Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 69 THE ALCOHOLS: ETHANOL, ETHYLENE GLYCOL, METHANOL, AND ISOPROPYL ALCOHOL488
KEY POINTS: ISOPROPANOL
1. Symptoms and toxicity are completely different from methanol and ethylene glycol.
2. Ketosis occurs, but acidosis does not.
3. Supportive treatment is adequate in almost all cases.
BIBLIOGRAPHY
1. Caravati EM, Erdman AR, Christianson G, et al: Ethylene glycol exposure: an evidence-based consensus
guideline for out-of-hospital management. Clin Toxicol 43(5):327–245, 2005.
2. D’Onofrio G, Rathlev NK, Ulrich AS, et al: Lorazepam for the prevention of recurrent seizures related to
alcohol. N Engl J Med 341:609–610, 1999.
3. Glaser DS: Utility of the serum osmol gap in the diagnosis of methanol or ethylene glycol ingestion. Ann
Emerg Med 27:343–346, 1996.
4. Hovda KE, Andersson KS, Urdal P, et al:. Methanol and formate kinetics during treatment with fomepizole.
Clin Toxicol 43(4):221–227, 2005.
5. Mayo-Smith MF: Pharmacological management of alcohol withdrawal: a meta-analysis and evidence-based
practice guideline. JAMA 278:144–151, 1997.
6. McDonald AJ, 3rd, Wang N, Camargo CA, Jr: US emergency department visits for alcohol-related diseases
and injuries between 1992. and 2000. Arch Intern Med 164:531, 2004.
7. Paasma R, Hovda KE, Tikkerberi A, et al:. Methanol mass poisoning in Estonia: outbreak in 154 patients. Clin
Toxicol 45(2):152–157, 2007.
8. Rathlev NK, Ulrich A, Shieh TC, et al: Etiology and weekly occurrence of alcohol-related seizures. Acad Emerg
Med 9:824, 2002.
9. Shale JH, Shale CM, Mastin WD: A review of the safety and efficacy of droperidol for the rapid sedation of
severely agitated and violent patients. J Clin Psychiatry 64:500, 2003.
10. Wiese JG, Shlipak MG, Browner WS: The alcohol hangover. Ann Intern Med 132:897–902, 2000.
ACKNOWLEDGMENT
The editors gratefully acknowledge the contributions of John A. Marx, MD, author of this chapter in
the previous edition.
489
ANTIPYRETIC POISONING
CHAPTER 70
James C. Mitchiner, MD, MPH
SALICYLATE POISONING
1. What are the causes of salicylate overdose?
A salicylate overdose may be intentional or accidental. Parental administration of adult doses
of aspirin to a child may cause toxicity. Bismuth subsalicylate (Pepto-Bismol), which contains
130 mg/tablespoon of salicylate, is occasionally the culprit. In adults, concurrent ingestion
of aspirin and aspirin-containing prescription or non-prescription medications may lead
to unintentional overdose with possible formation of gastric concretions. Liquid methyl
salicylate (oil of wintergreen) is especially toxic because of its high salicylate content
(1 teaspoon 5 7 g of salicylate) and rapid absorption. Dermal application of salicylic acid
ointment is a rare cause of acute salicylism. The minimal acute toxic ingestion is 150 mg/kg.
2. What are the characteristics of a patient who presents with an acute salicylate
overdose?
Patients may present with nausea, vomiting, tinnitus, vertigo, fever, diaphoresis, and
confusion. Hyperventilation may be ascribed mistakenly to anxiety. Patients also may present
with headache or chronic pain, which prompted the excess ingestion of salicylate.
