Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 68 GENERAL APPROACH TO POISONINGS478
14. Discuss some other useful antidotes for common poisonings.
n
Naloxone and dextrose are the most common antidotes and should be given routinely to
unconscious overdose patients. Intravenous administration of 2 mg of naloxone that results
in awakening of the patient is diagnostic of acute opiate overdose. Small, incremental doses
of 0.2 mg can be used if it is suspected that the patient is opioid dependent, because the
2-mg dose of naloxone will precipitate withdrawal. Many drugs and chemicals can cause
hypoglycemia, including ethanol, and for this reason dextrose likewise should be given,
unless it can be determined quickly that the blood glucose is normal.
n
Physostigmine is an antidote for the anticholinergic syndrome. Physostigmine can be used
diagnostically and therapeutically when the diagnosis of the anticholinergic syndrome is
suspected. It should not be used to treat tricyclic antidepressant poisoning (or in patients
with ECG changes suggestive of tricyclic antidepressant poisoning such as QRS widening
or a large R wave in AVR). Seizures and bradydysrhythmias have been reported when used
in this setting. A dose of 1 to 2 mg given slowly intravenously to an adult is usually
sufficient.
n
Digoxin immune Fab (Digibind, Digitab) is a safe and effective antidote for digitalis
glycoside poisoning and can rapidly reverse dysrhythmias and hyperkalemia, which can be
life-threatening. In contrast to naloxone, Digibind does not work immediately, and a full
response to therapy may not be seen until approximately 20 minutes after administration.
For a life-threatening digitalis overdose when the dose and the serum level are currently
unknown, 10 vials of Digibind should be given.
n
Atropine and pralidoxime (Protopam) are antidotes used for cholinesterase inhibitor
toxicity. This group of pesticides includes the organophosphates and carbamates, which
commonly are found in household insecticides. Atropine is used to dry up secretions,
primarily pulmonary, and pralidoxime is used primarily to reverse the skeletal muscle
toxicity of these agents, including weakness and fasciculations.
n
Flumazenil is a benzodiazepine antagonist that has been shown to be useful in cases of
acute benzodiazepine overdose resulting in significant toxicity. Its use may precipitate
benzodiazepine withdrawal, including seizures. It should not be used when tricyclic
antidepressants or other pro-convulsants have been coingested with benzodiazepine. The
usual adult dose is 0.2 mg followed in 30 seconds by 0.3 mg, followed in 30 seconds by
0.5 mg, repeated up to a total of 3 mg.
n
Ethanol and fomepizole are alcohol dehydrogenase blocking agents that are used to treat
methanol and ethylene glycol poisoning. They prevent the metabolism of methanol and
ethylene glycol to their toxic metabolites. Intravenous ethanol is less expensive than
fomepizole but is somewhat more difficult to use. The initial intravenous dose is 8 mL/kg
of 10% ethanol over 30 minutes, followed by an infusion of 0.8 mL/kg/h in a nondrinker,
1.4 mL/kg/h in an average drinker, and 2 mL/kg/h in a heavy drinker. Blood ethanol
concentration should be measured immediately after the loading dose and repeated every
hour initially, and the dose adjusted to maintain a blood ethanol of 100 to 125 mg/dL. The
KEY POINTS: MANAGEMENT OF SUSPECTED TOXIC INGESTION
1. Activated charcoal is sufficient decontamination for most overdose patients.
2. Urine toxicology screens are not indicated in patients with normal mental status and vital
signs.
3. Serum electrolytes and acetaminophen concentration should be obtained in patients with
deliberate overdose.
4. Although there are a few antidotes for specific toxins, most poisoned patients recover with
supportive care.
Chapter 68 GENERAL APPROACH TO POISONINGS 479
loading dose of fomepizole is 15 mg/kg intravenously over 30 minutes with subsequent
doses of 10 mg/kg every 12 hours. The dose of both agents must be increased in patients
undergoing dialysis.
n
N-ace tyl cys tei ne is extremely effective in preventing acetaminophen-induced liver
injury. It is most effective if administered within 8 hours of ingestion but reduces
morbidity and mortality even in patients with acetaminophen-induced acute liver failure.
