Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 82 CERVICAL SPINE AND SPINAL CORD TRAUMA578
with blunt trauma. A computed tomography (CT) or magnetic resonance imaging (MRI) would
give more information in the presence of specific clinical concerns for ligamentous damage or
fracture not diagnosed on plain films.
23. When would a CT or MRI be ordered?
Routine indications are when plain radiographs are inconclusive or difficult to interpret and
you have suspicion of spinal injury. A CT is good for detection of bony injury and to identify
surgical conditions such as hematoma or disk fragments within the spinal canal. With the
advent of rapid helical scanning, many centers are increasing their use of the CT scan in place
of plain radiographs, especially if the patient has an indication for a head CT. A CT scan is also
needed for the clearance of the cervical spine in comatose or obtunded patient. In a study of
patients with traumatic brain injury, 5.4% of the patients had C1 or C2 fractures and 4% had
occipital condyle fractures that were not visualized on the three-view radiography series. An
MRI is useful to identify injury to the spinal cord itself in the face of neurologic deficit. The
MRI can show areas of contusion and edema within the spinal space. An MRI can also detect
rupture of intervertebral disks and ligamentous injury. CT is better than MRI for the
identification of vertebral fractures.
24. What is SCIWORA?
It is Spinal Cord Injury Without Radiographic Abnormalities. Children are more susceptible to
SCIWORA because of the greater elasticity of their cervical structures. This leads to transient
spinal column subluxation and stretching of the spinal cord. These pediatric patients may have
a brief episode of upper extremity weakness or paresthesias with delayed development of
neurologic deficits that appear hours to days later. MRI should be obtained on all patients with
SCIWORA.
1. It is important to have a high index of suspicion for injury and ensure proper immobilization
and handling of the patient.
2. Use clinical decision rules such as NEXUS or Canadian C-spine Rule to minimize cervical
spine radiographs.
3. The use of steroids in blunt spinal cord trauma is not standard of care.
4. Special populations, such as pediatric and geriatric, need a more thorough work-up than the
normal adult.
5. The three-view c-spine series is mandatory in evaluations if you are getting plain radiographs,
whereas the flexion-extension view is not needed in the acute setting.
KEY POINTS: SPINAL CORD TRAUMA
25. Describe the Jefferson, Hangman, Clay Shoveler, and Chance fractures.
n
Jefferson fracture is a burst fracture of the ring of C1 that occurs from axial loading.
n
Hangman fracture is a disruption of the posterior arch of C2.
n
Clay-Shoveler fracture is a fracture of the spinous process that is classically caused by
forceful cervical extension.
n
Chance fracture is a vertebral fracture, usually in the lumbar segment, involving the
posterior spinous process, pedicles, and vertebral body. It is caused by the flexion forces
on the spinal column. This is associated with the use of lap belts.
26. Describe the incomplete cord syndromes or injuries.
n
Anterior cord syndrome results in loss of function in the anterior two thirds of the spinal
cord from damage to the corticospinal and spinothalamic pathways. Findings include loss
of voluntary motor function and pain and temperature sensation below the level of the
Chapter 82 CERVICAL SPINE AND SPINAL CORD TRAUMA 579
injury, with preservation of the posterior column functions of position and function.
The key issue is the potential reversibility of this lesion if a compressing hematoma or disk
fragment can be removed. This condition requires immediate neurosurgical evaluation.
n
Central cord syndrome results from injury to the central portion of the spinal cord.
Because more proximal innervation is placed centrally within the cord, this lesion results in
greater involvement of the upper extremities than of the lower extremities. Bowel or bladder
control is usually preserved. The mechanism of injury is hyperextension of a cervical spine
with a cord space narrowed by congenital variation, degenerative spurring, or hypertrophic
ligaments. This syndrome can occur without actual fracture or ligamentous disruption.
n
Brown-Séquard syndrome is a hemisection of the spinal cord, usually from penetrating
trauma. Contralateral sensation of pain and temperature is lost, and motor and posterior
column functions are absent on the side of the injury.
n
Cauda equina syndrome is an injury to the lumbar, sacral, and coccygeal nerve roots
causing a peripheral nerve injury. There can be motor and sensory loss in the lower
extremities, bowel and bladder dysfunction, and loss of pain sensation at the perineum
(saddle anesthesia).
