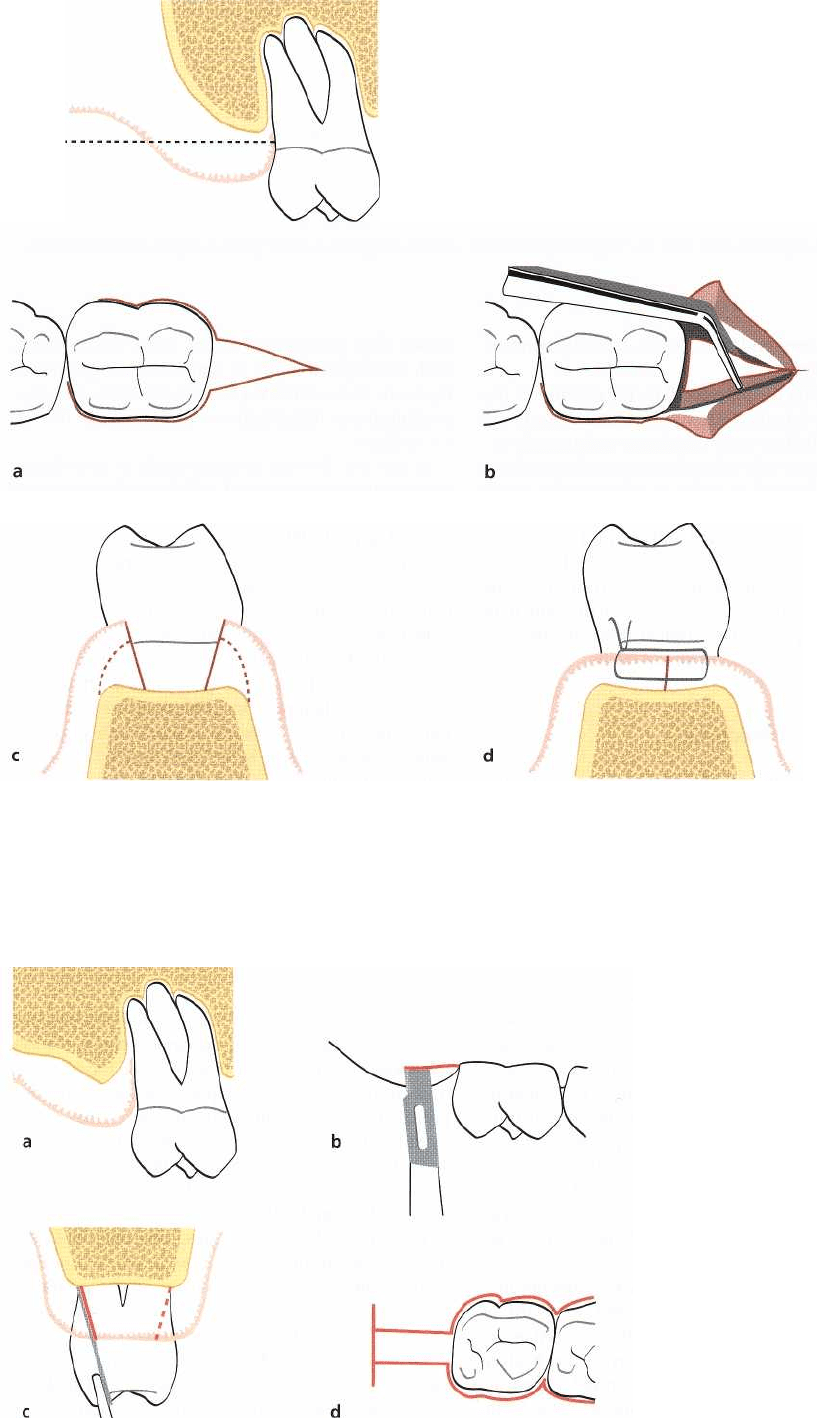
Fig. 25-22.
Beveled
flap.
