Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 62 ACUTE RESPIRATORY DISORDERS IN CHILDREN438
Step 5. Admission criteria
n
Albuterol treatment required every 2 hours or more.
n
Continued hypoxemia by pulse oximetry.
n
Continued poor response requiring escalation of treatment.
25. What about magnesium?
The mechanism of action of IV magnesium is not known but is hypothesized to be the
counteraction of calcium ions to prevent bronchial smooth muscle contraction. The benefit in
patients with mild to moderate exacerbations is unclear, and its use should be reserved for
those patients in severe distress or nonresponsive to albuterol and steroids. Dose is 75 mg/kg
IV (maximum of 2 g).
26. Does aminophylline have any use?
Aminophylline and theophylline do not have a role in the routine management of the pediatric
asthma patient in the ED. IV aminophylline has been shown to improve lung function in
children with severe asthma exacerbations, but it does not reduce symptoms, number of
nebulizer treatments, or length of stay. Several studies have failed to show benefit of
theophylline when added to bronchodilators and steroids in noncritically ill patients. There are
inconclusive data to suggest that theophylline may be equally effective to terbutaline in
pediatric intensive care unit (PICU) patients.
27. What about parenteral b-agonists?
Use of systemic b-agonists is controversial; few well-designed studies have evaluated their use.
They should be considered in patients with severe exacerbations who have failed to respond to
maximal inhaled therapy. Terbutaline, subcutaneously or intravenously, may be given as an initial
bolus of 10 mg/kg followed by a continuous infusion starting at 0.5 mg/kg/min. Epinephrine may
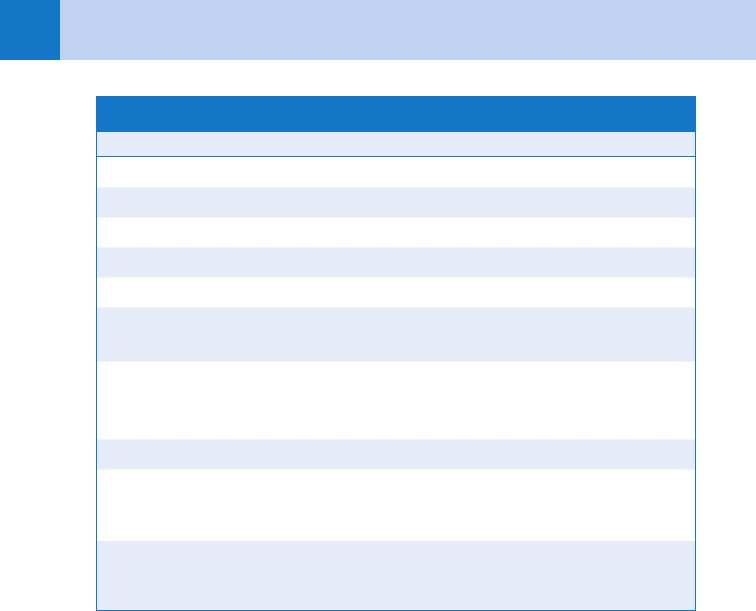
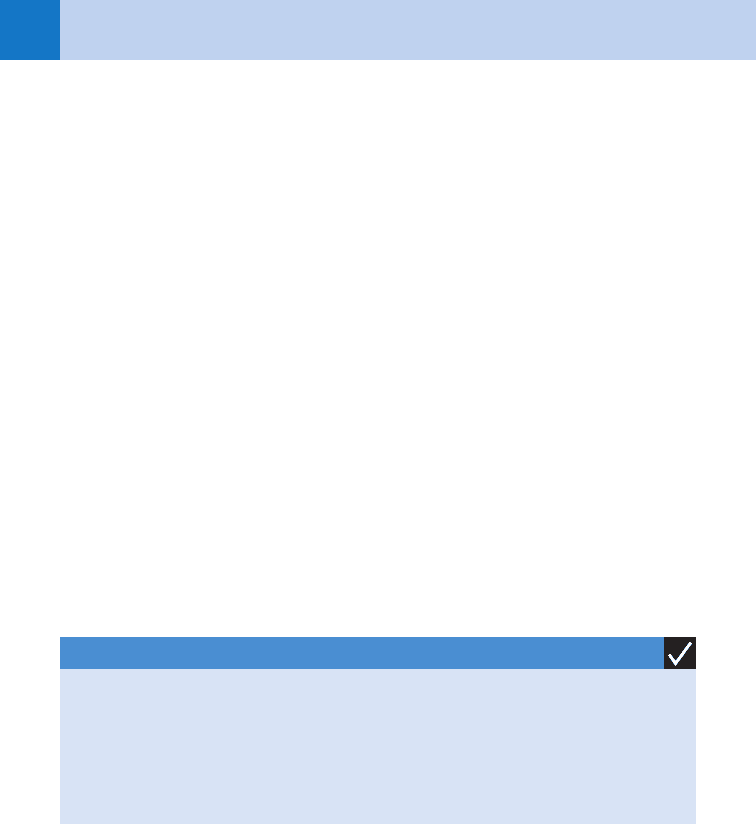
Score 1 2 3
Resp Rate
2–3 y #34 35–39 40
4–5 y #30 31–35 36
6–12 y #26 27–30 31
.12 #23 24–27 28
Oxygen
requirement
.90% on room air 85%–90% on room
air
,85% on room air
Auscultation Normal or end-
expiratory wheeze only
Expiratory wheezes Inspiratory/Expiratory
wheezes or decreased
breath sounds
Retractions 0–1 site 2 sites 31 sites
Dyspnea Speaks in sentences,
coos, babbles
Speaks in partial
sentences, short cry
Single words, short
phrases, grunting
Table 62-3. PEDIATRIC ASTHMA SCORE
Modified from Kelly CS, Anderson CL, Pestian JP, et al: Improved outcomes for hospitalized asthmatic
children using a clinical pathway. Ann Allergy Asthma Immunol 84:509–516, 2000.