27. What is the significance of sacral sparing and spinal shock?
Sacral sparing refers to the preservation of any function of the sacral roots, such as toe
movement or perianal sensation. If sacral sparing is present, the chance of functional
neurologic recovery is good. Spinal shock is a temporary concussive-like condition in which
cord-mediated reflexes, such as the anal wink, are absent. Spinal shock also may result in
bradycardia and hypotension. The extent of cord injury—and prognosis—cannot be determined
until these reflexes return.
28. What can physicians do to prevent spinal injuries?
Get involved in injury prevention and education. Due to the predominance of vehicle crashes
causing SCIs, one can work to reduce driving under the influence of alcohol and drugs. This
includes using cellphones or texting while driving. Further, the use of safety belts should be
emphasized at discharge in every ED visit, regardless of the reason the person came in for
treatment. Diving and sporting injuries can be reduced by proper public education and coaching.
CONTROVERSY
29. What is the status of steroids in spinal cord trauma?
This has been a very controversial topic. In 1975, the first National Acute Spinal Cord Injury
Study (NASCIS) was established. This was followed by NASCIS 2 and NASCIS 3, which
was completed in 1998. The dosage of methylprednisolone was an initial bolus of 30 mg/kg
intravenously over 15 minutes, followed 45 minutes later by a continuous infusion of
5.4 mg/kg/hr for 23 hours. This was given within 3 hours of injury. When the therapy was
initiated 3 to 8 hours after injury, patients were maintained on an infusion for 47 hours.
Initial support for the use of steroids was encouraging, but multiple reviews of the NASCIS
study and other literature have shown that there is insufficient evidence to support the use
of corticosteroids in the treatment of patients with acute SCI. Many believe that there were
study design, data presentation, interpretation, and analysis flaws in the NASCIS study.
Further, a recent Level I study showed that patients treated with methylprednisolone had a
higher incidence of complications, such as gastrointestinal (GI) bleed and respiratory
complications. Unfortunately, the overwhelming desire for any improvement has made
steroid therapy a de facto standard of care at many institutions. This conflicts with recent
position statements by the American Academy of Emergency Medicine, Canadian
Association of Emergency Physicians, American Academy of Neurological Surgeons,
and the Congress of Neurological Surgeons. In conclusion, the use of steroids is an
option but is certainly not a standard of care.
Chapter 82 CERVICAL SPINE AND SPINAL CORD TRAUMA580
BIBLIOGRAPHY
1. Barry TB, McNamara RM: Clinical decision rules & cervical spine injury in an elderly patient: a word of
caution. J Emerg Med 4:133–136, 2005.
2. Bracken MB: Steroids for acute spinal cord injury. Cochrane Database Syst Rev Issue 2, Art. No.: CD001046,
DOI:10.1002/14651858.CD001046. 2002.
3. Bracken MB, Shepard MJ, Holford TR, et al: Administration of methylprednisolone for 24 or 48 hours or
tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury: Results of the third national acute
spinal cord injury randomized controlled trial. JAMA 227:1597–1604, 1997.
4. Congress of Neurological Surgeons: Pharmacological therapy after acute cervical spinal cord injury.
Neurosurgery 50(3 Suppl):S63–S72, 2002.
5. Dickinson G, Stiell IG, Schull M, et al: Retrospective application of the NEXUS low-risk criteria for cervical
spine radiography in Canadian emergency departments. Ann Emerg Med 43:507-514, 2004.
6. Knopp R: Comparing NEXUS and Canadian C-spine decision rules for determining the need for cervical spine
radiography. Ann Emerg Med 43:518–520, 2004.
