Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

568
CHAPTER 81
MAXILLOFACIAL TRAUMA
Ethan M. Ross, MD, and Carlo L. Rosen, MD
1. What are the facial bones?
The facial bones are the frontal, temporal, nasal, ethmoid, lacrimal, palatine, sphenoid,
zygoma, maxilla, and mandible.
2. What is the initial approach to a patient with maxillofacial trauma?
The initial management of patients with facial trauma should follow the ABCs (airway,
breathing, and circulation) of trauma resuscitation. The airway is the primary concern and can
be challenging in these patients. Significant facial trauma may cause swelling or distortion of
the airway as a result of bleeding, loose teeth, or fractures. In patients with mandibular
fractures, the tongue loses its support and can occlude the airway. Early endotracheal
intubation should be considered in patients with significant midface or mandibular trauma,
especially if they exhibit any signs of airway distress. Standard methods of intubation, such as
rapid-sequence intubation, should be attempted first. However, airway distortion resulting
from facial trauma sometimes necessitates a cricothyrotomy. All patients with facial and head
trauma should be assumed to have a cervical spine injury. In-line cervical spine stabilization
should be used during intubation. The incidence of cervical spine injuries in patients with
facial trauma is 1% to 4%.
3. Which procedure is contraindicated in patients with maxillofacial trauma?
Nasogastric tube placement should not be performed because of the risk of intracranial
placement through a fracture in the cribriform plate. The small size and flexibility of the
nasogastric tube allow it to be misdirected through a fracture into the brain. There is
also a theoretical concern about placing a nasotracheal tube through the cribriform plate
into the brain. However, an endotracheal tube is larger and more rigid than a nasogastric
tube. The literature suggests that the risk of intracranial placement of a nasotracheal
tube is low.
4. What is a blow-out fracture? What is the entrapment syndrome?
A blow-out fracture is a fracture of the orbital floor that results from a direct blow to
the orbit. Increased intraorbital pressure causes rupture of the floor of the orbit. The
entrapment syndrome is binocular diplopia and paralysis of upward gaze that results from
entrapment of the inferior rectus muscle in the orbital wall defect. Diplopia is noted by
having the patient follow and count fingers on upward gaze. Other physical findings include
infraorbital anesthesia and enophthalmos (posterior displacement of the globe into the
orbit). Patients may have tenderness or step-offs at the infraorbital rim or subcutaneous
emphysema secondary to a fracture into the maxillary sinus. Ophthalmologic evaluation
for associated orbital trauma (globe rupture, hyphema, retinal tear or detachment,
blindness), despite an initially normal visual acuity and funduscopic examination,
should be considered.
