Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 40 HEMOSTASIS AND COAGULOPATHIES288
KEY POINTS: DIAGNOSIS AND TREATMENT
OF COAGULOPATHIES
1. Thrombocytopenia: Increased bleeding time, epistaxis, purpura, petechia, mucosal bleeding
(6 bags random donor platelets yields 30,000/mL increase)
2. PT and INR: Extrinsic and common paths—warfarin (i.e., II, VII, IX, X)
3. PTT: Intrinsic and common paths (all factors except VII and XIII)—heparin
4. For severe bleeding with hemophilia A, 50 U/kg factor VIII
5. FFP, 15 mL/kg (will support hemostasis until definitive diagnosis)
26. How does warfarin work? How do I deal with elevated INR?
Warfarin (an oral anticoagulant therapy [OAT]) inhibits the reduction of vitamin K to its active
form causing depletion of factors II, VII, IX, and X. Starting dose is 5 mg/day, with 4 to
5 days required for full anticoagulant effect. Heparin or LMWH is continued in the interim
due to the early inactivation of protein C and S, which causes a temporary procoagulant
effect. Target is usually an INR of 2 to 3. Significant bleeding occurs in 3% of patients on
chronic OAT. Drug interactions are common, and INR must be monitored. Head computed
tomography (CT) evaluation should be performed even in minor head trauma with
therapeutic dosing. Minor bleeding with elevated INR less than 5 can be treated by
withholding doses until INR returns to the desired range. The underlying need for
anticoagulation should be considered. Asymptomatic patients with an elevated INR may
receive oral vitamin K without significantly altering the ability to control anticoagulation.
Serious bleeding is treated with FFP (10–15 mL/kg) and 10 mg IV vitamin K, given slowly
(FFP for immediate effect; vitamin K effect takes several hours).
27. What’s new in antithrombotics?
Activated protein C. Sepsis causes a cascade of inflammation and coagulation with impaired
fibrinolysis. Microvascular hypoperfusion and organ dysfunction contribute to mortality.
Among its effects, activated protein C inactivates factors V and VIII inhibiting thrombosis and
promoting fibrinolysis. Early studies of activated drotrecogin alfa (Xigris), a recombinant
human activated protein C, showed a reduction in 30-day mortality in adult sepsis patients
with acute organ dysfunction who were at a high risk of death. However, its use remains
highly controversial within the critical care community.
28. What’s new in prothrombotics?
Recombinant activated factor VII (NovoSeven) is currently FDA approved for promoting
hemostasis in hemophiliacs with antibody inhibitors to coagulation factors VIII or IX. Although
it is also being used for a number of off-label uses in nonhemophilic patients, to date there
are not enough consistent high-level data to support its formal recommendation in these
situations.
29. Is it true they are close to developing safe and effective fake blood?
Development of a blood substitute has been a major goal of transfusion research groups for
many years. Advantages could include improved storage requirements and shelf-life, and
decreased antigen reactions and viral and bacterial contamination. Hemoglobin-based oxygen
carriers (HBOCs) had been developed in the 1980s and seem to have taken the lead over
perfluorocarbon blood substitutes. A number of agents have proceeded to clinical trials, many
of which have hit roadblocks due to adverse cardiovascular effects. Newer generations of
these substitutes are being developed to try to combat these issues. Despite more than a
decade of significant advances, much remains to be done.
Chapter 40 HEMOSTASIS AND COAGULOPATHIES 289
30. Is there anything we can do to help control massive hemorrhage from
trauma?
Holding pressure is the best way to start; but this is temporizing at best and not always
practical in situations of massive trauma and bleeding from noncompressible sites. The
military has been using new clotting agents to stabilize patients with traumatic bleeding on the
combat field. Quick Clot is a granulated mineral compound that can be poured directly into a
wound. It works by removing liquid substances and concentrating the clotting factors, thus
allowing a clot to form quickly. The HemCon bandage is made of chitosan, a substance with
mucoadhesive properties. It becomes extremely sticky when in contact with blood, and seals
the wound to control the bleeding. Although these two agents are already FDA approved for
civilian use, additional human studies are ongoing with a very promising dry fibrin-sealant
dressing. This dressing contains human fibrinogen, human thrombin, and calcium chloride,
but does not transmit human viruses as did older fibrin sealants. We should be seeing these
hemostatic agents more frequently in ambulances and hospitals in the near future.
