Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

PERIODONTAL SURGERY: ACCESS THERAPY • 545
sion. In the posterior tooth region, an apical position-
ing should be the standard.
Independent of flap positioning the goal should be
to achieve complete soft tissue coverage of the alveolar
bone, not only at buccal /lingual sites but also in proxi
mal sites. It is therefore of utmost importance to
care-
fully plan the incisions in such a way that this
goal can
be achieved at the termination of the surgical
interven
tion.
Hard tissue pockets
During conventional periodontal surgery one would
usually opt for the conversion of an intrabony defect
into a suprabony defect, which then is eliminated by
an apical repositioning of the soft tissues. Osseous
recontouring of angular bony defects and craters in-
volves excisional techniques which should be used
with caution and discrimination. However, the thera-
pist is often faced with the dilemma of deciding
whether or not to eliminate an angular bony defect.
There are a number of factors that should be consid-
ered in the treatment decision, such as:
•
esthetics
•
tooth/tooth site involved
•
defect morphology
•
amount of remaining periodontium
Since alveolar bone supports the soft tissue, an altered
bone level through recontouring will result in reces-
sion of the soft tissue margin. For esthetic reasons one
may therefore be conservative in eliminating proximal
bony defects in the anterior tooth region. For example,
in the case of an approximal crater it may often be
sufficient to reduce/eliminate the bone wall on the
lingual side of the crater, thereby maintaining the bone
support for the soft tissue on the facial aspect (Fig.
25-40). In favor of esthetics one may even have to
compromise the amount of bone removal and accept
that some pocket depth will remain in certain situ-
ations. In addition to esthetics, the presence of furca-
tions may limit the extent to which bone recontouring
can be performed.
Defect morphology is a variable of significance for
repair/regeneration during healing (Rosling et al.
1976a, Cortellini et al. 1993, 1995a). While two and,
especially, three-wall defects may show great poten-
tial for repair/regeneration, one-wall defects and ap-
proximal craters will rarely result in such a healing.
Further, the removal of intrabony connective tissue/
granulation tissue during a surgical procedure will
always lead to crestal resorption of bone, especially in
sites with thin bony walls. This results in reduction of
the vertical dimensions of the bone tissue at the site
(
Fig. 25-53). Thus, the potential for bone fill following
a
compromise in regard to osseous surgery is greater
in
areas with thick, non-supporting bone.
The various treatment options available for the
hard tissue defect may include:
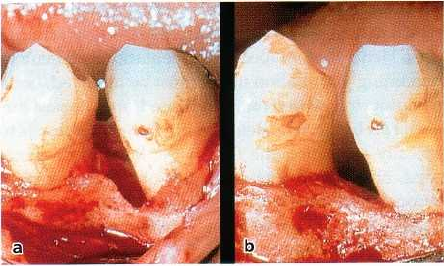
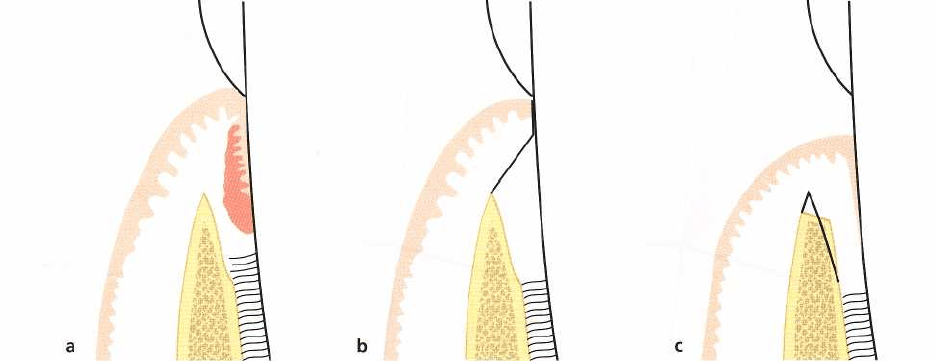
Fig. 25-53. Illustration of the amount of crestal bone re
-
sorption that may take place following a modified Wid
-
man flap procedure without bone recontouring. (a)
View of the area at time of initial surgical treatment. (b)
At the re-entry operation performed after 6 months of
healing.
•
elimination of the osseous defect by resection of
bone (osteoplasty and/or ostectomy)
•
maintenance of the area without osseous resection
(hoping for some type of periodontal repair, e.g.
bone fill leading to gain of clinical attachment),
•
compromising the amount of bone removal and
accepting that a certain pocket depth will remain
•
an attempt to improve healing through the use of a
regenerative procedure or
•
extraction of the involved tooth if the bony defect is
considered too advanced.
After careful consideration, indications for osseous
surgery in conjunction with apical repositioning of
flaps may also include subgingival caries, perfora-
tions or root fractures in the coronal third of the root
as well as inadequate retention for fixed prosthetic
restorations due to a short clinical crown (crown-
lengthening procedures). The "crown lengthening"
needed in such cases is performed by removing often
significant amounts of supporting bone and by recon-
touring. A "biologic width" of approximately 3 mm is
needed between the alveolar bone crest to be establ-
ished and the anticipated restoration margin for suc-
cessful results (Bragger et al. 1992, Herrero et al. 1995,
Pontoriero & Carnevale 2001).
Root surface instrumentation
Before incisions are made to excise or elevate the soft
tissue, a careful examination should be carried out to
identify at which tooth sites periodontal lesions re-
main. Only tooth sites with signs of pathology (bleed-
ing following pocket probing) should be subjected to
root instrumentation following surgical exposure.
