Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.


Chapter 72 SMOKE INHALATION508
13. Should I get a chest radiograph on all patients with a history of smoke
inhalation?
No. A chest radiograph offers little benefit in the ED. Chest radiographs are normal
immediately after smoke inhalation injury, and abnormalities appear only on a delayed basis.
A chest radiograph is not indicated in asymptomatic patients, and in most instances, it is
useful only as a baseline in symptomatic patients.
14. Can I use the standard burn formula for intravenous fluids if smoke inhalation
is present?
Patients with cutaneous and inhalation injuries pose a difficult problem because their fluid
requirements are usually greater, but because of leaky capillaries, they are much more likely to
develop membrane permeable pulmonary edema. Intravenous fluids must be guided by
regular clinical reevaluation (i.e., breath sounds, oxygen saturation, urinary output, vital signs)
rather than by formulas. Swan-Ganz monitoring may be required.
15. Is HBO therapy the only available therapy for cyanide poisoning?
No. Either the Lilly cyanide antidote kit or hydroxocobalamin (Cyano kit) can be used for
victims of cyanide toxicity.
16. Tell me about hydroxocobalamin.
Hydroxocobalamin (vitamin B
12
) reduces cyanide concentrations by combining with cyanide to
form cyanocobalamin. It can be considered for victims who are comatose, in cardiac arrest, or
have clear signs of cardiovascular extremis. If hydroxocobalamin is used, it should be given
as early as possible. The usual dose is 5 g intravenously (IV).
17. How does the Lilly cyanide antidote kit work?
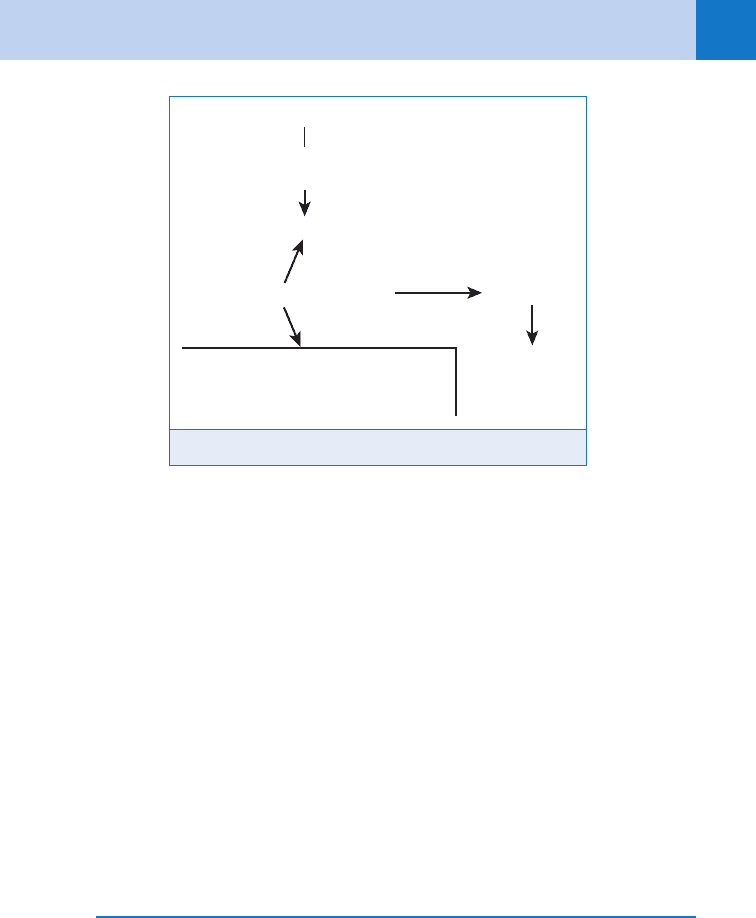
Cyanide binds to the ferric ions, blocking the mitochondrial cytochrome oxidase pathway and
cellular respiration. The cyanide antidote kit acts in two ways to limit this:
n
Nitrites generate methemoglobin, creating heme-ferric ions to compete with cyanide with
mitochondrial ferric ions
n
Sulfur transferase (rhodanese) binds cyanide molecules to sulfur-forming thiocyanate,
which is nontoxic and eliminated in the urine. Thiosulfate accelerates this process by
increasing available sulfur molecules. (Fig. 72-1.)