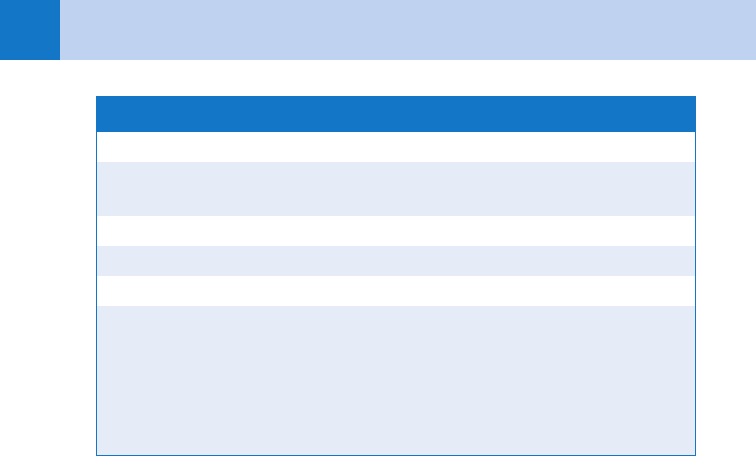
3. List some common signs of salicylate intoxication.
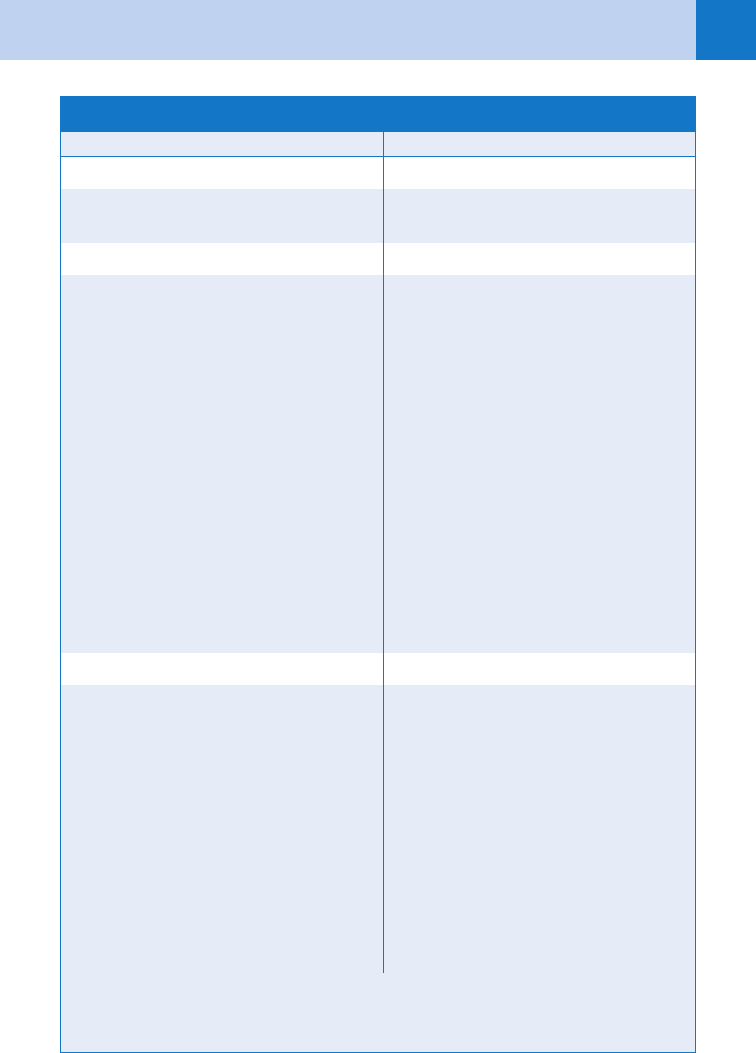
See Table 70-1.
4. Describe the acid-base disturbances associated with salicylate toxicity.
Acute respiratory alkalosis, without hypoxia, is due to salicylate stimulation of the respiratory
center. If the patient is hypoxic, salicylate-induced noncardiogenic pulmonary edema should be
considered. Within 12 to 24 hours after ingestion, the acid-base status in an untreated patient
shifts toward an anion gap metabolic acidosis. A mixed respiratory alkalosis and metabolic
acidosis typically is seen in adults. In patients presenting with respiratory acidosis, concomitant
ingestion of a central nervous system depressant should be suspected. Metabolic acidosis is the
predominant acid-base disturbance in children, patients who take massive amounts of salicylates,
hemodynamically unstable patients, and patients of all ages who have chronic salicylate toxicity.
5. What are some of the other metabolic disturbances seen in acute salicylate
poisoning?
The patient may be dehydrated secondary to vomiting, the diuretic effects of increased renal
sodium excretion, or diaphoresis in response to the hyperpyrexic state. Insensible losses are
increased in patients with hyperventilation. Hypokalemia is due to renal potassium excretion
and respiratory and metabolic alkalemia (secondary to bicarbonate therapy).
6. I thought aspirin was an antipyretic. How does it cause a fever?
At a cellular level, salicylate poisoning leads to the uncoupling of oxidative phosphorylation.
When this occurs, the energy obtained from oxygen reduction and reduced nicotinamide
adenine dinucleotide oxidation that is normally captured in the form of adenosine triphosphate
(ATP) instead is released as heat.