Chapter 62 ACUTE RESPIRATORY DISORDERS IN CHILDREN 439
BIBLIOGRAPHY
1. Beers SL, Abramo TJ, Bracken A, et al: Bilevel positive airway pressure in the treatment of status asthmaticus
in pediatrics. Am J Emerg Med 25:6–9, 2007.
2. Bjornson CL, Klassen TP, Williamson J, et al: A randomized trial of a single dose of oral dexamethasone for
mild croup. N Engl J Med 351:1306–1313, 2004.
3. Dobrovoljac M, Geelhoed GC: An update highlighting the effectiveness of 0.15 mg/kg of dexamethasone.
Emerg Med Australas 21:309–314, 2009.
4. Greenberg RA, Kerby G, Roosevelt GE: A comparison of oral dexamethasone with oral prednisone in pediatric
asthma exacerbations treated in the emergency department. Clin Pediatr 47:817–823, 2008.
5. Hartling L, Wiebe N, Russell K, et al: A meta-analysis of randomized controlled trials evaluating the efficacy of
epinephrine for the treatment of acute viral bronchiolitis. Arch Pediatr Adolesc Med 157:957–964, 2003.
6. King VJ, Viswanathan M, Bordley WC, et al: Pharmacologic treatment of bronchiolitis in infants and children:
A systematic review. Arch Pediatr Adolesc Med 158:127–137, 2004.
7. Mitra A, Bassler D, Goodman K, et al: Intravenous aminophylline for acute severe asthma in children over two
years receiving inhaled bronchodilators. The Cochrane Library, Vol. 3, 2005.
8. Rowe BH, Bretzlaff JA, Bourdon C, et al: Magnesium sulfate for treating exacerbations of acute asthma in the
emergency department. The Cochrane Library, Vol. 3, 2005.
9. Subcommittee on the diagnosis and management of bronchiolitis. Pediatrics 118:1774–1793, 2006.
10. Wagner T: Bronchiolitis. Pediatr Rev 10:386–394, 2009.
11. Wheeler DS, Jacobs BR, Kenreigh CA, et al: Theophylline versus terbutaline in treating critically ill children
with status asthmaticus: a prospective, randomized, controlled trial. Pediatr Crit Care Med 6:142–147, 2005.
12. Zhang L, Mendoza-Sassi RA, Wainwright C, et al: Nebulized hypertonic saline for acute bronchiolitis in infants.
The Cochrane Library, Vol 4, 2008.
also be given subcutaneously. These medications, which should not interrupt inhaled therapy,
require monitoring of cardiac function and serum potassium levels.
28. What should I do if my patient is going into respiratory failure?
Consider treatment with magnesium, terbutaline, and epinephrine. Bilevel positive airway
pressure (BiPAP; set initially at 10/5) has been shown in small studies to improve respiratory
rate and oxygenation in children. If intubation is necessary, ketamine (in conjunction with a
paralytic) stimulates the release of catecholamines causing bronchodilation, making it the
inductive agent of choice (dose: 1-2 mg/kg IV). To optimize oxygenation and prevent
barotrauma, initial ventilator settings should be set to a reduced rate of 8 to 12 breaths
per minute, allowing for permissive hypercapnia.
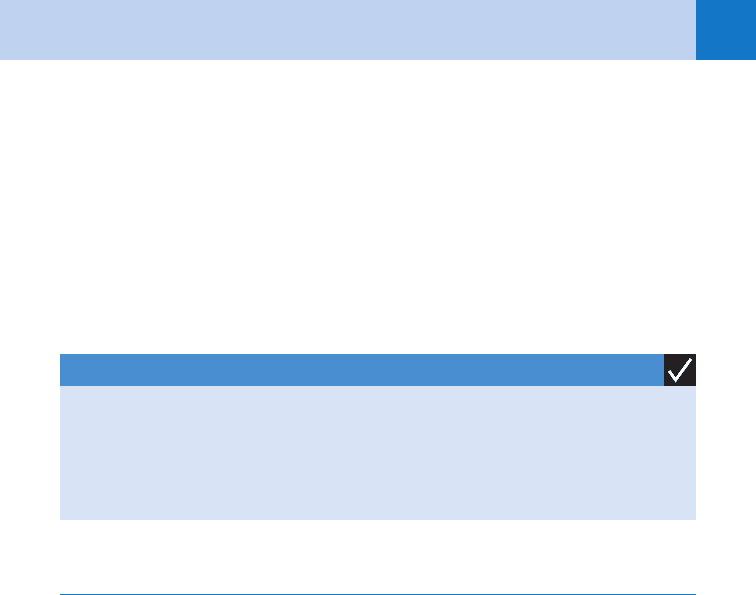
KEY POINTS: EVALUATION OF RESPIRATORY DISORDERS
1. Observation prior to auscultation helps to localize and differentiate etiologies of pediatric
respiratory complaints.