Chapter 81 MAXILLOFACIAL TRAUMA 569
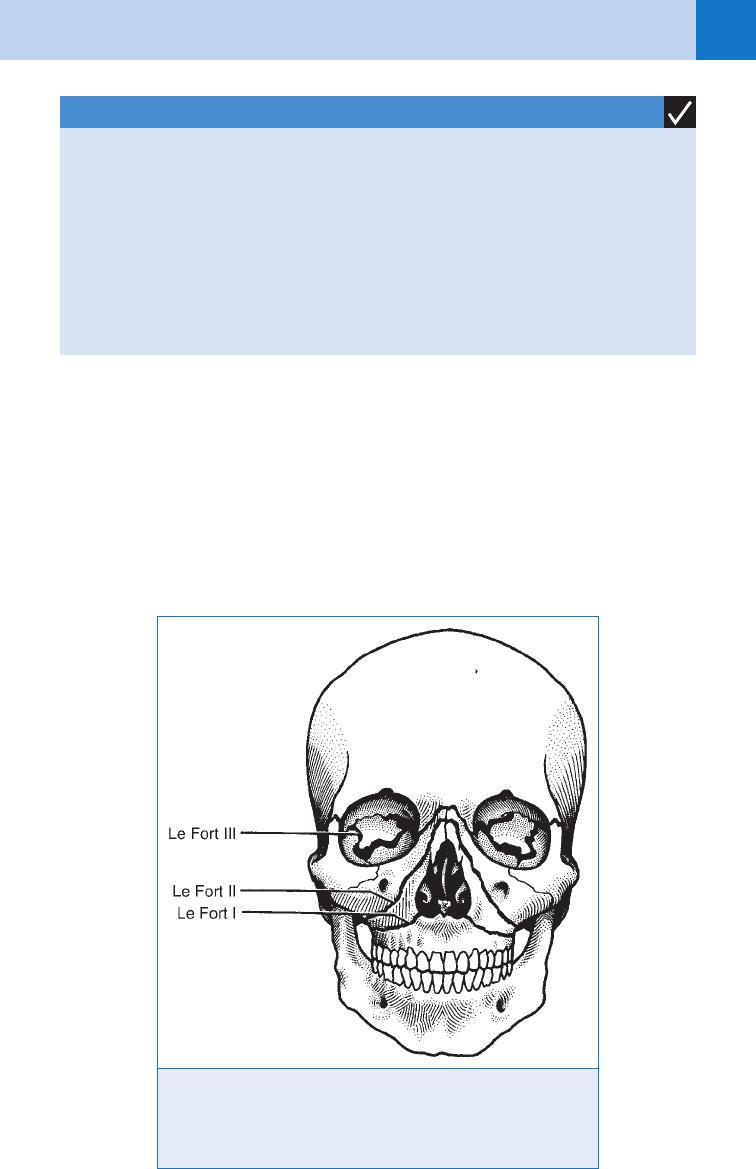
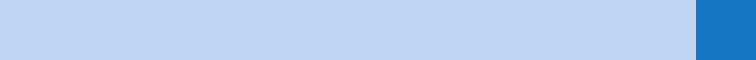
5. What are Le Fort fractures?
The Le Fort classification is used to describe maxillary fractures (Fig. 81-1). Midface fractures
are diagnosed by grasping the upper alveolar ridge and noting which part of the midface moves.
n
Le Fort I, a transverse fracture just above the teeth at the level of the nasal fossa, allows
movement of the alveolar ridge and hard palate.
n
Le Fort II, a pyramidal fracture with its apex just above the bridge of the nose and
extending laterally and interiorly through the infraorbital rims, allows movement of the
maxilla, nose, and infraorbital rims.
n
Le Fort III, the most serious of the Le Fort fractures, represents complete craniofacial
disruption and involves fractures of the zygoma, infraorbital rims, and maxilla.
1. Eyelid edema
2. Enophthalmos
3. Proptosis
4. Limitation of upward gaze
5. Diplopia
6. Infraorbital anesthesia
7. Subcutaneous emphysema
KEY POINTS: CLINICAL SIGNS OF ORBITAL FRACTURES
Figure 81-1. Le Fort classification of facial fractures. Le Fort I: palato
facial disjunction. Le Fort II: pyramidal disjunction. Le Fort III: craniofa-
cial disjunction. (From Cantrill SV: Face. In Marx JA, Hockberger RS,
Walls RM, et al, editors: Rosen’s emergency medicine: concepts and
clinical practice, ed 5, St. Louis, 2002, Mosby, p 325.)
Chapter 81 MAXILLOFACIAL TRAUMA570
It is rare for these fracture types to occur in isolation; they usually occur in combination (one
type on one side of the face and another on the other side).
6. Is there a role for screening patients with LeFort fractures for blunt
cerebrovascular injury?
Blunt cerebrovascular injury (BCVI) to the carotid or vertebral artery is becoming
increasingly recognized in blunt trauma and is found in nearly 1% of all blunt trauma
patients when screening protocols are used. Significant morbidity and mortality is
encountered if left untreated and there is frequently a clinically silent period before
symptoms occur. Although no standard exists for screening, guidelines are being
developed that suggest screening should be undertaken with computed tomographic
angiography (CTA) or standard angiography in patients with signs or symptoms of BCVI
and patients at high risk. High-risk patients include those with a LeFort II or III fracture,
certain cervical spine fracture patterns (subluxation, fractures extending into the
transverse foramen, fractures of C1–C3), basilar skull fracture with carotid canal
involvement, diffuse axonal injury with Glasgow Coma Scale ,6, or near hanging with
anoxic brain injury.
7. When are nasal radiographs indicated?
Almost never. Nasal fractures typically are a clinical diagnosis without the need for routine
radiographs. Physical examination may reveal swelling, angulation, bony crepitus, deformity,
pain on palpation, epistaxis, and periorbital ecchymosis. Nasal radiographs are neither
sensitive nor specific for fractures. The results do not alter management.
8. What is a septal hematoma? Why is it important?
All patients with nasal trauma and suspicion of a nasal fracture require inspection of the nasal
septum for a septal hematoma. This is a collection of blood between the mucoperichondrium
and the cartilage of the septum. It appears as a grape-like swelling over the nasal septum. If
left undrained, it may result in septal abscess, necrosis of the nasal cartilage, and permanent
deformity. If a septal hematoma is identified, incision and drainage is indicated in the ED,
followed by nasal packing, antistaphylococcal antibiotics (prophylaxis for toxic shock
syndrome), and prompt referral.