Further, at these sites, root surface instrumentation
should be limited to that part of the root that will be
covered by the soft tissue following flap replacement
and suturing. This is an important consideration since
instrumentation of the supragingival portion of the
546 • CHAPTER 25
root may lead to postsurgical dentin hypersensitivity,
which in turn may impede proper oral hygiene meas-
ures. Hence, before root instrumentation is executed,
remaining granulation tissue must be removed, bone
recontouring carried out, if indicated, and the postsur
-
gical soft tissue level determined. If the intention is to
apically reposition the flap at the level of the bone
crest, only approximately 3 mm of the root surface
coronal to the bone crest has to be carefully scaled and
root planed, whereas if the flap is to be coronally
positioned the entire exposed root often has to be
instrumented.
The root instrumentation can be performed with
hand or ultrasonic instruments according to the op-
erator's preferences. Ultrasonic (sonic) instrumenta-
tion offers the additional benefits of improved visibil-
ity due to the irrigating effect of the cooling water. For
root instrumentation within intrabony defects, root
concavities and entrances to furcations, the use of
rotating fine-grained diamond stones may be used.
Root surface conditioning/ biomodification
An important consideration in periodontal surgery is
to make the exposed root surface biologically compat-
ible with a healthy periodontium. This so-called con-
ditioning includes removing bacteria, endotoxins and
other antigens found within the cementum-dentin of
a
pathologically exposed root. In addition to scaling
and
root planing, agents such as citric acid/ortho-
phosphoric acid, tetracycline and EDTA are used for
root surface conditioning. Root surface condition-
ing/biomodification by means of an etching proce-
dure may serve several purposes:
•
removal of the smear layer following mechanical
debridement
•
demineralization of the root surface (citric acid)
•
selective removal of hydroxyapatite and exposure
of the collagenous matrix of the root surface (EDTA)
•
local delivery of antimicrobial compound (tetracy-
cline HCL)
•
inhibition of collagenolytic activity (tetracycline
HCL)
•
enhancing cellular responses (migration and
attach
ment)
•
preventing epithelial down-growth
•
improving retention of different biomolecules to
exposed collagen
•
expressing a cementoblast phenotype for coloniz-
ing cells.
It should be noted that etching of a root surface with
an agent operating at a low pH, e.g. citric acid or
orthophosphoric acid, might exert immediate ne-
crotizing effects on the surrounding periodontal liga-
ment and other periodontal tissues, whereas agents
operating at a neutral pH (e.g. EDTA) do not seem to
have this negative effect (Blomlof & Lindskog
1995a,
b).
Although
in vitro
results have indicated possible
benefits of the use of root surface conditioning/bio-
modification agents through enhanced cellular re-
sponses during wound healing, the usefulness of ac-
ids as well as other chemical agents for conditioning
of root surfaces in conjunction with conventional peri
-
odontal surgery has been questioned (Blomlof et al.
2000). Histological evidence indicates that healing fol-
lowing root surface conditioning with acids or other
chemical agents is generally dominated by a long
junctional epithelium or connective tissue attachment
without evidence of new cementum formation. How-
ever, root surface biomodification must still be re-
garded as an important method to facilitate regenera-
tion. Thus, in this treatment the root represents one of
the wound margins and must provide an appropriate
surface for cell attachment, colonization and prolifera
-
tion.
Suturing
When a flap procedure has been employed it is impor
-
tant to ensure that, at the end of surgery, the flaps are
placed in the intended position and that the flaps are
properly adapted to each other and to the tooth sur-
faces. Preferably, full coverage of the buccal/lingual
(
palatal) and interdental alveolar bone should be ob-
tained by full (primary) closure of the soft tissue flaps.
If this can be achieved, healing by first intention re-
sults and the postoperative bone resorption becomes
minimal. Therefore, prior to suturing, the flap margins
should be trimmed to properly fit the buccal and
lingual (palatal) bone margin as well as the interproxi
-
mal areas; excessive soft tissue must be removed. If the
amount of flap tissue present is insufficient to cover
the interproximal bone, the flaps at the buccal or
lingual aspects of the teeth must be recontoured and,
in some cases, even coronally displaced.
Following proper trimming, the flaps are secured
in
the correct position by sutures. The materials most
commonly used as sutures in periodontal surgery are
fabricated of silk and various synthetic materials. The
dimensions usually preferred are 3-0 or 4-0. These
materials are non-resorbable and should be removed
after 7-14 days. If the sutures need to be maintained in
place for several weeks, Teflon® suture material is
preferable due to minimal tissue reactions to the ma-
terial.
Since the flap tissue following the final preparation
is thin, non-traumatic needles (eyeless), either curved
or straight, with a small diameter should be used.
Such needles are available as rounded (non-cutting)
or with different cutting edges.