2. Foreign bodies should be suspected in any child presenting with signs of airway obstruction.
3. Labs and radiographs are not routinely indicated in many childhood respiratory disorders.
440
PEDIATRIC GASTROINTESTINAL DISORDERS
AND DEHYDRATION
CHAPTER 63
Joshua S. Easter, MD
1. What are the common causes of abdominal pain in children?
Abdominal pain is a common pediatric complaint, the differential for which is guided by age of
the patient, history, and physical examination with or without diagnostic studies (Table 63-1).
2. Can you determine if a child is dehydrated based on the history and physical
examination?
Historical factors, such as the number of wet diapers, frequency of vomiting or diarrhea, and
amount of oral intake, should be used in conjunction with other physical signs to assess
dehydration. The presence of sunken eyes, dry mucous membranes, cool extremities, weak
pulses, decreased tears, increased heart rate, and sunken fontanelle are often unreliable.
Capillary refill time (normally less than 2 seconds), skin turgor, and hyperpnea are better
indicators of severe dehydration.
3. How do you manage the different levels of dehydration?
n
Mild or moderate dehydration: Oral rehydration is the ideal treatment. Using the World
Health Organization (WHO) solution or Pedialyte, the patient drinks 50 to 100 (mL/kg) over
4 hours in the form of 5 mL aliquots administered via a medicine dropper or syringe every
5 minutes. An alternate and more simplified strategy involves administration of 1 mL/kg
every 5 minutes for 4 hours. If the child vomits, wait 15 minutes and try again. These
regimens have similar success rates to intravenous hydration and shorter times to initiation
of therapy and shorter ED length of stay.
n
Severe dehydration or patients failing oral rehydration: These children are ill appearing
and should receive intravenous fluids. They often require multiple 20-mL/kg boluses to
compensate for their dehydration. By avoiding fatty acid breakdown and ketosis, dextrose
containing fluids may lead to more rapid improvement in vomiting than normal saline.
4. How are maintenance fluids determined in a child?
Maintenance fluids per hour are calculated based on weight in kilograms using the 4-2-1 rule:
4 mL/kg for the first 1 to 10 kg, an additional 2 mL/kg for the next 11 to 20 kg, and 1 mL/kg
for every additional kg.
5. What are potential causes of vomiting without diarrhea in children?
The differential includes early gastroenteritis, urinary tract infection, appendicitis, diabetic
ketoacidosis, otitis media, pneumonia, strep pharyngitis, testicular or ovarian torsion,
meningitis, and head injury.
6. How do you differentiate between gastroenteritis and more severe abdominal
pathology?
This may be difficult and often requires a period of observation in the ED for other developing
signs or symptoms. Focal tenderness in the abdomen makes gastroenteritis less likely.
7. What diagnostic studies should be obtained on children with gastroenteritis?
Most require no tests. Infants with prolonged or severe symptoms can deplete their
glycogen stores and therefore should have a bedside glucose test. Electrolyte studies,
Chapter 63 PEDIATRIC GASTROINTESTINAL DISORDERS AND DEHYDRATION 441
looking for hypernatremia or renal insufficiency, may be considered for ill-appearing
children. In the setting of hypoglycemia, the infant or child should be given 4 mL/kg of
dextrose 10% (if younger than 3 months old) or 2 mL/kg of dextrose 25% (if more than
3 months old).
8. How do you differentiate between bacterial and viral causes of diarrhea?
n
Viruses cause the majority of diarrhea in children, with rotavirus the most common agent
in younger children and Norwalk virus in older children. Viral diarrhea tends to produce
voluminous watery diarrhea with diffuse abdominal cramping.
n
Bacterial diarrhea typically causes lower abdominal pain and bloody or mucousy stool.
However, these history and physical examination findings cannot reliably differentiate bacterial
from viral diarrhea. Stool cultures should be obtained in patients with significant
comorbidities, ill appearance, high fever, bloody stools, severe cramping, recent antibiotic use,
travel, or exposure to a patient with a known bacterial diarrhea.
KEY POINTS: GASTROENTERITIS AND DEHYDRATION
1. Young children with gastroenteritis can become dehydrated easily.
2. Vomiting in the pediatric population has a broad differential.
3. Most children can be successfully rehydrated without intravenous fluids.
9. Should narcotics be withheld from children with acute abdominal pain while
awaiting a surgical evaluation?
No. Multiple studies have shown diagnostic accuracy from physical examination increases
when patients’ pain is controlled.