BIBLIOGRAPHY
1. Ferguson E, Prowse C, Townsend E, et al: Acceptability of blood and blood substitutes. J Intern Med
263:244–255, 2008.
2. Hassan Y, Awaisu A, Aziz NA, et al: Heparin-induced thrombocytopenia and recent advances in its therapy.
J Clin Pharm Ther 32:535–544, 2007.
3. Hoffman, M: Therapeutic uses of recombinant coagulation factor VIIa. www.uptodate.com, 2008.
4. Houston G, Cuthbertson BH: Activated protein C for the treatment of severe sepsis. Clin Microbiol Infect
15:319–324, 2009.
5. Janz TG, Hamilton GC: Disorders of hemostasis. In Marx JA, Hockberger RS, Walls RM, et al, editors: Rosen’s
emergency medicine: concepts and clinical practice, ed 6, Philadelphia, 2006, Mosby, pp 1892–1906.
6. Pusateri AE, Holcomb JB, Kheirabadi BS, et al. Making sense of the preclinical literature on advanced
hemostatic products. J Trauma 60(3):674–682, 2006.
290
SICKLE CELL DISEASE
CHAPTER 41
Brad Talley, MD
1. What is sickle cell disease (SCD)?
SCD is a hereditary disorder that affects the structure and function of hemoglobin, the protein in
red blood cells that is responsible for oxygen delivery to tissues in the body. The sickle
hemoglobin (Hemoglobin S [HbS]) differs from the normal hemoglobin (Hemoglobin A [HbA])
by a single amino acid substitution—valine for glutamine—at the sixth position on the
b-globulin chain of the hemoglobin molecule. This substitution causes abnormal polymerization
of HbS when it is deoxygenated, resulting in sickle-shaped, nondeformable red blood cells that
cannot traverse small capillaries. These sickle cells are responsible for the vaso-occlusive
phenomena and hemolysis that are the hallmarks of the disease.
2. What is sickle cell trait?
SCD is an autosomal recessive disorder. Therefore, patients who are heterozygous for the
sickle cell gene (HbSA) are said to have sickle cell trait, whereas patients who are
homozygous for the sickle cell gene (HbSS) are said to have SCD. Unlike homozygous
individuals, patients with sickle cell trait have a normal life span and are generally
asymptomatic.
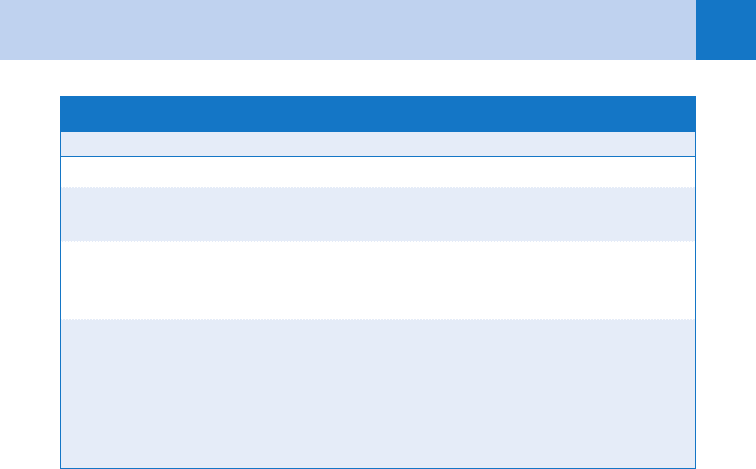
3. Are there sickle cell variants?
Hemoglobin C and b-thalassemia are abnormal hemoglobins that create hemolytic
anemias of their own. Hemoglobin C (HbC) is an inherited abnormal b-chain, which when
combined with the sickle cell gene produces a less severe form of SCD known as HbSC.
b-thalassemia is also an inherited abnormal b-chain. When combined with a copy of the
sickle cell gene, the clinical presentation of the disease can range from a mild to severe
form of SCD depending on the quantity of hemoglobin A. Table 41-1 summarizes the
spectrum of SCD.