9. When should a consultation be obtained for a nasal fracture?
Most nasal fractures do not require immediate reduction unless there is significant deformity
and malalignment. After anesthetizing the nose with lidocaine or tetracaine-soaked gauze
or pledgets, early reduction of an angulated fracture is performed by exerting firm, quick
pressure toward the midline with both thumbs. Patients should be referred to a maxillofacial
or plastic surgeon for follow-up in 4 to 7 days. Immediate consultation is suggested for nasal
fractures with associated facial fractures, cerebrospinal fluid rhinorrhea, and sustained
epistaxis.
10. How is a frontal sinus fracture diagnosed?
Frontal sinus fracture should be suspected in any patient with a severe blow to the forehead.
There is often an associated brain injury. The clinical signs include supraorbital nerve
anesthesia, anosmia, cerebrospinal fluid rhinorrhea, subconjunctival hemorrhage, crepitus,
and tenderness to palpation. The preferred diagnostic modality is computed tomography (CT)
to determine if there is involvement of the anterior or posterior walls of the sinus or
intracranial hemorrhage.
11. How are frontal sinus fractures treated?
After surgical consultation, patients with nondisplaced anterior wall fractures may be
discharged on prophylactic antibiotics, with instructions to avoid Valsalva maneuvers and
to follow up in 1 week with the surgical consultant. Patients with displaced anterior wall
and sinus floor fractures require surgical consultation, admission, and antibiotic therapy.

Chapter 81 MAXILLOFACIAL TRAUMA 571
Patients with posterior wall fractures require antibiotics and immediate neurosurgical
consultation.
12. What are the classic zygoma fractures?
The zygoma is the third most commonly fractured facial bone (after the nose and mandible).
Zygoma fractures are classified into three basic types:
n
Arch: The bone may be fractured in one or two places and may be nondisplaced or
displaced medially. Pain and trismus are caused by bony arch fragments abutting the
coronoid process of the mandible. Because the masseter muscle originates on the zygoma,
any movement causes further arch disruption. The fracture is diagnosed by the plain
radiograph bucket-handle view (submentovertex).
n
Tripod: Also termed a zygomaticomaxillary fracture, this is the most serious type of
zygoma fracture and involves the infraorbital rim, the zygomaticofrontal suture, and the
zygomaticotemporal suture. Clinical signs include deformity (flatness of the cheek),
infraorbital nerve hypesthesia, inferior rectus muscle entrapment, and diplopia on upward
gaze. Although these fractures may be detected on plain radiographs (Waters and Caldwell
views), CT is necessary to better define the extent of the fracture. For these fractures,
admission and consultation with a maxillofacial surgeon are required.
n
Body: Fracture of the body of the zygoma, which involves the clinical signs and symptoms
of the tripod fracture, results from severe force and leads to exaggerated malar depression.
13. What is the tongue blade test?
Patients with mandible fractures have mandibular tenderness and deformity, sublingual
hematoma, and malocclusion on physical examination. The jaw appears asymmetric, with
deviation toward the side of the fracture. The tongue blade test is performed by asking the
patient to bite down on a tongue depressor. The tongue blade should be twisted by the
examiner. If there is no fracture, the patient should be able to break the blade. In the presence
of a mandible fracture, the patient opens his or her mouth and the tongue blade remains intact.
14. Which imaging studies should be ordered to diagnose a mandible fracture?
Mandible fractures are the second most common facial fracture. Multiple fractures are
common (.50%) because of the ring structure of the bone. Always check for a second
fracture. If available, the Panorex view is the most useful view for detecting mandible
fractures. It provides a 180-degree view of the mandible and can detect fractures in all regions
of the mandible, including symphyseal fractures that can be missed with the other views. If a
Panorex radiograph is unavailable, the standard mandible series can be used. This comprises
a posteroanterior view (for detecting fractures of the angle and body of the mandible), lateral
and bilateral oblique views (for detection of rami fractures), Townes view (anteroposterior
view that projects the rami and condyles), and often a submentovertex view. A condylar
fracture may be missed by plain radiographs. If this fracture is suspected and the plain
radiographs are negative, facial CT is indicated.
15. What are the most commonly fractured areas of the mandible?
The most commonly fractured areas are the body, the condyle, and the angle of the mandible.
16. What is the mechanism for a temporomandibular joint dislocation? How is it
treated?