PERIODONTAL SURGERY: ACCESS THERAPY • 547
a a
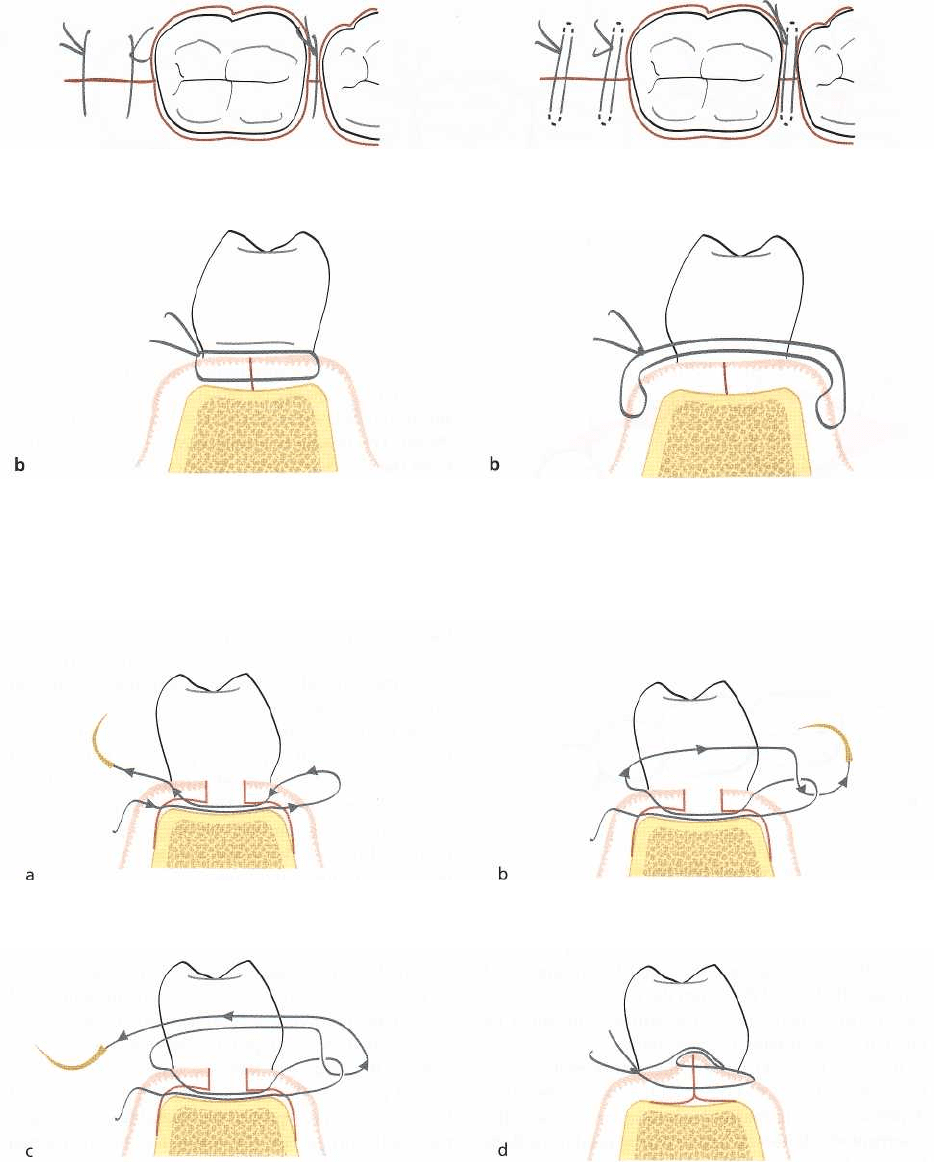
Fig. 25-54a,b.
Suturing.
Interrupted interdental suture.
Fig. 25-55a,b.
Suturing.
Modified interrupted interden-
tal suture. Note that with this suturing technique the
suture is lying on the surface of the interdental tissue
keeping the soft tissue flaps in close contact with the
underlying bone.
Fig. 25-56a-d.
Suturing.
Modified mattress suture.
Suturing technique
The three most frequently used sutures in periodontal
flap surgery are:
•
interrupted interdental sutures,
•
suspensory sutures and
•
continuous sutures.
The
interrupted interdental suture
(Fig. 25-54) provides
a
close interdental adaptation between the buccal and
lingual flaps with equal tension on both units. This
type
of suture is therefore not recommended when the buccal
and lingual flaps are repositioned at different
levels.
When this technique of suturing is employed,
548 • CHAPTER 25
a
b
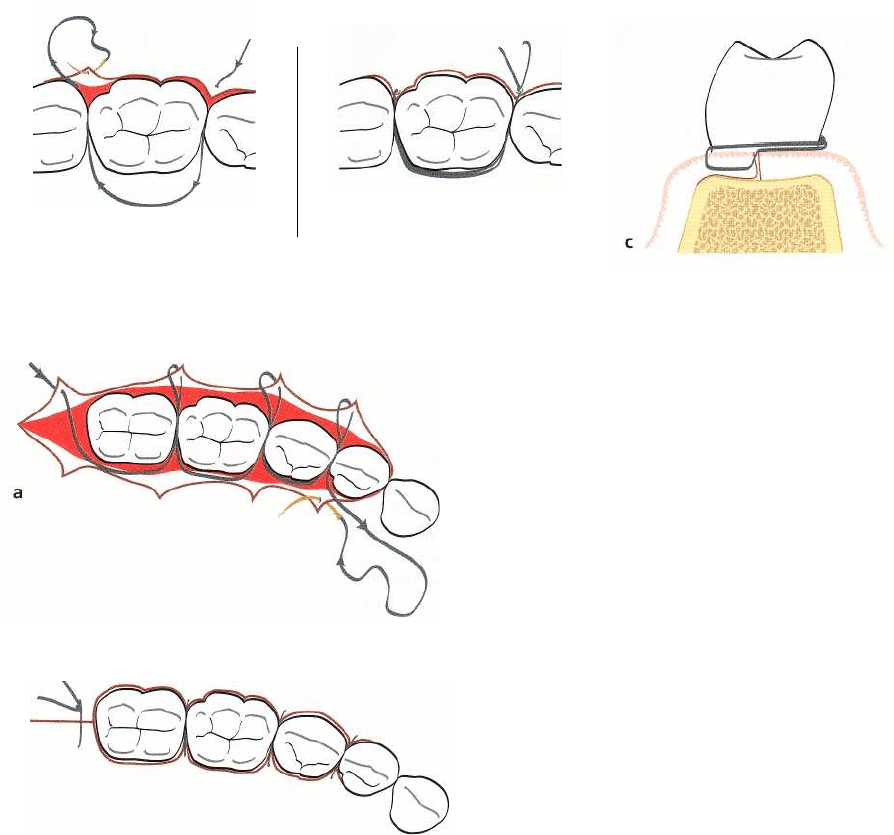
Fig. 25-57a-c.
Suturing.
Suspensory suture.
Fig. 25-58a,b.
Suturing.
Continuous suture.
the needle is passed through the buccal flap from the
external surface, across the interdental area and
through the lingual flap from the internal surface, or
vice versa. When closing the suture, care must be
taken to avoid tearing the flap tissues.