4. What causes red blood cells to sickle?
The rate and extent of polymer formation in a circulating HbS red cell depend primarily on three
independent variables: the cell’s degree of deoxygenation, the intracellular hemoglobin
concentration, and the presence or absence of hemoglobin F (fetal hemoglobin). Any factors that
promote global or local hypoxia, such as circulatory stasis, cardiovascular disease, pulmonary
disease, and high altitude, can cause sickling. Low temperature promotes sickling through
vasoconstriction. Acidosis also promotes sickling, as does radiographic contrast dye. The
presence of hemoglobin F in a red blood cell prevents sickling.
5. How common is SCD?
In the United States, 1 of every 600 people of African descent is born with SCD.
Approximately 8% are heterozygous for the sickle cell gene. The prevalence is increasing in
the United States, due to both population growth and improved longevity of patients with SCD.
Mortality rates for children with SCD have declined with the advent of newborn screening
programs, education initiatives for parents, antibiotic prophylaxis, and Haemophilus influenzae
and Streptococcus pneumoniae vaccination. Despite these improvements in the care provided,
the median age at death is 42 years for men and 48 years for women.
Chapter 41 SICKLE CELL DISEASE 291
6. What are the typical baseline laboratory findings in patients with SCD?
Because sickle cells have a shorter life span than normal red blood cells (17 days vs. normal
120 days), most patients will have a mild to moderate anemia with a hematocrit of 20% to
30% and a reactive reticulocytosis of 3% to 15%. The white blood cell count, platelet count,
and alkaline phosphatase levels are usually elevated. Mean bilirubin levels and lactate
dehydrogenase levels are also elevated, whereas serum haptoglobin levels are low, secondary
to early red cell death. Creatinine and electrolyte levels are generally normal.
7. What causes vaso-occlusion (pain) crisis?
Vaso-occlusion typically causes recurrent painful episodes (previously called sickle cell crisis)
that can result in a variety of serious organ system complications. There is a high degree of
clinical heterogeneity among patients who experience vaso-occlusion episodes. The
pathophysiology is poorly understood, but it is thought to be a combination of poorly pliable
sickled red blood cells, modified vascular endothelium, and an inflammatory response
involving leukocytes, platelets, and plasma proteins that result in microvascular occlusion. The
vaso-occlusion episode typically manifests as pain that can affect any part of the body and can
last from days to weeks at time. Many episodes are accompanied by objective clinical signs
such as low-grade fever, swelling, tenderness, tachypnea, hypertension, nausea, and vomiting.
Standard laboratory testing is not helpful in identifying vaso-occlusion crisis.
8. How should vaso-occlusive (pain) crisis be managed?
Vaso-occlusive (pain) crises are the most frequent reason patients with SCD seek medical
attention. These patients should be managed with oral (in mild cases) or intravenous
rehydration and analgesics. Pain is often undertreated because many physicians are not
familiar with the pharmacology of analgesia or are overly concerned with the potential for
addiction. If pain is refractory to treatment, the patient should be admitted.
9. What causes an acute or worsening anemia in sickle cell patients?
n
Sequestration crisis occurs when large numbers of red blood cells pool in the spleen due
to their abnormal shape and stiffness. Patients present with splenic enlargement,
abdominal pain, a falling hematocrit, pallor, tachycardia, and dyspnea. Massive
sequestration can lead to hypovolemic shock and death. This usually occurs between the
ages of 5 months and 2 years because by 2 years of age the spleen is typically
Hb, hemoglobin; HbSC, hemoglobin S and hemoglobin C; SCD, sickle cell disease.