Chapter 70 ANTIPYRETIC POISONING490
7. Name some of the hematologic abnormalities.
These are rare in an acute overdose. Features include decreased production of prothrombin
(factor II) and factor VII, an increase in capillary endothelial fragility, and a decrease in the
quantity and function of platelets (i.e., decreased adhesiveness). Significant hemorrhage is
unusual.
8. How is the severity of salicylate overdose assessed?
Salicylate levels should be obtained at the time of initial ED evaluation and repeated several
hours apart, while the patient is still under observation in the ED, so that the severity of
poisoning can be trended. The aspirin (Done) nomogram is of historic interest only and is
no longer recommended.
9. Which laboratory tests are indicated?
Serial serum salicylate levels (initial and 6 hours postingestion) should be obtained, along
with a complete blood cell count, serum electrolytes, blood urea nitrogen (BUN), creatinine,
glucose and a urinalysis. Prothrombin time (PT), international normalized ratio (INR), and
arterial blood gases should be considered. If the patient presents less than 6 hours after an
acute ingestion, a salicylate level should be repeated at 6 hours. A quantitative acetaminophen
level is also recommended because many patients confuse these two drugs or mix both kinds
in the same bottle.
10. What is the initial ED treatment for an acute salicylate overdose?
If poisoning is through dermal contact, the skin should be washed copiously with tap water.
For acute ingestions, intravenous normal saline should be given initially, with conversion to
alkaline diuresis if the patient is toxic. A slurry of activated charcoal mixed with cathartic
(sorbitol or magnesium sulfate) should be given orally or by gastric lavage tube at a dose of
1 g of charcoal per kg. Lavage may be useful even if the patient presents several hours after
ingestion because large amounts of aspirin may form gastric concretions with ongoing
absorption.
11. What else needs to be done in the ED?
After the patient has responded with diuresis, potassium losses should be replaced with
potassium chloride at a dose of 20 to 40 mEq/L. Patients with hyperthermia should be cooled
with a cooling blanket. Hypoglycemia should be treated with intravenous D50. Patients with
aspirin-induced noncardiogenic pulmonary edema should be treated with oxygen, noninvasive
CK, creatine kinase.
General Hyperthermia, dehydration
Respiratory Hyperventilation (may be mistaken for anxiety), noncardiogenic
pulmonary edema
Central nervous system Confusion, delirium, seizures, coma
Gastrointestinal Nausea, vomiting, gastrointestinal hemorrhage
Dermatologic Eyelid petechiae
Laboratory Acid-base disturbances, azotemia, hyperkalemia or hypokalemia,
hypoglycemia (children), elevated CK levels (rhabdomyolysis),
coagulopathy
TABLE 70-1. COMMON SIGNS OF ACUTE SALICYLATE TOXICITY

Chapter 70 ANTIPYRETIC POISONING 491
ventilation (continuous positive airway pressure [CPAP] or bi-level positive airway pressure
[BiPAP]), or intubation and positive end-expiratory pressure (PEEP). If possible, sedation
should be avoided because of the risk of respiratory depression leading to respiratory
acidosis and exacerbation of central nervous system toxicity.
12. Is there a role for repetitive dosing of activated charcoal?
Because of aspirin release from the aspirin-charcoal complex in the gastrointestinal tract and
subsequent reabsorption, salicylate levels may not decline significantly after a single dose of
activated charcoal. Repeated doses of charcoal (25 g every 3 hours, without cathartic) may be
indicated to enhance elimination.
13. What is the rationale for alkaline diuresis?
Because aspirin is an organic acid, administration of bicarbonate intravenously raises the
pH of the blood and traps salicylate ion, limiting the amount of salicylate that crosses
the blood-brain barrier. Similarly, an alkalotic urine retains salicylate ion, preventing its
reabsorption by the renal tubules. Isotonic alkaline diuresis is achieved by adding 3 ampules
of NaHCO
3
to 1 liter of D5W, with infusion at a rate of 2 to 3 mL/kg per hour. The patient
should be monitored for the development of pulmonary edema.
14. Explain the paradox of a decreasing serum salicylate concentration
and increasing clinical toxicity.
The serum salicylate level by itself does not reflect tissue distribution of the drug. If the
patient’s blood is acidemic, salicylate acid remains un-ionized and more penetrates the
blood-brain barrier, resulting in central nervous system toxicity. Salicylate levels should
be interpreted in light of the patient’s clinical condition and a concurrent blood pH; an
acidotic pH is associated with toxicity regardless of the salicylate level.
