Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.


Chapter 78 SPONTANEOUS ABORTION, ECTOPIC PREGNANCY, AND VAGINAL BLEEDING548
and an outer layer, called the decidua vera, which distinguish a true gestational sac from a
pseudosac that may be seen with an ectopic pregnancy.
n
Yolk sac: Seen at about 5 weeks’ GA by transvaginal ultrasound. This is a well-defined
echogenic ring seen within the gestational sac. For the purposes of emergency bedside
ultrasound, this is considered by many authors to be the most reliable finding confirming
the presence of an IUP and is easily recognized by sonographers of all skill levels.
n
Embryo: Fetal pole visible within the gestational sac, seen at about 5 to 6 weeks’ GA
by transvaginal ultrasound. Fetal cardiac activity is generally recognizable by about 6 to
7 weeks.
5. What are important questions to consider during the examination and
treatment of spontaneous abortion?
n
Is the patient hemodynamically stable?
n
Is there abdominal tenderness, guarding, or rebound (indicating a possible ectopic
pregnancy [EP])?
n
Are products of conception visible in the cervical os or vaginal canal (an incomplete
abortion)?
n
Is the cervical os open (inevitable abortion) or closed?
n
Is the patient febrile, indicating a possible septic abortion?
6. What is a septic abortion?
A spontaneous abortion complicated by endometritis, parametritis, or peritonitis.
7. What are the signs and symptoms of a septic abortion?
n
Malodorous discharge from the cervix or vagina
n
Pelvic and abdominal pain
n
Uterine tenderness
n
Fever/hyperthermia
n
Sepsis or septic shock
8. What are the earliest symptoms of a miscarriage?
Bleeding or spotting is usually first, followed by crampy abdominal, pelvic, or low back pain.
9. Describe the approach to the patient presenting with a positive pregnancy
test and first-trimester vaginal bleeding or pain?
n
Establish appropriate intravenous (IV) access. Two large-bore (18-gauge or larger)
intravenous (IV) lines are recommended if there is any concern for hemodynamic
instability.
n
Obtain a measurement of hemoglobin and/or hematocrit or complete blood count (CBC). A
blood type and screen should be sent if there is any possibility the patient may require a
blood transfusion.
n
Treat hypotension or tachycardia with IV fluids or transfusion of blood products, as
indicated by patient condition.
n
Determine whether an IUP has been previously documented by ultrasound. If no IUP has
been documented, perform a bedside ultrasound to evaluate for a possible ectopic
pregnancy. Unstable patients should not be allowed to leave the ED for diagnostic studies.
n
Perform a bimanual and speculum pelvic examination to assess the source of bleeding, and
examine the cervical os to assess for the presence of products of conception in the cervix
or vaginal vault.
n
If there is ongoing bleeding, remove any visualized tissue using gentle traction with ring
forceps. This may help abate ongoing bleeding.
n
Consult an ob/gyn for an open cervical os (suggesting inevitable or incomplete abortion),
ongoing profuse bleeding, hypovolemic shock, or continued decreasing hemoglobin or
hematocrit in the ED.
n
Establish maternal rhesus (Rh) type to determine the need for RhoGAM.
Chapter 78 SPONTANEOUS ABORTION, ECTOPIC PREGNANCY, AND VAGINAL BLEEDING 549
Quantitative serum b-human chorionic gonadotropin (b-hCG) assay is helpful in assessing
ectopic risk and coordinating follow-up.
10. What is the prognosis for patients with threatened abortion?
Patients with bleeding and a closed internal os have a risk of miscarriage estimated at 35% to
50%. If fetal cardiac activity is shown on ultrasound, risk of subsequent miscarriage is much
lower. There is no treatment regimen that influences the course of a threatened abortion.
Expectant management for women in early pregnancy failure can be as effective as medical or
surgical management if the fetus is less than 13 weeks of gestation and the mother has stable
vital signs without fever. Successful spontaneous abortion occurs in 91% of incomplete
miscarriages and 26% with missed abortions.
11. Do diagnostic radiographs cause spontaneous abortion?
No. Although there is a risk for the development of fetal chromosomal abnormalities, diagnostic
radiographs (,10 rads) place a pregnant woman at little or no increased risk for miscarriage.