Disease Genetics Clinical Severity
SCD Two copies of sickle cell gene Most severe
Sickle cell trait One copy of sickle cell gene,
other Hb gene is normal
Usually asymptomatic with a
normal life span
HbSC disease One copy of sickle cell gene,
one of Hb C gene
Less severe symptoms, life
span is approximately 20 years
longer than in SCD
Sickle cell-b-thalassemia One copy of sickle cell gene,
one of b-thalassemia gene
20% have symptoms as severe
as those with SCD; 80% have
less severe symptoms
TABLE 41–1. THE SPECTRUM OF SCD
Chapter 41 SICKLE CELL DISEASE292
autoinfarcted and fibrosed due to multiple vaso-occlusive events. It is the most dangerous
crisis for young children, with a mortality of 10% to 15%. Splenectomy is usually
recommended after the first event.
n
Aplastic crisis is caused by a transient arrest of erythropoiesis, characterized by a
decreased hematocrit and depressed reticulocyte count resulting in fatigue, dyspnea, and
pallor. It is frequently the result of an infection, with parvovirus B19 being the most
common precipitant. Most patients require acute transfusion therapy and reticulocytes
typically reappear within 2 to 14 days.
n
Hemolytic crisis usually occurs in response to infection or drugs, resulting in a more rapid
rate of hemolysis. A rapidly falling hematocrit, an elevated reticulocyte count, pallor, and
jaundice are observed. Patients with glucose 6-phosphate dehydrogenase (G6PD)
deficiency are even more prone to hemolysis and hypoxia. It can be precipitated by certain
foods (e.g., fava beans) and medications (e.g., aspirin and sulfonamides).
10. What treatments are available for SCD?
Because a definitive cure is not currently available for most patients, treatment is aimed largely
at symptom control during vaso-occlusive episodes. In the acute care setting, the goal is to
stop the cycle of deoxygenated sickling and microvascular sludging. Therapies include rest,
hydration, and analgesia. Transfusion and antibiotic therapy for infection are also indicated in
some cases. Hydroxyurea is the only FDA-approved therapy and works by increasing fetal
hemoglobin levels. Fetal hemoglobin alters the dynamics of HbS polymerization, thereby
decreasing the rates of vaso-occlusive crisis, acute chest syndrome (ACS), and transfusion.
However, long-term effects (mutagenic and carcinogenic properties) of prolonged hydroxyurea
are unknown. Bone marrow transplantation has been successful in a limited number of children
and may possibly provide a cure for SCD, but the experience is quite limited and long-term
outcomes are unknown. Patient selection, along with the risks of the procedure, are also
important factors still being researched. Gene therapy is still experimental but may have the
potential to cure SCD. Other experimental medical therapies include nitric oxide, which directly
inhibits polymerization of HbS; butyric acid, which modulates gene expression of Hemoglobin
F; and clotrimazole, which modifies the cellular dehydration that worsens cell sickling.
11. Do cerebrovascular accidents (CVAs) occur in SCD?
Yes. Children with SCD carry a 300-fold increased risk for stroke, making it the most common
cause of childhood stroke. By age 20, 10% to 20% of patients with SCD will have experienced
a clinical stroke syndrome, and a further 17% to 22% will have subclinical evidence of
cerebral infarction on brain magnetic resonance imaging (MRI). The mean age of onset of CVA
is 10 years. Of patients with CVA, 67% will suffer another, usually within 36 months. The
incidence of stroke in children has been decreasing by prophylactic transfusions and regular
transcranial Doppler studies for children at risk.
KEY POINTS: INDICATIONS FOR ADMISSION OF PATIENTS
WITH SCD
1. Pain not controlled with oral medications
2. Unable to hydrate orally
3. Neurologic findings
4. Pulmonary findings (e.g., hypoxia, infiltrate on chest X-ray, new rales)
5. Sequestration crisis
6. Aplastic crisis
7. Fever (If .40°C, toxic appearing, or poor follow-up)
Chapter 41 SICKLE CELL DISEASE 293
12. Is there a role for blood transfusion in SCD?
Simple transfusion is appropriate for single transfusions to restore oxygen-carrying capacity
or blood volume. Partial exchange transfusions are required in emergencies and in the setting
of chronic transfusions. Transfusion therapy to prevent or treat pain is controversial because
of the risk of iron overload and alloimmunization. Hemoglobin concentration should not be
raised above 10g/dL because of increases in blood viscosity and the risk of vaso-occlusive
episodes.