18. When should I use the cyanide antidote kit?
Symptomatic patients can have CO or cyanide toxicity. Nitrites can cause more prolonged
asphyxia in patients with hypoxemia and elevated carboxyhemoglobin (COHb) fractions.
These drugs should be reserved for patients in extremis or who remain critically ill after
intubation and 100% oxygenation. The sodium thiosulfate portion of the kit can be used
safely even when the measured oxygen saturation is low. High lactate levels can help
distinguish cyanide from CO because elevations in serum lactate correlate well with
cyanide toxicity.
KEY POINTS: SMOKE INHALATION
1. Obtain CO level and treat any patient who has inhaled smoke in an enclosed space with
nonrebreather high-flow mask oxygen.
2. Consider cyanide poisoning when the patient inhaled smoke from burning furniture fabric
(e.g., wool, silk, or polyurethanes).
Chapter 72 SMOKE INHALATION 509
19. How do I administer the cyanide antidote kit?
Administer a dose of 12.5 g of intravenous sodium thiosulfate. Amyl nitrite inhalers in patients
in extremis without intravenous access can be given every 3 to 4 minutes. If a patient is
apneic, break one of the amyl nitrite inhalants inside the resuscitation bag. When an
intravenous line is established and indications for nitrites are present, the full amount of a
10-mL ampule or 5 to 10 mg/kg of sodium nitrite should be administered IV over 4 minutes.
20. Why is CO so dangerous?
CO is a colorless, odorless gas that has a 210 times greater affinity for hemoglobin than does
oxygen. Even when exposed to low levels, it accumulates resulting in impaired cellular oxygen
utilization. Fetal hemoglobin has an even greater affinity for CO.
21. How do I make the diagnosis in the ED?
The obvious history of any exposure to fire or smoke in a confined space. The more subtle
presentation is early morning headache, which improves after exiting a residence with a
defective heating system. A CO level should be obtained on all patients in whom the diagnosis
is considered.
CONTROVERSY
22. Isn’t the early respiratory failure seen in smoke inhalation victims worsened
by aggressive crystalloid resuscitation?
Respiratory failure from interstitial fluid accumulation is a rare event. When it occurs, it is
caused by capillary leakage due to inflammation of pulmonary tissue. The amount of
crystalloid used during resuscitation does not increase the risk or the severity of the resultant
pulmonary edema. Fluids should not be withheld in a patient with severe cutaneous and
respiratory burns.
23. How do I treat CO poisoning?
All patients should be placed on high-flow O
2
via a nonrebreather bag reservoir mask, which
will reduce the half-life of CO from 4 to 5 hours on room air to 1 hour. Although the long-term
Figure 72-1. Lilly cyanide antidote kit.
ThiocyanateSulfurCyanide
Renal
elimination
+
Rhodanase
(Methemoglobin)
3 Sodium Thiosulfate
1 Amyl nitrate
2 Sodium nitrate
Heme-Fe
+++
Heme-Fe
++
Cyanide Antidote Kit
Fe
+++
Mitochondrial cytochrome oxidase
Cellular anoxia
Chapter 72 SMOKE INHALATION510
benefit of HBO therapy has been called into question with conflicting published studies, most
still recommend its use in the following patients:
n
A pregnant woman with a CO level greater than 15
n
Any patient with a neurologic abnormality (i.e., coma or altered momentum)
n
Any patient with cardiac ischemia or instability
BIBLIOGRAPHY
1. Blinn DL, Slater H, Goldfarb W: Inhalation injury with burns: a lethal combination. J Emerg Med 6:471–473,
1988.
2. Cohen MA: Inhalation of products of combustion. Ann Emerg Med 12:628–631, 1983.
3. Erdman AR: Is hydroxocobalamin safe and effective for smoke inhalation? Searching for guidance in the haze.
Ann Emerg Med 49:814–816, 2007.
4. Hampson N: Hyperbaric Oxygen Therapy Committee: Hyperbaric oxygen therapy. 1999. Committee report.
Kensington, MD, 1999, Undersea and Hyperbaric Medical Society.
5. Holm C, Tegeler J, Mayr M: Effect of crystalloid resuscitation and inhalation injury on extravascular lung
water: clinical implications. Chest 121:1956–1962, 2002.