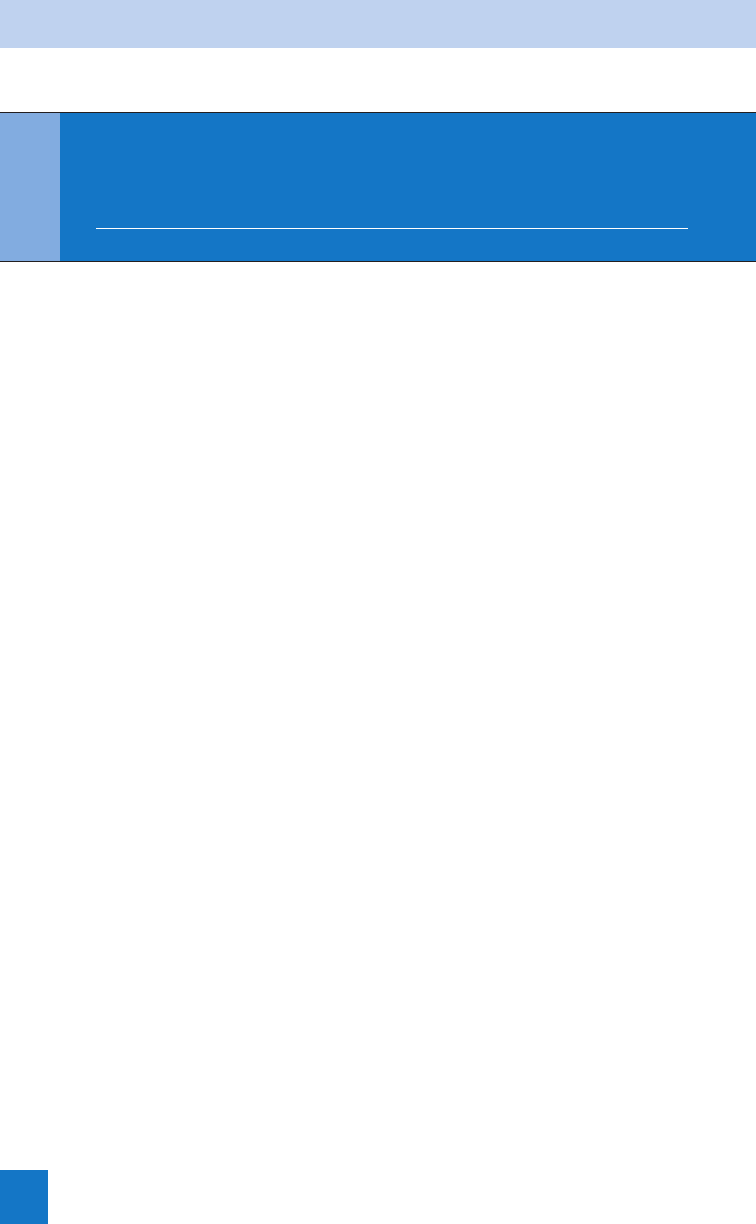
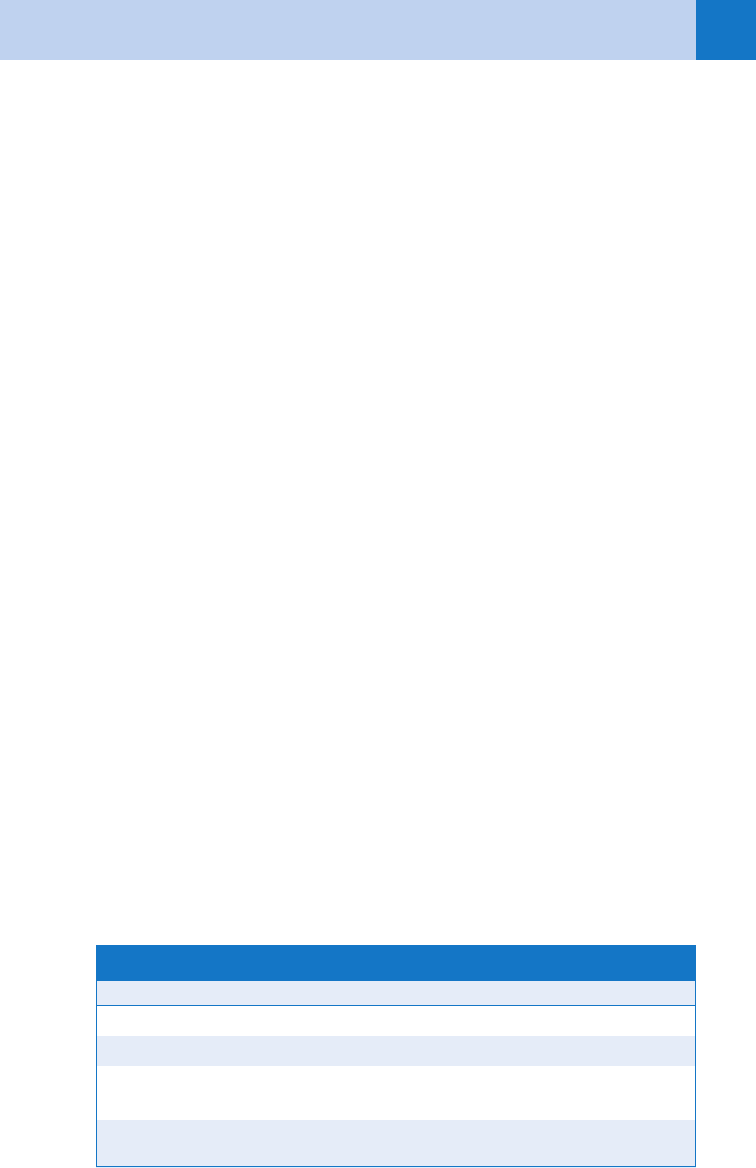
Neonate 2 months–2 years
Malrotation Incarcerated hernia
Necrotizing enterocolitis Intussusception
Testicular torsion Urinary tract infection
2–5 years 6–18 years
Appendicitis Appendicitis
Foreign body Ovarian/testicular torsion
Intussusception Kidney and gallbladder stones
Ovarian torsion Diabetic ketoacidosis
Urinary tract infection Ectopic pregnancy
Strep pharyngitis Pelvic inflammatory disease
Henoch-Schönlein purpura Gallbladder disease
TABLE 63-1. DIFFERENTIAL OF NONTRAUMATIC ABDOMINAL PAIN BY AGE

Chapter 63 PEDIATRIC GASTROINTESTINAL DISORDERS AND DEHYDRATION442
10. How does appendicitis present in younger children?
The diagnosis of appendicitis is commonly missed in younger children who often present with
nonspecific symptoms. Vomiting, abdominal pain, fever, diarrhea, irritability, and right hip pain
are some typical presentations, often attributed to other causes. Similarly, their physical
examinations frequently reveal diffuse abdominal tenderness or abdominal distention, while pain
localized to the right lower quadrant is an infrequent presentation. Appendicitis in the infant is
typically recognized only after perforation, which occurs in 70% to 95% of these cases.