Temporomandibular joint dislocation can result from blunt trauma to the mandible, but it also
can occur with exaggerated opening or closing of the jaw such as after a seizure or with
yawning. Patients with a temporomandibular joint dislocation present with jaw deviation away
from the side of the dislocation if it is a unilateral dislocation or with the mandible pushed
forward (underbite) if it is a bilateral dislocation. After conscious sedation with benzodiazepine
for masseter muscle relaxation and a narcotic for pain relief, the emergency physician should
place gauze-wrapped thumbs on the posterior molars while standing above and behind the
patient. The mandible is then pushed downward and posterior.
Chapter 81 MAXILLOFACIAL TRAUMA572
17. When is a CT scan indicated in the evaluation of maxillofacial trauma?
In patients with a history of facial trauma but with minimal physical findings consistent with
fractures or an equivocal examination, plain radiography should be used as a screening test.
The standard plain film series of the face includes a Waters (occipitomental) view, Caldwell
(occipitofrontal) view, submentovertex view, and lateral view. The Waters view visualizes
the orbital rim, infraorbital floor, maxilla, and maxillary sinuses and is useful as an initial
examination in patients with suspected orbital floor fractures. Performance of this view
requires that the cervical spine be clear because the patient is in the prone position. Fluid in
the maxillary sinus is indirect evidence of fracture. The Caldwell view allows visualization of
the superior orbital rim and the frontal sinuses. The lateral view shows the anterior wall of the
frontal sinus and the anterior and posterior walls of the maxillary sinus.
In patients with physical findings that are highly suggestive of facial fractures (tenderness,
step-offs, crepitus, or evidence of entrapment), some authors recommend proceeding directly
to CT. This allows appropriate surgical planning. High-resolution, thin-cut CT scanning is the
preferred modality for the elucidation of bony and soft-tissue injury in maxillofacial trauma.
This is the preferred test in any patient with suspected tripod, orbital, or midface fractures. In
patients with suspected orbital fractures, CT scan with coronal and axial sections should be
ordered (2- to 3-mm cuts).