7. Link TM, Schuierer G, Hufendiek A, et al: Substantial head trauma: value of routine CT examination of the
cervicocranium. Radiology 196:741–754, 1995.
8. Manoach S, Paladino L: Manual in-line stabilization for acute airway management of suspected cervical spine
injury: historical review and current questions. Ann Emerg Med 50(3): 236–245, 2007.
9. Mower WR, Hoffman J: Comparison of the Canadian C-spine rule and NEXUS decision instrument in
evaluating blunt trauma patients for cervical spine injury. Ann Emerg Med 43:515–517, 2004.
10. National Spinal Cord Injury Statistical Center, University of Alabama at Birmingham: 2004 Annual Statistical
Report, June 2004, p 119.
11. Nesathurai S: Steroids and spinal cord injury: revisiting the NASCIS 2 and NASCIS 3 trials. J Trauma
45:1088–1093, 1998.
12. Stiell IG, Clement CM, McKnight D, et al: The Canadian c-spine rule versus the NEXUS low-risk criteria in
patients with trauma. N Engl J Med 349:2510–2518, 2003.
13. Stiell IG, Wells GA, Vandemheen KL, et al: The Canadian c-spine rule for radiography in alert and stable
trauma patients. JAMA 286:1841–1848, 2001.
1. American Academy of Emergency Medicine:
www.aaem.org/positionstatements/steroidsinacuteinjury.shtml
2. Canadian Association of Emergency Physicians: www.caep.ca/
3. Eastern Association for the Surgery of Trauma: www.east.org
4. National Spinal Cord Injury Statistical Center: www.spinalcord.uab.edu
WEBSITES
581
CHAPTER 83
HEAD TRAUMA
Edward Newton, MD
1. What is the scope of head injury in the United States?
There are more than 1.1 million ED visits and approximately 70,000 deaths as a result of
head injury every year in the United States. Although the incidence of severe head injury is
decreasing, most likely owing to the preventive benefits of helmets and seat belts and air bags
in automobiles, head trauma remains the most lethal traumatic injury and accounts for a large
proportion of patients with permanent disability. The peak incidence of head injury is in the
15- to 24-year-old age group, with males affected twice as often as females. The spectrum of
head injury includes relatively minor problems, such as lacerations and scalp contusions, and
major, often lethal, intracranial trauma. Distinguishing between minor and potentially lethal
head injuries while using diagnostic resources appropriately is one of the most difficult tasks
facing the emergency physician.
2. What groups of patients are at particular risk from head trauma?
Because assessment of mental status is such an integral part of the evaluation of head-injured
patients, patients who are unable to communicate because they are preverbal (e.g., infants),
intoxicated, mentally impaired, aphasic, or have a language barrier pose a special challenge.
When such communication barriers are present, there should be a lower threshold for
obtaining a computed tomography (CT) scan.
Certain age groups are at higher risk for intracranial injury:
n
Infants are at higher risk because of their relatively large head size and compressibility of
the skull. Infants also are at high risk for nonaccidental trauma (e.g., abusive head trauma,
which is also known as shaken baby syndrome), in which case an accurate history may be
unavailable or deliberately withheld. If the cranial sutures and fontanelles are not closed,
the cranium can expand as a result of intracranial bleeding. Infants can bleed sufficiently
intracranially to produce hemorrhagic shock, whereas in older children and adults, another
source of bleeding is inevitably responsible for shock.
n
The elderly also are at higher risk of intracranial injury, particularly subdural hematoma
(SDH). Cerebral atrophy results in stretching of bridging veins from the dura to the brain
parenchyma, making these veins vulnerable to tearing from deceleration forces.
n
Chronic alcoholics are at risk because of their greater frequency of head trauma, cerebral
atrophy, and coagulopathy.
n
Patients who are taking anticoagulants or antiplatelet agents or who have intrinsic bleeding
diatheses bleed more actively than patients with normal coagulation and have higher
mortality from brain injury.