KEY POINTS: INDICATIONS FOR CONSIDERATION
OF TRANSFUSION IN PATIENTS WITH SCD
1. Aplastic crisis
2. Sequestration crisis
3. ACS
4. CVA
5. Prior to major surgery
6. Acute multiorgan failure
7. Pregnancy
8. Priapism
13. What is ACS?
ACS (acute chest syndrome) is defined as a new pulmonary infiltrate on chest radiograph
accompanied by either fever (.38.5°C), chest pain, cough, wheezing, or tachypnea. ACS
often develops after a vaso-occlusive crisis and is a leading cause of hospitalization and death
in SCD.
14. What causes ACS?
Infection, fat embolism, rib infarction, thromboemboli, reactive airway disease, fluid overload,
and atelectasis due to splinting can cause ACS. Regardless of the root cause, the final
common pathway in the pathogenesis of ACS is small-vessel vaso-occlusion, infarction, and
inflammation with alveolar wall necrosis. In a vicious cycle, these factors lead to regional
hypoxemia and acidosis, which in turn causes increased sickling and sludging.
15. How should ACS be managed?
If ACS is suspected after a thorough history and physical, a complete blood count, reticulocyte
count, blood cultures, and chest X-ray should be ordered. Sputum cultures may also be of
use in this population. If ACS is diagnosed, the patient should be admitted and treated with
intravenous hydration, antibiotics, analgesics, and aggressive pulmonary toilet. Early treatment
with broad-spectrum antibiotics, which should include a third-generation cephalosporin to
cover S. pneumoniae, H. influenza, and Klebsiella pneumonia and a macrolide to cover
Mycoplasma pneumoniae and Chlamydia pneumoniae, are recommended until culture results
are available. In many cases, exchange transfusion is indicated to lower the concentration of
HbS. Those who present with severe anemia, thrombocytopenia, or multilobar pneumonia
should receive a transfusion before respiratory distress develops. Early aggressive ventilatory
support is mandatory.
Chapter 41 SICKLE CELL DISEASE294
16. How should a patient with SCD be managed when he or she presents with
fever?
Patients with SCD are functionally asplenic, so they are at increased risk for serious bacterial
infection, especially with encapsulated organisms (S. pneumonia and H. influenza). Fever in
children should be considered a medical emergency, requiring a thorough search for the
source, blood cultures, and empiric antibiotics. The clinician should also have a low threshold
for admitting adults and administering empiric antibiotics. One approach is to divide patients
into two categories:
n
High risk: Patients with SCD or sickle cell-b-thalassemia who appear toxic, have
temperature .40°C, or are not receiving prophylactic penicillin. Admit for intravenous
ceftriaxone.
n
Low risk: Patients with SCD or sickle cell-b-thalassemia who appear to be well, have
temperature ,40°C, and are taking prophylactic penicillin; or patients with HbSC who have
temperatures .38.5°C. Obtain blood cultures, observe for several hours in the ED,
administer ceftriaxone, and arrange follow-up within 24 hours.
17. How is bone infarction differentiated from osteomyelitis in SCD?
It is extremely challenging. Both entities cause bone pain and fever. In attempting to make the
diagnosis, fever greater than 38.4°C may indicate osteomyelitis, although this cutoff is
imperfect. A presentation of multifocal, rather than unifocal, bone pain is more consistent with
bone infarction. The absence of leukocytosis or elevated erythrocyte sedimentation rate (ESR)
may also suggest infarction. Although positive cultures of bone can diagnose osteomyelitis, a
period of at least 48 hours is required to process them, and sensitivity is not 100%. The
leading cause of osteomyelitis is Salmonella, followed by Staphylococcus aureus. Plain
radiographs, contrast-enhanced computed tomography (CT) scan, MRI, and radio nucleotide
bone scans have all had disappointing results. Therefore, antibiotics are recommended for all
patients with fever and bone pain until osteomyelitis can be ruled out.
18. What other important clinical complications can occur with SCD?
Vaso-occlusion in the skin can cause frequent leg ulcers and myofascial syndromes in
patients with SCD. Hepatobiliary complications are common with patients often having
chronic cholelithiasis secondary to pigmented gallstones. Iron overload can occur in patients
requiring frequent transfusions. Males with SCD often present to the ED with priapism.