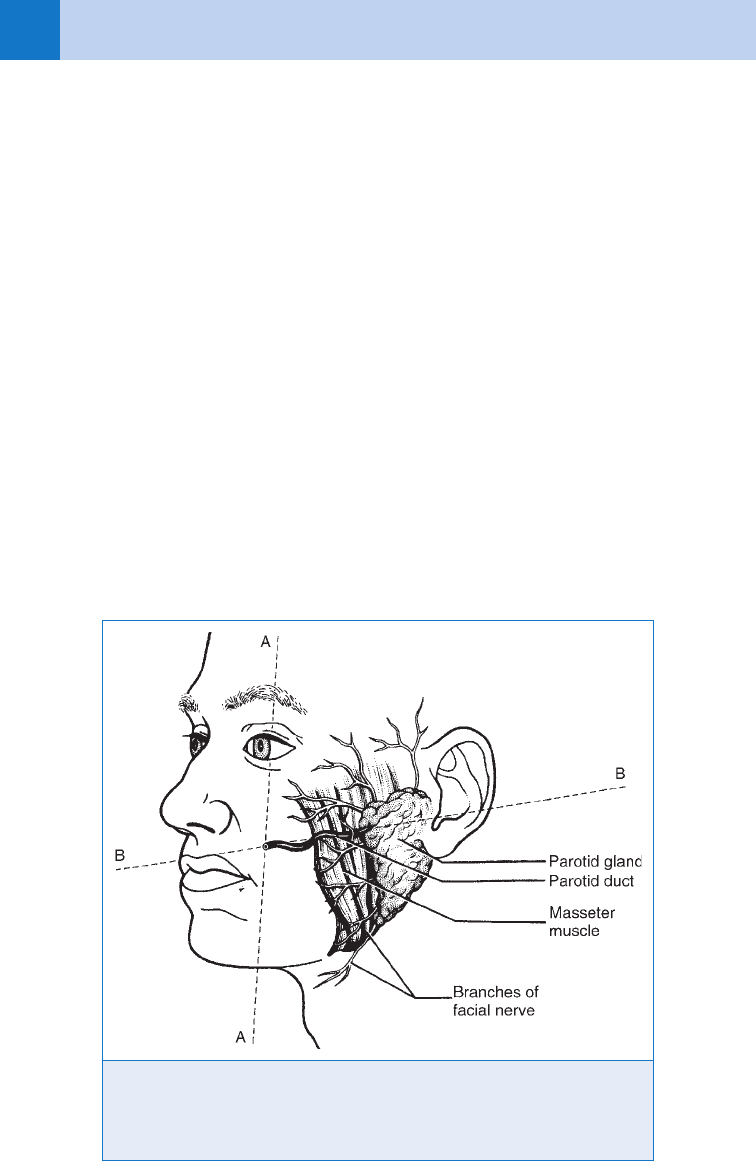
18. How do I recognize an injury to Stenson’s duct?
Stenson’s (parotid) duct arises from the parotid gland and courses from the level of the
external auditory canal (superficial) through the buccinator muscle to open at the level of the
upper second molar (Fig. 81-2). Any laceration at this level may involve the parotid gland,
parotid duct, or buccal branch of the facial nerve. Laceration of the parotid system is
Figure 81-2. Parotid gland and parotid duct with nearby branches of the facial nerve. Line
B demonstrates approximate course of parotid duct from parotid gland, entering mouth at
junction of lines A and B. (From Cantrill SV: Face. In Marx JA, Hockberger RS, Walls RM,
et al, editors: Rosen’s emergency medicine: concepts and clinical practice, ed 5 St. Louis,
2002, Mosby, p 323.)
Chapter 81 MAXILLOFACIAL TRAUMA 573
recognized by a flow of saliva from the wound or bloody drainage from the duct orifice.
Careful exploration reveals whether the flow is from the parotid gland or duct. The buccal
branch of the facial nerve travels in close proximity to Stenson’s duct; injury leads to drooping
of the upper lip, which indicates a possible parotid duct injury. To assess for parotid duct
patency, the parotid gland should be milked to see if saliva is expressed from the intraoral
opening of the parotid duct. Damage to the duct requires repair over a stent and plastic
surgical consultation.
19. When should closure of a facial laceration be deferred?
Closure of facial lacerations in the ED depends on the severity of facial and systemic injuries.
Complex lacerations in patients needing operative intervention should be cleansed with normal
saline, covered with moist gauze, and deferred for intraoperative closure. Closure of the highly
vascular tissues of the face may be delayed for up to 24 hours. Wounds involving the facial
nerve, lacrimal duct, parotid duct, and avulsions should be referred on presentation to the
appropriate surgeon for definitive care.
20. What deformity may arise from blunt trauma to the ear?
An acute auricular hematoma is a collection of blood separating the perichondrium from the
underlying cartilaginous layer that may develop after a blow to the ear. If a hematoma is left
undrained or an auricular compression dressing not applied after incision and drainage of a
hematoma or repair of a pinna laceration secondary to blunt trauma to the ear, necrosis of the
cartilage may develop with resultant deformity known as Cauliflower ear.
21. How is the ear anesthetized?
A subcutaneous circumferential injection of plain lidocaine should be placed at the base of the
pinna. Lacerations in the external auditory require topical anesthesia with 4% lidocaine or
local injection.
BIBLIOGRAPHY
1. Cantrill SV: Face. In Marx JA, Hockberger RS, Walls RM, et al, editors: Rosen’s emergency medicine: concepts
and clinical practice, ed 5, St. Louis, 2002, Mosby, pp 314–329.
2. Cothren CC, Biffl WL, Moore EE, et al: Treatment for blunt cerebrovascular injuries: equivalence of
anticoagulation and antiplatelet agents. Arch Surg 144(7):685–690, 2009.
3. Druelinger L, Guenther M, Marchand EG: Radiographic evaluation of the facial complex. Emerg Med Clin North
Am 18:393–410, 2000.
4. Ellis E, Scott K: Assessment of patients with facial fractures. Emerg Med Clin North Am 18:411–448, 2000.
5. Jones SE, Mahendran S: Interventions for an acute auricular haematoma. Cochrane Database Syst Rev
(2):CD004166, 2004.
6. MacLaughlin J, Colucciello S: Maxillofacial injuries. In Wolfson AB, Hendey GW, Hendry PL, et al, editors:
Harwood-Nuss’ Clinical practice of emergency medicine, ed 4, Philadelphia, 2005, Lippincott Williams &
Wilkins, pp 928–937.
7. Rosen CL, Wolfe RE, Chew S, et al: Blind nasotracheal intubation in the presence of facial trauma. J Emerg
Med 15:141–145, 1997.
574
CHAPTER 82
CERVICAL SPINE AND
SPINAL CORD TRAUMA
Michael J. Klevens, MD, FAAEM, and Robert M. McNamara, MD, FAAEM
1. What is the annual incidence of spinal cord injury (SCI)?
Approximately 12,000 new cases per year. Of these causes, the percentage of violent causes
has been increasing.