6. Kirk MA, Gerace R, Kulig KW: Cyanide and methemoglobin kinetics in smoke inhalation victims treated with
the cyanide antidote kit. Ann Emerg Med 22:1413–1418, 1993.
7. Miller K, Chang A: Acute inhalation injury. Emerg Med Clin North Am 21:573–577, 2003.
8. Murphy SM, Murray D, Smith S, et al: Burns caused by steam inhalation for respiratory tract infections in
children. BMJ 328:757, 2004.
9. Nelson LS, Hoffman RS: Inhaled toxins. In Rosen’s emergency medicine: concepts and clinical practice, ed 7,
St. Louis, 2009, Mosby, pp 2031–2038.
10. Ramzy PI, Barret JP, Herndon DM: Thermal injury. Crit Care Clin 15:333–352, 1999.
11. Stewart RJ, Mason SW, Taira MT, et al: Effect of radical scavengers and hyperbaric oxygen on smoke-induced
pulmonary edema. Undersea Hyperb Med 21:21–30, 1994.
511
COMMON DRUGS OF ABUSE
CHAPTER 73
Vikhyat S. Bebarta, MD
1. Aren’t the occurrences of heroin and other opioid abuse decreasing in
frequency?
Actually, it is just the opposite. The data collected by the American Association of Poison
Control Centers (AAPCC) demonstrated an increase from 5% to 13% in opioid-related deaths
from 1995 to 2003. Analgesics (opioids and non-opioids) are the most common killer in toxic
ingestions of pharmaceuticals every year since 1995. Opioids represent approximately half
of those deaths each year. The Drug Abuse Warning Network in the United States showed a
25% increase in ED visits involving heroin from 1998 to 2002.
2. What do the terms opium, opiate, opioid, and narcotic mean?
n
Opium is a mixture of alkaloids, including morphine and codeine, extracted from the opium
poppy.
n
An opiate is a natural drug derived from opium (e.g., heroin, codeine, and morphine).
n
An opioid is any drug that has opium-like activity, including the opiates and all synthetic
and semisynthetic drugs that interact with opioid receptors in the body (e.g., hydrocodone
and oxycodone).
n
The term narcotic is nonspecific; it refers to any addictive drug that reduces pain, alters
mood and behavior, and usually induces sleep or stupor and more specific to law
enforcement than medicine.
3. What is the typical clinical presentation of opioid poisoning?
The classic triad of opioid poisoning is central nervous system (CNS) depression,
respiratory depression, and miosis. Patients who have overdosed on opioids are hyporeflexic
and have decreased bowel sounds. They may be hypothermic, cyanotic, and mildly
hypotensive and bradycardic.
4. Do all opioid intoxication cases present with miosis?
No. Mydriasis or normal pupils can occur with:
n
Intoxication of specific synthetic opioids (i.e., meperidine, propoxyphene, or pentazocine)
n
Diphenoxylate-atropine (Lomotil)
n
After naloxone use
n
With hypoxia
n
With mydriatic eye drops use
n
Coingestion of other mydriatic drugs (e.g., anticholinergics)
n
Occasionally, phenylephrine, instilled into the patient’s nares by paramedics for nasal
intubation, may spill into the patient’s eyes causing mydriasis (Table 73-1).
5. How should a patient with respiratory compromise from opioid overdose
be treated?
Resuscitation takes precedence over naloxone administration. Support the patient’s ventilation
with a bag-mask until the opioid antagonist is administered. Intubate the apneic or cyanotic
patient if the patient does not awaken after naloxone. Obtain a serum glucose level, administer
oxygen, and consider thiamine administration in the patient with altered consciousness.
Administer activated charcoal if the opioid ingestion was recent.
Chapter 73 COMMON DRUGS OF ABUSE512
6. What is the appropriate naloxone dose?
For children younger than 5 years old or less than 20 kg, administer 0.1 mg/kg intravenously.
In a patient who has CNS depression only, infuse an initial dose of 0.2 to 0.4 mg
intravenously. If there is no response to this dose, repeated doses up to 2 mg can be given.
Administer 2 mg intravenously initially for the apneic or cyanotic adult or child. For patients
who abuse opioids or who use opioids for chronic pain, infuse 0.1 mg to wake the patient
without inducing opioid withdrawal. Additional doses should be given judiciously to patients
who consume opioids chronically. Opioid withdrawal is unpleasant to the patient but is not
life-threatening.