1. Very young and very old patients
2. Chronic alcoholics
3. Patients with coagulopathy
KEY POINTS: PATIENTS AT HIGH RISK FOR HEAD INJURY

Chapter 83 HEAD TRAUMA582
3. What is a cerebral concussion?
Sudden, transient loss of central neurologic function secondary to trauma. It is characterized
by loss of consciousness, transient amnesia, confusion, disorientation, or transient visual
changes, without any gross cerebral abnormalities or neurological deficits on examination.
4. What is the postconcussive syndrome?
Although the patient may have a completely normal neurologic examination after a concussion,
there are common sequelae from this type of injury. Patients frequently report migraine-type
headaches, dizziness, inability to concentrate, and irritability. Although in 90% of cases these
symptoms resolve within 2 weeks, they rarely may persist for up to 1 year. Treatment is
supportive, and the long-term prognosis is good. A phenomenon known as the second impact
syndrome is recognized in which a second head trauma during a vulnerable period after a
concussion results in severe and often fatal diffuse cerebral edema. Consequently, athletes
should be held out of contact sports until all postconcussive symptoms have resolved.
5. How do you detect cerebrospinal fluid (CSF) leaks caused by basilar skull
fractures?
A patient with signs of basilar skull fracture (i.e., raccoon eyes, hemotympanum, or Battle
sign) with clear drainage from the nose or ear canal should be suspected of having a CSF
leak. Analysis of the glucose content of the drainage by Glucometer or laboratory analysis may
distinguish CSF (containing 60% of serum glucose levels) from nasal mucus (glucose not
present). In cases in which blood is mixed with CSF, applying a drop of the fluid to filter paper
reveals CSF in a target shape with blood at the center and pink-tinged CSF forming an outer
ring. However, bedside tests are neither specific nor sensitive for detecting CSF leaks.
6. How are CSF leaks treated?
CSF leaks through tears in the dura generally are managed conservatively. The use of
prophylactic antibiotics is controversial because they have not been shown to significantly
reduce the incidence of meningitis and may select for antibiotic-resistant bacteria. Patients
must be followed closely until the dural tear heals because of the risk of meningitis. Dural
tears that fail to close spontaneously over 2 to 3 weeks usually require operative repair.
7. How does a patient with epidural hematoma present?
Epidural hematoma occurs in 5% to 10% of severe head injuries. In the classic pattern, a
patient loses consciousness from the initial concussion, gradually recovers over a few
minutes, and enters a lucid interval wherein he or she is relatively asymptomatic and has a
normal neurologic examination. During this interval, accumulation of arterial blood in the
epidural space, usually from a lacerated middle meningeal artery, eventually causes
compression and shift of brain across the midline. This process is accompanied by a
second reduction in the level of consciousness and the pupillary and motor signs of
herniation. This classic pattern occurs in only about 30% of cases, however. Many patients
remain unconscious after the initial impact or with minor hemorrhages, may not develop
increased intracranial pressure (ICP) at all. The characteristic CT scan appearance of an
epidural hematoma is a hyperdense lenticular collection of blood that indents adjacent
brain parenchyma and does not extend beyond cranial sutures where the dura is attached.
8. How does a subdural hematoma (SDH) present?
SDH may be acute, subacute (6–14 days), or chronic (.14 days after trauma).