15. What are the indications for hemodialysis?
Standard indications include persistent, refractory metabolic acidosis (arterial pH ,7.10),
renal failure with oliguria, cardiopulmonary dysfunction (e.g., pulmonary edema,
dysrhythmias, cardiac arrest), central nervous system deterioration (e.g., seizures,
coma, cerebral edema), and an acute salicylate level greater than 130 mg/dL at 6 hours
post-ingestion. Because ingestion of more than 300 mg/kg predicts severe toxicity, a
nephrologist should be contacted early in anticipation of the possible need for dialysis.
16. What are the most common findings in chronic salicylate poisoning?
In contrast to acute salicylate poisoning, chronic salicylism is usually accidental. The principal
diagnostic feature is a change in mental status manifested by weakness, tinnitus, lethargy,
confusion, drowsiness, slurred speech, hallucinations, agitation, or seizures. Because these
signs are common to many other disorders, the diagnosis frequently is missed, resulting in a
mortality rate of 25%. Most patients are tachypneic, which is a compensatory response to an
anion gap metabolic acidosis. The serum salicylate level may be normal or minimally elevated.
ACETAMINOPHEN POISONING
17. Is there anything new in acetaminophen toxicology?
Yes. There’s much more to worry about now that we have extended release preparations and
reports of hepatotoxicity due to unintentional supratherapeutic ingestions.
18. What are the characteristics of acetaminophen overdose?
Acetaminophen is the drug most commonly involved in acute analgesic ingestions, either as a
single agent or in combination with various cough, cold, or pain remedies. Early diagnosis of
acute (phase I) acetaminophen toxicity is important because early symptoms may be subtle or
absent; the onset of hepatotoxicity, the major manifestation, is delayed by several days after
Chapter 70 ANTIPYRETIC POISONING492
ingestion. Failure to recognize and treat toxicity within 16 hours of ingestion results in significant
morbidity and mortality. The main issue in treatment is the prevention of hepatotoxicity.
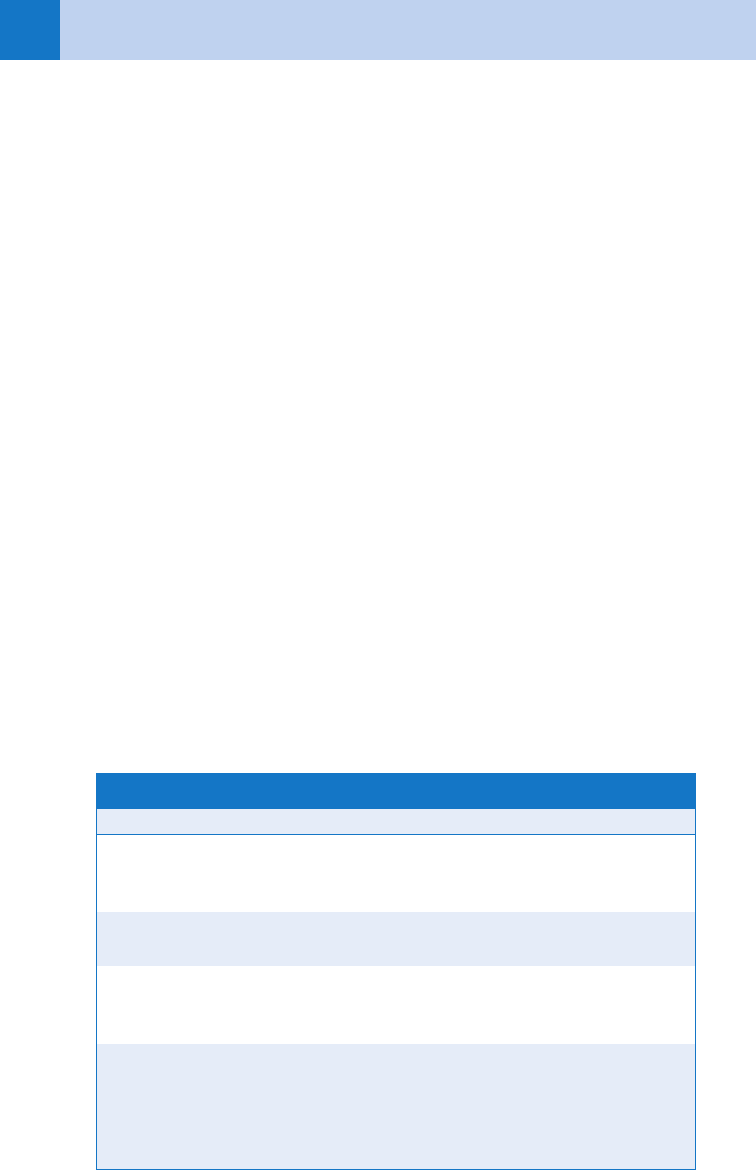
19. Outline the four phases of acetaminophen overdose.
See Table 70-2.