Therapeutic radiation, as well as antineoplastic agents, do increase the incidence of spontaneous
abortion.
12. What factors are associated with spontaneous abortion and/or fetal
abnormalities?
n
Cigarette, alcohol (at high-exposure range), and cocaine use
n
Progesterone-containing, but not copper-containing, intrauterine devices increase the risk
of spontaneous abortion. Oral contraceptives taken either before or during pregnancy have
not been associated with spontaneous abortion.
n
Environmental chemicals (i.e., anesthetic agents, arsenic, aniline, benzene, ethylene oxide,
formaldehyde, lead)
n
Accutane (isotretinoin). Do not use in pregnant women or in women planning to become
pregnant.
n
Increased maternal parity and advanced maternal and paternal age (The frequency
increases from 12% in women younger than age 20–26 to 40% in women age 40.)
n
Conception within 3 months after a live birth
n
Systemic disease of the mother (e.g., diabetes mellitus, cancer, hypothyroidism, or
hyperthyroidism)
n
Laparotomy: The closer the surgery to the pelvic organs, the greater the risk of
spontaneous abortion
n
Uterine defects, including leiomyomas (fibroids), where the location is more important than
the size (submucosal fibroids carry higher risk); and developmental abnormalities including
müllerian duct malformation or fusion and a septate, bicornuate, or unicornuate uterus
13. Is minor trauma a significant factor associated with spontaneous abortion?
No. Fetuses are well protected by maternal structures and amniotic fluid from minor falls
or blows, but penetrating trauma, such as a gunshot wound or stab wound, is dangerous to
the fetus.
14. Is exposure to spermicide before or after conception deleterious to a
pregnancy?
No.
15. Define cervical incompetence.
Cervical incompetence is the painless dilation of the cervix during the second trimester that
leads to spontaneous rupture of membranes and subsequent expulsion of uterine contents.
16. Name the drug used to prevent Rh immunization.
Rh immunoglobulin or RhoGAM. Any pregnant woman who is experiencing vaginal bleeding
must have an Rh type checked. If she is Rh negative and less than 12 weeks’ gestation, she

Chapter 78 SPONTANEOUS ABORTION, ECTOPIC PREGNANCY, AND VAGINAL BLEEDING550
should receive a mini-dose of RhoGAM, 50 mg intramuscularly. If she is greater than 12 weeks’
gestation, the full dose of RhoGAM, 300 mg, should be given.
17. What follow-up instructions should be given to a patient with a threatened
abortion?
Careful instructions are given to return for an increase in pain, bleeding, or signs of
hemodynamic instability, such as syncopal or near-syncopal episodes. The patient should
also be instructed to return for heavy vaginal bleeding. In practice, patients are commonly
instructed to return if bleeding exceeds saturation of 1 pad per hour for 4 to 6 hours,
regardless of symptomatology. The patient should be instructed to bring any passed tissue
to the ED or primary care physician (PCP). Arrangements to repeat quantitative hCG
measurements should be made. Patients with a history of recurrent miscarriages need referral
to a specialist for further evaluation. Patients are instructed to avoid sexual intercourse and
inserting objects into the vagina, such as tampons or douches.
18. What about the emotional aspects of an early miscarriage?
Miscarriage is associated with a significant amount of psychological stress and grieving.
Important therapeutic messages include informing the patient that early miscarriages are
common and that miscarriages are usually due to spontaneous chromosomal abnormalities
and not to the patient’s own actions.
19. What is an ectopic pregnancy (EP)?
An EP is a pregnancy in which implantation of the gestational sac occurs outside of the
uterus. In most cases, the pregnancy is located in the fallopian tubes, but EPs can occur in
the interstitial or cornual portion of the uterus (2%), intra-abdominally (1.5%), on the ovary
(0.1%), or within the cervix (0.1%). EP occurs in approximately 1 in 60 pregnancies in the
United States; the risk is higher in older women and minorities. EP is still the leading cause of
pregnancy-related first-trimester maternal deaths. Most ED series report that about 7% of
first-trimester patients presenting to EDs have an EP diagnosed. Typically, patients with EP will
present with abdominal pain, amenorrhea, or vaginal bleeding. However, more than 50% of
women with EP are asymptomatic before tubal rupture and do not have a risk factor for EP.
