Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.


Chapter 61 SEIZURES IN INFANCY AND CHILDHOOD428
n
Juvenile myoclonic epilepsy: Begins from 12 to 18 years old. Triad of morning myoclonic,
generalized tonic-clonic, and absence seizures. Seizures are brought on by stress, alcohol,
and sleep deprivation. It often requires lifelong treatment with an agent such as Depakote
or Lamictal.
21. What work-up should be done following an afebrile seizure in an asymptomatic
child?
If the child has returned to normal, he or she can go home and follow up with an
outpatient EEG and MRI. A neurological consultation should also be scheduled. If the
patient does not return to baseline, in addition to standard lab testing (i.e., bedside
glucose, CBC, electrolytes, liver function tests [LFTs], ammonia, or urine toxicology), an
imaging study (CT or MRI) should be performed emergently. If a clinical indication, an
LP should be performed. Occasionally, an acute EEG should also be performed to rule out
subclinical status.
22. Under what conditions should afebrile seizures be treated using anti-
epileptics?
Treatment of seizures with anti-epileptics balances the risk of recurrence with the risks of the
medication. The risk of having a second afebrile seizure after a first is slightly below 50%.
Therefore, unless there are other factors, it is customary not to start an antiepileptic
medication until after the second seizure. Things that confer additional risk such as
dramatically abnormal EEG, very strong family history, or abnormal neurological examination
may impact the decision of whether or not to start medication. This decision should be made
with a pediatric neurologist.
23. What are the older and newer antiepileptics and how do they vary?
n
Older antiepileptics: phenobarbital, phenytoin, carbamazepine, ethosuximide, and valproate.
n
Newer antiepileptics: topiramate, lamotrigine, levetiracetam, felbamate, gabapentin,
oxcarbazepine, zonisamide, pregabalin, and rufinamide.
Older drugs have the advantage of cost and experience. Newer drugs have the advantages of
better side-effect profile, decreased monitoring requirements, less frequent dosing regimens,
and decreased interaction with other drugs.
24. What are important side effects of the different antiepileptic drugs?
Recently almost all anti-epileptics have been linked to suicidal behavior. Specific side
effects:
n
Phenobarbital: sedation, hyperkinesis, and cognitive dysfunction
n
Carbamazepine (Tegretol): ataxia, dizziness, sedation, and rash
n
Valproic acid (Depakote): alopecia, weight gain, and tremor
n
Phenytoin (Dilantin): hirsutism, gingival hyperplasia, and ataxia
n
Ethosuximide (Zarontin): gastrointestinal (GI) distress, headaches, drowsiness, and
hiccoughs
n
Levetiracetam (Keppra): psychotic behavior and irritability
n
Lamotrigine (Lamictal): rash
n
Topiramate (Topamax): sedation, glaucoma, and kidney stones
n
Felbamate (Felbatol): aplastic anemia, insomnia, and anorexia
n
Tiagabine (Gabitril): GI intolerance
n
Oxcarbazepine (Trileptal): hyponatremia
n
Zonisamide (Zonegran): weight loss, kidney stones, headache, and decreased sweating
n
Lacosamide (Vimpat): dizziness, headache, nausea, and diplopia
n
Carisbamate(Comfyde): dizziness, headache, somnolence, and nausea
n
Pregabalin (Lyrica): rhabdomyolysis
n
Rufinamide (Banzel): somnolence, nausea, and headache
n
Vigabatrin (Sabril): peripheral vision loss
Chapter 61 SEIZURES IN INFANCY AND CHILDHOOD 429
25. If an individual stopped taking their antiepileptic drug because they weren’t
having seizures, and then started to have them again, at what dose should he
restart the medication?
If it has been longer than 1 week, the drug must be started as if you had never been on it.
This is especially important for a drug such as Lamictal where a rash or Stevens-Johnson
syndrome can occur if it is started too quickly. The individual should be reminded that
medication should only be stopped after consultation with a physician.
26. When should antiepileptic drugs be discontinued?
The general rule is that an antiepileptic drug can be stopped after 2 years of seizure freedom.