A primary incision is made intracrevicularly through the bottom of the periodontal pocket
(
a) and a conventional mucoperiosteal flap is elevated (b).
Fig. 25-23.
Beveled
flap.
Scaling, root planing and osse- Fig. 25-24.
Beveled
flap.
The palatal flap is replaced and
ous recontouring is performed in the surgical area. a secondary, scalloped, reverse bevel incision is made
to adjust
the length of the flap to the height of the re
maining
alveolar bone.
Fig. 25-25.
Beveled
flap.
The shortened and thinned flap
is replaced over the alveolar bone and in close contact
with the root surfaces.
528 • CHAPTER 25
Fig. 25-26.
Modified Widman flap.
The initial incision is placed 0.5-1
mm from the gingival margin (a)
and parallel to the long axis of the
tooth.
Fig. 25-27.
Modified Widman flap.
Following careful elevation of the
the flaps, a second intracrevicular
incision (a) is made to the alveolar
bone crest (b) to separate the tis-
sue
collar from the root surface.
Fig. 25-28.
Modified Widman flap.
The third incision is made perpen-
dicular to the root surface (a) and
as
close as possible to the bone
crest (
b), thereby separating the
tissue
collar from the alveolar
bone.
Fig. 25-29.
Modified Widman flap.
(a) Following proper debridement
and currettage of angular bone de-
fects, the flaps are carefully ad-
justed to cover the alveolar bone
and sutured. (b) Complete cover-
age
of the interdental bone as well
as
close adaptation of the flaps to
the
tooth surfaces should be ac-
complished.
PERIODONTAL SURGERY: ACCESS THERAPY • 529
The modified Widman flap
Ramfjord & Nissle (1974) described the
modified Wid-
man flap
technique, which is also recognized as the
open flap curettage
technique. It should be noted that,
while the
original Widman flap
technique included both
apical displacement of the flaps and osseous recon-
touring (elimination of bony defects) to obtain proper
pocket elimination, the
modified Widman flap
technique
is not intended to meet these objectives.
Technique
•
According to the description by Ramfjord & Nissle
(
1974) the
initial incision
(Fig. 25-26), which may be
performed with a Bard-Parker knife (No. 11),
should be parallel to the long axis of the tooth and
placed approximately 1 mm from the buccal gingi-
val margin in order to properly separate the pocket
epithelium from the flap. If the pockets on the buc-
cal aspects of the teeth are less than 2 mm deep or if
esthetic considerations are important, an intracre-
vicular incision may be made. Furthermore, the
scalloped incision should be extended as far as pos
-
sible in between the teeth, to allow maximum
amounts of the interdental gingiva to be included
in the flap. A similar incision technique is used on
the palatal aspect. Often, however, the scalloped
outline of the initial incision may be accentuated by
placing the knife at a distance of 1-2 mm from the
midpalatal surface of the teeth. By extending the
incision as far as possible in between the teeth suf-
ficient amounts of tissue can be included in the
palatal flap to allow for proper coverage of the
interproximal bone when the flap is sutured. Verti-
cal releasing incisions are not usually required.
•
Buccal and palatal full thickness flaps are carefully
elevated with a mucoperiosteal elevator. The flap
elevation should be limited and allow only a few
millimeters of the alveolar bone crest to become
exposed. To facilitate the gentle separation of the
collar of pocket epithelium and granulation tissue
from the root surfaces, an intracrevicular incision is
made around the teeth
(second incision)
to the alveo-
lar crest (Fig. 25-27).
• A
third incision
(Fig. 25-28) made in a horizontal
direction and in a position close to the surface of the
alveolar bone crest separates the soft tissue collar of
the root surfaces from the bone.
•
The pocket epithelium and the granulation tissues
are removed by means of curettes. The exposed
roots are carefully scaled and planed, except for a
narrow area close to the alveolar bone crest in which
remnants of attachment fibers may be preserved.
Angular bony defects are carefully curetted.