20. What are common risk factors for EP?
n
Pelvic inflammatory disease, which can be seen histologically in 50% of patients with EP
n
Prior EP
n
Tubal ligation
n
Intrauterine device use
n
Pelvic surgery
n
Infertility and fertilization procedures (New technology, such as artificial fertilization,
ovulation stimulation, and surgical procedures that result in salvage of potentially abnormal
fallopian tubes, also may contribute to the increased incidence.)
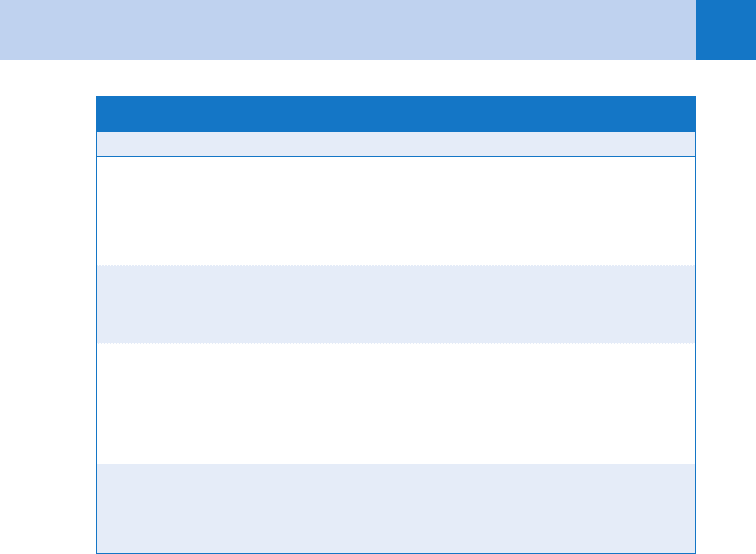
Odds ratios are given in Table 78-1.
21. Define heterotopic pregnancy. What is the main risk factor for this condition,
and what is its incidence?
A heterotopic pregnancy is defined as the simultaneous implantation of an embryo at two or
more sites, most commonly manifested as an IUP and EP. The most significant risk factor is
assisted fertility treatment. In the general population the incidence is thought to be low and
has been historically cited as 1 in 30,000, but it is thought to be increasing, with some
estimating the incidence as 1 in 4,000 or higher. Among patients undergoing fertility
treatments, the incidence is as high as 1 in 100.
22. How reliable are routine serum and urine pregnancy tests in a patient with EP?
Sensitive serum or urine pregnancy tests are almost always positive in EP. b-hCG is secreted
from the time of implantation and is detectable about 7 to 8 days after implantation of the
Chapter 78 SPONTANEOUS ABORTION, ECTOPIC PREGNANCY, AND VAGINAL BLEEDING 551
fertilized ovum. Qualitative pregnancy tests positive at a level of 10 to 50 mlU/mL are positive
in 99% of patients with EP. Home pregnancy tests and less sensitive tests with higher
thresholds may have false-negative results. Serum and urine tests provide similar accuracy for
qualitative testing if their thresholds are similar.
23. What clinical signs and symptoms are useful to increase suspicion of an EP?
The classic picture of EP is of vaginal bleeding, pelvic or abdominal pain, prior missed
menses, and an adnexal mass. However, this picture is neither sensitive nor specific. Missed
menses occur in only 85% of EP patients. Vaginal bleeding and pain may occur only later,
when the growing EP begins to fail or overstretch its abnormal implantation site. Adnexal
masses are palpated in only 50% of patients, even under anesthesia; they may also represent
the corpus luteum of the pregnancy rather than the ectopic gestation itself. Patients at high
risk for EP are those with first-trimester pregnancy and either pelvic pain or risk factors for EP.
Peritoneal signs, severe pain on pelvic examination, and cervical motion tenderness increase
suspicion of a ruptured EP. There is, however, no constellation of historical factors or findings
that confirms or excludes EP with sufficient reliability to obviate the need for evaluation.