11. What physical examination findings are found in older children with
appendicitis?
The most common findings are tenderness in the right lower quadrant and involuntary
guarding. Rovsing’s sign (pain in the right lower quadrant with palpation of the left lower
quadrant), obturator sign (pain with internal rotation of the flexed hip), and the psoas sign
(pain with extension of the right thigh) have not been shown to be particularly sensitive or
specific for appendicitis in children. Their absence should not be used to rule out appendicitis.
12. What laboratory tests are helpful in children with appendicitis?
If the history and physical examination are highly suspicious for appendicitis, no further tests
are required and a surgeon should be consulted.
The white blood cell count (WBC) does not provide useful levels of sensitivity and
specificity. A WBC .10,000/mm
3
has a sensitivity of 88%, but specificity of 53%; a WBC
.15,000/mm
3
improves specificity to over 60%, but the sensitivity declines to 19%. An
elevated C-reactive protein has similar sensitivity and specificity to a WBC.10,000, with even
lower sensitivity and specificity when measured in the first 12 hours. A positive urinalysis
cannot exclude appendicitis; 30% of children with appendicitis have pyuria or bacteriuria.
13. What are the advantages and disadvantages of the different radiographic tests
for appendicitis?
n
Plain films: Insensitive and nonspecific, these are normal in 82% of children with
appendicitis.
n
Ultrasound (US): If available, US should be the initial study of choice in children with
suspected appendicitis since lack of peritoneal fat favors ideal imaging with this modality.
In experienced hands, US provides a high sensitivity (71%–92%) and specificity (96%–
98%). Appendicitis will show an appendiceal diameter .6 mm, wall thickness .2 mm,
obstruction of the appendiceal lumen, appendicolith, high echogenicity surrounding the
appendix, or pericecal free fluid. Obesity, uncooperative patients, or atypical locations of the
appendix may limit this study.
n
Computerized tomography (CT): With CT, appendicitis shows an appendiceal diameter
.6 mm, wall thickness .1 mm, periappendiceal fat stranding or fluid collection, or an
appendicolith. In children, CT has a higher sensitivity (94%–99%) and specificity
(87%–99%) than US. Higher cost, potential need for sedation, and radiation exposure are
the major drawbacks of CT.
KEY POINTS: APPENDICITIS
1. Younger children have atypical presentations of appendicitis, resulting in delays in diagnosis
and high perforation rates.
2. Lab tests are relatively non-specific and should not be used to exclude a diagnosis of
appendicitis.
3. In equivocal cases, ultrasound should be the first imaging study in children with suspected
appendicitis.

Chapter 63 PEDIATRIC GASTROINTESTINAL DISORDERS AND DEHYDRATION 443
14. How does intussusception present?
Intussusception, an invagination of one portion of bowel into a distal segment (most commonly
at the ileocecal junction), afflicts children most commonly between infancy and 3 years of age.
The classic triad of colicky abdominal pain, vomiting, and bloody stool is present in less than
25% of children. Intermittent periods of irritability, where children may pull their knees up
toward their chest, is often the only symptom. Although often cited in the literature, currant
jelly stools are a late, rare, and ominous finding from bowel ischemia. Younger children may
present with nonspecific findings such as altered mental status or lethargy.
15. How do you diagnose intussusception?
The classic crescent sign on plan radiography from the intussuscepting mass is rarely seen.
Nevertheless, abdominal X-rays can be helpful in low risk cases; when air is seen in the
ascending colon on at least two of three views (i.e., supine, prone, and lateral decubitus),
likelihood of intussusception is substantially reduced. US may identify a donut or target sign,
yielding a sensitivity and specificity of over 90%. Air enema may be utilized to both diagnose
and treat intussusception.
16. How should intussusception be treated?
Air enemas provide equivalent success rates to contrast enemas with less radiation exposure.
Due to a 1% risk of perforation with enema reduction, a surgeon should be available. Because
up to 10% of patients will have recurrence within the first 24 hours, caregivers must ensure
appropriate family education on strict return precautions. Shock or suspected intestinal
perforations necessitate surgical consultation for operative repair.
17. What is the significance of bilious emesis in a neonate?
Bilious emesis in a neonate is a surgical emergency until proven otherwise because it could
represent malrotation with volvulus (midgut volvulus). Congenital malrotation of the midgut
predisposes the bowel to twisting on itself, leading to bowel obstruction and vascular
compromise, with bowel necrosis developing in as little as 2 hours.
Midgut volvulus classically presents with sudden onset of bilious emesis and
abdominal pain; however, early in the course of illness, more than half of patients have
normal abdominal examinations and one third have abdominal distention without
tenderness. Thus, all infants with bilious emesis should undergo diagnostic testing
regardless of their abdominal examinations. Although X-rays can show small bowel
obstruction, a double bubble sign, or paucity of distal bowel gas with volvulus, imaging is
often normal. An upper gastrointestinal (UGI) series with contrast is the gold standard
because it will show a cork screwing of contrast or the duodenojejunal junction not
crossing to the left of the vertebral column.