It can be administered orally (loading dose 140 mg/kg, subsequent doses 70 mg/kg
every 4 hours) or intravenously (initial dose 150 mg/kg in 200 ml D
5
W over 15 minutes,
followed by 50 mg/kg in 500 ml D
5
over 4 hours, followed by 100 mg/kg in 1 L D
5
W
infused over 16 hours).
BIBLIOGRAPHY
1. American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists:
Position Paper: Gastric lavage. J Toxicol Clin Toxicol 42:933–943, 2004.
2. American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists:
Position Paper: Ipecac syrup. J Toxicol Clin Toxicol 42:133–143, 2004.
3. American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists:
Position Paper: Single-dose activated charcoal. J Toxicol Clin Toxicol 43:61–87, 2005.
4. American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists:
Position Paper: Whole bowel irrigation. J Toxicol Clin Toxicol 43:129–130, 2005.
5. Bronstein AC, Spyker DA, Cantilena JR, et al: 2007. Annual Report of the American Association of Poison
Control Centers’ National Poison Data System (NPDS): 25th Annual Report. Clin Toxicol 46(10):927–1057, 2007.
6. Pond SM, Lewis-Driver DJ, Williams GM, et al: Gastric emptying in acute overdose: a prospective randomised
controlled trial. Med J Aust 163:345–349, 1995.
7. Proudfoot AT, Krenzelok EP, Vale JA: Position paper on urine alkalinization. J Toxicol Clin Toxicol 42:1–26, 2004.
8. Vale JA, Krenzelok EP, Barceloux GD: Position statement and practice guidelines on the use of multi-dose
activated charcoal in the treatment of acute poisoning. J Toxicol Clin Toxicol 37:731–751, 1999.
480
THE ALCOHOLS: ETHANOL, ETHYLENE GLYCOL,
METHANOL, AND ISOPROPYL ALCOHOL
CHAPTER 69
Louis J. Ling, MD
1. Is a patient with altered mental status, who smells of alcohol, simply
intoxicated?
In most cases, yes. However intoxicated patients are at increased risk for injury,
immunosuppression, poor nutrition, poor thermal regulation, and many medical conditions.
Every patient assumed to be drunk (only) needs a thoughtful initial evaluation and subsequent
serial evaluations.
2. How should intoxicated patients be evaluated?
Patients who arrive primarily with intoxication and without a history of trauma or injury should
have vital signs taken; a rapid scan for recent trauma; a rapid glucose determination; and
assessment for level of consciousness, responsiveness, and respiratory depression. Examination
should include a look for unequal pupils, ecchymosis, deformity, and palpation everywhere for
abdominal and bony tenderness. If no concerns are identified, it is important to return and
reexamine the patient every hour or two to ensure that the patient is improving.
3. When should an acutely intoxicated patient be intubated?
Hypopnea and hypoventilation are rarely the issue, but the inability of the patient to protect the
airway is. For patients who are heavily intoxicated but not deemed to require intubation, lateral
decubitus positioning is preferred. Restraining a patient supine or prone can be dangerous
because of the risk of aspiration and airway compromise.
4. Which medications are best for management of alcohol withdrawal?
Benzodiazepines, usually diazepam or lorazepam, can be given orally, intravenously, or in
combination and titrated by clinical response. Patients with mild withdrawal (normal vital
signs, no hallucinosis) may be discharged with a 2- to 3-day course of a single agent (e.g.,
lorazepam, 1–2 mg twice a day). Haloperidol is an appropriate adjunct for hallucinosis.
Theoretical concerns over haloperidol lowering seizure threshold and exacerbating
hemodynamic abnormalities have not been substantiated. More severe withdrawal
syndromes require increasingly aggressive therapy with these same agents while under
observation by medical personnel.