7. Can naloxone be administered by other routes besides intravenously?
Yes. If venous access cannot be accomplished, administer the naloxone intramuscularly or
subcutaneously. A dose of 0.8 mg subcutaneously has an equal time to effect as 0.4 mg
intravenously. Naloxone can also be administered through the endotracheal tube, intranasally,
intraosseously, or injected sublingually. Naloxone is not effective orally because of significant
first pass metabolism.
8. Do all patients respond to a standard dose of naloxone?
No. Larger doses of naloxone may be required to reverse the effects of synthetic opioids, such
as codeine, diphenoxylate-atropine (Lomotil), propoxyphene (Darvon), pentazocine (Talwin),
codeine, dextromethorphan, and the fentanyl derivatives. If an opioid overdose is suspected
and the patient does not respond to an initial naloxone dose, repeat additional doses until a
response is noted or until 10 mg has been given. If there is no response to 10 mg of
naloxone, it is unlikely to be an isolated opioid overdose.
9. How long does the clinical effect of naloxone last?
The duration of action of intravenous naloxone is 40 to 75 minutes, although the serum half-
life is shorter. Many oral and some injected opioids produce clinical effects that last for 3 to
6 hours. Although the duration of action of most opioids is much longer than that of naloxone,
resedation is uncommon, particularly with short-acting parenteral opioids (e.g., heroin). Most
oral opioids, particularly long-acting agents (e.g., methadone or sustained release morphine)
last several hours and may require additional naloxone doses and hospital admission.
10. How should recurrent sedation and respiratory depression resulting from a
long-acting opioid be treated?
Treat most patients with boluses of naloxone as needed, along with hospital admission,
supplemental oxygen, and close monitoring in an intensive care setting. On occasion, patients
require several doses of naloxone over a short time interval to maintain normal oxygenation.
In these cases, a continuous naloxone infusion may be started. A naloxone infusion is
administered at an hourly rate that provides two thirds of the dose needed to reverse the
respiratory depression. Thus, multiply the bolus dose being given by 6.6, mix it into one liter
of crystalloid, and infuse it at 100 mL/h. The infusion can be adjusted based on the patient’s
symptoms of withdrawal or sedation.
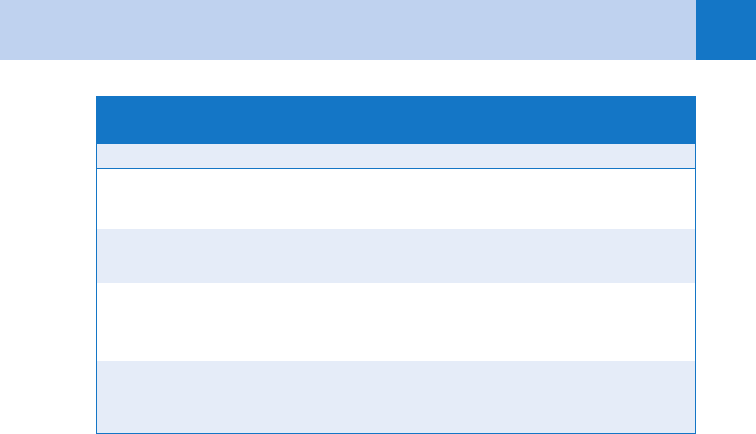
Sympatholytic agents Clonidine, antipsychotics, oxymetazoline, and tetrahydrozoline
Cholinergic agents Organophosphates, carbamates, nicotine, pilocarpine,
phencyclidine, and similar congeners
Miscellaneous Pontine infarct and Horner’s syndrome
TABLE 73-1. COMMON CAUSES OF NONOPIOID-RELATED MIOSIS
Chapter 73 COMMON DRUGS OF ABUSE 513
11. Should naloxone be administered empirically to every patient with altered
mental status?
No. Although naloxone is a safe medication, the response to naloxone has been shown
to occasionally cloud the diagnostic picture. If a patient presents with an obvious
sympathomimetic or anticholinergic syndrome (i.e., agitated and stimulated), the patient
will not benefit from naloxone. In addition, if the opioid toxidrome is obvious and the patient’s
ventilatory status is adequate, naloxone may stimulate opioid withdrawal, which is more
difficult to control in a busy ED than a slightly sedated patient.