If volvulus is suspected, intravenous fluids should be given, a nasogastric tube inserted,
broad-spectrum antibiotics administered, and surgical consultation obtained immediately.
18. What characteristics of a patient’s history help differentiate pyloric stenosis
from other causes of vomiting in infants?
True projectile emesis, where the vomitus shoots away from the patient, is most commonly
found with pyloric stenosis. A hypertrophy of the pylorus develops between 1 to 5 weeks of
age. Initially, infants vomit only at the end of feeds, later developing more classic projectile
vomiting. Unlike more severe conditions such as malrotation, emesis is usually nonbilious due
to the stenosis being proximal to the duodenum. The patient will remain hungry and continue
attempts to feed. Unlike more benign causes of vomiting such as reflux, the patient does not
gain weight appropriately.
19. What diagnostic findings arise with pyloric stenosis?
Vomiting leads to loss of hydrogen ions from the stomach, the kidneys attempt to conserve
sodium in a response to dehydration, spilling potassium into the urine, all resulting in a
hypokalemic, hypochloremic metabolic alkalosis.
Chapter 63 PEDIATRIC GASTROINTESTINAL DISORDERS AND DEHYDRATION444
The diagnostic study of choice is an US, which has a sensitivity and specificity of nearly
100%. In pyloric stenosis, the pyloric wall is greater than 4 mm wide or 14 mm long. If the
US is equivocal, then an UGI will classically show a string sign as contrast travels through the
narrowed pylorus.
Patients with pyloric stenosis require rehydration and eventual surgical correction,
although in developing countries often patients can be supported long enough to allow the
hypertrophy to resolve without surgery.
20. Are inguinal hernias dangerous?
One percent to 2% of children develop inguinal hernias, with 10% ultimately incarcerating.
This happens most commonly in children younger than 1 year of age. If the incarceration
persists, the bowel can strangulate, cutting off its blood supply and leading to bowel
obstruction or necrosis.
Unless bowel necrosis is already suspected, manual reduction can be attempted on
incarcerated hernias to prevent strangulation. With the patient in Trendelenburg, using
constant gentle pressure, 95% of inguinal hernias can be reduced and these patients can be
safely discharged for outpatient surgical repair. If necessary, sedation can be used to assist in
pushing the hernia back through the inguinal ring. If reduction is unsuccessful or
strangulation suspected, immediately consult a surgeon.
21. What is the difference between a hernia and a hydrocele?
A hydrocele arises from an incomplete obliteration of the processus vaginalis, which allows
the peritoneum to translocate into the scrotum. Unlike hernias, these can be transilluminated.
In addition, they are readily separable from the testes. If you cannot differentiate a hydrocele
from a hernia on examination, you can obtain a scrotal ultrasound. Hydroceles are benign and
often resolve spontaneously.
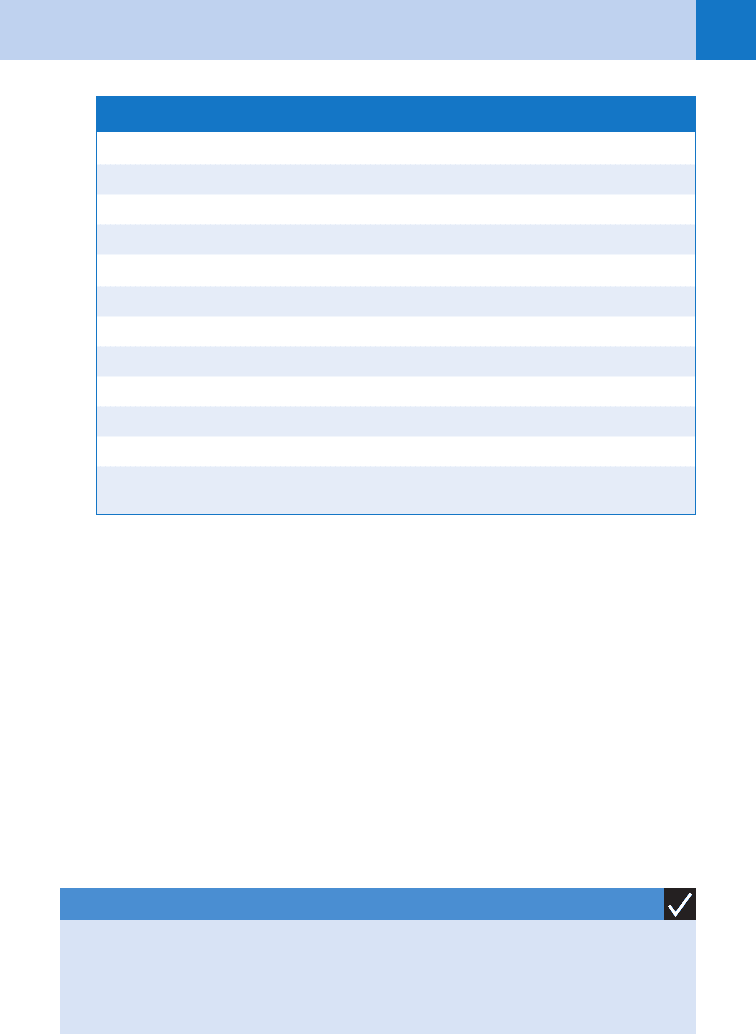
KEY POINTS: SURGICAL EMERGENCIES IN YOUNG CHILDREN
1. Intussusception rarely presents with the classic triad of colicky abdominal pain, currant jelly
stools, and vomiting. More often only intermittent irritability is present.