5. What is an appropriate work-up for alcohol withdrawal seizures (AWDs)?
Typically, AWDs occur approximately 6 to 96 hours after the last drink and in clusters of one
to four seizures. The seizures are usually generalized and self-limited. Coincident features of
withdrawal may be lacking, and lateralizing findings during the seizure, the postictal state, or
both, are often present because of underlying structural pathology.
In a first-time evaluation, other causes of or contributors to seizures should be sought.
Laboratory studies (i.e., electrolytes, glucose, magnesium, calcium, toxicologic screen) are
rarely useful unless history or physical examination is suggestive. Noncontrast computed
tomography (CT) shows traumatic, infectious, vascular, or other abnormalities in nearly 10%
of patients Generally, electroencephalography is not integral to the work-up. Lumbar puncture
is indicated when meningitis, meningoencephalitis, or subarachnoid hemorrhage is suspected.
Subsequent visits for suspected AWDs demand scrupulous history and physical examination
to ensure that other pathologic causes have not developed in the interim. If the presentation

Chapter 69 THE ALCOHOLS: ETHANOL, ETHYLENE GLYCOL, METHANOL, AND ISOPROPYL ALCOHOL 481
matches prior episodes and the findings on current neurologic examination are baseline, no
other work-up, including CT, is necessary. Lingering postictal confusion warrants a check of
glucose and electrolytes. If the history or examination has changed significantly or is worrisome,
the clinician should start from scratch.
6. How should AWDs be managed?
n
Acute: As with all seizures, ensure a patent airway and administer 50% dextrose (D
50
) and
benzodiazepines intravenously (as needed). An observation period of 6 hours is optimal
because recurrent seizures are common within this period. Benzodiazepines in the
immediate and 2-day postseizure period decrease the incidence of additional seizures
during this time.
n
Chronic: Patients whose seizures have an epileptogenic focus (e.g., old subdural) should
have an anticonvulsant, such as phenytoin, administered. However, compliance is typically
poor. In the patient with pure AWDs, long-term anticonvulsant therapy is contraindicated.
Physicians must resist the imperative to prescribe something unless there is clear
justification.
7. Can AWDs be prevented?
Benzodiazepines in the acute withdrawal period, particularly in patients with a history of
AWDs, can decrease seizures.
8. Who is at risk for alcohol-induced hypoglycemia (AIH)? What is the clinical
presentation?
AIH results from:
a. Insufficient glycogen stores
b. Alcohol-induced impairment of gluconeogenesis
The three groups vulnerable to AIH are:
a. Chronic alcoholics
b. Binge drinkers
c. Young children
AIH may occur during intoxication or up to 20 hours after the last drink. Manifestations of
neuroglycopenia (e.g., headache, depressed mental status, seizure, or coma) predominate.
Evidence of catecholamine excess, typical of insulin-induced hypoglycemia (tremulousness,
diaphoresis, anxiety), is unusual. Seizures are a frequent presentation in children. Localized
central nervous system signs, including a stroke-like picture (alcohol-induced hypoglycemic
hemiplegia), often occur in adults.
9. What causes alcoholic ketoacidosis (AKA)?
This common metabolic disturbance occurs early after heavy binge drinking and is heralded
by starvation and vomiting and occasionally shortness of breath (Kussmaul respirations) and
abdominal pain. Ketoacidosis results from accumulation of acetoacetate and, particularly,
b-hydroxybutyrate. Because the latter is not measurable on routine blood and urine tests, the
patient may have trace or absent ketones at presentation. Similarly, as the patient improves
and b-hydroxybutyrate is metabolized to acetoacetate, there may be a paradoxical spike in
urine and serum ketones.
At presentation, serum pH and bicarbonate average 7.1 and 10, respectively. These values
vary widely because of the frequently overlapping ketoacidosis (metabolic acidosis),
withdrawal-related hyperventilation (respiratory alkalosis) and protracted emesis (metabolic
alkalosis). When all three are coincident, the result is a triple acid-base disturbance. This
allows you to interpret arterial blood gases and electrolytes pretty much any way you wish
and be at least partially correct. Decreased body stores of potassium and phosphate are
typical. In AKA, serum glucose is usually normal or low, a distinguishing feature from diabetic
ketoacidosis.