24. What are the incidence and risk factors for tubal rupture?
The overall rate of tubal rupture is 18%. Risk factors include the following:
n
History of tubal damage and infertility
n
Induction of ovulation
n
High b-hCG level (510,000 IU/L) at time of diagnosis of EP
25. Why are corpus luteum cysts frequently confused with EPs?
The corpus luteum of the ovary, originating from the Graafian follicle, supports the pregnancy
with secretion of b-hCG and progesterone during the first 6 to 7 weeks of gestation and may
become cystic, growing to 5 cm in diameter or more. Cyst rupture can occur in the first
trimester, presenting as a patient in early pregnancy with sudden pain, unilateral peritoneal
findings, adnexal tenderness, and perhaps a mass.
DES, diethylstilbestrol.
Adapted from data in Ankum WM, Mol BWJ, Van Der Veen F, et al: Risk factors for ectopic pregnancy—
a meta-analysis. Fertil Steril 65:1093, 1996.
Degree of Risk Risk Factors
High (odds ratios 5 2.4–25) Previous ectopic pregnancy
Previous tubal surgery
Tubal pathology
In utero DES exposure
Moderate (odds ratios 5 2.1–21) Previous genital infections
Infertility
Multiple sexual partners
Low (odds ratios 5 0.9–3.8) Previous pelvic/abdominal surgery
Smoking
Vaginal douching
Early age of intercourse (,18 years)
TABLE 78–1. ODDS RATIO FOR RISK FACTORS FOR ECTOPIC PREGNANCY
Chapter 78 SPONTANEOUS ABORTION, ECTOPIC PREGNANCY, AND VAGINAL BLEEDING552
26. What is the most efficient way to diagnose or exclude EP in the ED?
Ultrasound evaluation of early pregnancy is the best first ancillary study; 50% to 75% of
patients have a definitive diagnosis of either IUP or EP. Normal IUPs can be seen by
transvaginal sonography by about 5 weeks’ GA. EPs can be seen on occasion, but an
empty uterus may be the only finding. The risk of EP can be defined further by obtaining a
quantitative hCG level if the ultrasound is inconclusive. IUP, if present, should be detected
on ultrasound when the b-hCG concentration is above the discriminatory zone.
27. Describe the concept of the discriminatory zone as it applies to the serum
b-hCG level.
In the early stages of a normal pregnancy, b-hCG levels increase at a predictable rate,
correlating to expected stages of fetal development. The discriminatory zone is that b-hCG
level at which a normally developing IUP, if present, should be visible by ultrasound. For
transvaginal ultrasonography, the discriminatory zone is generally considered to be between
1,000 and 2,000 mIU/mL, depending on institutional protocols. If a patient has a serum
b-hCG level above the discriminatory zone, but no IUP can be seen by ultrasound, the
suspicion for EP increases significantly.
28. How else is quantitative b-hCG used?
Levels of hCG double every 2 to 3 days during the first 7 to 8 weeks of normal pregnancies.
Because many women do not know the date of their last menstrual period, quantitative levels
may be useful to estimate gestational age and correlate with expected sonographic findings.
With b-hCG above the discriminatory zone, a healthy IUP should be visible by transvaginal
sonography. Failure to double normally during the first 7 weeks indicates a failed pregnancy—
either within the uterus or at an ectopic site. EP is likely if the ultrasound is indeterminate and
the quantitative hCG is above the discriminatory zone or rising on serial measurements. A
rapidly falling hCG level (less than half of the original in 48 hours) is unlikely to be an EP,
whereas slowly falling levels may be seen with EP. A failed pregnancy is more likely to be
ectopic if dilation and curettage fails to detect villi or if no products of conception are found at
the time of miscarriage.
29. Does every patient with bleeding or pain in the first trimester require
ultrasound before discharge from the ED?
All first-trimester complaints are treated as rule out EP until diagnosis of an IUP is
established. In general, an ultrasound should be performed in all patients presenting with
a positive pregnancy test and vaginal bleeding or pain. Unstable patients or those with
peritoneal signs, severe pain, or heavy ongoing bleeding should have their ultrasound
performed in the ED. If ED ultrasound is not available, an ultrasound by radiology should
be ordered.
