Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 98 INTIMATE PARTNER VIOLENCE678
7. State some of the reasons why physicians choose not to inquire about IPV.
The most commonly cited reason is lack of time. Health care providers believe that this issue
is too time consuming to deal with, especially in a busy ED. Other reasons include the beliefs
that it is none of the physician’s business, that women would “tell” if they wanted to, that
there is nothing that can be done, that the woman deserved the abuse, and that a woman
could just leave the situation if she wanted to.
8. Why are victims of partner abuse reluctant to disclose the abuse to health
care providers, even if asked?
Men and women may be embarrassed and humiliated that it is happening to them. There may
be cultural or religious beliefs that lead a woman to believe that this is normal or to be
expected. A woman may have been told that she deserved the abuse. An abuser might have
threatened to harm a woman, her children, or other loved ones if she discloses to others; or
she may believe that no one can help her.
9. What are some of the structural and system barriers that might prevent a
victim from disclosing abuse?
Lack of privacy is a real concern in the ED. Victims should be interviewed alone, without
children or partners present. If necessary, hospital security may be recruited to ensure their
safety. Also, family members or children should not be used as translators when inquiring
about abuse. The use of computer kiosks can help to identify patients that health providers do
not personally screen for IPV as it allows patients to disclose IPV anonymously and obtain
information on community resources.
10. What clues to IPV might be evident in a patient’s history?
Most importantly, a history that is inconsistent with the physical examination findings should
raise physician suspicion for IPV. Partner abuse should also be considered in patients with
suicidal intentions or attempts, patients who are depressed, patients who have evidence of
drug and alcohol abuse, and patients with frequent visits for chronic pain or other somatic
complaints.
11. What clues may be present on physical examination in a victim of IPV?
Common injury patterns include injuries to the face, neck, and throat (especially signs or
symptoms of strangulation), chest, breasts, abdomen, and genitals. Any injury that does not
“fit” with the history obtained should create suspicion of abuse. Other physical examination
findings of concern include evidence of sexual assault or frequent, recurrent sexually
transmitted diseases.
1. Injuries to face, neck, throat, chest, abdomen (“central” pattern)
2. Injuries to chest and abdomen
3. Any injury that does not “fit” with the history
4. Evidence of sexual assault or frequent, recurrent sexually transmitted diseases
5. Injuries in multiple stages of healing
KEY POINTS: PHYSICAL EXAMINATION FINDINGS IN IPV
12. How can I increase my recognition of partner abuse?
First, ask about IPV. Any woman who presents with an injury should be specifically asked who
injured her. Second, raise your level of suspicion in women without injuries. Remember the
clues that might be present in the history or physical examination. If you are considering
partner abuse, ask about it.

Chapter 98 INTIMATE PARTNER VIOLENCE 679
13. What questions about partner violence can I ask a woman without injuries?
a. Have you ever been hurt or injured by a partner or ex-partner?
b. Are there situations in your relationship where you have felt afraid?
c. Has your partner ever abused you or your children?
d. Do you feel safe in your current relationship?
e. Is there a partner from a past relationship who is making you feel unsafe now?
14. What about screening all women for IPV?
Good idea! Because of the prevalence of this problem, many organizations have advocated
screening all women for the presence of IPV. One screening tool that has been tested clinically
is the Partner Violence Screen. This consists of these three questions:
n
Have you been hurt or injured in the past year by anyone? If so, by whom?
n
Do you feel safe in your current relationship?
n
Is there a partner from a previous relationship who is making you feel unsafe now?
This tool is 71% sensitive for detecting IPV. Women who screen positive for IPV are 11 times
more likely to experience physical violence in the next 4 months than women who screen
negative for IPV.
15. What comments or questions would be inappropriate when discussing IPV
with women?
n
“What did you do to him?”
n
“What did you do that made him so mad?”
n
“This has happened before, and you are still married to him?”
n
“Why didn’t you tell anyone?”
n
“You let him do that to you?”
n
“I wouldn’t let anyone do that to me.”
n
“Why don’t you just leave?”