•
Following the curettage, the flaps are trimmed and
adjusted to the alveolar bone to obtain complete
coverage of the interproximal bone (Fig. 25-29). If
this adaptation cannot be achieved by soft tissue
recontouring, some bone may be removed from the
outer aspects of the alveolar process in order to
facilitate the all-important flap adaptation. The
flaps are sutured together with individual inter-
proximal sutures. Surgical dressing may be placed
over the area to ensure close adaptation of the flaps
to the alveolar bone and root surfaces. The dressing,
as well as the sutures, are removed after 1 week.
The main advantages of the
modified Widman
flap
tech
-
nique in comparison with other procedures pre-
viously described are, according to Ramfjord & Nissle
(1974):
•
the possibility of obtaining a close adaptation of the
soft tissues to the root surfaces,
•
the minimum of trauma to which the alveolar bone
and the soft connective tissues are exposed and
•
less exposure of the root surfaces, which from an
esthetic point of view is an advantage in the treat-
ment of anterior segments of the dentition.
530 • CHAPTER 25
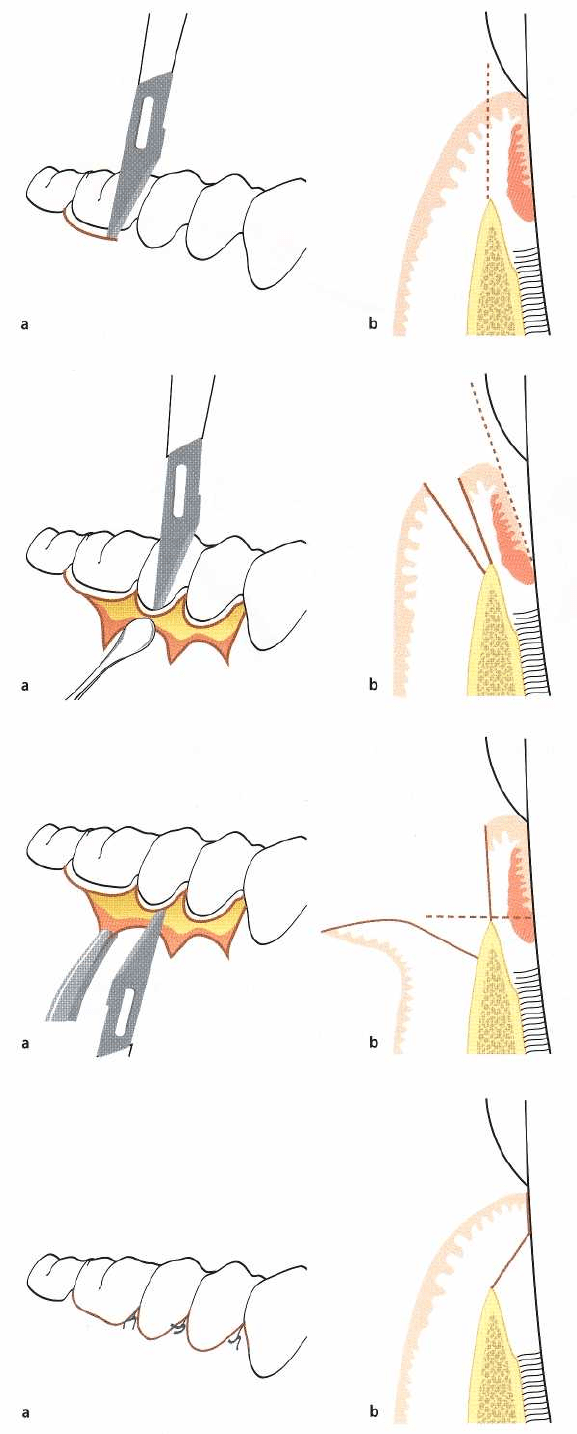
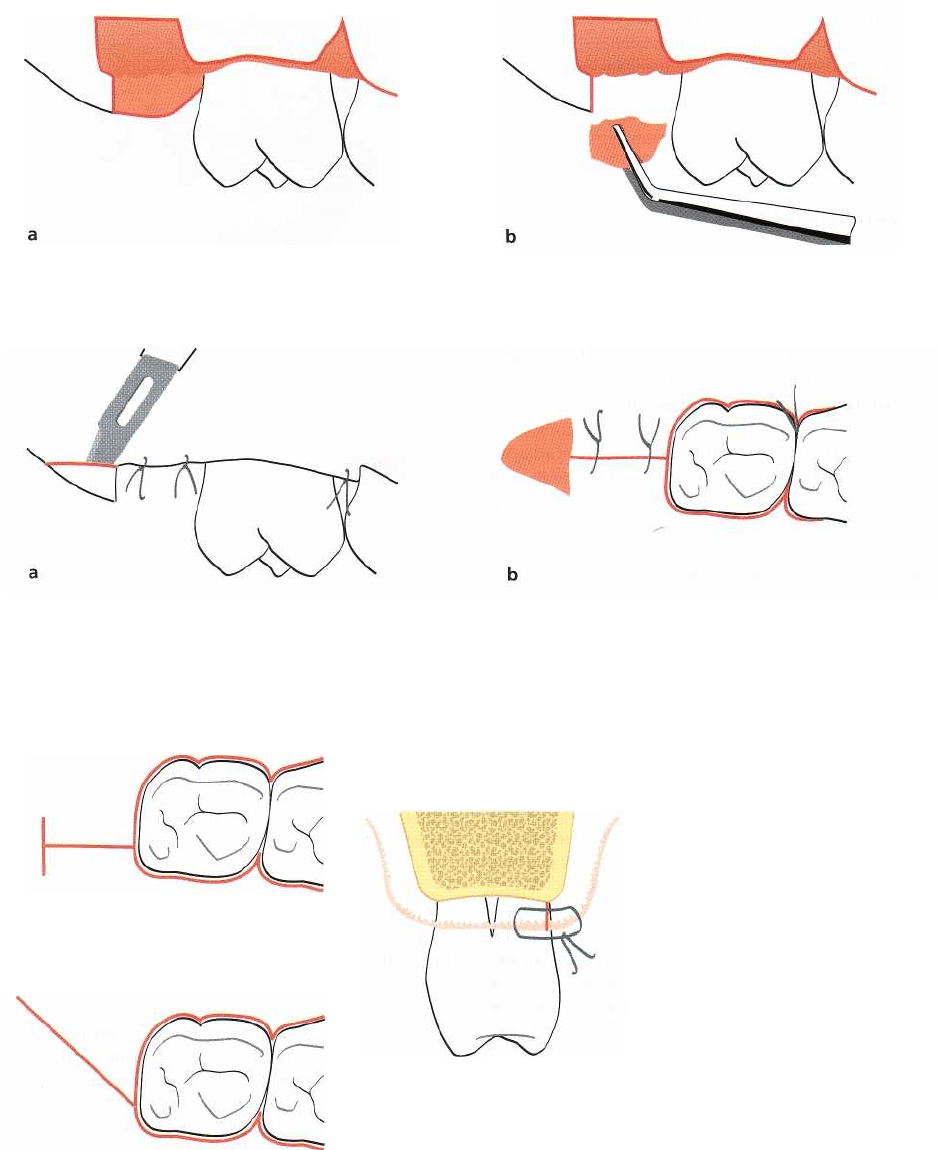
Fig. 25-30.
Papilla preservation flap.
Intrasulcular incisions are made at the facial and proximal aspects of the teeth.
Fig. 25-31.
Papilla preservation flap.
(a) An intrasulcular incision is made along the lingual/palatal aspect of the teeth
with a semi-lunar incision made across each interdental area. (b) A curette or interproximal knife is used to care
-
fully free the interdental papilla from the underlying hard tissue. (c-d) The detached interdental tissue is pushed
through the embrasure with a blunt instrument to be included in the facial flap.