30. What are the ultrasound findings in patients with suspected EP?
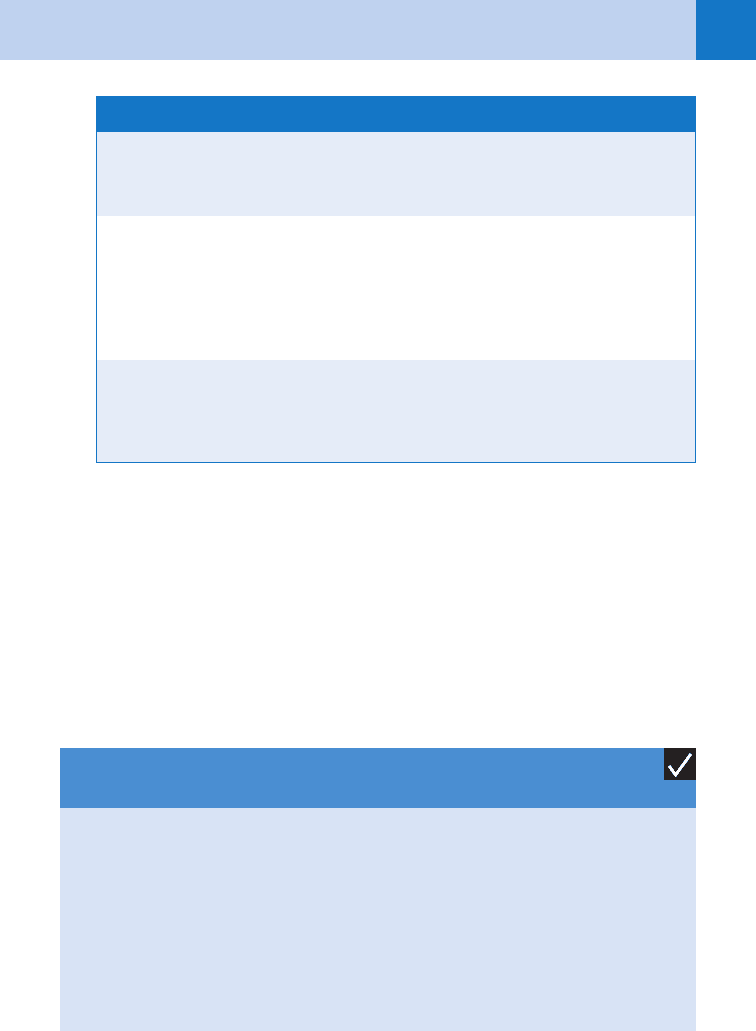
See Table 78-2.
31. What patients with EPs can be discharged from the ED?
Women who are unstable with significant pain or signs of significant blood loss require
admission. ED or inpatient observation may be useful in stable patients with worrisome
symptoms, risk factors, or expected poor compliance to facilitate rapid sonography,
quantitative hCG interpretation, or specialist consultation. Stable patients with indeterminate
ultrasound results (rule out EP) may be followed on an outpatient basis. Expectant
management or chemotherapy for women with few symptoms and low hormonal levels
should be determined in consultation with an ob/gyn. The role of the ED physician is to
consider the diagnosis, make every effort to exclude or make the diagnosis of EP
expeditiously, and make the patient aware of the differential diagnosis and signs that should
be of concern to her, ensuring access to close follow-up care for this potentially fatal
condition.
Chapter 78 SPONTANEOUS ABORTION, ECTOPIC PREGNANCY, AND VAGINAL BLEEDING 553
32. Which EPs should be treated medically with methotrexate?
Medical treatment is often less expensive than laparoscopic surgery and single-dose
methotrexate is effective in 85% of patients. Methotrexate, a folic acid antagonist that inhibits
DNA synthesis and cell reproduction, targets rapidly growing cells and has replaced surgery
for many patients with EPs at low risk for rupture (no fetal heart tones, ,3.5 cm diameter and
without peritoneal signs). Because of significant failure rates, patients must be followed
closely. Failure rates are higher when the b-hCG is .5,000. Patients commonly have
significant pain with or without peritoneal signs several days after treatment with
methotrexate. Abnormal vital signs, a decreasing hematocrit, or diffuse peritoneal signs are
indications of EP rupture.