n
Acute SDH is associated with a high incidence of underlying brain injury. The presentation
varies with the severity of the underlying injury, but patients commonly present with a
diminished level of consciousness, headache, and focal neurologic deficits corresponding
to the area of brain injury. If sufficient bleeding occurs, ICP increases and herniation may
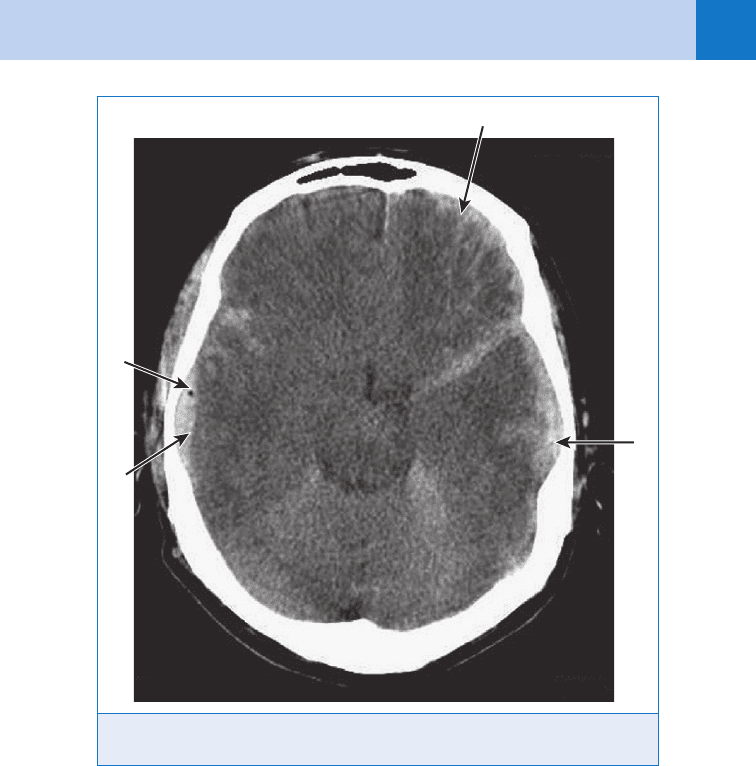
occur. The characteristic appearance of an acute SDH on CT scan is a collection of
hyperdense blood in a crescent-shaped pattern conforming to the convexity of the
hemisphere and often extending past cranial sutures. (Fig. 83-1) At times, the injury causes
Chapter 83 HEAD TRAUMA 583
a minimal amount of bleeding and the patient does not immediately seek medical care. The
SDH undergoes lysis over a period of several days and eventually organizes into an
encapsulated mass.
n
Subacute or chronic SDH is a difficult clinical diagnosis because the symptoms are vague
and common (e.g., persistent headache, difficulty concentrating, lethargy), and the trauma
may have been forgotten. Even the CT scan diagnosis is difficult because subacute SDH
becomes isodense and indistinguishable from surrounding brain unless special contrast-
enhanced CT techniques are used. Chronic SDH appears as an encapsulated lucent
collection of fluid in the same position as the acute type.
9. What is axonal shear injury?
Axonal shear injury occurs during abrupt deceleration because white and gray matter have
different densities and different rates of deceleration. This produces a shearing force that
may tear axons at the white-gray interface, resulting in severe neurologic derangements
such as prolonged coma or persistent vegetative state. The CT scan may appear completely
normal or show only small petechial hemorrhages. Magnetic resonance imaging (MRI) of
the brain is a more sensitive tool in detecting these injuries but is currently impractical in
the acute phase.
Figure 83-1. Computed tomographic scan of the head showing A, Subarachnoid hemorrhage.
B, Subdural hemorrhage. C, Subdural hemorrhage with D, intracranial free air (black dot).
A
B
D
C
Chapter 83 HEAD TRAUMA584
10. What is brain herniation?
Herniation is caused by increased ICP. Because the cranium is a rigid structure, pressure
varies with the volume of its contents. Approximately 10% of intracranial volume is blood,
another 10% is CSF, and the remainder is brain parenchyma and intracellular fluid. An
increase in any of these compartments by blood, tumor, or edema causes a predictable
response. Initially, CSF is forced into the spinal canal, and the ventricles and cisterns collapse.
Once this has occurred, ICP rises steeply, and the brain parenchyma shifts away from the
accumulating blood and herniates through one of several spaces, eventually causing death
by compressing the brainstem.