16. What do I do if my patient has an injury caused by her partner?
n
Treat her injuries.
n
Document her history and her injuries carefully in the medical records.
n
Provide support and empathy; women should be informed that IPV is a common problem,
that no one deserves this abuse, and that help is available. Helping victims access
community resources should be a primary goal of ED treatment.
n
Inquire about the woman’s safety and that of her children. Not all women want or require
shelter placement. Women who are experiencing increasingly severe physical injuries or
whose batterers have access to firearms are at risk for severe or lethal injuries. Some of
these interventions may be by a social worker or by a domestic violence advocate,
depending on the clinical setting.
17. Summarize some important points to remember when documenting IPV.
Document what happened in the patient’s own words, and document the relationship to the
batterer. Record all areas of bruising or tenderness; a body map may be helpful. Photographs
may be used, but care should be taken to follow local legal guidelines for photographing
injuries. Be sure to obtain the patient’s permission. Any treatment and intervention should be
documented. In cases in which abuse is highly suspected and the patient is denying abuse,
document the reason that you suspect abuse (e.g., the history does not match the physical
examination findings). A well-documented medical record can mean the difference between
convicting an abuser and allowing him to go free.
18. Don’t I have any legal responsibilities?
You might. As of March 2001, 45 states had a law that mandates reporting intentionally
inflicted injuries; however, these laws vary greatly as to what injuries must be reported
(Table 98-1). Each emergency physician must be familiar with the current reporting
requirement in his or her state.