12. Who should be observed in the ED, and for how long?
It depends. Patients who inject heroin can be observed for at least 2 hours after a dose of
naloxone, as resedation and noncardiogenic pulmonary edema almost always occur during this
period. Most consider observation for up to 4 hours after the last dose of naloxone adequate in
an asymptomatic patient who used a parenteral opioid. This extended period may allow for
recognition of coingestants and recurrent respiratory depression. Occasionally, patients who
have inadequate ventilation, which necessitates treatment, or who develop complications of
opioid use must be admitted. Patients who ingest long-acting opioids, such as methadone, may
require admission for 24 hours or longer. Patients who inject long-acting opioids should be
observed for 4 to 8 hours or admitted. Patients should be normoxic off oxygen, awake, and
ambulatory before discharge, and preferably discharged into the care of a competent adult.
13. What are the signs of opioid withdrawal?
Signs of withdrawal include anxiety, yawning, lacrimation, rhinorrhea, diaphoresis, mydriasis,
nausea and vomiting, diarrhea, piloerection, abdominal pain, and diffuse myalgias. Opioid
withdrawal typically occurs approximately 12 hours after last heroin use and 30 hours after
last methadone use. Seizures, dysrhythmias, and other life-threatening complications are not
consistent with opioid withdrawal.
14. How is opioid withdrawal best treated?
Treatment is symptomatic. Intravenous fluids, sedation, antiemetics, and antidiarrheal agents
are mainstays of treatment. Clonidine, 0.1 to 0.2 mg orally, may also be helpful. However,
published cases describe a concomitant abuse of clonidine, because the user feels it enhances
the opioid euphoria. If naloxone is given, the most severe withdrawal symptoms typically
resolve in 45 to 75 minutes.
15. What are body packers and stuffers?
n
Body packers are individuals who carefully pack large amounts of illegal drugs into small,
glass, or plastic vials. The vials are sealed and ingested by the human carrier along with an
antimotility agent. The individual then travels by plane or other vehicle to another location.
Body packing is used to transport illegal drugs, such as heroin or cocaine to other
countries. The individual then defecates the vials and delivers them to the recipient.
The packets rarely rupture, but it can be life-threatening if they do.
n
Body stuffers are individuals who quickly ingest (stuff) poorly wrapped illegal drugs while
attempting to evade law enforcement. The wrapping containing the drug is usually referred
to as a baggie. Commonly it is a much smaller amount of drug than body packers handle
and is loosely wrapped. The drug is typically absorbed quickly, and the patient usually
develops symptoms shortly after ingestion.
16. How should body stuffers/packers be managed?
Urine drug screening is not helpful for determining which drug or if any drug was
ingested. In addition, the patient’s history for timing, content, and amount of the ingestion
is unreliable.
n
Body stuffers should receive activated charcoal and be observed in a monitored setting for
at least 8 hours. Radiographs are not helpful. If the patient develops symptoms, admit the
patient to an intensive care setting for observation.
Chapter 73 COMMON DRUGS OF ABUSE514
n
The packets from body packers can be seen on plain abdominal radiographs, radiographs
with oral contrast material (Gastrografin), or abdominal computed tomography (CT). Based
on limited data, contrasted radiographs and CT scan are the most sensitive. Body packers
should receive activated charcoal and polyethylene glycol electrolyte solution (Colyte,
GoLYTELY) to enhance elimination through the colon. Polyethylene glycol may be
administered through a nasogastric tube at approximately 2 L/h until all packets have
cleared. Clear rectal effluent is not a sufficient end point to end decontamination. Repeat
radiologic testing with abdominal CT or a radiograph with oral contrast should be used to
determine when all packets have cleared. Enemas may be used if the packets are in the
distal colon or are felt on digital rectal examination. Typically, bowel irrigation for more than
6 hours is futile in moving stubborn vials. Surgery is rarely needed to remove retained
packets. Occasionally, packets may take days to evacuate.
17. How useful are toxicologic screens for opioids, and which opioids are not
often detected?
Toxicologic screens are not generally helpful in acute management. Not only are the results
delayed, but the clinical presentation is also more helpful than the insensitive test. Opiate
screens do not detect methadone or other synthetic opioids, such as fentanyl, pentazocine,
meperidine, oxymorphone, oxycodone, and propoxyphene. Ingestion of poppy seeds does not
commonly cause a positive screen because the lower limit threshold has been raised.