2. Name the most common causes of SCI.
n
Vehicular crashes (42.1%)
n
Falls (26.7%)
n
Violence, primarily gunshot wounds (15.1%)
n
Sports (7.6%)
n
Other (8.6%)
3. What are the most common levels of injury?
The most frequent level of injury is C5, followed by C4, C6, C7, T12, and L1. Overall about half
are cervical injuries.
4. In patients discharged from the hospital with neurologic impairment, what
percentage has paraplegia and what percentage has tetraplegia
(quadriplegia)?
n
Incomplete tetraplegia (30.1%)
n
Complete paraplegia (25.6%)
n
Complete tetraplegia (20.4%)
n
Incomplete paraplegia (18.5%)
One percent has complete recovery by discharge. An injury to one of the eight cervical
vertebrae can cause tetraplegia. People with paraplegia have injuries to the thoracic, lumbar,
or sacral regions. Over the past 15 years, the percentage of people with incomplete tetraplegia
has increased slightly, while complete paraplegia has decreased slightly.
5. If most spinal injuries do not cause neurologic injury, why do I care?
The management of any spinal injury is important because improper care can result in
permanent neurologic injury. It is important to have an index of suspicion for injury and
proper immobilization and handling of the patient. It is imperative to have good-quality
diagnostic imaging because inadequate studies and interpretation errors can lead to
permanent injury.
6. What is the financial impact of an SCI?
Huge. The health care and living costs can vary greatly, depending on what severity of injury
was sustained and the age of the individual at time of injury. The estimated yearly costs can
range from $16,500 to $143,500. This does not include the first year costs, which range from
$236,000 to $801,000. The lifetime costs can range from $704,000 to $3.1 million.
7. What is the average age of the person who sustains an SCI?
SCI is devastating in that it primarily affects young healthy adults. Since 2005, the average age
at injury is 40.2 years. The predominant age range is between 16 and 30. An overwhelming
percentage of injuries are suffered by males. There has been a slight trend toward older age
recently, likely reflecting the preserved mobility of an aging population.
Chapter 82 CERVICAL SPINE AND SPINAL CORD TRAUMA 575
8. Name the causes of reduced life expectancy in SCI patients.
Pneumonia, pulmonary emboli, and sepsis.
9. Are there any underlying conditions that could precipitate or heighten the
chance of an SCI?
Less force is required to cause fractures in the elderly. Rheumatoid arthritis can lead to
subluxation problems at C1 and C2. Normal development of the odontoid may not occur in a
Down syndrome patient. Osteoporosis and metastatic cancer may lead to a vertebral fracture
with insignificant trauma.
10. How do I immobilize the potential spinal injury patient?
When any spinal injury is suspected, initially, the entire spine should be immobilized with a
long board. The cervical spine is immobilized with a hard collar. There are several different
types of stiff cervical collars, such as the Philadelphia or Ambu brand collars. The emergency
medical service (EMS) stabilization may also include the forehead taped to the board and
accessory towel, sandbag, or other bolsters to prevent further neck movement. The sandbag
and tape method without a rigid collar support should not be used. It is interesting that total
spinal immobilization has never been proven to prevent secondary spinal injury. However,
there continue to be sporadic case reports of such injuries. Therefore, it is prudent to follow
these initial guidelines. It is recommended that the patient be removed from the long board as
soon as possible to prevent soft tissue injury.
11. How should one approach the patient with potential spinal injury?
There are several mnemonics for the initial stabilization of any trauma patient. Advanced
trauma life support (ATLS) teaches the ABCDE mnemonic:
A 5 Airway
B 5 Breathing
C 5 Circulation
D 5 Disability
E 5 Exposure
According to another mnemonic, a proper history is A MUST:
A 5 Altered mental state. Check for drugs or alcohol.
M 5 Mechanism.* Does the potential for injury exist?
U 5 Underlying conditions. Are high-risk factors for fractures present?
S 5 Symptoms. Is pain, paresthesia, or neurologic compromise part of the picture?
T 5 Timing. When did the symptoms begin in relation to the event?
*Because fall injuries are common, the physician should get information as to the height
of the fall and any preceding events such as syncope, chest pain, or seizure.
12. What should be assessed on physical examination?
There are two key areas: the spine itself and the neurologic examination. The spine is palpated
to assess for tenderness, deformity/step-off, and muscle spasm. It is important to understand
that the examiner feels only the posterior elements of the vertebrae; therefore, a fracture may
be present despite a lack of tenderness. The neurologic examination should include motor
function, sensory function, some aspect of posterior column function (position and vibration),
and a rectal examination. Regarding sensory testing, the assessment of light touch examines
the integrity of the posterior neurological column while pinprick testing assesses the anterior
column. In an unconscious patient, the only clues may be poor rectal tone, priapism, absence
of deep tendon reflexes, or diaphragmatic breathing.