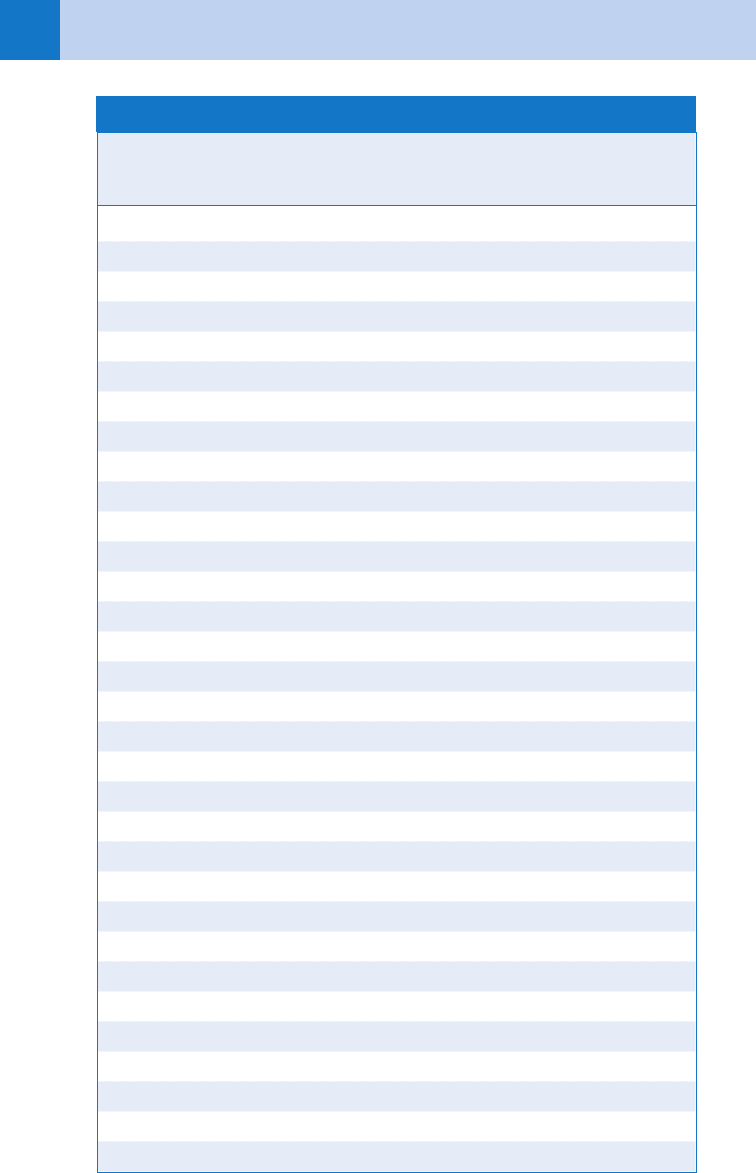
Chapter 98 INTIMATE PARTNER VIOLENCE680
State (Statute)
Injuries
from
Weapons
Injuries
from
Crimes
Injuries from
Domestic
Violence
Alabama No No No
Alaska (Statute 08.64.369) Yes Yes No
Arizona (Rev Stat 13-3806) Yes Yes No
Arkansas (Code Ann 12-12-602) Yes No No
California (Pen Code 11172 AB74 3 19) Yes Yes Yes
Colorado (Rev Stat 12-36-135) Yes Yes Yes
Connecticut (Acts 269) Yes No No
Delaware (Code Ann 24-17-1762) Yes No No
District of Columbia (Ann 2-1361) Yes No No
Florida (Stat Ann 790.24) Yes Yes No
Georgia (Code Ann 31-7-9) No Yes No
Hawaii (Rev Stat 453-14) Yes Yes No
Idaho (Code 39-1390) Yes Yes No
Illinois (Code Ann 20-2630-3) Yes Yes No
Indiana (Code Ann 35-47-1) Yes No No
Iowa (Code Ann 147.111) Yes Yes No
Kansas (Stat 21-4213) Yes No No
Kentucky (Stat Ann 209.020) No Yes Yes
Louisiana (Rev Stat 403.5) Yes No No
Maine (Rev Stat 17A Ch 21.512) Yes No No
Maryland (Ann Code 336, art 27) Yes No No
Massachusetts (Gen Laws 112-12) Yes No No
Michigan (Comp Laws 750.411) Yes Yes No
Minnesota (Stat Ann 626.52) Yes No No
Mississippi (Code Ann 45-9-31; 93-21-1) Yes No Yes
Missouri (Rev Stat 578-350.1) Yes Yes No
Montana (Code Ann 37-2-302) Yes No No
Nebraska (Rev Stat 28-902) No Yes No
Nevada (Rev Stat Ann 629.041) Yes No No
New Hampshire (Rev Stat Ann 631.6) Yes Yes No
New Jersey (Stat Ann 2C: 58-8) Yes No No
New Mexico No No No
TABLE 98–1. LEGAL REQUIREMENT FOR REPORTING INJURIES BY STATE
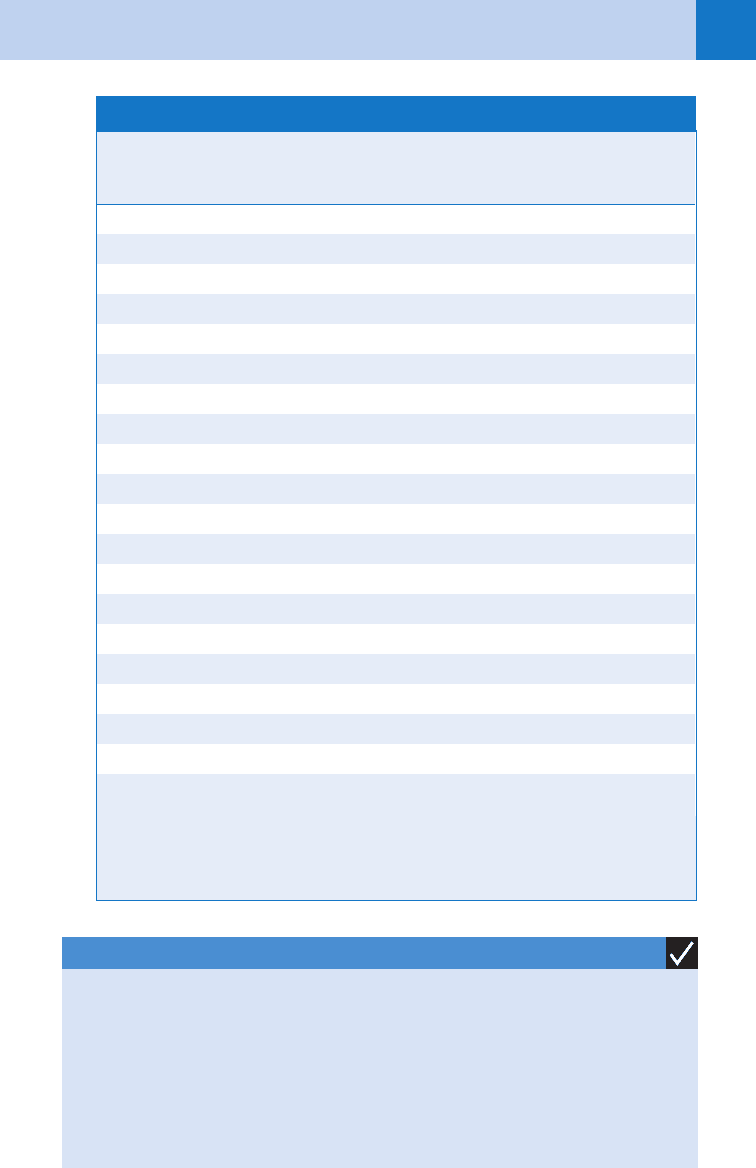
Chapter 98 INTIMATE PARTNER VIOLENCE 681
*Verified as of March 2001.
From Houry D, Sachs CJ, Feldhaus KM, et al: Violence-inflicted injuries: reporting laws in the fifty states.
Ann Emerg Med 39:56–60, 2002.
State (Statute)
Injuries
from
Weapons
Injuries
from
Crimes
Injuries from
Domestic
Violence
New York (Penal Code 265.25) Yes No No
North Carolina (Gen Stat 90-21.20) Yes Yes No