20. What are the initial central nervous system manifestations of acetaminophen
poisoning?
Gotcha! In the early stages, there are none, and abnormalities in mental status or level of
consciousness should be attributed to other drugs (e.g., salicylates, opiates, sedatives) or to
other disease states. Hepatic encephalopathy can occur in phase III.
21. Describe the pathophysiology of acetaminophen toxicity.
Acetaminophen is metabolized primarily by the liver. About 90% of it is conjugated with
glucuronic or sulfuric acid to form nontoxic compounds that are excreted in the urine. About
2% of the drug is excreted unchanged in the urine. The remainder is metabolized by the
cytochrome P-450 mixed-function oxidase system. This involves formation of a toxic
intermediary compound, which is conjugated rapidly with hepatic glutathione. The resulting
conjugate is metabolized further, and its byproducts are excreted in the urine. Because the
liver normally has a fixed amount of glutathione, this compound is depleted rapidly in an acute
overdose. The toxic intermediary then accumulates, unmetabolized, and binds to the
sulfhydryl groups of hepatic enzymes. The result is irreversible centrilobular hepatic necrosis.
22. How is hepatotoxicity predicted?
An acute ingestion of 7.5 gm or more in an adult or 140 mg/kg in a child is generally
predictive of hepatotoxicity. The most accurate predictor of hepatotoxicity is the serum
acetaminophen level obtained between 4 and 24 hours after acute ingestion. The Rumack-
Matthew nomogram, which plots serum concentration against hours postingestion, is the
standard reference for predicting hepatotoxicity in an acute overdose. Certain drugs, such as
cimetidine, compete with acetaminophen for metabolism by the P-450 pathway and
theoretically offer some protection from hepatotoxicity. Other drugs, such as phenytoin and
phenobarbital, may induce P-450 enzymes and facilitate acetaminophen metabolism to the
toxic intermediary, thereby increasing the risk of toxicity.
LFTs, liver function tests.
Phase Onset Clinical Characteristics Laboratory Findings
I ,24 hours Anorexia, nausea, vomiting,
diaphoresis (patient may be
asymptomatic)
Toxic acetaminophen level
II 24–72 hours Right upper quadrant
abdominal pain
Mild elevation in LFTs
III 3–5 days Vomiting, jaundice, encepha-
lopathy, oliguria
Marked elevation in LFTs,
coagulopathy, azotemia, hypo-
glycemia, hypophosphatemia
IV about
1 week
Gradual resolution of toxicity Improvement in laboratory
values
TABLE 70-2. PHASES OF ACETAMINOPHEN TOXICITY
Chapter 70 ANTIPYRETIC POISONING 493
23. Are serial serum acetaminophen levels helpful?
If an accurate estimate of the time of ingestion cannot be obtained, the nomogram cannot be
used and serial levels should be obtained. Patients with rising levels are at risk for
hepatotoxicity and should be treated with N-acetylcysteine (NAC).
24. Why is hepatotoxicity in children rare?
No one knows for sure. Toxicity in children is rare, even when toxic levels of acetaminophen
are found. One theory holds that acetaminophen metabolism in children shows a preference
for alternative pathways other than the P-450 system. The conversion from juvenile to adult
metabolism is believed to occur between 6 and 9 years of age.
25. Which laboratory tests are helpful?
If a serum acetaminophen level is in the toxic range on the nomogram, additional blood
should be obtained for a complete blood cell count, electrolytes, BUN, glucose, PT, INR, and
liver function tests. A limited toxicology screen also should be ordered, with attention to
treatable concomitant ingestions, such as salicylates, opiates, barbiturates, ethanol, and cyclic
antidepressants.