Chapter 69 THE ALCOHOLS: ETHANOL, ETHYLENE GLYCOL, METHANOL, AND ISOPROPYL ALCOHOL482
10. How should AKA be managed?
Treatment consists of rehydration with dextrose-containing crystalloid, antiemetics if needed,
benzodiazepines for withdrawal, and multivitamins, potassium, and phosphate as indicated.
Bicarbonate is rarely required, and insulin therapy is proscribed. Metabolic abnormalities
usually resolve with 12 to 16 hours of therapy.
11. What is the relationship between alcohol and metabolic acidosis?
n
Ethanol: Acute ethanol ingestion results in a mild increase in the lactate-to-pyruvate ratio.
Clinically significant metabolic acidosis does not ensue.
n
AKA: This ethanol abstinence syndrome produces marked elevations in acetoacetate and
b-hydroxybutyrate with resultant and occasionally profound increased anion gap metabolic
acidosis. During the correction phase, a non-anion gap, hyperchloremic picture often
develops (because some of the bicarbonate-bound ketoacids are excreted in the urine) on
the road to normalization.
n
Ethylene glycol and methanol: Toxic metabolites of these compounds produce increased
anion-gap metabolic acidosis. In the suspected alcoholic patient who presents with
significant metabolic acidosis, a quick method of distinguishing the presence of ethylene
glycol or methanol from AKA is the osmolal gap. If this exceeds 25 mOsm/Kg, it is 88%
specific for the presence of ethylene glycol or methanol.
n
Isopropyl alcohol: A significant portion of isopropyl alcohol is metabolized to acetone.
This is a ketone but not a ketoacid, causing ketosis and ketonuria but not acidosis.
12. How is coagulation affected in a chronic alcoholic?
Bone marrow depression from ethanol, folate deficiency, and hypersplenism secondary to
portal hypertension all cause thrombocytopenia. Platelet counts less than 30,000/mL,
resulting from alcohol usage alone, are unlikely. Qualitative platelet defects also occur.
Hepatocyte loss from chronic alcohol abuse depletes all coagulation factors except VIII,
particularly II, VII, IX, and X. Alcoholics often have inadequate vitamin K, a requisite cofactor
for the production of factors II, VII, IX, and X because of hepatobiliary dysfunction and poor
diet. When faced with gastrointestinal hemorrhage in a chronic alcoholic, an intravenous
vitamin K supplementation trial is warranted. The far more likely culprit is hepatocellular
destruction, however, for which vitamin K would not be helpful. Vitamin K does not begin to
restore factor levels for 2 to 6 hours, so for emergent scenarios, fresh frozen plasma provides
immediate factor supplementation.
13. How should the combative alcoholic patient be managed?
When the patient or staff is in jeopardy, the first step is physical restraint of the patient.
A sufficient number of competent personnel and restraint devices are necessary. Closed
head injury, hypoxia, or a full bladder may be the source of distress and should be excluded,
managed, or relieved.
For chemical sedation, haloperidol (5–10 mg intravenous push) has rapid onset of
sedation (5 minutes), but repeat doses may be required. This agent is not detrimental to
airway patency, ventilation, or hemodynamics. There is a 5% to 10% incidence of
extrapyramidal reactions, usually within 12 to 24 hours. Droperidol (2.5–5 mg
intramuscularly) is another effective butyrophenone, but it received a black-box warning
in 2004 due to reports of QT prolongation and torsades de pointes. In any case, haloperidol
and droperidol have been shown to be relatively comparable in efficacy and side effects.
14. When is an intoxicated patient safe to discharge from the ED?
From a management perspective, there are two fundamental concerns:
n
Acute intoxication obfuscates the verification of certain diagnoses and the exclusion of
others.
n
A physician who discharges an acutely intoxicated (i.e., incompetent) patient may be
held accountable for the actions of that patient subsequent and proximate to discharge
from the ED.