Diagnostic of IUP
Intrauterine fetal pole or yolk sac
Intrauterine fetal cardiac activity
Suggestive of EP
Moderate or large cul-de-sac fluid without IUP
Adnexal mass* without IUP
Diagnostic of EP
Ectopic fetal heart activity or
Ectopic fetal pole
Indeterminate
Empty uterus
Nonspecific fluid collections
Echogenic material
Abnormal gestational sac
TABLE 78–2. ULTRASOUND FINDINGS IN PATIENTS WITH SUSPECTED ECTOPIC PREGNANCY
EP, ectopic pregnancy; IUP, intrauterine pregnancy.
*Complex mass most suggestive of EP but cyst also can be seen with EP.
Modified from Dart RG: Role of pelvic ultrasonography in evaluation of symptomatic first trimester
pregnancy. Ann Emerg Med 33:310-320, 1999.
KEY POINTS: CANDIDATES FOR MEDICAL TREATMENT OF
ECTOPIC PREGNANCY WITH METHOTREXATE
†
*Sac size .3.5 cm or presence and cardiac activity are relative, not absolute, contraindications.
†
Adapted from ACOG Practice Bulletin No. 94: Medical management of ectopic pregnancy.
1. Hemodynamically stable
2. No evidence of ectopic rupture
3. The ability and willingness to comply with post-treatment monitoring
4. Ectopic gestational sac ,3.5 cm*
5. No fetal cardiac activity on ultrasonographic examination*
33. What are contraindications to methotrexate therapy for ectopic pregnancy?
n
Hemodynamic instability
n
Breastfeeding
n
Immunodeficiency
n
Alcoholism

Chapter 78 SPONTANEOUS ABORTION, ECTOPIC PREGNANCY, AND VAGINAL BLEEDING554
n
Hepatic or renal disease
n
Preexisting blood dyscrasia (e.g., significant leukopenia, anemia, thrombocytopenia)
n
Active pulmonary disease
n
Peptic ulcer disease
n
Known sensitivity to methotrexate
34. Name the sources and causes of third-trimester vaginal bleeding.
The sources are the vagina, cervix, and uterus. In the following list, life-threatening causes are
indicated by an asterisk:
n
Placenta previa: 0.3% to 0.5% of live births*
n
Placental abruption: 0.8% to 1.2% of pregnancies (15%–20% present without vaginal
bleeding)*
n
Uterine rupture: 0.05% of pregnancies*
n
Marginal sinus rupture
n
Bloody show
n
Local trauma
n
Cervical polyps and lesions
35. What is placenta previa? How is it diagnosed?
Placenta previa occurs when the placenta implants on or near the cervical os. Total coverage
of the cervical os by placenta is called complete placenta previa, whereas subtotal coverage
is called partial placenta previa. Marginal placenta previa occurs when the margin of the
placenta approaches but does not cover any of the cervical os.
Placenta previa should be suspected when a pregnant patient in the second half of
pregnancy presents with bright red vaginal bleeding. It is usually painless and may present with
or without uterine contractions. Placenta previa is dangerous, because vaginal penetration or
manipulation of the cervix during a pelvic examination may rupture placental blood vessels and
cause massive hemorrhage. Color flow Doppler ultrasound is 82% sensitive and 91% to 96%
specific for placenta previa. It is frequently diagnosed early in pregnancy and followed with
serial ultrasound studies until delivery, spontaneously resolving in up to 90% of cases
diagnosed before 20 weeks’ gestational age.
36. How is placenta previa treated?
Early consultation with ob/gyn should be obtained when the diagnosis is suspected.
Administer supplemental oxygen, obtain two large-bore intravenous lines, and perform
maternal cardiopulmonary monitoring, and fetal monitoring. Obtain a CBC, hemoglobin, or
hematocrit, and blood type and screen for anticipated transfusion. Place the patient in the left
lateral decubitus position. In the stable patient, ultrasound may confirm the diagnosis.