26. Outline the general treatment of acetaminophen poisoning.
Activated charcoal (1 g/kg) mixed with cathartic (e.g., sorbitol or magnesium sulfate) should
be administered orally or by gastric lavage tube, if there is an indication for gastric lavage
(see Chapter 68). The specific antidote is NAC. This agent is a glutathione substitute with a
high therapeutic-to-toxic safety ratio. It should be given orally or intravenously as soon as
possible after an acute overdose with a toxic plasma acetaminophen level, as documented by
the nomogram. NAC should also be given intravenously to patients with hepatic failure where
acetaminophen poisoning is suspected, even if the acetaminophen level is in the normal
range.
KEY POINTS: ED APPROACH TO ANALGESIC TOXICITY
1. Serial salicylate levels should be used to exclude toxicity prior to admitting the suicidal
patient to the psychiatric floor.
2. Salicylate levels must be interpreted in light of the patient’s clinical condition, the formulation
of the drug (pills, capsules or liquids), and a concurrent blood pH.
3. The primary goal in the treatment of acetaminophen toxicity is the prevention of
hepatotoxicity.
4. The antidote for acetaminophen overdose is N-acetylcysteine. It is most effective when
administered within 10 hours, regardless of whether it is given orally or intravenously.
27. How is NAC administered?
Oral NAC (Mucomyst™) is given by mouth or nasogastric tube after diluting it 1:5 with water or
juice. This dilution produces a 20% solution, which is given as a loading dose of 140 mg/kg,
followed by a maintenance dose of 70 mg/kg every 4 hours for 17 additional doses. If the patient
vomits a dose within 1 hour, the dose should be repeated. Antiemetics should be given if
vomiting is persistent. The intravenous NAC formulation (Acetadote™) is indicated for patients
in whom oral NAC is contraindicated (e.g., persistent vomiting, encephalopathy, gastrointestinal
bleeding, bowel obstruction, concomitant ingestion with anticholinergic drug). The dose is
150 mg/kg in D
5
W over 15 minutes, followed by 50 mg/kg over 4 hours, then 100 mg/kg over
16 hours.

Chapter 70 ANTIPYRETIC POISONING494
28. Which route is better for administering NAC, oral or intravenous?
It depends. Compared to the oral route, intravenous NAC is easier to administer, takes less
time (20.25 hours vs. 72 hours for the oral route), and can be given to patients who are
vomiting. Disadvantages include a higher rate of adverse reactions (up to 17%) and greater
expense. There is no evidence to date that one route is preferable to the other in terms of
reducing the risk of hepatotoxicity.
29. Is there a critical window in time to administer NAC?
Yes. Whenever possible, NAC should be given within 10 hours of acute acetaminophen
overdose. NAC still may be of benefit if given more than 10 hours after acute ingestion,
particularly in patients who have taken extended-release formulations or staggered overdoses,
and in patients with persistently toxic acetaminophen levels or elevated liver enzymes. The
intravenous route is recommended in these cases.
30. Should I be concerned about potential adverse reactions to intravenous NAC?
Yes. The incidence of such reactions is 5% to 17%, and they tend to occur during infusion of
the loading dose. Typical symptoms not requiring therapy include nausea, vomiting, and
flushing; mild urticaria can be treated with diphenhydramine. Interruption of NAC therapy is
not necessary, but the initial infusion rate should be slowed. Serious reactions, such as
bronchospasm, angioedema, and hypotension, require aggressive therapy with antihistamines,
steroids, and epinephrine and discontinuation of the NAC.
31. What is the acetaminophen-alcohol syndrome?
Acute alcohol ingestion is said to be protective because alcohol competes with acetaminophen
as a substrate for cytochrome P-450. In contrast, chronic alcohol abuse affects acetaminophen
detoxification in two ways:
a. It lowers hepatic glutathione stores, resulting in a reduced capacity to detoxify the toxic
intermediate compound.
b. It induces the cytochrome P-450 system, increasing the proportion of ingested
acetaminophen that is converted to the toxic intermediate.
Diagnostic findings include a history of acetaminophen ingestion and elevated aspartate
transaminase levels (usually .800 IU/L) in patients with known or occult alcohol abuse who
regularly take acetaminophen. The diagnosis initially is missed in one third of cases, and the
mortality rate is greater than 30%. Treatment is generally supportive, although NAC has been
tried, and liver transplantation is an option.
32. What is the treatment for chronic acetaminophen toxicity?
In chronic acetaminophen poisoning, the nomogram is not helpful in predicting toxicity.
Repetitive ingestion is thought to be of serious concern only in alcoholics, patients on
anticonvulsants, children with febrile illnesses, individuals taking large doses (e.g., .10 g/day),
and patients with symptoms of toxicity. NAC is recommended only for patients with detectable
acetaminophen levels and evidence of liver injury.