Exceptions to this rule would occur for dramatically abnormal EEG or abnormal neurological
examination. Approximately one third of patients remain seizure free after drug withdrawal. If
seizures are to reappear, they will within the first 6 months in 80%.
There is no evidence that a trial off of medicine significantly impacts the eventual control
of seizures.
27. What happens if a dose of antiepileptic drug is missed?
If it is time for the next dose, it is reasonable to simply continue on without giving additional
medication. If it is not time for the next dose, it is reasonable to try to squeeze in the missed
dose while slightly delaying the next dose.
28. What if vomiting occurs shortly after taking an antiepileptic drug?
If it is more than an hour since the dose was taken, no action is necessary. If it is between half
an hour and an hour, a half dose can be taken. If it is less than half an hour since the dose or
fragments of the medicine can be seen in the vomit, the dose should be repeated
29. What is the definition of status epilepticus?
Continuous or intermittent seizure activity for longer than 30 minutes.
30. What is the treatment for status epilepticus?
Airway, breathing, and circulation (ABCs) first, of course. A bedside glucose, chemistry panel
(with calcium, magnesium, and phosphorous), urine toxicology and anticonvulsant levels
along with intracranial imaging (usually CT) should be obtained. If possible, a continuous EEG
(performed in consultation with a neurologist) is helpful and should establish a burst-
suppression pattern.
After establishing intravenous (IV) access, a benzodiazepine, such as lorazepam, should
be given and repeated multiple times if necessary. If seizures persist, phenobarbital,
phenytoin, or levetiracetam should be given next. If the seizure is still not controlled, the next
step is a midazolam drip, propofol, or pentobarbital.
31. What should an onlooker do if the child has another seizure?
n
If possible, place the child on his or her side.
n
Remove anything that may injure the child.
n
Place something soft under the head.
n
Time the event.
n
Do not place anything near the mouth.
n
If less than 5 minutes, it may not be necessary to do anything.
n
If greater than 5 minutes, administer Diastat (rectal diazepam) or go to the ED.
n
If greater than 10 minutes, go to the ED.
32. What cautions should you give to parents of children who have seizures?
n
No bathing or swimming alone.
n
No activities that may result in harm if there is a temporary loss of consciousness.
n
Driving guidelines vary by state.
n
A complete list of recommended activities can be found at the Epilepsy Foundation’s website.
Chapter 61 SEIZURES IN INFANCY AND CHILDHOOD430
KEY POINTS: SEIZURES IN INFANCY AND CHILDHOOD
1. Seizures have characteristic patterns that distinguish from nonepileptic events. There are
typical childhood seizure patterns that guide prognosis and treatment.
2. ED evaluation of a pediatric seizure is dependent on the age, type, and clinical suspicion for
infection or nonaccidental trauma.
3. The evaluation of a child in status or not returning to baseline neurologic state requires
consultation with a pediatric neurologist for treatment and EEG monitoring.
BIBLIOGRAPHY
1. Fenichel GM: Clinical pediatric neurology: a signs and symptoms approach, ed 6 Philadelphia, 2009,
W. B. Saunders.
2. Pellock JM, Bourgeois BFD, Dodson WE, et al, editors: Pediatric epilepsy: diagnosis and therapy, ed 3,
New York, 2008, Demos Medical Publishing.
3. Wylie E, Gupta A, Lachhwani DK: The treatment of epilepsy: principles and practice, ed 4, Philadelphia, 2005,
Lippincott Williams & Wilkins.