Because life-threatening bleeding may occur with placenta manipulation, do not perform a
pelvic examination unless you are in the operating room or delivery suite with an experienced
obstetrician. Patients who are hemodynamically stable with small amounts of bleeding may
be admitted for ongoing maternal and fetal monitoring. In selected cases, delivery is delayed
to optimize fetal development. Unstable patients or patients with life-threatening bleeding are
treated by emergency delivery.
37. What is placental abruption (abruptio placentae)? Why is it dangerous?
Placental abruption is the premature separation of the placenta from its insertion on the
uterine wall where a large amount of blood may collect between the placenta and the uterine
wall, causing maternal shock and fetal demise. Abruption occurs spontaneously or after
abdominal trauma. The uterus is firm and the patient reports severe abdominal pain.
Hypotension may occur with vaginal bleeding occurring in about 80% of patients. If vaginal
bleeding does occur, the blood is dark red. This presentation is in contrast to the painless,
bright red bleeding of placenta previa. Placental abruption is diagnosed by ultrasound.
Chapter 78 SPONTANEOUS ABORTION, ECTOPIC PREGNANCY, AND VAGINAL BLEEDING 555
38. Describe the treatment of placental abruption.
Immediately consult an ob/gyn specialist. Start two large-bore intravenous lines, and administer
oxygen. Monitor fetal heart tones and the maternal vital signs. Obtain a CBC, hemoglobin, or
hematocrit, type and screen for anticipated transfusion, and coagulation studies. If the mother
and fetus are stable, arrange an immediate ultrasound. Unstable patients should be transferred
directly to the operating room or delivery suite for delivery.
39. What is uterine rupture? Why is it dangerous?
A grave complication of late pregnancy in which the uterus ruptures, usually during contractions.
It can produce massive, life-threatening intra-abdominal hemorrhage. Maternal mortality is 8%,
and fetal mortality is estimated at 50%. Uterine rupture presents with sudden abdominal pain,
uterine contractions and shock late in pregnancy. There may be scant vaginal bleeding, but the
abdomen is extremely tender. The most significant risk factor for uterine rupture is prior
caesarean section or other uterine surgery.
40. What is the treatment of uterine rupture?
Start two large-bore intravenous lines, and administer oxygen with immediate transfer to the
operating room or delivery suite for laparotomy and hysterectomy. Ultrasound may be
necessary in selected cases to distinguish uterine rupture from placental abruption.
41. Describe the non-life-threatening causes of third-trimester vaginal bleeding.
n
Bloody show is a pink mucous discharge caused by cervical changes that precedes labor
by several hours to a week.
n
The cervix is prone to hemorrhage during late pregnancy, and local trauma from vaginal
penetration, including intercourse, may cause bleeding.
n
Cervical erosions or preexisting polyps produce limited bleeding.
n
Marginal sinus rupture is a premature separation of the placenta limited to the placental
margin.
ACKNOWLEDGMENT
The editors gratefully acknowledge the contributions of Dane M. Chapman, MD, author of this
chapter in the previous edition.
BIBLIOGRAPHY
1. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 94: Medical management of
ectopic pregnancy. Obstet Gynecol 111(6):1479–1485, 2008.
2. Barnhart KT, Gosman G, Asnby R, et al: The medical management of ectopic pregnancy: a meta-analysis
comparing “single-dose” and “multidose” regimens. Obstet Gynecol 101:778–784, 2003.
3. Chou MM, Ho ES, Lee YH: Prenatal diagnosis of placenta previa accreta by transabdominal color Doppler
ultrasound. Ultrasound Obstet Gynecol 15:28–35, 2000.
4. Dart RG, Kaplan B, Varaklis K: Predictive value of history and physical examination in patients with suspected
ectopic pregnancy. Ann Emerg Med 33:283–290, 1999.
5. Garcia CR, Barnhart KT: Diagnosing ectopic pregnancy: decision analysis comparing six strategies. Obstet Gynecol
97:464–470, 2001.
6. Goddijn M, Leschot NJ: Genetic aspects of miscarriage. Baillieres Best Pract Res Clin Obstet Gynaecol
14:855–865, 2000.
7. Luise C, Jermy K, May C, et al: Outcome of expectant management of spontaneous first trimester miscarriage:
observational study. BMJ 324:873–875, 2002.