11. List the four types of herniation syndrome.
n
Uncal herniation
n
Central herniation
n
Cingulate herniation
n
Posterior fossa cingulation
12. Describe uncal herniation syndrome.
The uncus is the most medial portion of the hemisphere and is often the first structure to shift
below the tentorium that separates the hemispheres from the midbrain. As the uncus is forced
medially and downward, the ipsilateral third cranial nerve is compressed, producing pupillary
dilation, ptosis, and oculomotor paresis. As herniation progresses, the ipsilateral cerebral
peduncle and pyramidal tract are compressed, resulting in contralateral hemiplegia.
In approximately 10% of cases, the hemiparesis occurs on the same side as the brain
lesion, making this a less reliable finding for localizing the injury. Further progression results
in brainstem compression with respiratory and cardiac arrest. Transtentorial herniation of this
type is the most common variety.
13. What is central herniation syndrome?
Occasionally, hematomas located at the vertex or frontal lobes cause simultaneous downward
herniation of both hemispheres through the tentorium. Clinical findings are similar to uncal
herniation, except that bilateral motor weakness occurs.
14. How does cingulate herniation occur?
Rarely, the cingulate gyrus is forced medially beneath the falx by an expanding lateral
hematoma, causing compression of the ventricles and impairing cerebral blood flow.
15. Explain posterior fossa herniation.
Bleeding or edema in the posterior fossa can result in herniation of the cerebellar tonsils either
upward through the tentorium or downward through the foramen magnum. In the latter case,
coma and fatal brainstem dysfunction may occur rapidly and with little warning.
16. What is the ED treatment for increased ICP?
n
Maintain adequate cerebral perfusion pressure. Although there is often misguided
reluctance to hydrate vigorously patients with concomitant head and systemic injuries,
cerebral perfusion must be maintained for resuscitation to be successful. Hypotension must
be avoided, and often laparotomy to correct intraabdominal bleeding must take precedence
over neurosurgical intervention to maintain cerebral perfusion. Patients who experience
hypotension (systolic blood pressure , 90 mm Hg) have a twofold increase in mortality.
n
Avoid secondary injuries to the central nervous system. After brain trauma, there is a
cascade of secondary neuronal metabolic injuries that are detrimental to recovery of
neurological function. At present, few interventions have proved effective in limiting these
changes. Certain other treatable conditions either increase the metabolic demands of the
brain or decrease cerebral perfusion and worsen the prognosis unless they are corrected.
The 5 Hs (hypotension, hypoxia, hypercarbia, hypoglycemia, and hyperthermia) and
seizures are conditions that should be avoided or corrected in the ED. Anticonvulsant

Chapter 83 HEAD TRAUMA 585
prophylaxis with diphenylhydantoin or levetiracetam is indicated particularly for penetrating
injuries and depressed skull fractures. It is crucial to avoid hypoxia as well because head-
injured patients who experience hypoxia (pO
2
, 60 mm Hg) also have a twofold increase in
mortality. Consequently, early and careful airway management and ventilation are essential.
Coagulopathies should be corrected with fresh frozen plasma, and platelet transfusion
should be considered in patients who have recently taken aspirin or other antiplatelet
drugs.
n
Hyperventilation. Carbon dioxide is one of the main determinants of cerebrovascular tone.
High levels produce cerebral vasodilation; low levels cause vasoconstriction.
Hyperventilation to a PCO
2
level of 25 mm Hg decreases blood flow to the brain by 50%,
which decreases the vascular compartment of the brain and may “buy some time” for
definitive surgical interventions. When blood flow to the brain decreases, delivery of oxygen
and glucose also decreases, resulting in ischemic injury and worse edema. The optimal
level of hypocarbia is uncertain at present, but most clinicians recommend moderate short-
term hyperventilation, with a PCO
2
level no less than 30 to 35 mm Hg as the goal in
patients with evidence of herniation. To accomplish this degree of hypocarbia, it is
necessary to intubate the patient with rapid-sequence intubation and mechanically ventilate
with settings determined by arterial blood gases to maintain the PCO
2
between 30 and
35 mm Hg. The indication for implementing hyperventilation is increased ICP resulting in
clinical signs of focal neurologic deficit (i.e., herniation). Hyperventilation is not used
prophylactically but is reserved for patients with elevated ICP and rapid clinical
deterioration.