However, with further testing, this erroneous cause of positive screens can be excluded.
Fluoroquinolones can cause a false-positive for opiates.
18. Are there any other tests that should be checked in patients with opioid
ingestions?
Obtain acetaminophen levels in all patients because it is often combined with hydrocodone,
oxycodone, propoxyphene, and codeine. Also obtain a metabolic panel, salicylate level, and
electrocardiogram.
19. What is the most common pulmonary complication of opioid use?
Noncardiogenic pulmonary edema occurs in 3% of nonhospitalized opioid intoxications. The
mechanism is unclear, but it may be a result of capillary permeability and fluid leak, or from
breathing deeply and quickly against a closed glottis. The patient presents with pink frothy
sputum, cyanosis, and rales. Bilateral alveolar infiltrates are seen on the chest radiograph.
Naloxone does not reverse the process, and many patients will need mechanical ventilation.
Heroin, methadone, morphine, and propoxyphene have been associated with noncardiogenic
pulmonary edema.
20. Can opioids cause seizures?
Seizures are rare in patients with therapeutic doses of opioids, but they have been reported
with use of synthetic opioids (i.e., meperidine, tramadol, pentazocine, and propoxyphene) and
chronic use of morphine.
21. Is it safe to give dextromethorphan or meperidine to patients on
antidepressant medications?
The combination of these opioids with antidepressants may precipitate serotonin syndrome.
Meperidine and dextromethorphan inhibit serotonin reuptake similar to selective serotonin
reuptake inhibitors. A combination of these opioids and monoamine oxidase inhibitors
(MAO-Is) is also contraindicated as MOA-Is decrease serotonin metabolism.
22. Why should I avoid prescribing meperidine (Demerol)?
The duration of action of meperidine is only 2 to 3 hours, shorter than morphine or
hydromorphone. In contrast to morphine, meperidine’s half-life is prolonged by hepatic
disease, resulting in toxic effects after repeated doses in patients with liver disease. Seizures
are an adverse effect of normeperidine, a renally cleared metabolite of meperidine.
Normeperidine levels are elevated with repetitive administration of oral meperidine, renal

Chapter 73 COMMON DRUGS OF ABUSE 515
failure, and concomitant use of drugs that induce hepatic enzymes, such as phenytoin,
phenobarbital, and chlorpromazine. Naloxone does not terminate the seizures. Normeperidine
can cause CNS agitation, tremors, and psychosis. Meperidine can produce serotonin
syndrome when combined with other serotonergic agents.
23. Which antidiarrheal agent can cause significant toxicity if ingested?
Lomotil (diphenoxylate 2.5 mg 1 atropine 0.025 mg). Most toxic cases occur in children.
Classically the overdose is a two-phase toxicity: Phase 1, anticholinergic symptoms (flushing,
dry mouth) and Phase 2, opioid effects. However, this pattern is uncommon. Delayed
presentations have been reported, and all children should be observed in a monitored setting
for at least 24 hours.
Loperamide is a nonprescription antidiarrheal agent derived from diphenoxylate. Acute
overdoses usually produce only mild drowsiness.
24. Which opioid can produce ventricular dysrhythmias, a wide QRS complex,
mydriasis, and seizures?
Propoxyphene has a quinidine-like effect that blocks sodium channels, similar to cyclic
antidepressants. Large doses of naloxone (10 mg) may reverse the CNS depression, but not
the cardiotoxic effects. Sodium bicarbonate has been used successfully for propoxyphene-
induced dysrhythmias. Propoxyphene is no more effective for analgesia than salicylates,
acetaminophen, or codeine.
25. What are designer drugs, and what are the two most notorious designer drugs
that have been used?
Designer drugs are substitutes for other chemicals or drugs that are popular with illicit drug
users. They are made inexpensively in clandestine laboratories. 3-Methylfentanyl is an analog of
fentanyl known as China white or Persian white. It is 2,000 times more potent than morphine and
20 times more potent than fentanyl. It can cause respiratory compromise quickly. It does not
cause the abbreviated rush of heroin, but instead causes a longer duration of euphoria.