13. What is neurogenic shock? How is it treated?
Neurogenic shock is a syndrome with loss of neurologic function and accompanying
autonomic tone. This is usually exhibited by flaccid paralysis with loss of reflexes and loss
of urinary and rectal tone. Accompanying this are bradycardia, hypotension, hypothermia,
and ileus. The diagnosis of neurogenic shock should only be made after all other forms of

Chapter 82 CERVICAL SPINE AND SPINAL CORD TRAUMA576
shock have been eliminated. Hypotension is usually successfully treated with rapid infusion
of crystalloid. If intravenous fluids are not adequate to maintain organ perfusion, the use
of dopamine or phenylephrine may be beneficial. Bradycardia can be treated with atropine or
dopamine. In refractory bradycardia, a pacemaker may be required. In most cases of
neurogenic shock, hypotension resolves within 24 to 48 hours.
14. What are the general principles of emergency treatment in the patient with
spinal cord trauma?
First, do no harm. As stated previously, that means proper immobilization and coordinated
movement of the patient, when absolutely necessary. A higher level of cervical injury results in a
more devastating injury to the patient. Any patient with an injury above C5 probably should be
intubated because the phrenic nerve roots, which supply the diaphragm, emerge from C3 to C5.
Rapid-sequence intubation (RSI) oral-tracheal intubation with manual in-line cervical-spine
stabilization is considered the safest way to intubate these patients. Early gastric and bladder
decompression are also indicated. Overhydration should be avoided so as to not cause pulmonary
edema. The absence of pain below the level of injury can mask other injuries. The patient with
neurologic deficit faces a difficult hospital stay, and the ED should use full sterile precautions for
any procedure such as urinary catheters or central venous access when possible.
15. How do I determine which patients need spine radiographs?
There are two validated decision rules available to the emergency physician. One is the
National Emergency X-Radiography Utilization Study (NEXUS) decision rule. The other is the
Canadian C-Spine Rule (CCR). Both have been shown to reduce the number of radiographs
necessary to identify important cervical-spine injury.
16. What are the NEXUS criteria?
n
No midline cervical tenderness
n
No focal neurologic deficit
n
Normal alertness
n
No intoxication
n
No painful distracting injury
If patients meet the criteria, there is a high likelihood that they have a low probability of injury
and that cervical radiography is not needed. In this large multicenter study, the overall rate of
missed cervical spine injuries was less than 1 in 4,000 patients. Note that there are specific
definitions of the previous five criteria that must be reviewed when applying the NEXUS
criteria. This rule was 99.6% sensitive and 12.9% specific for significant injury.
17. What is the CCR?
The CCR asks three questions:
n
Is there any high-risk factor that mandates radiography? These are:
a. age . 65
b. significant mechanism of injury (i.e., fall from .1 m, axial loading injury, high speed
MVA/rollover/ejection, bike collision)
c. the presence of paresthesias
n
Can the patient be assessed safely for range of motion (simple mechanism, sitting position
in the ED. ambulatory at any time, delayed onset of neck pain, or absence of midline
cervical spine tenderness)?
n
Can the patient actively rotate the neck 45 degrees to the left and the right?
This study had a sensitivity of 100% and a specificity of 42.5% for identifying clinically
important cervical-spine injuries. Again, one needs to review the rule completely before
applying it to patients.
18. What are distracting injuries?
NEXUS: includes a long list such as long bone fractures, large lacerations, visceral injury, and
burns
CCR: injuries such as fractures that are so severely painful that the neck examination is unreliable.
Chapter 82 CERVICAL SPINE AND SPINAL CORD TRAUMA 577
19. Can these decision rules be applied to children?
It is difficult to validate the NEXUS or CCR in children because there has been a paucity of
studies in this population. Additionally, some of the criteria in the CCR and NEXUS are difficult
to verify in toddlers and children because of their inherent immaturity and unpredictability.
20. Which type of radiographs should be
obtained?
The standard three-view of the cervical spine is
an anteroposterior (AP), lateral, and open-mouth
(odontoid). During the initial evaluation, a cross-
table lateral radiograph should be taken because
the patient does not have to move. It is extremely
important that cervical-spine precautions not be
discontinued based solely on the cross-table
lateral. Some studies have reported that up to
18% of cervical-spine injuries are missed with the
cross-table lateral radiograph alone. The most
commonly missed injuries are at C1 to C2,
followed by the lower C6-C7-T1 junction. In the
elderly, C1 and C2 fractures account for
approximately 70% of cervical-spine fractures.