North Dakota (Cent Code 43-17-41) Yes Yes No
Ohio (ORC 2921; 2151) Yes Yes Yes
Oklahoma (Stat 2105-846.1) No Yes No
Oregon (Rev Stat 146.750) Yes No No
Pennsylvania (Cons Stat Anns 18-5106) Yes Yes No
Rhode Island (Gen Laws 12-29-9; 11-47-48) Yes No Yes
South Carolina No No No
South Dakota (Codified Laws 23-13-10) Yes No No
Tennessee (Stat 36-3-621; 38-1-101) Yes Yes Voluntary
Texas (Fam Code 91.003,161.041) Yes No Yes
Utah (Code Ann 26-23a) Yes Yes No
Vermont (Stat Ann 13-4012) Yes No No
Virginia (Code Ann 54.1-2967) Yes No No
Washington No No No
West Virginia (Code Ann 61-2-27) Yes No No
Wisconsin (Stat Ann 146.995) Yes Yes No
Wyoming No No No
Total (including DC) “yes” 42 23 7
1. Treat the injuries.
2. Document the history and injuries carefully. (Consider drawing a picture or taking a photo.)
3. Provide support and empathy.
4. Inquire about the woman’s safety and that of her children.
5. Refer to community resources or social worker.
6. Notify law enforcement if required by your state.
KEY POINTS: WHAT TO DO WITH AN IPV VICTIM
TABLE 98–1. LEGAL REQUIREMENT FOR REPORTING INJURIES BY STATE—cont’d
Chapter 98 INTIMATE PARTNER VIOLENCE682
19. Why is she going home to her batterer? Why doesn’t she just leave him?
Why a woman does not leave her batterer is the wrong question to ask. It implies that the
woman is to blame and that if she would just leave everything would be okay. Battered women
are most likely to be killed during the act of leaving or after they have left their abuser. There
are many other valid reasons why women stay in an abusive situation. She may:
n
Have no money or job skills
n
Have nowhere else to go
n
Feel she must stay to protect her children
20. What can we do about IPV?
A more appropriate response to IPV is to ask ourselves why society tolerates this behavior
and how we, as health care providers, might change those attitudes.