In order to avoid having the suture material be-
tween the mucosa and the alveolar bone in the inter-
dental area, an alternative technique for the use of the
interrupted interdental suture can be used if the flaps
have not been elevated beyond the mucogingival line
(
Fig. 25-55). With the use of a curved needle the suture
is anchored in the attached tissue on the buccal aspect
of the proximal site, the suture brought to the lingual
side through the proximal sites, and anchored in the
attached tissue on the lingual side. The suture is then
brought back to the starting point and tied (Fig. 25-
55b). Hence, the suture will be lying on the surface of
the interdental tissue, keeping the soft tissue flaps in
close contact with the underlying bone.
In regenerative procedures, which usually require
a
coronal advancing of the flap,
a modified mattress suture
may be used to secure close flap adaptation (Fig.
25-56)
. The needle is passed through the buccal flap
from the
external surface, across the interdental area and
through the lingual flap from the internal surface.
The
suture is run back to the buccal side by passing
the
needle through the lingual and buccal flaps. There-
after, the suture is brought through the approximal site
coronally to the tissue, passed through the loop of the
suture on the lingual aspect, and then brought back to
the starting point on the buccal side and tied.
The
suspensory suture
(Fig. 25-57) is used primarily
when the surgical procedure is of limited extent and
involves only the tissue of the buccal or lingual aspect
of the teeth. It is also the suture of choice when the
buccal and lingual flaps are repositioned at different
levels. The needle is passed through the buccal flap
from its external surface at the mesial side of the tooth,
the suture placed around the lingual surface of the
tooth and the needle passed through the buccal flap
on the distal side of the tooth (Fig. 25-57a). The suture
is
brought back to the starting point via the lingual
surface of the tooth and tied (Fig. 25-57b,c). If a lingual
flap has been elevated as well, this is secured in the
intended position using the same technique.
The
continuous suture
(Fig. 25-58) is commonly used
when flaps involving several teeth are to be apically
repositioned. When flaps have been elevated on both
sides of the teeth, one flap at a time is secured in its
correct position. The suturing procedure is started at
the mesial/distal aspect of the buccal flap by passing
the needle through the flap and across the interdental
area. The suture is laid around the lingual surface of
the tooth and returned to the buccal side through the
next interdental space. The procedure is repeated
tooth
by tooth until the distal/mesial end of the flap
is
reached. Thereafter, the needle is passed through the
lingual flap (Fig. 25-58a), with the suture laid around
the buccal aspect of each tooth and through each
interproximal space. When the suturing of the lingual
flap is completed and the needle has been brought
back to the first interdental area, the positions of the
b
PERIODONTAL SURGERY: ACCESS THERAPY • 549
flaps are adjusted and secured in their proper posi-
tions by closing the suture (Fig. 25-58b). Thus, only
one knot is needed.
Periodontal dressings
Periodontal dressings are mainly used:
•
to protect the wound postsurgically,
•
to obtain and maintain a close adaptation of the
mucosal flaps to the underlying bone (especially
when a flap has been apically repositioned) and
•
for the comfort of the patient.
In addition, periodontal dressings can, during the
initial phase of healing, prevent postoperative bleed-
ing and, if properly placed in the operated segment
(
especially interproximally), prevent the formation of
excessive granulation tissue.
Periodontal dressings should have the following
properties:
•
The dressing should be soft, but still have enough
plasticity and flexibility to facilitate its placement in
the operated area and to allow proper adaptation.
•
The dressing should harden within a reasonable
time.
•
After setting, the dressing should be sufficiently
rigid to prevent fracture and dislocation.
•
The dressing should have a smooth surface after
setting to prevent irritation to the cheeks and lips.
•
The dressing should preferably have bactericidal
properties to prevent excessive plaque formation.
•
The dressing must not detrimentally interfere with
healing.
It has been suggested that antibacterial agents should
be incorporated in periodontal dressings to prevent
bacterial growth in the wound area during healing.
Results from clinical studies and
in vitro
evaluation of
the antibacterial properties of various periodontal
dressings, however, suggest that the antibacterial ac-
tivity of most commercial dressings probably is ex-
hausted long before the end of the 7-14-day period
during which the dressing is frequently maintained in
the operated segment (O'Neil 1975, Haugen et al.
1977).
Mouth rinsing with antibacterial agents such as
chlorhexidine does not prevent the formation
of
plaque
under
the dressing (Plyss et al. 1975) and
should therefore not be regarded as a means to im-
prove or shorten the period
of
wound healing. On the
other hand, results from clinical studies as well as
clinical experience suggest that a periodontal dressing
may often be unnecessary or even undesirable after
periodontal flap procedures and may be usefully re-
placed by rinsing with chlorhexidine only (Sanz et al.
1989, Vaughan & Garnick 1989).
A commonly used periodontal dressing is Coe-
Pak
TM
(Coe Laboratories Inc., Chicago, IL, US), which
is
supplied in two tubes. One tube contains oxides of
various metals (mainly zinc-oxide) and lorothidol (a
fungicide). The second tube contains non-ionizing
carboxylic acids and chlorothymol (a bacteriostatic
agent). Equal parts from both tubes are mixed together
immediately prior to insertion. The setting time can be
prolonged by adding a retarder.
A light curing dressing, e.g. Barricaid
TM
(Dentsply
International Inc., Milford, DE, US), is useful in the
anterior tooth region and particularly following mu-
cogingival surgery, because it has a favorable esthetic
appearence and it can be applied without dislocating
the soft tissue. However, the light curing dressing is
not the choice of dressing to be used in situations
where the flap has to be apically retained, due to its
soft state before curing.
Cyanoacrylates have also been used as periodontal
dressings with varying success. Dressings of the cy-
anoacrylate type are applied in a liquid directly onto
the wound, or sprayed over the wound surface. Al-
though the application of this kind of dressing is
simple, its properties often do not meet clinical de-
mands, which is why its use is rather limited at pre-
sent.