MPTP (1-methyl-4-phenyl-1,2,5,6 tetrahydropyridine) is a compound that was produced
accidentally during the synthesis of MPPP, a meperidine analog. MPTP is cytotoxic for
dopaminergic neurons in the substantia nigra. It produces a Parkinson-like syndrome that is
permanent and occurs after a single ingestion of MPTP. The symptoms do not respond to
typical anti-Parkinsonism medications.
26. What over-the-counter cold remedy is sometimes abused by teenagers?
Dextromethorphan (DM) is the d-isomer of codeine. Its metabolite stimulates the release of
serotonin and acts at the phencyclidine receptor site, which accounts for its abuse as a
hallucinogen. While Coricidin is the trade name most well known, DM is available in many
other cough medications. It is also known as ROBO, DEX, red devils, triple C, CCC, and
skittles. DM toxicity may present with symptoms of opioid toxicity but more commonly
presents with slurred speech, nystagmus, hyperexcitability, vomiting, and ataxia. Not all
individuals can metabolize dextromethorphan to its psychoactive metabolite. Naloxone does
not usually reverse the symptoms of toxicity. DM does cause false positive phencyclidine
results on urine screening, but it usually does not produce positive results for opiates.
Coingredients may cause a predominance of that clinical syndrome (anticholinergic or
sympathomimetic toxidrome). Acetaminophen is commonly a coingredient and should be
screened for in all patients abusing DM.
27. Name another analog of codeine.
Tramadol (Ultram) is a synthetic analog of codeine. The usual effects with overdose are mild
sedation and opioid effects. Overdoses have occasionally been associated with seizures,
hypertension, respiratory depression, and agitation. The seizures do not respond to naloxone.
Although the drug has a low abuse potential, it is not recommended for patients with an
opioid dependence history.
Chapter 73 COMMON DRUGS OF ABUSE516
SEDATIVE-HYPNOTICS
28. What is a sedative-hypnotic?
Sedatives-hypnotics are drugs that primarily cause relaxation and tranquilization and induce
drowsiness and sleep. There is no consistent structural relationship among the agents of this
group. In sufficient quantities all drugs of this group result in CNS depression.
29. What medications fall into this category?
There are three groups: benzodiazepines, barbiturates, and miscellaneous. Some examples of
miscellaneous sedative-hypnotics are chloral hydrate, ethanol, and gamma-hydroxy butyrate
(GHB). Many of the miscellaneous agents are also pharmaceutical agents. For example,
ethanol is used in the treatment of methanol and ethylene glycol toxicity and GHB (Xyrem) is
used for narcolepsy. These drugs are also commonly abused.
30. What is a typical presentation of sedative hypnotic intoxication?
Mild intoxication presents with slurred speech, ataxia, and loss of coordination. Moderate to
severe intoxication presents with greater CNS depression. Respiratory depression may occur
with large ingestions, and is compounded by other agents that suppress respiratory drive,
such as opioids or ethanol. Pupils are usually midsize and reactive, and may be disconjugate.
There are also symptoms specific to individual drugs. Some examples are choral hydrate
(pear odor), ethchlorvynol (pulmonary edema, vinyl odor), and glutethimide (anticholinergic
effects) (Table 73-2).
31. Don’t many overdoses present this way?
Many overdoses present with CNS depression. However, some intoxications also present with a
pattern of symptoms known as a toxidrome (Table 73-3). Signs of antipsychotic intoxication
include sedation and are similar to sedative-hypnotics but also commonly include tachycardia,
mild hypotension, and occasionally miosis. CNS depression is also a common presentation of
illness other than intoxication. Maintain a broad differential while evaluating these patients for
such illnesses as meningoencephalitis, intracranial hemorrhage, hypoglycemia, shock, and sepsis.
32. How do sedative-hypnotics cause CNS depression?
Most sedative-hypnotics, particularly benzodiazepines and barbiturates, cause CNS depression
by enhancing the effects of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter
in the brain. Benzodiazepines increase the frequency of the opening of chloride channels
associated with GABA. Propofol and barbiturates directly open the chloride channels,
potentially causing greater sedation and respiratory suppression. Propofol may also inhibit
excitatory brain neurotransmitters, adding to the GABA effects.