Chapter 69 THE ALCOHOLS: ETHANOL, ETHYLENE GLYCOL, METHANOL, AND ISOPROPYL ALCOHOL 483
The degree of clinical intoxication at a specific serum alcohol level is variable in accordance
with the patient’s chronicity and severity of drinking. A veteran drinker with a level in excess of
500 mg/dL can look less drunk than a teenager at 100 mg/dL. Documentation of the discharge
examination includes mental status, gait, and the fact that the patient is clinically sober.
Particular attention should be paid to potential abdominal or closed head trauma. The patient
should be discharged to an appropriate environment. Serum or breath alcohol determinations
sometimes can be helpful at the outset of care but unneeded at discharge.
KEY POINTS: ALCOHOL-RELATED DISORDERS
1. Airway protection: Clinical judgment is the key factor in determining whether an acutely
intoxicated patient requires intubation for airway protection.
2. Phenytoin should only be given to patients with clear indication of an epileptogenic focus.
Otherwise, its use for prevention of alcohol withdrawal seizures is strictly proscribed.
3. Discharge documentation: The critical determination in the discharge of the patient is the
progression to and documentation of clinically sober.
15. Must thiamine be administered before glucose in the alcoholic patient?
Wernicke-Korsakoff syndrome develops over hours to days. The precipitous initiation of
Wernicke-Korsakoff syndrome by dextrose has not been substantiated. The consequences
of neuroglycopenia begin within 30 minutes and are easily prevented. In alcoholic patients
with known or suspected hypoglycemia, promptly administer glucose and deliver thiamine
empirically as soon afterward as possible. Because magnesium is a cofactor of thiamine
and because alcoholics are frequently hypomagnesemic, 2 g of IV magnesium should be
administered when there is suspicion of Wernicke-Korsakoff syndrome.
16. Is it dangerous to administer thiamine intravenously?
Orally administered thiamine is often absorbed poorly in the alcoholic patient. The
intramuscular route is painful and can result in hematomas or abscesses, particularly in
patients with impaired coagulation status. The experience with intravenous thiamine is
extensive. Thiamine may be given as part of fluid hydration with multivitamin preparations
or by bolus infusion.
17. Is there a cure for a hangover?
Probably not, at least not one with solid scientific credentials. There is no shortage of
remedies, however, from the well-worn “hair of the dog that bit you” (i.e., start drinking again)
to a more recently acclaimed concoction of vitamin B
6
, nonsteroidal anti-inflammatories, and
hydration. The only sure-fire measure is the avoidance of drinking in the first place.
18. Are there specific criteria for the diagnosis of Wernicke-Korsakoff syndrome?
Criteria require two of the following four signs to be present:
a. Dietary deficiencies
b. Oculomotor abnormalities
c. Cerebellar dysfunction
d. Either an altered mental state or mild memory impairment.
19. Why is it important to understand the metabolism of methanol?
The metabolites of methanol are the toxins and depend on alcohol dehydrogenase (ADH) for
their conversion from the non-toxic parent methanol. Ethanol and fomepizole both saturate
ADH and greatly slow the metabolism of methanol to the toxic metabolite. Folate is a cofactor
in the breakdown of formic acid, and in monkeys (and other primates) folate supplementation
Chapter 69 THE ALCOHOLS: ETHANOL, ETHYLENE GLYCOL, METHANOL, AND ISOPROPYL ALCOHOL484
maximizes its metabolism and decreases injury. Knowledge of the metabolism directs the
treatment.