2. Bilious emesis in a neonate is a surgical emergency until proven otherwise.
3. Infants with pyloric stenosis have projectile emesis but remain hungry and interested in
feeding.
22. Why is jaundice concerning in a neonate?
While newborns often have physiologic jaundice that is self-limited, significantly elevated
levels of unconjugated bilirubin can lead to kernicterus, with resulting deafness,
developmental delay, or death. These elevated levels can arise from a myriad of causes
including Rh or ABO incompatibility, prematurity, polycythemia, intestinal obstruction, sepsis,
or dehydration. All patients with visible jaundice need a documented bilirubin level, and if
elevated a search made for etiology. This may include a blood type, Coomb’s test and
complete blood count (CBC). Patients with elevated age-specific bilirubin levels may require
phototherapy, with exchange transfusion considered for marked elevations (.25 mg/dl).
23. Is it normal for a child to have constipation?
It is normal for infants to strain during bowel movements, but parental anxiety over infant
straining or lack of frequent bowel movements may lead to an ED visit. Bottle-fed infants can
often pass as few as one stool every other day. Breastfed infants may pass a stool with each
feed or as infrequently as once every 7 to 10 days. As infants age, it is typical for stool
frequency to decrease; by 4 years of age children average 1.2 bowel movements per day.
Chapter 63 PEDIATRIC GASTROINTESTINAL DISORDERS AND DEHYDRATION 445
Rarely, infants presenting with constipation have more serious conditions. A thorough
history and physical examination can give clues to some of these entities: onset of symptoms
in the first week of life (Hirschsprung’s), abnormal tone, lethargy and weak cry (botulism and
hypothyroidism), or worrisome abdomen examination (volvulus).
The diagnosis of constipation should be based on difficulty or pain with passage of a
bowel movement rather than absolute frequency. In older children, constipation most
commonly arises with changes in diet or inadequate fluid intake. School-age children may
have behavioral issues, such as a fear of having a bowel movement at school that ultimately
affects their bowel patterns.
24. How can you treat constipation in the ED?
Most patients with constipation not arising from a serious etiology can be managed as
outpatients. A trial of a soy-based formula may relieve constipation in infants with suspected
cow’s milk intolerance. A one-time enema can occasionally help, but hypertonic phosphate
enemas and tap water enemas should be avoided because they can cause severe electrolyte
abnormalities. Mineral oil (1–4 ml/kg/dose), lactulose (1–2 ml/kg/dose), milk of magnesia
(1–3 ml/kg/dose), or MiraLax (mix 17g in 8 oz fluid) can be administered in the short term.
Long-term management includes increasing fluid intake and adding fiber to the diet.
25. What is a Meckel’s diverticulum?
It is a remnant of the omphalomesenteric duct in children. It is the most significant cause of
painless rectal bleeding and can lead to obstruction or intussusception. Sixty percent contain
heterotopic gastric, pancreatic, or endometrial tissue. If suspected, a technetium 99m
Meckel’s scan can identify ectopic gastric mucosal tissue, thus making the diagnosis.
26. What is Meckel’s rule of twos?
Meckel’s diverticulum occurs in 2% of the population; 2% of patients will manifest symptoms;
the diverticulum is typically 2 inches long and within 2 feet of the ileocecal valve; average age
at presentation is 2 years.
27. How do you manage an ingested gastrointestinal foreign body?
The management of foreign bodies depends on the nature of what was ingested and its
location. Any patient with a known ingestion and hematochezia, melena, or signs of an acute
abdomen requires immediate surgical consultation. See Table 63-2.
28. What are the possible complications of an esophageal foreign body?
Airway obstruction, esophageal stricture, esophageal perforation, mediastinitis, or
paraesophageal abscess.
29. What diseases are associated with these classic findings on X-ray?
See Table 63-3.
Emergent Endoscopy Gastrointestinologist Consultation
Sharp objects in the esophagus Button battery past the esophagus
Button battery in the esophagus Sharp objects past the pylorus
Objects causing difficulty controlling secretions
or breathing
Long objects past the pylorus
(.5 cm)
Objects in the esophagus for more than 24 hours Multiple magnets
TABLE 63-2. MANAGEMENT OF GASTROINTESTINAL FOREIGN BODIES
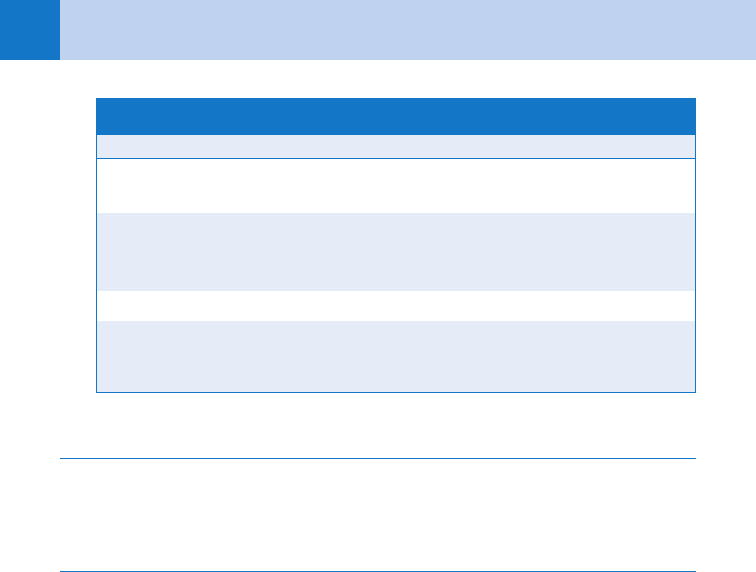
Chapter 63 PEDIATRIC GASTROINTESTINAL DISORDERS AND DEHYDRATION446
Finding X-ray Description Disease Process
Double Bubble Paucity of gas with air bubble in
stomach and duodenum
Volvulus
Crescent Curvilinear mass often found near
transverse colon beyond hepatic
flexure
Intussusception
Pneumatosis Intestinalis Air in bowel wall Necrotizing enterocolitis
Enlarged pylorus Wall of pylorus .4 mm thick
Canal .14 mm
Pyloric stenosis
TABLE 63-3. RADIOGRAPHIC FINDINGS IN PEDIATRIC ABDOMINAL PAIN
BIBLIOGRAPHY
1. Gardikis S, Touloupidis S, Dimitriadis G, et al: Urological symptoms of acute appendicitis in childhood and
early adolescence. Int Urol Nephrol 34(2):189–192, 2002.