Application technique
•
Ensure that bleeding from the operated tissues has
ceased before the dressing material is inserted.
•
Carefully dry teeth and soft tissue before the appli-
cation for optimal adherence of the dressing.
•
Moisten the surgical gloves to avoid the material
sticking to the fingertips.
•
When using the Coe-Pak
TM
' dressing material, the
interproximal areas are filled first. Thin rolls of the
dressing, adjusted in length to cover the entire field
of operation, are then placed against the buccal and
lingual surfaces of the teeth. The rolls are pressed
against the tooth surfaces and the dressing material
is forced into the interproximal areas. Coe-Pak
TM
may also be applied to the wound surfaces by
means of a plastic syringe. It is important to ensure
that dressing material is never introduced between
the flap and the underlying bone or root surface.
•
The surface of the dressing is subsequently
smoothed and excess material is removed with a
suitable instrument. The dressing should not cover
more than the apical third of the tooth surfaces.
Furthermore, interferences of the dressing with mu-
cogingival structures (e.g. the vestibular fold, fre-
nula) should be carefully checked to avoid displace-
ment of the dressing during normal function.
The light curing dressing (Barricaid
TM
) is preferably
applied with the supplied syringe, adjusted and then
550 • CHAPTER 25
cured by light. It is important to carefully dry teeth
and soft tissue before the application for optimal ad-
herence. Excess of dressing material can easily be
removed following the curing with a knife or finishing
burs in a low-speed handpiece.
Postoperative pain control
In order to minimize postoperative pain and discom-
fort for the patient, the surgical handling of the tissues
should be as atraumatic as possible. Care should be
taken during surgery to avoid unnecessary tearing of
the flaps, to keep the bone moistened and to ensure
complete soft tissue coverage of the alveolar bone at
suturing. With a carefully performed surgical proce-
dure most patients will normally experience only
minimal postoperative problems. The pain experience
is usually limited to the first days following surgery
and is of a level that in most patients can be adequately
controlled with normally used drugs for pain control.
However, it is important to recognize that the pain
threshold level is subjective and may vary between
individuals. It is also important to give the patient
information about the postsurgical sequence and that
uncomplicated healing is the common event. Further,
during the early phase of healing, the patient should
be instructed to avoid chewing in the area subjected
to surgical treatment.
Postsurgical care
Postoperative plaque control is the most important
variable in determining the long-term result of peri-
odontal surgery. Provided proper postoperative
plaque
control levels are established, most surgical treatment
techniques will result in conditions which favor the
maintenance of a healthy periodontium.
Although there are other factors
of
a more general
nature affecting surgical outcome (e.g. the systemic
status of the patient at time of surgery and during
healing), disease recurrence is an inevitable complica
-
tion, regardless of surgical technique used, in patients
not given proper postsurgical and maintenance care.
Since self-performed oral hygiene is often associ-
ated with pain and discomfort during the immediate
postsurgical phase, regularly performed professional
toothcleaning is a more effective means of mechanical
plaque control following periodontal surgery. In the
immediate postsurgical patient management self-per-
formed rinsing with a suitable antiplaque agent, e.g.
twice daily rinsing with 0.1-0.2% chlorhexidine solu-
tion, is recommended. Although an obvious disad-
vantage with the use of chlorhexidine is the staining
of teeth and tongue, this is usually not a deterrent for
compliance. Nevertheless, it is important to return to
and maintain good mechanical oral hygiene measures
as soon as possible. This is especially important since
rinsing with chlorhexidine, in contrast to properly
performed mechanical oral hygiene, is not likely to
have any influence on subgingival recolonization of
plaque.
Maintaining good postsurgical wound stability is
another important factor affecting the outcome of
some types of periodontal flap surgery. If wound sta-
bility is judged an important part of a specific proce-
dure, the procedure itself as well as the postsurgical
care must include measures to stabilize the healing
wound (e.g. adequate suturing technique, protection
from mechanical trauma to the marginal tissues dur-
ing the initial healing phase). If a mucoperiosteal flap
is replaced rather than apically repositioned, early
apical migration of gingival epithelial cells will occur
as a consequence of a break between root surface and
healing connective tissue. Hence, a maintained tight
adaptation of the flap to the root surface is essential
and one may therefore consider keeping the sutures
in place for a longer period of time than the 7-10 days
usually prescribed following standard flap surgery.
Following suture removal, the surgically treated
area is thoroughly irrigated with a dental spray and
the teeth are carefully cleaned with a rubber cup and
polishing paste. If the healing is satisfactory for start-
ing mechanical toothcleaning, the patient is instructed
in gentle brushing of the operated area using a tooth-
brush that has been softened in hot water. For cleaning
of the interdental area, toothpicks are prescribed. At
this early phase following the surgical treatment the
use of interdental brushes is abandoned due to the risk
of traumatizing the interdental tissues. Visits are
scheduled for supportive care at 2-week intervals to
closely monitor the patient's plaque control. During
this postoperative maintenance phase, adjustments of
the methods for optimal self-performed mechanical
cleaning are made depending on the healing status of
the tissues. Dictated by the patient's plaque control
standard, the time interval between visits for suppor-
tive care may gradually be increased.