Retinal complications can occur, including proliferative retinopathy, retinal artery occlusion,
and retinal detachment and hemorrhage. Patients with SCD can experience renal insufficiency
from vaso-occlusion of the vasa recta capillaries in the renal medulla. Patients with SCD are
also at increased risk for developing pulmonary hypertension.
19. Are pregnant patients with SCD at an increased risk of complications?
Yes. Pregnancy is associated with both fetal and maternal complications related to
compromised placental blood flow. The fetus is at risk for spontaneous abortion, preterm
labor, intrauterine growth restriction, and low birth weight, whereas pregnant females are at
risk for cerebral vein thrombosis, pneumonia, pyelonephritis, deep venous thrombosis,
postpartum infection, and sepsis. They are also more likely to undergo cesarean delivery, to
experience pregnancy-related complications (such as hypertension, pre-eclampsia/eclampsia,
abruption, and antepartum bleeding) and to have cardiomyopathy or pulmonary hypertension.
Close maternal-fetal surveillance is warranted.
Chapter 41 SICKLE CELL DISEASE 295
BIBLIOGRAPHY
1. Bernard AW, Yasin Z, Venkat A: Acute chest syndrome of sickle cell disease. Hospital Physician 44:15–23, 2007
2. Bunn HF: Mechanisms of disease: pathogenesis and treatment of sickle cell disease. N Engl J Med 337:
762–769, 1997.
3. Conran N, Franco-Penteado CF, Costa FF: Newer aspects of the pathophysiology of sickle cell disease
vaso-occlusion. Hemoglobin 33(1):1–16, 2009.
4. Embury SH, Vichinsky EP: Overview of the management of sickle cell disease. UpToDate, version13.1, June
2009, www.uptodate.com/online/content/topic.do?topicKey5red_cell/22897&view.
5. Hoppe C: Defining stroke risk in children with sickle cell anaemia. Br J Haematol 128:751–766, 2005.
6. Minter KR, Gladwin MT: Pulmonary complications of sickle cell anemia. Am J Respir Crit Care Med 164:
2016–2019, 2001.
7. Vichinsky EP, Neumayr LD, Earles A, et al: Causes and outcomes of the acute chest syndrome in sickle cell
disease. N Engl J Med 342:1855–1865, 2000.
8. Vichinsky EP: Overview of the clinical manifestations of sickle cell disease. UpToDate, version 17.2, May
2009, www.utdol.com/online/content/topic.do?topicKey5red_cell/24936&view.
9. Villers MS, Jamison MG, DeCastro LM, et al: Morbidity associated with sickle cell disease in pregnancy.
Am J Obstet Gynecol 199:125.e1–125.e5, 2008.
10. West MS, Wethers D, Smith J, et al: Laboratory profile of sickle cell disease: a cross-sectional analysis.
The Cooperative Study of Sickle Cell Disease. J Clin Epidemiol 45:893–909, 1992.
11. Wong AL, Sakamoto KM, Johnson EE: Differentiating osteomyelitis from bone infarction in sickle cell disease.
Pediatr Emerg Care 17:60–63, 2004.
KEY POINTS:
1. Patients with SCD have functional asplenia and therefore are at an increased risk for bacterial
infections, in particular encapsulated organisms. Initiate broad-spectrum antibiotics for sus-
pected bacterial infections.
2. Patients with vaso-occlusion crisis are often undertreated for pain.
3. Diagnosis of uncomplicated vaso-occlusive pain crisis is one of exclusion and can only be
made after all other causes of pain and precipitating events have been ruled out first.
ACKNOWLEDGMENT
The editors gratefully acknowledge the contributions of Kurt Whitaker, MD, author of this chapter in
the previous edition.
296
ONCOLOGIC EMERGENCIES
CHAPTER 42
Nicholas J. Jouriles, MD
1. What is an oncologic emergency?
An oncologic emergency is a life- or limb-threatening problem in a patient with an underlying
neoplasm. These problems may be caused by the cancer, its systemic effects, or by
therapeutic interventions against the cancer. There may also be psychosocial issues.
2. Is this important in the ED?
Yes. Cancer is the second leading cause of death in the United States. It is also
second only to trauma in years of potential life loss. In addition, as cancer treatments
improve, we will see an ever-increasing number of ED patients with oncologic
emergencies.