2. Grönroos JM: Do normal leucocyte count and C-reactive protein value exclude acute appendicitis in children?
Acta Paediatr 90(6):649–651, 2001.
3. Horwitz JR, Gursoy M, Jaksic T, et al: Importance of diarrhea as a presenting symptom of appendicitis in very
young children. Am J Surg 173(2):80–82, 1997.
4. Kim MK, Strait RT, Sato TT, et al: A randomized clinical trial of analgesia in children with acute abdominal
pain. Acad Emerg Med 9(4):281–287, 2002.
5. Kokki H, Lintula H, Vanamo K, et al: Oxycodone vs placebo in children with undifferentiated abdominal pain:
a randomized, double-blind clinical trial of the effect of analgesia on diagnostic accuracy. Arch Pediatr Adolesc
Med 159(4):320–325, 2005.
6. Kwok MY, Kim MK, Gorelick MH: Evidence-based approach to the diagnosis of appendicitis in children.
Pediatr Emerg Care 20(10):690–698, 2004.
7. Levy JA, Bachur RG: Intravenous dextrose during outpatient rehydration in pediatric gastroenteritis. Acad
Emerg Med 14(4):324–330, 2007.
8. Roskind CG, Ruzal-Shapiro CB, Dowd EK, et al: Test characteristics of the 3-view abdominal radiograph series
in the diagnosis of intussusception. Pediatr Emerg Care 23(11):785–789, 2007.
9. Rothrock SG, Green SM, Hummel CB: Plain abdominal radiography in the detection of major disease in
children: a prospective analysis. Ann Emerg Med 21(12):1423–1429, 1992.
10. Spandorfer PR, Alessandrini EA, Joffe MD, et al: Oral versus intravenous rehydration of moderately
dehydrated children: a randomized, controlled trial. Pediatrics 115(2):295–301, 2005.
ACKNOWLEDGMENT
The editors gratefully acknowledge the contributions of Mark Anderson, MD, author of this chapter
in the previous edition.
447
PEDIATRIC INFECTIOUS DISEASES
CHAPTER 64
Roger M. Barkin, MD, MPH, FACEP, FAAP
1. Are infectious diseases important to recognize in the pediatric patient?
Infectious diseases account for a significant percentage of pediatric visits to the ED for acute
illness. Although most conditions are self-limited and infrequent, some infections are
significant in that they may be multisystem or life threatening, requiring consideration in the
differential diagnosis of many presenting complaints.
2. What is the mechanism of spread of measles (rubeola)?
By direct contact with infectious droplets or airborne dissemination.
3. What is the incubation period for measles?
From exposure to the onset of symptoms, 8 to 12 days. It is 14 days from exposure to the onset
of the rash. Patients are contagious 1 to 2 days before they become symptomatic and 4 days
after the rash appears.
4. List the common signs and symptoms of patients with measles.
n
High fever.
n
Three Cs: Conjunctivitis, coryza, and cough may be observed.
n
Rash: Discrete red maculopapular rash first appears on the forehead, becoming coalescent
as it spreads down the trunk to the feet by the third day of the illness. The rash fades in the
same head-to-feet pattern as it appeared.
n
Koplik’s spots: 1- to 3-mm bluish white spots on a bright red surface, which appear first on
the buccal mucosa opposite the lower molars. They are a pathognomonic exanthem of
measles. They appear approximately within 48 hours after the onset of symptoms. The
spots may spread to involve the buccal and labial mucosa and disappear on the second day
after the onset of the rash.
n
Photophobia may be noted.
5. Name the complications of measles.
Otitis media and bronchopneumonia. Encephalitis may occur as well.
6. What is subacute sclerosing panencephalitis?
A rare degenerative central nervous system disease caused by a latent measles infection,
occurring an average of 10 years after a primary measles illness. Patients have progressive
intellectual and behavioral deterioration and convulsions. This disease is not contagious.
7. Describe the exanthem seen in rubella. Why is it also called 3-day measles?
Numerous discrete rose-pink maculopapules first appear on the face and, as in rubeola,
spread downward to involve the trunk and extremities. The rash on the face fades on day 2,
and the rash on the trunk becomes coalescent. By the third day, the rash disappears, which is
why rubella is also called 3-day measles. Rubella is now rarely reported in the United States
secondary to the efficacy of immunizations.
8. What are Forschheimer spots?
Pinpoint red macules on the soft palate seen early in rubella; however, in contrast to Koplik’s
spots, they are not pathognomonic.