n
Diuresis. The use of an osmotic diuretic, such as mannitol, 0.5 to 1.0 g/kg intravenously
over 15 minutes, or a loop diuretic, such as furosemide, 0.5 to 1.0 mg/kg intravenously,
is effective in reducing brain edema. Infusion of mannitol creates an osmotic gradient
between the intravascular space and the extracellular fluid, drawing fluid from the
extracellular fluid and reducing brain water content and ICP. Mannitol is filtered by
the kidneys, producing systemic dehydration. Clinical experience and animal studies
seem to support the concomitant administration of osmotic diuretics and volume
resuscitation in patients with hypovolemic shock.
n
Hypertonic saline. Various concentrations of hypertonic saline ranging from 3% to 23%
have been used to simultaneously decrease brain edema, maintain cerebral perfusion
pressure, and restore systemic volume. It has been shown to be at least as effective as
mannitol in treating elevated ICP. Patients receiving hypertonic saline will develop
significant hypernatremia and hyperosmolarity. Unless serum sodium exceeds 160 mEq/L,
these abnormalities should be allowed to correct themselves gradually over a period of
several days.
n
Ventriculostomy. Although generally an intensive care unit (ICU) technique, removal of CSF
through a ventriculostomy is occasionally implemented in the ED and is perhaps the most
effective way of rapidly lowering ICP.
n
Barbiturates. Conscious patients who are paralyzed for intubation also must be sedated.
A short-acting barbiturate such as thiopental is the ideal agent for this purpose because it
lowers ICP, prevents seizures, and decreases cerebral metabolism. Such agents cannot be
used in a hypotensive patient, however. In these cases, a reversible agent, such as
morphine, 0.1 mg/kg; lorazepam, 0.01 mg/kg; or midazolam, 1 mg/kg/h, is preferred
because adverse effects on blood pressure and cardiac output can be reversed by specific
antagonists. Etomidate, 0.2 mg/kg, is a short-acting agent that decreases ICP without
adversely affecting cardiac output, cerebral perfusion pressure, and systemic blood
pressure and can be used for sedation, although suppression of adrenal function is a
known complication. Fentanyl, 3 to 5 mcg/kg, causes a slight increase in ICP and is not the
preferred agent for sedation of a head-injured patient.
n
Therapeutic hypothermia. Reducing a patient’s body temperature to 32°C to 33°C for 24 to
48 hours has shown some benefit in preserving neurological function in cardiac arrest
survivors and it was hoped that it would show the same benefits in brain-injured patients.
Chapter 83 HEAD TRAUMA586
BIBLIOGRAPHY
1. Banks CJ, Furyk JS: Review article: hypertonic saline use in the emergency department. Emerg Med Aust
20:294–305, 2008.
2. Bey T, Ostick B. Second impact syndrome West J Emerg Med 10:6–10, 2009.
3. Bratton SL, Chestnut RM, Ghajar J, et al: Prophylactic hypothermia. J Neurotrauma 24:S21–S25, 2007.
4. Chestnut RM: Management of brain and spinal injuries. Crit Care Clin North Am 20:25–55, 2004.
5. Geijerstam JL, Britton M: Mild head injury: reliability of early computed tomographic findings in triage for
admission. Emerg Med J 22:103–107, 2005.
6. Heegaard W, Biros M: Traumatic brain injury. Emerg Med Clin North Am 25:655–678, 2007.
7. Marion D, Bullock MR: Current and future role of therapeutic hypothermia. J Neurotrauma 26:455–467, 2009.
8. Tyai R, Donaldson K, Loftus CM et al: Hypertonic saline: a clinical review. Neurosurg Rev 30:277–290, 2007.
However, the results of several trials have been conflicting. If any benefit occurs, it is likely
in those who present with a Glasgow Coma Scale(GCS) 5 to 8, but even in these patients
the treatment should be considered experimental. Fever should be treated aggressively,
however, and patients who arrive in the ED with mild hypothermia should be allowed to
passively rewarm.