ADH Folate
Methanol → Formaldehyde → Formic Acid → CO
2
1 H
2
O
(toxic) (toxic) (nontoxic)
20. List the signs and symptoms of methanol poisoning.
Gastrointestinal toxicity
n
Nausea and vomiting
n
Abdominal pain
Central nervous system toxicity
n
Headache
n
Decreased level of consciousness
n
Confusion
Ocular toxicity
n
Retinal edema
n
Hyperemia of the disc
n
Decreased visual acuity
Other toxicity
n
Metabolic acidosis
KEY POINTS: METHANOL
1. Symptoms and acidosis are delayed.
2. Osmolal gap is often absent.
3. Persistent acidosis correlates with a poor prognosis.
4. Fomepizole, ethanol, and dialysis can all be used to treat the poisoned patient.
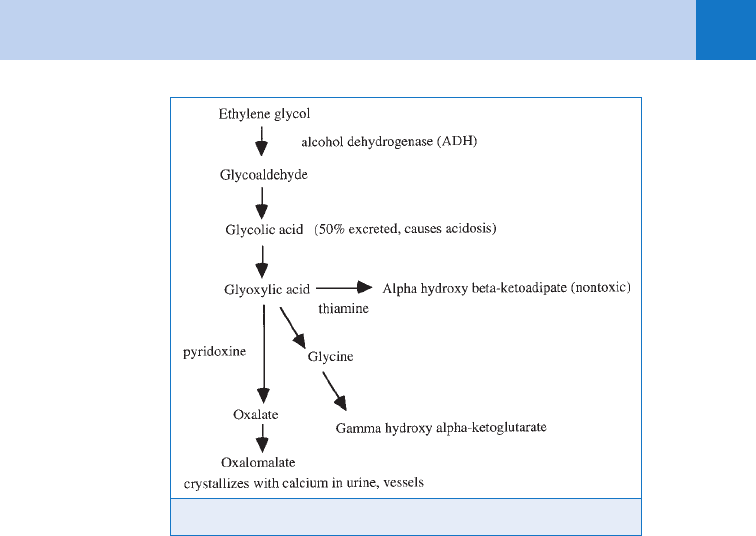
21. Why is it important to understand the metabolism of ethylene glycol?
As with methanol, ethanol and fomepizole saturate ADH, inhibiting conversion of ethylene glycol
into its harmful metabolites. Pyridoxine (vitamin B
6
) and thiamine are cofactors in the final steps
to form nonharmful end products and should be given to ensure maximal metabolism. Oxalate
crystals may not appear until late in the course of the poisoning (Fig. 69-1).
22. Why are the symptoms of ethylene glycol and methanol overdose often
delayed?
It may take 6 to 12 hours for sufficient quantities of the toxic metabolites to accumulate and
cause symptoms. The delay in symptoms is even greater with concurrent ethanol intoxication
because the ethanol slows down the rate of methanol and ethylene glycol metabolism and
delays the appearance of the toxic metabolites.
KEY POINTS: ETHYLENE GLYCOL
1. Symptoms and acidosis are often delayed.
2. Urinary oxalate crystals, fluorescence, early osmolal gap, and metabolic acidosis all suggest
ethylene glycol poisoning.
3. Fomepizole, ethanol, and dialysis can all be used to treat the poisoned patient.
Chapter 69 THE ALCOHOLS: ETHANOL, ETHYLENE GLYCOL, METHANOL, AND ISOPROPYL ALCOHOL 485
23. How are methanol and ethylene glycol poisonings similar?
Methanol and ethylene glycol are metabolized initially by ADH. Methanol is metabolized further to
formic acid, and ethylene glycol is metabolized to glycolic acid, glyoxylic acid, oxalate, and several
nontoxic metabolites. Because of these end products, both poisons result in metabolic acidosis
with an anion gap. Because of their low molecular weight, both increase the osmolar gap.
24. What is an anion gap?
A normal anion gap is the difference between measured and unmeasured anions (e.g., various
proteins, organic acids, phosphates) and measured and unmeasured cations (e.g., potassium,
calcium, and magnesium). The anion gap can be calculated from the formula:
Anion gap 5 (Na
1
) 2 (HCO
3
2
1 Cl
2
)
25. What causes an increased anion gap?
When metabolic acidosis results from an ingestion of nonvolatile acids, there are increased
hydrogen ions with positive charges. Because there is an equal increase in unmeasured
negatively charged anions but no increase in chloride, the difference between the measured
cations and measured anions is increased, causing an increased anion gap. The normal anion
gap is about 6 to 10 mEq/L. The causes of increased anion gap can be remembered by the
mnemonic A MUD PILES.