431
ACUTE RESPIRATORY DISORDERS
IN CHILDREN
CHAPTER 62
Kelly Flett, MD, and Joan P. Bothner, MD
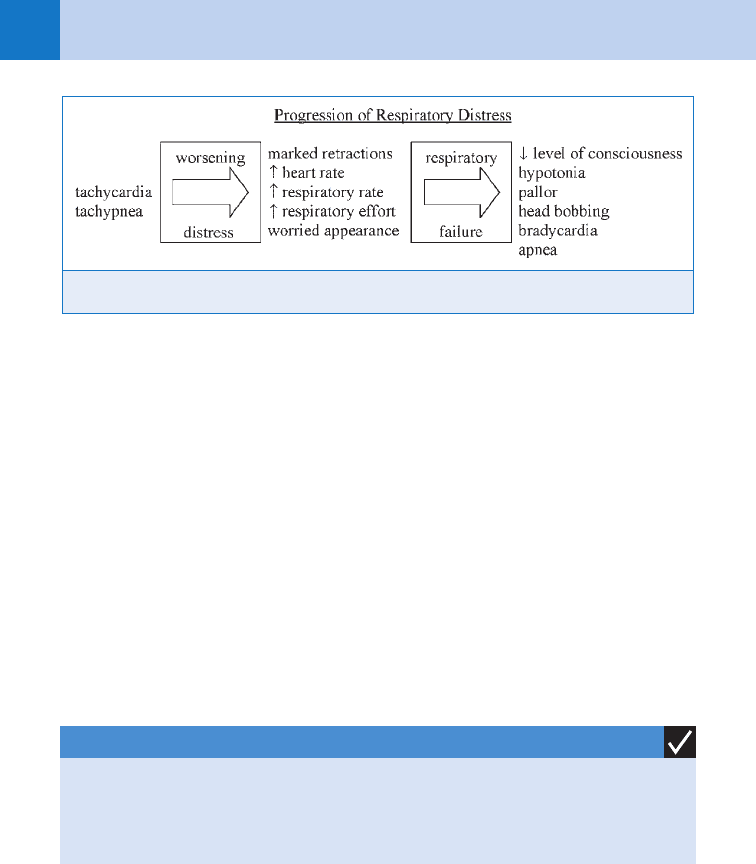
1. What are the signs and symptoms of respiratory distress in a child?
The progression of respiratory distress is shown in Figure 62-1. Tachypnea is often the
earliest sign in younger children because they cannot significantly increase their tidal volume.
Normal respiratory rate in children decreases with age: newborns breathe approximately
50 breaths per minute, while a 12-month-old infant averages 30 breaths per minute. Until
respiratory failure leads to hypoventilation and hypercarbia, arterial blood gases are of limited
clinical value. Oxygen saturation should not be the sole determinant of severity, with the
clinical state primarily dictating any need for intervention. Mental status is often the most
important parameter; crying with examination is appropriate (a well-behaved child may
actually be altered).
2. Why are airway problems more serious in pediatric patients than in adults?
There are several important differences between the adult and the pediatric airway. The child’s
tongue is large, and is the most common cause of airway obstruction in the obtunded child.
The narrowest portion of the pediatric airway is at the cricoid ring, making obstruction with
subglottic pathology more likely than in adults. The small size of the pediatric airway means
that small changes in diameter cause significant increases in resistance. (Remember physics!
Resistance is inversely related to the fourth power of the radius.) Higher oxygen consumption
in children contributes to more rapid decrease in arterial oxygen levels after airway
obstruction.
3. How can I determine where the problem is?
All noisy breathing is not asthma; a few seconds of observation often helps differentiate upper
and lower airway obstruction. Generally, extrathoracic lesions (e.g., epiglottis, croup) produce
inspiratory stridor (i.e., harsh, vibratory sound), while intrathoracic lesions (e.g., asthma,
bronchiolitis) produce prolonged expiratory wheezing (i.e., high-pitched). Regardless of the
location, severe pathology can produce both inspiratory and expiratory sounds.
4. What are common causes of upper airway obstruction in children?
See Table 62-1.
5. Discuss the signs and symptoms of croup, who gets it, what causes it,
and what the physician can do for it.
Croup, or laryngotracheitis, is the most common cause of infectious acute upper airway
obstruction. The etiology is viral (e.g., parainfluenza, influenza and respiratory syncytial
viruses) with erythema and swelling of the trachea just below the vocal cords, and patients
classically present with a barky or seal-like cough. The mean age of affected patients is
18 months with a seasonal increase in autumn and early winter. Patients are often febrile,
with a prodrome of mild upper respiratory symptoms that progress to stridor. Symptoms
are worse with agitation and at night, classically peaking on day 2 of illness. Because the
lungs are not directly affected, oxygen saturation can be maintained even in severe illness.
Laboratory data are useless. Diagnosis is clinical; X-rays are not indicated unless diagnosis
is unclear and foreign body obstruction is a consideration.