The papilla preservation flap
In order to preserve the interdental soft tissues for
maximum soft tissue coverage following surgical in-
tervention involving treatment of proximal osseous
defects, Takei et al. (1985) proposed a surgical ap-
proach called
papilla
preservation technique.
Later,
Cortellini et al. (1995b, 1999) described modifications
of the flap design to be used in combination with
regenerative procedures. For esthetic reasons, the pa-
pilla preservation technique is often utilized in the
surgical treatment of anterior tooth regions.
Technique
• According to the description by Takei et al. (1985)
the
papilla preservation flap technique
is initiated by an
intrasulcular incision at the facial and proximal as-
pects of the teeth without making incisions through
the interdental papillae (Fig. 25-30a,b). Subsequen-
tly, an intrasulcular incision is made along the lin-
gual/palatal aspect of the teeth with a semi-lunar
incision made across each interdental area (Fig. 25-
31a). The semi-lunar incision should dip apically at
least 5 mm from the line-angles of the teeth, which
will allow the interdental tissue to be dissected from
the lingual/palatal aspect so that it can be elevated
intact with the facial flap. In situations where an
osseous defect has a wide extension into the lin-
gual/palatal area, the semi-lunar incision may be
placed on the facial aspect of the interdental area to
have the papillae included with the lingual/palatal
flap.
•
A curette or interproximal knife is used to carefully
free the interdental papilla from the underlying
hard
tissue (Fig. 25-31b). The detached interdental
tissue
is pushed through the embrasure with a blunt
instrument (Fig. 25-31c,d).
•
A full-thickness flap is reflected with a periosteal
elevator on both facial and lingual/palatal surfaces.
The exposed root surfaces are thoroughly scaled
PERIODONTAL SURGERY: ACCESS THERAPY • 531
Fig. 25-32.
Papilla preservation flap.
The flap is replaced and sutures are placed on the palatal aspect of the interden
-
tal areas.
and root planed and bone defects carefully curetted
(Fig. 25-31d).
•
While holding the reflected flap, the margins of the
flap and the interdental tissue are scraped to remove
pocket epithelium and excessive granulation tissue.
In anterior areas, the trimming of granulation tissue
should be limited in order to maintain the maxi-
mum thickness of tissue.
•
The flaps are repositioned and sutured using cross
mattress sutures (Fig. 25-32). Alternatively, a direct
suture of the semi-lunar incisions can be done as the
only means of flap closure. A surgical dressing may
be placed to protect the surgical area. The dressing
and sutures are removed after 1 week.
Regenerative procedures
In the 1980s treatment of periodontal pockets was
given a new dimension when it was shown that with
specific surgical handling of the periodontal wound a
significant amount of new connective tissue attach-
ment is achievable following surgical treatment (Ny-
man et al. 1982, Bowers et al. 1989).
To obtain periodontal regeneration has always been
a major challenge to the periodontist and several ap-
proaches to periodontal regeneration have been used
throughout the years. The earliest attempts involved
various bone grafting procedures, such as the use of
autogenous grafts from both extraoral and intraoral
donor sites, allogenic marrow grafts and non-decalci-
fied/decalcified lyophilized bone grafts, or "implant"
procedures utilizing slowly resorbable tri-calcium-
phosphate and non-resorbable, non-porous hydroxy-
apatite. Other approaches to periodontal regeneration
involved the use of citric acid for root surface demin-
eralization or the use of methods for improved root
surface biocompatibility or to enhance cellular re-
sponses.
The use of physical barriers, such as membranes
(
non-biodegradable or biodegradable), to retard or
prevent apical migration of epithelium as well as ex-
clude gingival connective tissue from the healing
wound, formed the basis for the concept known as
"
guided tissue regeneration" (Gottlow et al. 1986). The
procedure can be described as a coronally reposi-
tioned flap procedure without bone recontouring,
with
the adjunctive use of a membrane tightened to the
tooth to cover the exposed root surface and adja
cent
intrabony defect before repositioning of the soft
tissue
flaps.