3. Name several oncologic emergencies.
See Table 42-1.
4. Which of the entities on this list are life- or limb-threatening?
The life-threatening diseases are those that can lead to shock or death. They can be
divided into the standard categories of shock: volume loss (bleeding) or impaired vascular
return (superior vena cava syndrome [SVCS]); pump impairment (cardiac tamponade); and
derangement of systemic vascular resistance (sepsis). There are serious metabolic
derangements (hypercalcemia) and disabling neurologic problems (spinal cord
compression [SCC]).
5. Tell me about these.
n
SVCS: Caused by obstruction of the superior vena cava. Although it may be caused by
mediastinitis or aortic aneurysms, most cases are caused by a neoplastic process. Lung
cancer is the most common, usually the small cell or squamous types. Adenocarcinoma of
the breast and lymphoma are also common. SVCS may also occur secondary to metastatic
lesions from distant primary sites. Diagnosis is clinical and is verified by imaging.
Treatment usually involves radiation therapy, but chemotherapy and endovascular stenting
are also options.
n
Cardiac tamponade: Usually occurs secondary to metastatic disease of the
pericardium. It has been found in 2% to 21% of patients dying of cancer (Fig. 42-1).
Patients with cardiac tamponade usually have a large tumor burden and a poor
6-month survival. The diagnosis of a malignant cardiac effusion with tamponade is
suspected clinically in the hypotensive patient with muffled heart sounds, elevated
neck veins, and an enlarged cardiac silhouette on chest X-ray. It is most commonly
seen in lung and breast carcinomas and lymphoma. Treatment involves pericardial
drainage. ED bedside ultrasound is the best way to make the diagnosis and to guide
drainage.
n
Infections: Because all patients with tumors are by definition immunocompromised, the
variety of potential infections is unlimited. Immune status may be further compromised by
chemotherapeutic agents. When patients become neutropenic—total neutrophil count less
than 500—any type of infection may occur. This includes bacterial, viral, or fungal
Chapter 42 ONCOLOGIC EMERGENCIES 297
DNR, do not resuscitate; GI, gastrointestinal; SIADH, syndrome of inappropriate secretion
of antidiuretic hormone.
Airway compromise
Head and neck mass
Tracheal compression
Adrenal crisis
Primary tumor
Metastatic lesion
Anemia
Bone marrow replacement with tumor
Chemotherapy effects
Bleeding
Primary mass
Low platelet count
Abnormal clotting factors secondary
to liver metastases
Carcinoid syndrome
Complications of chemotherapy
Bone marrow suppression
Cardiac toxicity
GI toxicity
Pulmonary toxicity
Renal toxicity
Graft vs. host disease
Hemorrhagic cystitis
Chemotherapy induced
Radiotherapy induced
Hyperviscosity syndrome
Infection
With neutropenia
Postobstructive pneumonia
Intestinal obstruction
Intestinal perforation
Malignant pericardial effusion
with tamponade
Metabolic abnormalities
Hypercalcemia
Acute tumor lysis syndrome
Hyponatremia/SIADH
Hyperuricemia
Hypoglycemia
Obstructive jaundice
Obstructive uropathy
Pain
Complications of radiotherapy
Dermatitis
GI toxicity
Emotional stress
Death and dying
DNR orders
Family issues
Seizures
Spinal cord compression
Motor/sensory loss
Incontinence
Back pain
Superior vena cava syndrome
Tinnitus
TABLE 42–1. EMERGENCIES IN PATIENTS WITH UNDERLYING NEOPLASTIC DISEASES
(PARTIAL LIST)
infections that can lead to septic shock, adult respiratory distress syndrome, and death.
The neutropenic febrile patient should be placed in isolation and treated with broad-
spectrum antibiotics.
n
Hypercalcemia: Occurs in up to 30% of patients with cancer. Neoplasms that lead to
metastatic involvement of the skeletal system are commonly associated with
hypercalcemia. Common presenting signs are lethargy, constipation, and altered mental
status. Treatment involves hydration with normal saline and bisphosphates, such as
pamidronate.