A 5 Alcohol, M 5 Methanol, U 5 Uremia, D 5 Diabetic ketoacidosis, P 5 Paraldehyde,
I 5 Iron, Isoniazid (INH), L 5 Lactate, E 5 Ethylene glycol, S 5 Salicylate
26. What is an osmolal gap?
Small atoms and molecules in solution are osmotically active, and this activity can be
measured by a depression in the freezing point or an elevation in the boiling point of the
solution. If there is an increase in low-molecular-weight molecules, such as acetone,
methanol, ethanol, mannitol, isopropyl alcohol, or ethylene glycol, the osmolality is greater
than what is calculated from the usual serum molecules. The difference between the actual
measured osmolality and the calculated osmolality is the osmolal gap, and a gap greater than
about 10 mOsm is considered abnormal.
Figure 69-1. Metabolism of methanol and ethylene glycol.
Chapter 69 THE ALCOHOLS: ETHANOL, ETHYLENE GLYCOL, METHANOL, AND ISOPROPYL ALCOHOL486
27. How is an osmolal gap calculated?
One formula is 2 3 Na
1
(mEq/L) 1 glucose (mg/dL)/18 1 blood urea nitrogen (BUN)
(mg/dL)/2.8 1 ethanol (mg/dL)/4.3. The inclusion of the ethanol level excludes patients who
have an elevated osmolal gap from ethanol ingestion alone. Using International System (SI)
units, the calculated osmolality 5 2 3 Na (mEq/L) 1 glucose (mmol/L) 1 BUN (mmol/L) 1
ethanol (mmol/L). The calculated osmolality is 285 6 5 mOsm/L. A toxic ethylene glycol level
of 25 mg/dL can be predicted to increase the osmolal gap 5 mOsm/L. Because of the small
effects on the osmolality and the imprecision of the measurement, this test is not precise
enough to be definitive so a normal osmolal gap does not exclude toxic levels of methanol
or ethylene glycol. The laboratory must use the method of freezing-point depression so that
volatile alcohols contributing to an osmolal gap are not boiled away during a boiling point
elevation procedure.
28. What comes first, the anion gap or the osmolal gap?
With initial absorption, the small parent molecules cause an early osmolal gap, but with
metabolism, acidic metabolites are formed causing a late metabolic anion-gap acidosis.
29. How toxic are methanol and ethylene glycol?
Death is reported after 15 to 30 mL (1–2 tablespoons) of methanol. Others have
survived larger ingestions, however. A minimal lethal dose for ethylene glycol is
approximately 1–2 mL/kg.
30. What is the toxicity of ethylene glycol?
Initially, there is central nervous system intoxication and gastrointestinal irritation, followed by
metabolic acidosis. Renal failure occurs frequently and typically is delayed in presentation.
Cranial nerve deficits are a rare complication.
31. Why is ethylene glycol so dangerous to animals?
Ethylene glycol is a frequent cause of death in animals who ingest antifreeze (especially dogs,
who drink almost anything). The taste is sweet and a small volume is deadly. The cause of
death for these animals may not be apparent because toxicity is delayed, and death occurs
long after the animal has left the scene.
32. Why does antifreeze have such a bright color?
Antifreeze is a bright color that fluoresces with ultraviolet (UV) light so that leaks from
auto radiators can be detected more easily. If the mouth and the urine are examined with a
UV light, fluorescein can be detected in about 30% of patients after ingestion. A positive
test should encourage immediate treatment, but a negative test misses two thirds of
ingestions.
33. How should patients with methanol and ethylene glycol poisoning be
treated?
Airway protection is paramount in patients with decreased level of consciousness or
respiratory depression. Small volumes and rapid absorption limit the effectiveness of gastric
lavage and charcoal. Acidosis (pH ,7.2) should be treated aggressively with sodium
bicarbonate. Ethanol and 4-methylpyrazole (4-MP) are antidotes that competitively block the
conversion of methanol and ethylene glycol to their toxic metabolites, allowing for elimination
of the unchanged poison without injury.