In the late 1990s a new approach to periodontal
regeneration was presented, which involves the use of
a derivate of enamel matrix proteins (Hammarstrom
1997, Heijl et al. 1997). These proteins are involved in
the embryogenesis of cementum, periodontal liga-
ment and supporting bone, and when applied to the
exposed root surface facing an intrabony periodontal
defect they mediate regeneration of a new attachment
apparatus. The surgical procedure is performed as a
coronally repositioned flap procedure without bone
recontouring. Before repositioning of the soft tissue
flaps, the exposed roots are treated with EDTA for
removal of the "smear layer", followed by the appli-
cation of the derivate of enamel matrix proteins.
Various regenerative procedures for surgical treat-
ment of periodontal lesions, as well as the biological
basis for periodontal regeneration, are discussed in
detail in Chapter 28.
DISTAL WEDGE PROCEDURES
In many cases the treatment of periodontal pockets on
the distal surface of distal molars is complicated by
the presence of bulbous tissues over the tuberosity or
by a prominent retromolar pad. The most direct ap-
proach to pocket elimination in such cases in the
maxilla is the gingivectomy procedure. The incision is
started on the distal surface of the tuberosity and
carried forward to the base of the pocket of the distal
surface of the molar (Fig. 25-33).
However, when only limited amounts of kerati-
nized tissue are present, or none at all, or if a distal
angular bony defect has been diagnosed, the bulbous
tissue should be reduced in size rather than being
removed
in toto.
This may be accomplished by the
distal wedge procedure
(Robinson 1966). This technique
facilitates access to the osseous defect and makes it
possible to preserve sufficient amounts of gingiva and
mucosa to achieve soft tissue coverage.
532 • CHAPTER 25
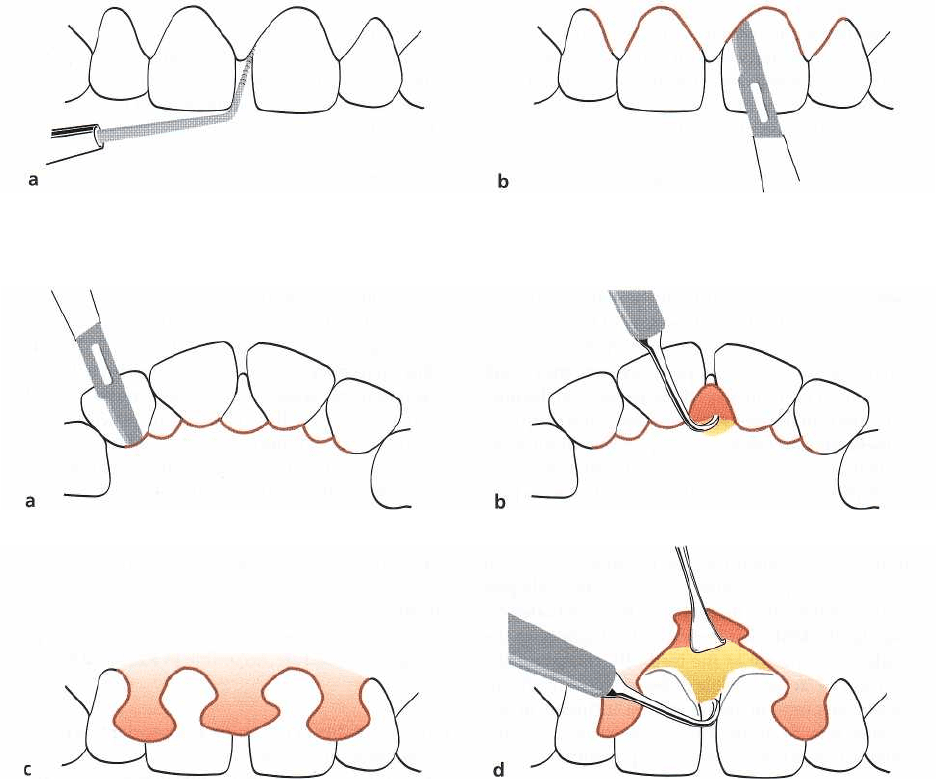
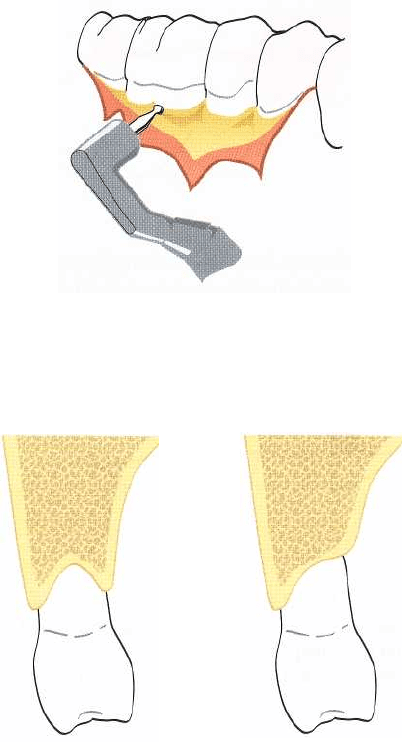
Fig. 25-33.
Distal wedge procedure.
Simple gingivectomy
incision (broken line) can be used to eliminate a soft tis-
sue pocket and adjacent fibrous tissue pad behind a
maxillary molar.
Fig. 25-35.
Modified distal wedge pro-
cedure. A
deep periodontal pocket
combined with an angular bone
defect at the distal aspect of a max-
illary molar (a). Two parallel re-
verse bevel incisions, one buccal