Chapter 62 ACUTE RESPIRATORY DISORDERS IN CHILDREN432
6. Who needs nebulized epinephrine?
Aerosolized epinephrine decreases airway obstruction. It is indicated for children with stridor
at rest or marked work of breathing (e.g., tachypnea, retractions). Racemic epinephrine
(0.5 mL of 2.25% solution) is used most commonly, but L-epinephrine alone (5 mL of 1:1000
solution) is equivalent. Maximal effect is seen within 30 minutes, with potential rebound to
baseline within 3 hours. Patients without resting stridor after 3 hours can be safely discharged
home. Criteria for admission include continued stridor at rest, cyanosis, signs of respiratory
distress, dehydration, or questionable follow-up. Intubation is rarely needed, but when
necessary often requires relatively smaller endotracheal tube (ETT) sizes.
7. What about steroids and croup?
Steroids should be considered for any child who presents to the ED with croup. A single oral
dose of dexamethasone 0.6 mg/kg (maximum of 8 mg) decreases the need for hospitalization
and return ED visits. There is no evidence to suggest that repeat dosing is indicated or helpful,
but this might be considered for young patients presenting prior to the peak of illness (day 1).
Nebulized budesonide does not provide benefit over dexamethasone.
Figure 62-1. Signs and symptoms of respiratory distress in children.
KEY POINTS: CROUP
1. Treatment is with oral dexamethasone 0.6 mg/kg (maximum of 8 mg).
2. Racemic epinephrine is used for patients with moderate to severe respiratory distress or
stridor at rest.
8. When should I worry about epiglottitis and bacterial tracheitis?
Although both conditions are rare, they warrant careful consideration. Children generally
appear toxic with rapid onset of symptoms. Epiglottitis, now rare with universal vaccination
against Haemophilus influenzae type B, is a bacterial cellulitis of the supraglottic structures,
most notably the lingual surface of the epiglottitis. Children lack cough and present with
drooling, dysphagia, and a predilection for the sniffing position. Radiographic evidence
includes a swollen epiglottis (the thumb sign), thickened aryepiglottic folds, and obliteration
of the vallecula. Bacterial tracheitis, although rare, may be emerging as a more significant
problem. Patients present with croup-like symptoms but toxic in appearance with significant
respiratory distress. Radiographs may show shaggy subglottic narrowing and clouding of
the trachea. Airway management and broad-spectrum antibiotics (second- or third-
generation cephalosporins) are the mainstay of therapy for both disorders.
Chapter 62 ACUTE RESPIRATORY DISORDERS IN CHILDREN 433
RSV, respiratory syncytial virus; URI, upper respiratory infection.
Etiology Age Range Onset Toxicity Drooling Treatment
Croup Parainfluenza type 1, influenza A and B,
RSV, rhinovirus
6 mo–3 yr URI prodrome Mild Absent Mist, steroids, aerosolized
epinephrine
Epiglottitis Haemophilus influenzae, group A,
b-hemolytic Streptococcus, Staphylococcus
aureus, Streptococcus pneumoniae, viruses
3–7 yr Acute Marked Frequent Airway management,
antibiotics
Retropharyngeal
abscess
Multiple: anaerobes Infancy–6 yr URI, sore throat Variable Variable Antibiotics, drainage
Bacterial tracheitis S. aureus, H. influenzae, S. pneumoniae,
Branhamella catarrhalis after viral insult
3 yr “Croup” prodrome Moderate Usually
absent
Airway management,
antibiotics
TABLE 62-1. CAUSES OF UPPER AIRWAY OBSTRUCTION

Chapter 62 ACUTE RESPIRATORY DISORDERS IN CHILDREN434
9. What is the appropriate initial management of a patient with suspected
epiglottitis?
Immediately call a surgical or ear, nose, throat (ENT) consultant for anticipated emergent
airway management in the operating room; do not agitate the child in any way. Direct
examination or manipulation of the oropharynx can cause contraction of the pharyngeal
muscles and worsen airway obstruction. If the patient will tolerate without agitation, start
high-flow oxygen via a nonrebreather bag reservoir mask. Radiographs, blood work,
intravenous (IV) lines, and antibiotics can wait; if a child obstructs, bag-valve-mask ventilation
should be attempted first.