IBUPROFEN POISONING
33. What are the characteristics of ibuprofen overdose?
Ibuprofen is readily available as an over-the-counter medication used in the treatment of
mild-to-moderate pain and fever. Rapid absorption leads to peak drug levels within 2 hours.
Symptoms usually are seen within 4 hours of ingestion and are more likely to be serious in
children. Toxicity is limited in patients who ingest less than 100 mg/kg, whereas patients,
primarily children, who ingest more than 400 mg/kg may be at risk for more severe
symptoms.
Chapter 70 ANTIPYRETIC POISONING 495
34. List the primary symptoms of ibuprofen toxicity.
n
Gastrointestinal toxicity is manifested by nausea, vomiting, abdominal pain, and
hematemesis.
n
Nephrotoxicity results in acute renal failure.
n
Central nervous system toxicity (seen mostly in children) includes somnolence, apnea,
seizures, and coma.
n
Severe metabolic acidosis and thrombocytopenia have also been described.
35. Should a serum ibuprofen level be obtained?
No, because the serum ibuprofen level does not correlate with clinical symptoms, there is no
role for this test in medical decision-making.
36. Describe the treatment for ibuprofen toxicity.
Treatment is directed at alleviating symptoms and providing supportive care (see Chapter 68).
If hematemesis is present or there is blood in the stool, a nasogastric tube should be placed;
if blood is present, the stomach should be irrigated with saline. A limited toxicology screen to
search for other readily treatable toxins (i.e., salicylates, acetaminophen, opiates, barbiturates,
cyclic antidepressants, and ethanol) is recommended. Seizures should be treated with
intravenous diazepam. Renal and hepatic function tests should be ordered. Children with
ingestions of greater than 400 mg/kg should be observed in the hospital. Forced diuresis,
alkalinization, and hemodialysis are not indicated.
BIBLIOGRAPHY
1. Bailey B, McGuigan MA: Management of anaphylactoid reactions to intravenous N-acetylcysteine. Ann Emerg
Med 31:710–715, 1998.
2. Flomenbaum NE: Salicylates. In Goldfrank LR, Flomenbaum NE, Lewin NA, et al, editors: Goldfrank’s
toxicologic emergencies, ed 8, Norwalk, CT, 2006, McGraw Hill, pp 550–564.
3. Hall AH, Smolinske SC, Kulig KW, et al: Ibuprofen overdose: a prospective study. West J Med 48:653–656,
1988.
4. Hendrickson RG, Bizovi KE: Acetaminophen. In Goldfrank LR, Flomenbaum NE, Lewin NA, et al, editors:
Goldfrank’s toxicologic emergencies, ed 8, Norwalk, CT, 2006, McGraw Hill, pp 523–543.
5. Johnson SC, Pelletier LL: Enhanced hepatotoxicity of acetaminophen in the alcoholic patient: two case reports
and a review of the literature. Medicine 76:185–191, 1997.
6. Oker EE, Hermann L, Baum CR, et al: Serious toxicity in a young child due to ibuprofen. Acad Emerg Med
7:821–823, 2000.
7. Prescott L: Oral or intravenous N-Acetylcysteine for acetaminophen poisoning? Ann Emerg Med 45:409–413,
2005.
8. Smilkstein MJ, Knapp GL, Kulig KW, et al: Efficacy of oral N-acetylcysteine in the treatment of acetaminophen
overdose: analysis of the national multicenter study 1976–1985. N Engl J Med 319:1557–1562, 1988.
9. Wolf SJ, Heard K, Sloan EP, Jagoda AS. Clinical policy: issues in the management of patients presenting to
the emergency department with acetaminophen overdose. Ann Emerg Med 50:292–313, 2007.
10. Yip L, Dart RC, Hurlbut KM: Intravenous administration of oral N-acetylcysteine. Crit Care Med 26:40–43,
1998.