Chloral Hydrate Vomiting and ventricular dysrhythmias
Ethchlorvynol Vinyl-like odor on breath, prolonged coma, and
noncardiogenic pulmonary edema
Glutethimide Cyclic coma, anticholinergic symptoms (tachycardia
uncommon), and thick secretions
Methaqualone Hyperreflexia, clonus, and muscle hyperactivity
Meprobamate/Carisoprodol Euphoria and concretions in stomach may be seen on
radiographs
TABLE 73-2. CLINICAL PRESENTATIONS OF LESS COMMON SEDATIVE-HYPNOTICS
Chapter 73 COMMON DRUGS OF ABUSE 517
33. How do I make the diagnosis of sedative/hypnotic overdose in a patient with
undifferentiated CNS depression?
Making the diagnosis can be difficult. Elicit help from friends, family, and involved prehospital
providers and police. Review the patient’s medical records for previous visits and search the
belongings for paraphernalia and empty bottles. Often a specific agent will not be identified;
rather, only a constellation of symptoms seen with sedative hypnotic intoxication may be
recognizable. Routine laboratory and radiologic studies including chemistries, cerebrospinal
fluid analysis, and cranial CT scans may assist in ruling out metabolic, infectious, and CNS
disorders as the cause. Urine drug screens are available, but typically are not helpful.
34. Is there a role for drug screens or specific drug levels?
Routine drug screens are often not useful in acute patient management. The sensitivities and
specificities of the assays for detecting specific drugs are variable. For example, the assay for
benzodiazepines in the most commonly used urine drug screen is designed only to detect the
metabolite of some older, long-lasting benzodiazepine medications. Many newer benzodiazepines
will not be detected. The same is true for many barbiturates. Most sedative-hypnotics are not
tested for on the routine urine drug screen and thus their use cannot be excluded. If the screen
is positive, it only indicates use within the past several days and may not correlate with clinical
presentation. Other agents can cause a false-positive result and lead to missing the true etiology
for the altered mental status. In addition, many other chemicals and drugs cause altered mental
status but will not be present on urine toxicology screening (e.g., jimson weed, isopropanol,
inhalant toxicity, lithium, ketamine, chloral hydrate, and bromides).
Because the most important treatment in sedative-hypnotic intoxication is supportive care,
recognizing the intoxication pattern is more helpful than toxicology testing.
35. What is the treatment for sedative-hypnotic overdose?
Rapid resuscitation is the initial treatment. Manage the patient’s airway, assess the respiratory effort
and oxygenation, evaluate the circulation and perfusion, and examine for neurological deficits
(ABCDs). After resuscitation, initiate gastrointestinal decontamination with activated charcoal (within
approximately 1 hour of ingestion) and then exclude other causes for altered mentation, acid-base
disturbances, or unstable hemodynamics. Do not use flumazenil in the undifferentiated intoxication.
36. How do patients die of sedative-hypnotic overdose?
Respiratory depression and resultant hypoxia is the cause of most deaths.
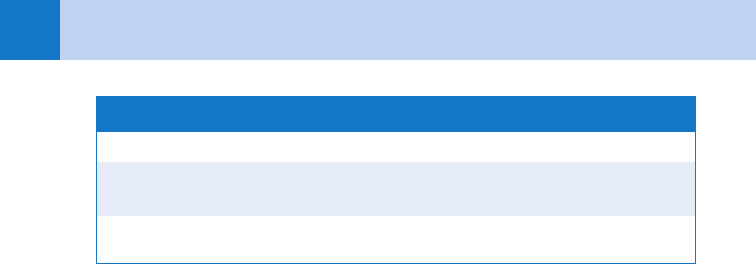
Toxidrome Presentation
Opioid Central nervous system depression, miosis, respiratory
depression, hypothermia, and mild bradycardia
Sympathomimetic Psychomotor agitation, mydriasis, hypertension, tachycardia,
diaphoresis, hyperthermia, and seizure
Cholinergic Bradycardia, bronchorrhea, miosis, salivation, lacrimation,
urination, diaphoresis, diarrhea, vomiting, diarrhea, altered
mental status, and seizures
Anticholinergic Delirium, sedation, mydriasis, dry/flushed skin, tachycardia,
decreased/absence of bowel sounds, seizures, and mild pyrexia
TABLE 73-3. CLINICAL PRESENTATION OF TOXIDROMES RESULTING IN DEPRESSED OR ALTERED
MENTAL STATUS