34. What are the indications for ethanol or 4-MP therapy?
They should be used if ethylene glycol or methanol levels exceed 20 mg/dL; if acidosis is
present, regardless of drug level; and if there is a history of a toxic ingestion while awaiting
confirmatory blood methanol or ethylene glycol levels.
Chapter 69 THE ALCOHOLS: ETHANOL, ETHYLENE GLYCOL, METHANOL, AND ISOPROPYL ALCOHOL 487
35. How do you choose between fomepizole (4-MP) and ethanol?
Ethanol is difficult to give consistently; ethanol blood levels are required to adjust the dose
and infusion can cause pain, resulting in the use of a central catheter. Ethanol may cause
hypoglycemia and respiratory depression, especially in children. These patients usually require
the close monitoring of an intensive care unit (ICU). 4-MP is replacing ethanol because it does
not cause sedation, does not require blood testing, is easily given as a bolus, and does not
require ICU management.
36. How do you use 4-MP?
The dose is 15 mg/kg every 12 hours and is increased to every 4 hours during dialysis.
Typical treatment is for 48 hours.
37. What are the indications for hemodialysis?
Dialysis used to be the primary treatment for these poisons and should be done in patients
with blood levels greater than 50 mg/dL, when the metabolic acidosis is not correctable, with
pending renal failure, or with visual symptoms in a methanol overdose. Many clinicians
recommend dialysis when blood levels exceed 25 mg/dL, if dialysis is readily available.
Hemodialysis can be avoided with prolonged fomepizole treatment.
38. What if dialysis is unavailable?
Patients with ethylene glycol poisoning can be treated successfully with 4-MP alone without
dialysis if there is no acidosis or renal failure. Because the half-life of ethylene glycol is
prolonged to 17 hours, the treatment may be extended but avoids invasive treatment of
dialysis. In methanol poisoning, 4-MP slows the metabolism and increases the half-life of
methanol to 30-52 hours. The use of 4-MP alone would not suffice for these patients.
39. How is isopropyl alcohol poisoning different from methanol and ethylene
glycol poisoning?
Isopropyl or rubbing alcohol is metabolized in the liver to acetone, which results in
measurable ketonemia in the serum. Acetone is excreted by the kidney, resulting in ketonuria,
and is exhaled through the lungs, giving patients an acetone aroma on their breath. Because
these metabolites are not acidic, isopropyl alcohol poisoning does not result in metabolic
acidosis and is far less toxic than either methanol or ethylene glycol.
40. What are the symptoms of isopropyl alcohol ingestion?
Isopropyl alcohol has a three-carbon chain rather than the two-carbon chain of ethanol.
Because of this, it crosses the blood-brain barrier faster and is about twice as intoxicating as
ethanol. Because it is commonly found in concentrated solutions and is more potent, the
central nervous system depression can occur rapidly and can continue from residual poison in
the stomach. Isopropyl alcohol is much more irritating than ethanol to the gastric mucosa and
often causes abdominal pain, vomiting, and hematemesis.
41. Why is isopropanol so frequently abused?
Isopropanol is easy and legal to obtain; rubbing alcohol is 70% isopropanol. Unlike
consumable beer, wine, and liquor, it is not taxed and is very inexpensive.
42. What treatment is advisable for isopropyl alcohol poisoning?
Patients need observation to watch for respiratory depression similar to patients
intoxicated with ethanol. An isopropyl alcohol level is roughly equivalent to an ethanol level
twice as high. An isopropyl level usually does not add greatly to clinical observation. In
the rare instance of coma or hypertension corresponding to isopropyl levels greater than
500 mg/dL, intubation and ventilation may be necessary, and hemodialysis can greatly
enhance removal of isopropyl alcohol from the body. An antidote is not available for
isopropyl alcohol (nor is one needed).