and one palatal, are made from the
distal surface of the molar to
the
posterior part of the tuberosity
(b-
d), where they are connected with a
buccolingual incision (d).
The
buccal and palatal incisions
are
extended in a mesial direction
along the buccal and palatal sur-
faces of the molar to facilitate flap
elevation.
Fig. 25-34.
Distal
wedge procedure.
(a) Buccal and lingual vertical incisions are made through the retromolar pad to
form a triangle behind a mandibular molar. (b) The triangular-shaped wedge of tissue is dissected from the under-
lying bone and removed. (c) The walls of the buccal and lingual flaps are reduced in thickness by undermining inci-
sions (broken lines). (d) The flaps, which have been trimmed and shortened to avoid overlapping wound margins,
are sutured.
PERIODONTAL SURGERY: ACCESS THERAPY •
533
Fig. 25-36.
Modified distal wedge procedure.
Buccal and palatal flaps are elevated (a) and the rectangular wedge is re-
leased from the tooth and underlying bone by sharp dissection and removed (b).
Fig. 25-37.
Modified distal wedge procedure.
Following bone recontouring and root debridement, the flaps are
trimmed and shortened to avoid overlapping wound margins and sutured (a). A close soft tissue adaptation
should be accomplished to the distal surface of the molar. The remaining fibrous tissue pad distal to the buccolin
gual incision line is "leveled" by the use of a gingivectomy incision (b, c).
Fig. 25-38.
Modified incision tech-
niques in distal wedge procedures.
To
ensure optimal flap adaptation at
the furcation site the incision tech-
nique may be modified. The
amount of attached keratinized tis-
sue present as well as the accessi-
bility to the retromolar area has to
be considered when placing the in-
cision.
Technique
•
Buccal and lingual incisions are made in a vertical
direction through the tuberosity or retromolar pad
to
form a triangular wedge (Fig. 25-34a). The facial
and
lingual incisions should be extended in a mesial
direction along the buccal and lingual surfaces of
the
distal molar to facilitate flap elevation.
•
The facial and lingual walls of the tuberosity or
retromolar pad are deflected and the incised wedge
of
tissue is dissected and separated from the bone
(Fig.
25-34b).
•
The walls of the facial and lingual flaps are then
reduced in thickness by undermining incisions (Fig.