ACKNOWLEDGMENT
Kim M. Feldhaus, MD, was an author on previous editions and developed the initial version.
BIBLIOGRAPHY
1. Feldhaus KM, Koziol-McLain J, Amsbury HL, et al: Accuracy of 3 brief screening questions for detecting
partner violence in the emergency department. JAMA 277:1357–1361, 1997.
2. Houry D, Kaslow NJ, Kemball RS, et al: Does screening in the emergency department hurt or help victims of
intimate partner violence? Ann Emerg Med 51:433-42, 2008.
3. Houry D, Rhodes KV, Kemball RS, et al: Differences in female and male victims and perpetrators of partner
violence with respect to WEB scores. J Interpers Violence 23:1041–1055, 2008.
4. Houry D, Feldhaus K, Peery B, et al: A positive domestic violence screen predicts future domestic violence.
J Interpers Violence 19:955–966, 2004.
5. Houry D, Parramore C, Fayard G, et al: Characteristics of household addresses that repeatedly contact 911 to
report intimate partner violence. Acad Emerg Med 11:662–667, 2004.
6. Houry D, Sachs CJ, Feldhaus KM, et al: Violence-inflicted injuries: reporting laws in the fifty states. Ann Emerg
Med 39:56–60, 2002.
7. Muelleman RL, Lenaghan PA, Pakieser RA: Battered women: injury locations and types. Ann Emerg Med
28:486–492, 1996.
8. Walton-Moss BJ, Manganello J, Frye V, et al: Risk factors for intimate partner violence and associated injury
among urban women. J Community Health 30:377–389, 2005.
683
CHAPTER 99
COST CONTAINMENT AND RISK
MANAGEMENT IN EMERGENCY MEDICINE
Stephen V. Cantrill, MD
XVIII. EMERGENCY MEDICINE ADMINISTRATION AND RISK MANAGEMENT
COST CONTAINMENT
1. What is cost containment in emergency medicine?
An approach to limit medical care expenses without compromising quality of care.
2. Why is cost containment so important?
Medical care currently consumes more than 16% of the U.S. gross domestic product (GDP),
and health care costs traditionally have increased at a rate far above inflation. Because the
federal government directly or indirectly pays for at least 42% of health care, they are quite
concerned about this ongoing increase. This has led to active involvement by the National
Quality Forum and the Center for Medicare and Medicaid Services in dealing with what is felt
to be excessive patient diagnostic testing. One study concluded that one third of medical
care may be unnecessary. The proliferation of health-maintenance organizations (HMOs)
and capitated-care contracts has also placed additional pressure on physicians to curtail
unnecessary health care costs, often with the health care provider sharing in the financial risk
of providing patient care. In addition, many practice environments are developing physician
practice profiling systems to identify practitioners who order excessive numbers of tests and
procedures.
3. In what area do emergency physicians have the most control in terms of
containing costs?
Ancillary tests (clinical laboratory and radiology) constitute 44% of patient ED charges—the
largest component. These tests are done at the request of the emergency physician and
represent an area directly under our control.
4. List some reasons for excessive test ordering in emergency medicine.
n
Peer pressure (e.g., wanting to please a consultant)
n
Out-of-date hospital policies
n
Intellectual curiosity
n
Ignorance of the costs of tests
n
Patient expectations (and demands)
n
Defensive medicine
n
Reflex ordering or old habits
None of these reasons is adequate justification for ordering tests that are not medically
indicated based on the patient’s presentation.