496
BITES AND STINGS
CHAPTER 71
Shawn M. Varney, MD, FACEP
ARACHNIDA (CHIGGERS. SCABIES, SCORPIONS, AND SPIDERS)
1. What is a tarantula?
It is a large spider of the family Theraphosidae. The largest is the South American
Grammostola mollicoma, with a leg span of up to 27 cm and a body length of up to
10 cm! Not much is known about tarantula venom, although it seems to contain a mixture
of hyaluronidase, nucleotides, and polyamines (which act as neurotransmitters to paralyze
the prey). On the whole, these bites tend to be of low toxicity in humans with a mild,
briefly active venom causing pain, numbness, and lymphangitis. The bites usually do
not cause necrosis or serious sequelae. The spider has little urticating hairs that are
barbed and can cause skin and mucous membrane irritation with edema and pruritus
that can last for weeks. Eye exposure can cause a severe keratoconjunctivitis and
ophthalmia nodosa.
2. What spider bites are likely to be an issue?
Although all spiders possess venom, there are two spiders of particular clinical importance in
the United States: Latrodectus (black widow) and Loxosceles (brown recluse or fiddle back).
In 2007, the American Association of Poison Control Centers (AAPCC) reported 2,514 bites
from Latrodectus and 1,783 from Loxosceles. There were no deaths and only 16 major
reactions attributed to Latrodectus bites (0.64%). Similarly, no deaths and 15 major reactions
(0.84%) were attributed to Loxosceles. The envenomation syndromes (and treatment) of these
two spiders are quite distinct (Table 71-1).
3. What is Mustov’s disease?
It is a play on words. Although there were 13,479 bites attributed to spiders reported to the
AAPCC in 2007, this number is likely an inaccurate estimate of the true incidence because:
n
These are only the cases that were reported to poison control centers.
n
The effect of Mustov’s disease (as in, “Doc, I woke up with this. I must’ve been bitten by a
spider in my sleep.”). It seems that a number of nonbite skin lesions (especially community
acquired methicillin-resistant Staphylococcus aureus abscesses) are unfairly blamed on
spiders. Mustov’s disease is not specific to spider bites.
4. A 5-year-old boy presents with genital itching that started several hours after
sitting on the lawn watching a fireworks display. His examination reveals
intensely pruritic, erythematous papules around his groin. What is this?
How can it be treated? (Clue: he had been wearing shorts.)
Chiggers. They are tiny mite larvae that cause intense pruritus. The diagnosis is based on
identifying the characteristic skin lesions in a person with an outdoor exposure. Itching begins
within a few hours of exposure, and the papules can enlarge to form nodules in 1 to 2 days.
There may be fever and erythema multiforme. Treatment is with antihistamines and steroids
(topical or oral) for the symptoms, and lindane, permethrin, or crotamiton for definitive
therapy.
Chapter 71 BITES AND STINGS 497
Latrodectus: Black Widow Loxosceles: Brown Recluse
Markings Markings
Red hourglass shape on the ventral
abdomen (♀)
Dark, violin-shaped spot anterodorsally
Presentation Presentation
Pain at the bite within 1 hour
Target-shaped erythema, swelling, diaphoresis
Typically, an initially mild bite characterized
by erythema
Bite becomes necrotic over 2–4 days
n
Diffuse large muscle cramping, including
the back, chest, and abdomen (which
may mimic peritonitis)
n
Latrodectisima: characteristic facial mus-
cle spasm, lacrimation, photophobia, and
periorbital edema
n
Headache
n
Light-headedness
n
Nausea and vomiting
Systemic reaction may occur in 1–2 days:
n
Fever
n
Chills
n
Vomiting
n
Arthralgia
n
Myalgia
n
Hemolysis
n
Coagulapathy
May result in renal failure and death
Severe envenomations may result in dysphagia,
hypertension, respiratory failure, shock,
and coma
Treatment Treatment
n
Wound care
n
Analgesics, benzodiazepines for spasm
n
Tetanus prophylaxis
n
Calcium gluconate (IV) is ineffective and
is no longer recommended
n
Horse-serum IgG antivenom: administer
a subcutaneous test dose, and then, if no
severe reaction, 1 vial mixed in 50 mL
saline over 30 min IV
n
New Latrodectus immune F(ab)2
antivenom being studied
n
Wound care
n
Analgesics
n
Tetanus prophylaxis
n
Surgical debridement and possible
grafting for lesions greater than 2 cm
n
Transfusion or dialysis, as necessary
n
Hyperbaric oxygen therapy, corticoste-
roids, and dapsone have been advocated
by some, but there is no clear evidence
of efficacy in humans
n
Currently, there is no commercially
available antivenom
Saucier JR: Arachnid envenomation. Emerg Med Clin North Am 22(2):405–422, ix, 2004.
TABLE 71-1. COMPARISON OF BLACK WIDOW AND BROWN RECLUSE SPIDERS