17. If a patient has a normal CT scan after head trauma, is it completely safe to
discharge him or her home?
Nothing is completely safe. There are well-documented instances of delayed epidural and
subdural bleeding many hours after injury. Consequently, although it is generally safe to
discharge such patients, head injury instructions should be given to responsible family
members, and the patient should be instructed to return immediately if symptoms worsen.
If the patient is socially isolated or unreliable, a judgment has to be made regarding the
seriousness of the mechanism of injury and the risk of discharge. Intoxicated patients should
be kept under observation until their mental status can be evaluated properly.
18. Because CT scan is available, is there any role for plain skull films?
The usefulness of plain radiographs of the skull has been far outstripped by more informative
imaging modalities such as CT and MRI. Skull films still have certain indications in evaluation
of the following:
n
Penetrating trauma (gunshot wounds)
n
Suspected depressed skull fracture
n
Suspected basilar skull fracture
n
As part of the skeletal survey for suspected child abuse
n
In patients with prior craniotomies or shunts
1. Maintain cerebral perfusion and avoid hypotension.
2. Maintain oxygenation.
3. Secure airway using RSI if the GCS is less than 8.
4. Seizure prophylaxis with diphenylhydantoin (15 mg/kg IV).
5. Hyperventilate to pCO
2
5 30 to 35 mm Hg only if patient has elevated ICP and is clinically
herniating.
6. Osmotic therapy using either mannitol or hypertonic saline.
7. Correct coagulopathy.
KEY POINTS: TREATMENT OF HEAD INJURY
587
CHAPTER 84
TRAUMATIC OPHTHALMOLOGIC
EMERGENCIES
Harold Thomas, MD
1. Name the two most time-critical emergencies in ophthalmology.
Central retinal artery occlusion and chemical burns to the eyes.
2. What is the treatment for a chemical burn of the eye?
Immediate copious irrigation of the eyes (for at least 20 minutes). Irrigation should be initiated
before transport to the ED.
3. How do you know when you have irrigated the eye enough?
Nitrazine paper can be used to ensure that the pH has been corrected to normal. This usually
requires at least 3 L of normal saline in each eye and continuous irrigation for 20 minutes.
Alkalis, which cause the most damaging burns, tend to adhere to the tissue of the eye and are
difficult to remove completely with irrigation. After irrigation, emergent ophthalmologic
consultation is indicated.
4. What is the significance of pain from an eye injury that is not relieved with
topical anesthesia?
Complete symptomatic relief with topical anesthesia indicates a superficial injury involving
only the cornea. If a patient still has significant pain after application of anesthetic drops, a
deeper injury (often traumatic iritis) must be suspected, even in the presence of an obvious
superficial injury.
5. List nine potential injuries that must be considered in a patient sustaining a
blunt injury to the eye.
n
Blow-out fracture of the floor of the orbit
n
Corneal abrasion
n
Anterior hyphema
n
Lens dislocation
n
Traumatic mydriasis
n
Vitreous hemorrhage
n
Retinal detachment
n
Traumatic iritis
n
Ruptured globe (rare after blunt injuries)
6. What is the most common eye injury seen in the ED?
Corneal abrasion with or without a superficial foreign body.
7. How is corneal abrasion diagnosed?
The anesthetized eye can be stained with fluorescein and illuminated by an ultraviolet or Wood
lamp; corneal defects fluoresce bright yellow-orange. Visual acuity should be checked, and the
eye should be inspected, with particular emphasis on the anterior chamber to look for an
anterior hyphema.
8. What is the treatment for a corneal abrasion?
Because this injury is extremely painful, narcotic analgesics are indicated. Sending a patient
home with topical anesthesia is controversial; most recommend against it. One frequently