5. Can just knowing the cost of the tests have an effect?
Yes. This has been demonstrated by several studies, including one in which just having the
patient charges for tests on the order slip reduced overall patient test charges by 27%.
6. What is the golden question to ask before ordering any test?
The question is “How useful will this test be in establishing a diagnosis, assisting in treatment,
or making the appropriate disposition?” If the answer is it won’t, serious thought should be
given regarding the necessity of ordering the study.
Chapter 99 COST CONTAINMENT AND RISK MANAGEMENT IN EMERGENCY MEDICINE684
7. List some additional strategies to reduce inappropriate test ordering.
n
Avoid ordering reflexively. Carefully consider the benefits before ordering a test.
n
Do not order a test because it would be nice to know, unless you are willing to pay for the
test yourself.
n
Learn how much routine laboratory tests and radiographs cost. Prepare yourself for a
shock.
n
Establish guidelines for the use of new technologies. Medicine is notorious for developing
and using new tests without discontinuing tests that are old or outdated.
n
Avoid ordering studies for medicolegal reasons. Good medicine is good law. Order only
studies that are medically indicated.
n
Use patient education to reshape patient expectations when possible.
n
Cancel studies that were ordered but later found to be unnecessary.
8. Shouldn’t we order tests to cover ourselves?
No. Again, good medicine is good law. The criteria for ordering studies should be strictly
medical, not based on the physician’s notion of what would be helpful to have in a court of
law. Laboratory or radiographic studies should not be used as a substitute for a proper
history, physical examination, and good documentation.
9. Name some commonly over-ordered tests.
n
Extremity radiographs
n
Urine culture and sensitivity
n
Chest radiographs
n
Throat culture (excluding streptococcal screen)
n
Abdominal radiographs
n
Blood type and cross-match
n
Rib radiographs
n
Blood ethanol level
n
Electrolyte panel
n
Arterial blood gases
n
Complete blood count
n
Toxicology screens
10. How much can be saved with no compromise in patient care?
In a multicenter study of 20 hospital EDs, both teaching and nonteaching, a cost-containment
educational program was used. Seventeen tests or groups of tests or studies (including those
listed previously) were targeted. A 12.5% decrease in targeted test charges was shown. No
decrease in the perceived quality of care could be shown. Careful implementation of clinical
decision rules, such as the Ottawa ankle rule, can save up to 35% in ordering X-rays, with no
decrease in sensitivity. Implementation of specific cost-effective guidelines has been shown to
decrease the hospital ED charge by 28%, with the laboratory charge decreased by 46%. This
clearly demonstrates that the costs of medical testing in the ED can be contained by careful,
thoughtful ordering without compromising patient care.
11. Can good medication-prescribing habits impact the cost of patient care?
Without question! Common, costly, unnecessary practices in prescribing practices include
prescribing:
n
Antibiotics when no true medical indication exists (e.g., for a viral upper respiratory tract
infections [URI]).
n
The latest and greatest antibiotic that gives unnecessarily broad coverage.
n
By brand name when a generic has demonstrated adequate bioequivalence.
Avoiding these practices will not only help control costs but will also improve the quality of
your care.
Chapter 99 COST CONTAINMENT AND RISK MANAGEMENT IN EMERGENCY MEDICINE 685
12. How is the Center for Medicare and Medicaid Services (CMS) concerned about
appropriateness of testing?
CMS requires that documentation be supplied to support that the diagnostic testing ordered
was reasonable and medically necessary. Often, routine screening tests are disallowed, even
if the ordering physician thought them to be appropriate. Retrospective audits have been
performed, with some institutions having to return tens of millions of dollars to the federal
government for not being able to demonstrate the medical necessity of many diagnostic
studies.
13. Is the National Quality Forum (NQF) concerned about appropriate resource
use in medicine?