10. What are retropharyngeal space infections?
The retropharynx is a potential space located immediately posterior to the pharynx, larynx,
and trachea. Infection is believed to arise from extension of an acute infection of the ear, nose,
or throat, with spread to the lymph nodes in the prevertebral space and subsequent abscess
formation. Trauma to the nasopharynx is also a predisposing factor. About 90% of patients are
younger than 6 years; the affected child usually appears alert (but mildly toxic), with upper
respiratory symptoms, fever, and a stiff slightly extended neck.
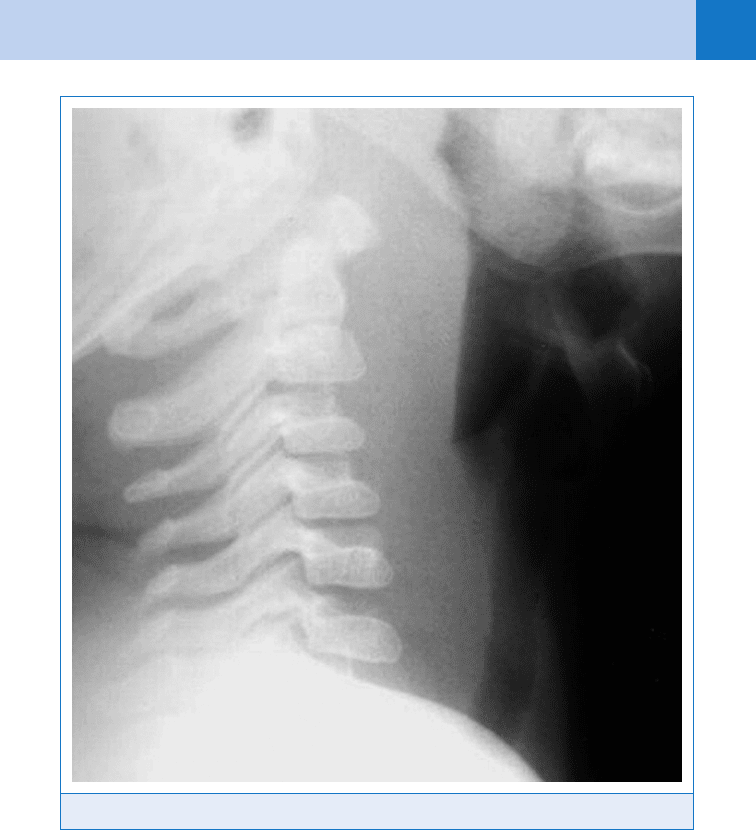
11. What imaging studies are helpful in the diagnosis of retropharyngeal
infections?
Lateral neck films are often diagnostic (90% sensitivity) but can be difficult to interpret
depending on the phase of respiration and neck position. Findings include an increase in the
width of the prevertebral space to greater than the anteroposterior width of the adjacent
cervical vertebral body, anterior displacement of the airway, and loss of the normal step-off at
the level of the larynx. Air-fluid levels may be seen after abscess formation (Fig. 62-2).
Computed tomography (CT) scanning is highly sensitive and is used to differentiate abscess
from phlegmon or soft-tissue cellulitis.
12. How are they managed?
Treatment includes hospital admission, parenteral antibiotic therapy, and incision and drainage
if an abscess is present. Most children do not need acute airway management.
13. When should a foreign body be suspected?
Most patients who present with foreign-body aspiration are males between 5 months and
3 years old. Although a history of an aspiration event (found in 50%–70%) is the most predictive
factor, any sudden onset of cough, dyspnea, or wheezing should raise suspicion. Respiratory
signs such as stridor or focal wheezing may be absent. Radiographs will only show radiopaque
objects. For other objects, expiratory or lateral decubitus films may reveal asymmetric expansion
due to a ball-valve mechanism of the foreign body. Endoscopy is diagnostic.
14. How are suspected foreign bodies managed in pediatric patients?
Immediate management depends on the degree of respiratory distress but should be minimal
unless respiratory failure is imminent. For unconscious patients, call for emergent ENT
evaluation and attempt direct laryngoscopy with removal of any visualized foreign object with
Magill forceps. If this fails, attempt bag-valve-mask ventilation and intubation, to push the
offending object into one bronchus. If the child cannot be intubated, a needle cricothyroidotomy
should be performed.