25-34c). Loose tags of tissue are removed and the
root
surfaces are scaled and planed. If necessary, the bone
is recontoured.
•
The buccal and lingual flaps are replaced over the
exposed alveolar bone, and the edges trimmed to
avoid overlapping wound margins. The flaps are
secured in this position with interrupted sutures
(Fig.
25-34d). The sutures are removed after ap
proximately
1 week.
534 • CHAPTER 25
The original distal wedge procedure may be modified
according to individual requirements. Some com-
monly used modifications of the incision technique
are illustrated in Figs. 25-35 to 25-38, all having as a
goal to eliminate the deep pocket and to achieve mu-
cosal coverage of the remaining periodontium.
OSSEOUS SURGERY
The principles of osseous surgery in periodontal ther
-
apy were outlined by Schluger (1949) and Goldman (
1950). They pointed out that alveolar bone loss
caused by inflammatory periodontal disease often
results in an uneven outline of the bone crest. Since,
according to these authors, the gingival contour is
closely dependent on the contour of the underlying
bone as well as the proximity and anatomy of adjacent
tooth surfaces, the elimination of soft tissue pockets
often has to be combined with osseous reshaping and
the elimination of osseous craters and angular bony
defects to establish and maintain shallow pockets and
optimal gingival contour after surgery.
Osteoplasty
The term
osteoplasty
was introduced by Friedman in
1955. The purpose of osteoplasty is to create a physi
-
ologic form of the alveolar bone
without
removing any
"
supporting" bone. Osteoplasty therefore is a tech-
nique analogous to gingivoplasty. Examples of osteo-
plasty are the thinning of thick osseous ledges and the
establishment of a scalloped contour of the buccal
(
lingual and palatal) bone crest (Fig. 25-39). In flap
surgery without bone recontouring, interdental mor-
phology may sometimes preclude optimal mucosal
coverage of the bone postsurgically, even if pro-
nounced scalloping of soft tissue flaps is performed.
In such a situation, removal of non-supporting bone
by vertical grooving to reduce the faciolingual dimen-
sion of the bone in the interdental areas may facilitate
flap adaptation, thereby reducing the risk of bone
denudation as well as reducing the risk of ischemic
necrosis of unsupported mucosal flaps due to flap
margin deficiencies.
Removal of non-supporting bone may sometimes
also be required to gain access for intrabony root
surface debridement. The leveling of interproximal
craters and the elimination (or reduction) of bony
walls of circumferential osseous defects are often re-
ferred to as "osteoplasty" since usually no resection of
supporting bone is required (Fig. 25-40).
Ostectomy
By
ostectomy,
supporting bone, i.e. bone directly in-
volved in the attachment of the tooth, is removed to
reshape deformities caused by periodontitis in the
Fig. 25-39.
Osteoplasty.
Thick osseous ledges in a
mandibular molar region area are eliminated with the
use of a round bur to facilitate optimal flap adaptation.
Fig. 25-40.
Osteoplasty.
Leveling of an interproximal
bone crater through the removal of the palatal bone
wall. For esthetic reasons the buccal bone wall is main
tained to support the height of the soft tissue.
marginal and interdental bone. Ostectomy is consid
-
ered to be an important part of surgical techniques
aimed at pocket elimination. As a general rule, how-
ever, care must be exercised when supporting bone is
to be removed.
After exposing the alveolar bone by elevation of a
flap, buccal and/or lingual crater walls are reduced to
the base of the osseous defect using bone chisels and
bone rongeurs (Fig. 25-41). A round bur or a diamond
stone under continuous saline irrigation can also be
used. If bone resection has been carried out in the
interdental area, the buccal and lingual/palatal bone
margins may subsequently have to be recontoured to
compensate for discrepancies in bone height resulting
from the interdental bone resection (Fig. 25-41b). It is
considered important to remove the small peaks of
bone which often remain in the area of the line angles.
The objective of bone surgery is thus to establish a
"
physiologic" anatomy of the alveolar bone, but at a
more apical level.