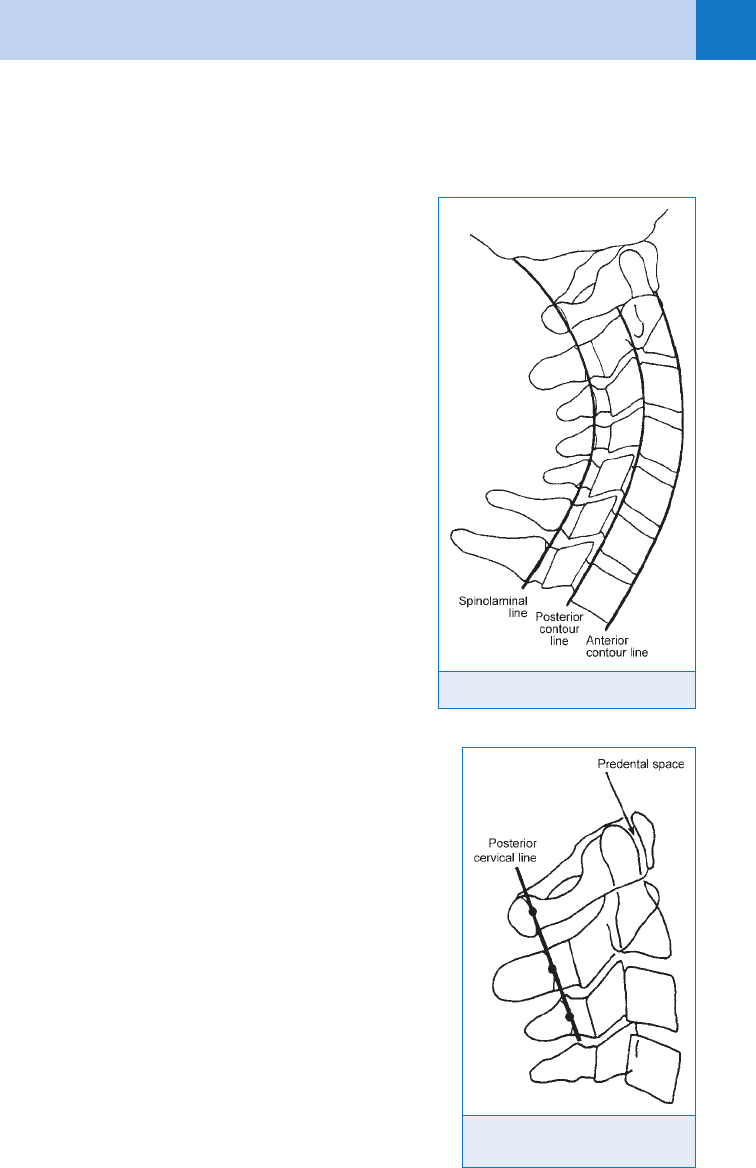
21. How do I interpret the lateral cervical
spine radiograph?
The first rule is to make sure that the radiograph is
technically adequate and that the top of T1 is visible
on the film. Next, follow the mnemonic ABCS:
A 5 Alignment. Check for a smooth line at the
anterior and posterior aspect of the
vertebral bodies and the spinolaminar
line from C1 to T1 (Fig. 82-1)
B 5 Bones. Check each vertebral body to
ensure that the anterior and posterior heights
are similar (.3 mm difference suggests
fracture); follow the vertebrae out to the
laminae and spinous process. Look carefully
at the upper and lower cervical segments
where fractures are likely to be missed.
Examine the ring of C2, which can show a
fracture through the upper portion of the
vertebral body of C2.
C 5 Cartilage. Check the intervertebral joint
spaces and the facet joints.
S 5 Soft-tissue spaces. Look for prevertebral
swelling, especially at the C2 to C3 area
(. 5 mm) and check the predental space
(Fig. 82-2), which should be less than
3 mm in adults and less than 5 mm in
children. From C4 to C7 the soft-tissue
thickness should not be greater than 22 mm.
22. What are the indications for flexion-
extension views of the cervical spine?
Based on the NEXUS study, flexion-extension imaging
is unnecessary in the acute evaluation of patients
Figure 82-1. Curve of alignment.
Figure 82-2. Posterior cervical
line and predental space.