15. What is bronchiolitis and who does it affect?
Commonly found in children younger than 2 years of age, bronchiolitis is a predominantly
wintertime infection (usually from RSV), characterized by inflammation, edema, and
mucus accumulation of the bronchioles. Progression of illness leads to lower airway
obstruction and consequently ventilation-perfusion mismatch. With small bronchioles
more prone to mucous plugging and obstruction, peak incidence and severity is at 3 to
6 months of age.
Chapter 62 ACUTE RESPIRATORY DISORDERS IN CHILDREN 435
16. What are the clinical signs and symptoms of bronchiolitis?
Fever, tachypnea, wheezing, and signs of respiratory distress such as nasal flaring and
retractions are coupled with copious mucus secretions. Symptoms follow a predictive course
with a 1-to 2-day prodrome of rhinorrhea, cough, and low-grade fever that progresses to
lower respiratory signs and respiratory distress. Symptoms peak around days 3 to 4 of
illness. Auscultation reveals diffuse wheezing and crackles that often vary between
examinations. Children are generally not toxic appearing. Findings of more severe disease
include hypoxemia, inability to feed, irritability, and lethargy. Young infants may present with
periods of apnea.
17. Do patients with bronchiolitis need chest radiographs?
Generally, infants with classic bronchiolitis do not need any laboratory or radiologic
evaluation. Chest X-ray (CXR) findings are nonspecific and include hyperinflation, a flattened
diaphragm caused by air trapping, perihilar peribronchial infiltrates, and atelectasis. Findings
can be confused with pneumonia and lead to unnecessary use of antibiotics. Children with
atypical presentations or examinations may warrant CXR to rule out other causes of first-time
Figure 62-2. X-ray of lateral neck showing thickening of prevertebral space.
Chapter 62 ACUTE RESPIRATORY DISORDERS IN CHILDREN436
wheezing, including foreign body, congenital airway anomalies, congestive heart failure, or
bacterial pneumonia.
18. When are labs needed for bronchiolitis?
Labs are not routinely indicated for bronchiolitis. Infants older than 1 month with bronchiolitis
are at low risk for serious invasive bacterial infection. Routine complete blood count (CBC),
lumbar puncture, or blood culture is not warranted. Infants with bronchiolitis and fever
continue to be at risk for concurrent urinary tract infection (UTI) and should have a
catheterized urine specimen for culture performed. Management of fever in neonates (younger
than 1 month) with bronchiolitis is unchanged and includes a full septic work-up.
19. What is the treatment for bronchiolitis?
Bronchiolitis treatment is supportive; supplemental oxygen, nasal suctioning, and hydration.
There is no evidence to support the routine use of bronchodilators, steroids, or antivirals in the
ED. Studies addressing the combined use of these agents, as well as nebulized hypertonic
saline, are inconclusive. Children with bronchiolitis and a moderate work of breathing after
nasal suctioning are often trialed with a bronchodilator. Albuterol leads to clinical improvement
in only 20% to 30% of patients, likely those who have a “reactive component” similar to
asthma. Alternatively, albuterol may worsen ventilation/perfusion mismatch and exacerbate
hypoxemia. Nebulized epinephrine may be slightly more effective, likely due to vasoconstrictive
effects; since there is no outpatient equivalent, it should only be used for admitted patients.
KEY POINTS: BRONCHIOLITIS
1. Less than 20% to 30% of infants with bronchiolitis will respond to inhaled b-agonist or
epinephrine therapy. Response should be carefully assessed and treatment continued only
in patients with a clear benefit.
20. Who is admitted for bronchiolitis?
Patients who are hypoxemic, have more than mild respiratory distress, have history of apnea,
or are unable to adequately self-hydrate should be admitted. Admission should be strongly
considered for all children with risk factors for severe disease (Table 62-2). Some centers
utilize home oxygen therapy protocols for otherwise well-appearing patients requiring less
than one half a liter of oxygen per hour. These patients require 24-hour follow-up, as well as
reliable caretaker oversight.