OUTCOME OF SURGICAL
PERIODONTAL THERAPY
Healing following surgical pocket therapy
Gingivectomy
(Fig. 25-59): Within a few days following
excision of the inflamed gingival soft tissues coronal
to the base of the periodontal pocket, epithelial cells
start to migrate over the wound surface. The epi-
thelialization
of
the gingivectomy wound is usually
complete within 7 to 14 days following surgery
(
Engler et al. 1966, Stahl et al. 1968). During the follow
-
ing weeks a new dento-gingival unit is formed. The
fibroblasts in the supra-alveolar tissue adjacent to the
tooth surface proliferate (Waerhaug 1955) and new
connective tissue is laid down. If the wound healing
occurs in the vicinity of a plaque-free tooth surface, a
PERIODONTAL SURGERY: ACCESS THERAPY • 551
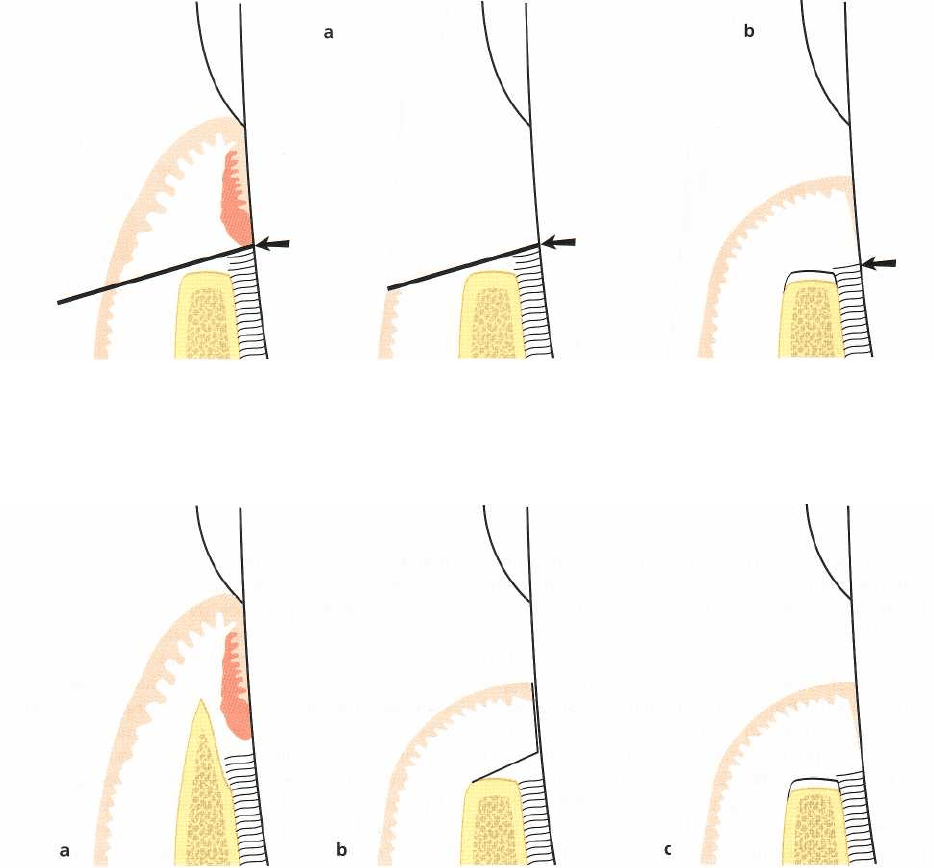
Fig. 25-59.
Gingivectomy.
Dimensional changes as a result of therapy. (a) The preoperative dimensions. The line indi
-
cates the location of the primary incision, i.e. the suprabony pocket is eliminated with the gingivectomy technique.
(b) Dimensions following proper healing. Minor resorption of the alveolar bone crest as well as some loss of connec
tive tissue attachment has occurred.
Fig. 25-60.
Apically repositioned flap.
Dimensional changes. (a) The preoperative dimensions. The broken line indi
-
cates the site from which the mucoperiosteal flap is reflected. (b) Bone recontouring has been completed and
the
flap repositioned to cover the alveolar bone. (c) Dimensions following healing. Minor resorption of the
marginal al
veolar bone has occurred as well as some loss of connective tissue attachment.
free gingival unit will form which has all the charac-
teristics of a normal free gingiva (Hamp et al. 1975).
The height of the newly formed free gingival unit may
vary not only between different parts of the dentition
but also from one tooth surface to another due to
primarily anatomical factors.
The re-establishment of a new, free gingival unit by
coronal regrowth of tissue from the line of the
"
gingivectomy" incision implies that sites with so-
called "zero pockets" only occasionally occur follow-
ing gingivectomy. Complete healing of the gingivec-
tomy wound takes 4-5 weeks, although the surface of
the gingiva may appear by clinical inspection to be
healed already after approximately 14 days (Ramfjord
et al. 1966). Minor remodeling of the alveolar bone
crest may also occur postoperatively.
The apically repositioned flap
(Fig. 25-60): Following
osseous surgery for elimination of bony defects and
the establishment of "physiologic contours" and repo-
sitioning of the soft tissue flaps to the level of the
alveolar bone, healing will occur primarily by first
intention, especially in areas where proper soft tissue
coverage of the alveolar bone has been obtained. Dur
-
ing the initial phase of healing, bone resorption of
varying degrees almost always occurs in the crestal
area of the alveolar bone (Ramfjord & Costich 1968).
The extent of the reduction of the alveolar bone height
resulting from this resorption is related to the thick-
ness of the bone in each specific site (Wood et al. 1972,
Karring et al. 1975).
During the phase of tissue regeneration and matu-
ration a new dento-gingival unit will form by coronal
growth of the connective tissue. This regrowth occurs
in a manner similar to that which characterized heal-
ing following gingivectomy.
The modified Widman flap
(Fig. 25-61): If a "modified
552 • CHAPTER 25
Fig. 25-61.
Modified Widman flap.
Dimensional changes. (a) The preoperative dimensions. The broken line indicates
the site from which the mucoperiosteal flap is reflected. (b) Surgery (including curettage of the angular bone de
-
fect) is completed with the mucoperiosteal flap repositioned as close as possible to its presurgical position. (c) Di
mensions following healing. Osseous repair as well as some crestal bone resorption can be expected during
healing
with the establishment of a "long" junctional epithelium interposed between the regenerated bone tissue
and the
root surface. An apical displacement of the soft tissue margin has occurred.