Yes. The National Quality Forum is a nonprofit organization that is involved in the development
and endorsement of national consensus standards for measuring and reporting medical
performance. As such, the NQF is currently involved in medical performance measurements
relating to resource use:
n
Imaging efficiency standards regarding the appropriate and effective use of imaging in a
clinical setting
n
Evaluation of episode-based and per capita resource use measures of 18 specific diseases
and conditions (many of which involve emergency medicine).
1. Only diagnostic studies that directly impact the diagnosis or treatment of the patient’s
presenting problem should be ordered in the ED.
2. CMS will not reimburse a hospital for diagnostic testing if the documentation does not
support that the tests were reasonable and necessary.
KEY POINTS: COST CONTAINMENT
RISK MANAGEMENT
14. What is risk management?
Efforts to identify (and, when possible, improve or rectify) situations that place a service
provider in jeopardy. Good risk management not only deals with situations as they arise (e.g.,
dealing appropriately with a patient’s complaint about care) but also anticipates health-delivery
problems before they occur (e.g., establishing in advance the procedures for dealing with a
patient who wishes to leave against medical advice).
15. Why are emergency physicians at high risk for malpractice lawsuits?
The primary reason is the lack of an established physician-patient relationship. The patient
often feels little rapport with a physician unknown to the patient before the visit to the ED. The
visit is usually not at the patient’s wish, occurring at an unscheduled time and in a situation in
which the patient is under stress and sometimes pain. All of these factors may contribute to
feelings of anger and hostility, laying the groundwork for feelings of dissatisfaction about the
provided care. A second major reason is that in emergency medicine, the decisions are often
irrevocable. If a mistake or misjudgment is made on a patient who is admitted to the hospital,
a second chance to correct the error usually exists because the patient is still accessible. In
patients wrongly discharged from the ED, sometimes no such second chance exists.
16. What must be proved in a malpractice case?
n
Duty to treat. Was there an obligation for the physician in question to treat the patient? In
emergency medicine, this answer is almost always yes. By working in an ED, an emergency
Chapter 99 COST CONTAINMENT AND RISK MANAGEMENT IN EMERGENCY MEDICINE686
physician automatically assumes the duty to treat any patient presenting to the ED and
requesting care. The EMTALA statute mandates a medical screening examination on all
patients presenting to the ED. (See Chapter 100.)
n
Actual negligence. Was the care provided actually negligent? This often involves showing
(to the jury’s satisfaction) that the care provided fell below what is to be considered the
standard of care. This point is the one most often contested by the opposing sides in a
malpractice suit. Negligence may result from acts of commission or omission.
n
Damages. Did the patient suffer actual damages? This can include the nebulous pain and
suffering.
n
Proximate cause. Did the negligence cause the damages? It must be shown to the jury’s
satisfaction that the alleged damages were truly the result of the alleged negligent care.
17. Give some examples of high-risk patients.
n
The hostile or belligerent patient. These patients are difficult to deal with and sometimes get
less than complete, careful evaluation. Intoxicated patients represent a significant subgroup
of this class of patients. Demanding patients also fall into this class. When confronted with
patients in this category, remember that you don’t have to love them to give them proper care.
n
The patient with a problem that may be a potential life threat. With these patients, the
challenge is to discover and address the life threat (see Chapter 1). Inappropriately
discharging these patients often results in a risk-management issue.
n
The returning patient. The patient who returns unscheduled to the ED should raise a red
flag. What problem is being missed? These patients deserve extra care in reevaluation.
The threshold for admitting an unscheduled returning patient should be low.
n
The private patient. Patients may be sent to the ED by a private physician for diagnostic
studies or treatment but not to be seen and evaluated by the emergency physician. In
general, any patient in the ED becomes the responsibility of the emergency physician. If
something goes wrong with the care of these patients, the emergency physician also may
be held liable. It is advisable to have very clear established policies concerning private
patients in the ED. These patients should be seen by the emergency physician on duty if the
patient so requests, if there is a delay in the arrival of the private physician, or if their triage
category so warrants.