8. Mirza F, Gaddipati S: Obstetric emergencies. Semin Perinatol 33:97–103, 2009.
9. Morlock RJ, Lafata JE, Eisenstein D: Cost-effectiveness of single-dose methotrexate compared with laparoscopic
treatment of ectopic pregnancy. Obstet Gynecol 95:407–412, 2000.
Chapter 78 SPONTANEOUS ABORTION, ECTOPIC PREGNANCY, AND VAGINAL BLEEDING556
10. Nadukhovskaya L, Dart R: Emergency management of the nonviable intrauterine pregnancy. Am J Emerg Med
19:495–500, 2001.
11. Oyelese Y, Smulian J: Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol 107(4):927–941, 2006.
12. Paul M, Schaff E, Nichols M: The roles of clinical assessment, human chorionic gonadotropin assays, and
ultrasonography in medical abortion practice. Am J Obstet Gynecol 183:S34–S43, 2000.
13. Reardon R, Joing S: First-trimester pregnancy. In: Ma OJ, Mateer J, Blaivas M. Emergency ultrasound, ed 2,
New York, 2008, McGraw-Hill, pp. 279–318.
14. Shelley JM, Healy D, Grover S: A randomized trial of surgical, medical and expectant management of first
trimester spontaneous miscarriage. Aust N Z J Obstet Gynaecol 45:122–127, 2005.
557
THIRD-TRIMESTER COMPLICATIONS
AND DELIVERY
CHAPTER 79
Gina Soriya, MD
1. What is preeclampsia?
Preeclampsia is a condition that occurs in pregnancy after 20 weeks’ gestation, characterized
by new-onset high blood pressure and proteinuria with widespread vascular endothelial
malfunction and vasospasm.
2. What level of hypertension and proteinuria qualify as preeclampsia?
n
Hypertension: In a woman who was normotensive prior to 20 weeks’ gestation, a systolic
blood pressure (BP) greater than 140 mm Hg and a diastolic BP greater than 90 mm Hg. In
a woman who has preexisting hypertension, if the systolic BP has increased by 30 mm Hg,
or the diastolic BP by 15 mm Hg.
n
Proteinuria: Excretion of 300 mg or more of protein in the urine in a 24-hour period.
Note: Edema was previously part of the classic diagnostic triad for preeclampsia; however,
this can be a common finding in pregnancy. In addition, up to one third of preeclamptic
patients do not have edema. It is no longer considered part of the diagnosis of preeclampsia.
3. What are the diagnostic criteria for severe preeclampsia?
The presence of one of the following defines severe preeclampsia: systolic BP greater than
160 mm Hg or diastolic BP greater than 110; pulmonary edema; thrombocytopenia,
microangiopathic hemolysis, symptoms suggesting end-organ involvement, such as
headache, vision changes, and epigastric or right upper quadrant pain; oliguria defined as less
than 500 mL in 24 hours; severe intrauterine growth retardation; oligohydramnios.
4. What causes preeclampsia?
The exact pathophysiology is unknown. Research suggests there may be incomplete invasion
of cytotrophoblasts into the uterine spiral arteries. This leads to placental hypoperfusion,
which may cause the placenta to release factors that circulate in the maternal blood stream,
resulting in widespread endothelial dysfunction and end-organ damage.
5. What are the risk factors for preeclampsia?
Preeclampsia is primarily a complication of first pregnancies. Other risk factors include
conception before age 20, personal or family history of preeclampsia, multi-fetal pregnancies,
advanced maternal age, high body mass index, and adverse outcome in previous pregnancy.
There are also several preexisting medical conditions that can contribute to preeclampsia,
including insulin-dependent diabetes, connective tissue disease, renal disease, chronic
hypertension, and antiphospholipid antibody syndrome.
6. How common is preeclampsia?
Worldwide, 5% to 18% of pregnancies are complicated by preeclampsia. In the United States,
the incidence is 5% to 8%.
7. What is the treatment for preeclampsia?
For mild disease, expectant management is appropriate, with delivery if the patient is at term.
Patients with severe preeclampsia should be admitted and given magnesium sulfate. Anti-
hypertensives should be used for sustained systolic BP greater than 160 mm Hg or sustained