Widman flap" is carried out in an area with a deep
infrabony lesion, bone repair may occur within the
boundaries of the lesion (Rosling et al. 1976a, Poison
& Heijl 1978). However, crestal bone resorption is also
seen. The amount of bone fill obtained is dependent
upon (1) the anatomy of the osseous defect (e.g. a
three-walled infrabony defect often provides a better
mould for bone repair than two-walled or one-walled
defects), (2) the amount of crestal bone resorption, and
(3) the extent of chronic inflammation, which may
occupy the area of healing. Interposed between the
regenerated bone tissue and the root surface, a long
junctional epithelium is always found (Caton & Zan-
der 1976, Caton et al. 1980). The apical cells of the
newly formed junctional epithelium are found at a
level on the root that closely coincides with the pre-
surgical attachment level.
Soft tissue recession will take place during the heal
-
ing phase following a modified Widman flap proce-
dure. Although the major apical shift in the position
of the soft tissue margin will occur during the first 6
months following the surgical treatment (Lindhe et al.
1987), the soft tissue recession may often continue for
more than 1 year. Among factors influencing the de-
gree of soft tissue recession, besides the period for soft
tissue remodeling, are the initial height and thickness
of the supracrestal flap tissue and the amount of cre-
stal bone resorption.
Clinical outcome of surgical access therapy
in comparison to non-surgical therapy
Surgical treatment of periodontal lesions mainly
serves the purpose of (1) creating accessibility for
proper professional debridement of the infected root
surfaces and (2) establishing a gingival morphology
that facilitates the patient's self-performed plaque
control, in order to enhance the long-term preserva-
tion of the dentition. Hence, the amount of tooth loss
would be the most relevant criterion in an evaluation
of the relative importance of surgical access therapy
in the overall treatment of periodontal disease. How-
ever, since the rate of tooth loss is comparatively low,
this would require studies with extremely long peri-
ods of follow-up. Other criteria, such as resolution of
gingivitis (bleeding on probing), probing pocket
depth
reduction and clinical attachment level change,
have
therefore commonly been used to evaluate the
efficacy of periodontal therapy, even if these may only
be considered as surrogate end points. An additional
variable often of concern is gingival recession, since
this outcome variable may affect the patient's overall
appreciation of the treatment result. With regard to
changes in probing attachment levels, it should be
recalled that healing following conventional surgical
access therapy consistently results in the formation of
a junctional epithelium to a level on the root that
closely coincides with the presurgical attachment
level. Hence, when evaluating the outcome of various
therapeutic approaches the magnitude of
gain
of clini-
cal attachment may be of less importance since it
mainly is a measure of "pocket closure". Instead,
maintained probing attachment levels or further loss
should be focused on as the pertinent outcome vari-
able.
Pioneering contributions to the understanding of
the relative importance of the surgical component of
periodontal therapy were generated by the classic
longitudinal studies by the Michigan group (Ramfjord
and co-workers) and the Gothenburg group (Lindhe
and co-workers). Subsequently, several other clinical
research centers contributed with important data re-
garding the efficacy of surgical access therapy in corn-
PERIODONTAL SURGERY: ACCESS THERAPY • 553
Approximal tooth surfaces
Approximal tooth surfaces
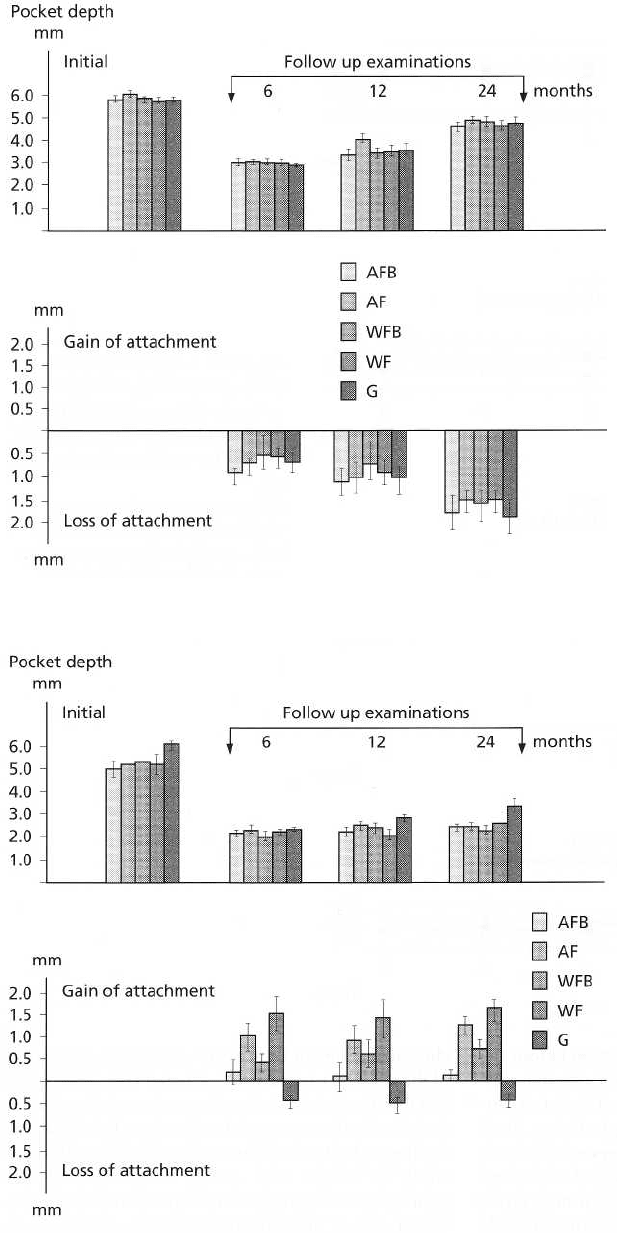
Fig. 25-62. Average
ap proximal
pocket depths at the initial exami-
nation and 6, 12 and 24 months af-
ter surgery (top) and alterations in
approximal
attachment levels from
the initial examination immediately
prior to surgery to the reex-
aminations 6, 12 and 24 months
postoperatively (bottom). Note
that
only areas with pockets which at
the initial examination had a depth
of 3 mm or more are
included in
the analysis. I = stan
dard error.