1. Treat every patient as you would want your mother treated.
2. If possible, avoid writing admission orders.
3. Always address the potential life threats, based on the patient’s presentation.
KEY POINTS: RISK MANAGEMENT
18. What clinical problems tend to get emergency physicians into malpractice
difficulty?
There is regional variation in clinical problems that tend to cause malpractice problems for
emergency physicians, but the following entities are generally major causes:
n
Acute coronary syndromes
n
Meningitis/sepsis (especially in young children)
n
Missed fractures (including spine and pelvis)
n
Appendicitis
n
Stroke management
n
Retained foreign bodies
n
Aortic aneurysms
n
Tendon/nerve injuries associated with wounds

Chapter 99 COST CONTAINMENT AND RISK MANAGEMENT IN EMERGENCY MEDICINE 687
n
Intracranial hemorrhage (subdural, epidural, and subarachnoid hemorrhages)
n
Wound infections
19. What is the most common error emergency physicians make with regard to
their malpractice insurance policy?
Failure to read carefully and understand the conditions of the policy (i.e., what is covered,
what is not covered, what is required for a malpractice occurrence to be covered, what are the
settlement options, and what are the “tail” requirements to provide coverage for past patient
encounters when the current policy is no longer in force).
20. What common deficiencies in the medical record exacerbate malpractice
problems for emergency physicians?
In a malpractice case, your record of a patient’s visit can be your greatest friend or your worst
foe. The following problems will place the record on the side of the opposing team:
n
An illegible record. Think about how the record will look when it is enlarged to 4 feet by
4 feet by the plaintiff’s attorney to show to the jury. Electronic, dictated, or typed records
avoid this problem.
n
Not addressing the chief complaint or nurses’ and paramedics’ notes. Make sure your
evaluation addresses why the patient came to the ED and what others observed and
documented about the patient.
n
Not addressing abnormal vital signs. As a rule, patients must not be discharged from the
ED with abnormal vital signs. Whenever this is done, the record must contain a discussion
of why the physician is taking this action.
n
An incomplete recorded history. As with all other parts of the medical record, an attempt
will be made to convince the jury that not recorded equals not done. The history must
include information concerning all potential serious problems consistent with the patient’s
presentation. Significant negatives should be recorded as well.
n
Labeling the patient with a diagnosis that cannot be substantiated by the rest of the record.
This not only may cause difficulty if the physician’s guess is wrong but also leads to
premature closure on the part of the next physician to treat the patient, removing the slim
chance of correcting the diagnostic error if the patient returns to the ED because of no
improvement.
n
Inadequate documentation of the patient’s course in the ED with inadequate attention to the
patient’s condition at discharge. Often the patient’s condition may improve dramatically
while in the ED, justifying discharge, but this fact is not reflected in the record. If this case
becomes a malpractice problem, it appears that the patient was discharged in the original
(unimproved) condition.
n
Inadequate discharge (follow-up, aftercare) instructions. The greatest risk in dealing with
patients is being wrong in our judgment. The best insurance is careful and complete patient
discharge instructions that include when and where to follow up and under what conditions to
return to the ED. It is striking how little effort is put into this component of the record. After
completing your evaluation and treatment of a patient, ask yourself, “What if I am wrong,
and what is the worst possible complication that can occur?” Address these possibilities
completely in your discharge instructions, and document them carefully in the record.
21. What systems problems often lead to lawsuits?
n
Systems problems are not under the emergency physician’s control, but can still cause
difficulty. Such problems include:
n
Inadequate follow-up on radiology rereads of radiographs
n
Inadequate follow-up of cardiology rereads of electrocardiograms (ECGs)
n
Inadequate follow-up of delayed clinical laboratory results (e.g., cultures)
n
Poor availability of previous medical records
n
Inadequate handling of patient complaints (your chance possibly to head off a malpractice suit)
n
Inadequate physician and ED staffing patterns (leading to prolonged patient waits and
subsequent patient hostility