21. How are bronchodilators used in the management of acute asthma?
Selective b
2
agonists are the mainstay of medications to reverse bronchospasm. Delivery of
albuterol by nebulizer or meter-dosed inhaler (MDI) with a spacer has been shown to be
Congenital heart disease
Chronic lung disease (cystic fibrosis, bronchopulmonary dysplasia)
Congenital or acquired immunodeficiency
Major congenital anomalies
Prematurity ,37 weeks
Age ,6–12 weeks
TABLE 62-2. BRONCHIOLITIS: RISK FACTORS FOR SEVERE DISEASE

Chapter 62 ACUTE RESPIRATORY DISORDERS IN CHILDREN 437
equally clinically effective, with 4 to 10 puffs of an MDI equivalent to one nebulizer treatment.
Delivery by nebulizer remains the preferred route in the ED setting for young patients, as well
as those in too much distress to cooperate with MDI use. Albuterol is a racemic mixture of the
R and S isomers of the compound, which have bronchodilatory and bronchoconstrictive
properties. Levalbuterol, the pure R isomer, may cause less tachycardia but has not, in large
clinical trials, been demonstrated to be significantly more effective and is more costly. In
children with moderate-to-severe asthma, inhaled anticholinergic therapy (ipratropium
bromide) decreases severity and hospitalization rates when given in conjunction with b
2
agonists (albuterol).
22. When and how should steroids be administered?
Controlling inflammation is the cornerstone of asthma treatment. There is lack of consensus
regarding the dose and duration of steroid therapy. Generally, a loading dose of prednisone
2 mg/kg (maximum 80 mg) in the ED is followed by a 4-day course of either 1 mg/kg/day as a
single daily dose or 2 mg/kg/day divided twice daily. IV steroids are reserved for children who
cannot tolerate oral medications. Dexamethasone, with its higher potency and longer half-life,
provides an appealing alternative. Multiple small studies have shown that oral dexamethasone
0.6 mg/kg (maximum, 16 mg) given once is equivalent to 5 days of prednisone in children
with mild to moderate asthma symptoms.
23. When should a CXR be obtained? What are the typical findings?
A CXR is not indicated in the routine evaluation of a child with asthma but should be obtained
if pneumonia, pneumothorax, pneumomediastinum, or foreign body is suspected clinically.
CXRs commonly show hyperinflation, atelectasis, and peribronchial thickening, indicating
lower airway obstruction. Pneumothorax is rare. Pneumomediastinum is more common in
older children (age .10 years), whereas infiltrates are more common in younger children.
24. Outline the evaluation and treatment of an asthma exacerbation in the ED.
Step 1. Initial assessment
n
Evaluate vital signs with pulse oximetry, use of accessory muscles, retractions, alertness,
auscultation, and peak expiratory flow rate (PEFR) in patients older than 5 years.
n
Consider an asthma score for objective assessment and later reassessment (Table 62-3).
Step 2. Initial treatment
n
Administer oxygen as needed to keep saturation in the normal range.
n
Administer three consecutive treatments of nebulized albuterol (2.5–5 mg or 0.15 mg/kg
per treatment) plus ipratropium 250 to 500 mg.
n
Administer steroids.
Step 3. Repeat assessment
n
Patient should be assessed after initial treatment to determine if additional treatments are
needed or if they can be observed for potential discharge. Full effect of albuterol may take
15 minutes beyond the end of the treatment.
n
If PEFR is greater than 70% baseline and the patient continues to have no wheezing,
retractions, or accessory muscle use at least 2 hours after the last nebulized treatment,
they can be safely discharged (Step 4a). If symptoms continue, they should be given
additional therapy (Step 4b).
Step 4a. Discharge
n
Discharge home with a reliable caretaker, patient education, medications, and follow-up
instructions.
n
Medications should include albuterol, nebulized or inhaled every 4 hours as needed for
wheezing and oral steroids.
Step 4b. Continued therapy
n
Continuous albuterol by nebulization (7.5–10 mg/h, can increase to 20 mg/h)
n
Ipratropium 500 mg every 4 hours
n
Frequent reassessment of patient