AFB = apically reposi
tioned flap
with bone recontour
ing. AF =
apically repositioned
flap. WFB =
modified Widman
flap with bone
recontouring. WF
= modified
Widman flap. G =
gingivectomy
including curettage
of bone defects. (
Data from Ny
man et al. 1977.)
Fig. 25-63. Average approximal
pocket depths at the initial exami-
nation and 6, 12 and 24 months af-
ter surgery (top), and alterations
in
approximal attachment levels
from
the initial examination imme
diately
prior to surgery to the re-
examinations 6, 12, and 24 months
postoperatively (bottom). Note
that
only areas with pockets which at
the initial examination
had a depth
of 3 mm or more
have been
included in the statistical analysis.
I = standard error.
AFB = apically
repositioned flap
and bone
correction. AF = apically
repositioned flap. WFB = Widman
flap and bone correction. WF =
Widman Flap. G = gingviectomy,
including curettage of the bony
defects. (Data from Rosling et al.
1976.)
parison to non-surgical periodontal therapy The topic
Plaque accumulation
has been extensively reviewed in several publications An important factor to consider in the evaluation of
(e.g. Kaldahl et al. 1993, Palcanis 1996) and some of the
the relative effect of the surgical component of peri-
general conclusions from these reviews will be high-
odontal therapy is the standard of postoperative
lighted below.
plaque control. Nyman et al. (1977) reported on a
clinical study in which the patients received only a
554 • CHAPTER 25
single episode of oral hygiene instruction before the
surgical treatment and no specific postoperative sup-
portive care. As a consequence both plaque and gin-
gival indices remained relatively high during the 2
years of postoperative follow-up. Independent of sur-
gical technique used, the patients showed a rebound
of pocket depths to more or less pretreatment levels
and further deterioration of clinical attachment levels
at both proximal and lingual tooth sites (Fig. 25-62). In
contrast, in a parallel study in which the patients
received repeated oral hygiene instructions and pro-
fessional tooth-cleaning once every 2 weeks during
the postoperative period (Rosling et al. 1976b), the
patients maintained the surgically reduced pocket
depth throughout the 2-year follow-up period and
clinical attachment level gains were observed for most
of the surgical procedures evaluated (Fig. 25-63). The
fact that the standard of postoperative oral hygiene is
decisive for the outcome of surgical pocket therapy is
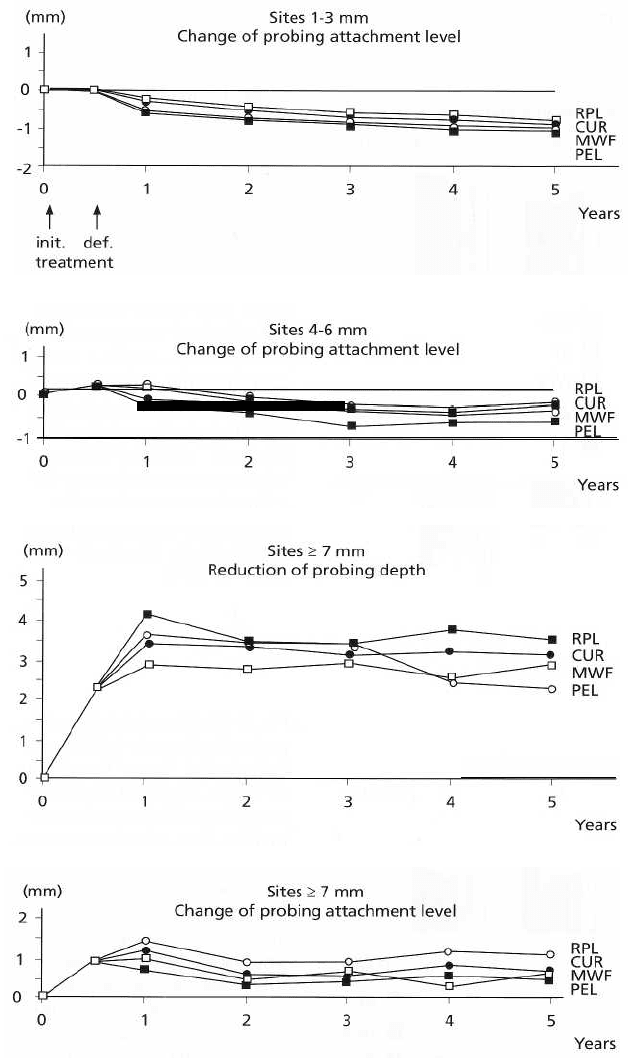
further underlined by data from a 5-year longitudinal
study by Lindhe et al. (1984), which showed that
patients with a high standard of plaque control main-
tained clinical attachment levels and probing depth
reductions following treatment more consistently
than
patients with poor plaque control. On the other
hand,
professional tooth cleaning including subgingi
val
scaling every 3 months may partly compensate for
the
negative effects of variations in self-performed
plaque
control (Ramfjord et al. 1982, Isidor & Karring
1986).
Fig. 25-64. Longitudinal evalu-
ation of four treatment modalities
in three categories of initial prob-
ing depth 1-3 mm, 4-6 mm and > 7
mm. RPL = scaling and root plan-
ing.
CUR = subgingival curettage.
MWF = Modified Widman Flap.
PEL = pocket elimination surgery.
(Data from Ramfjord et al. 1987,
presented by Egelberg 1995.)
