Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 96 DEPRESSION AND SUICIDE668668
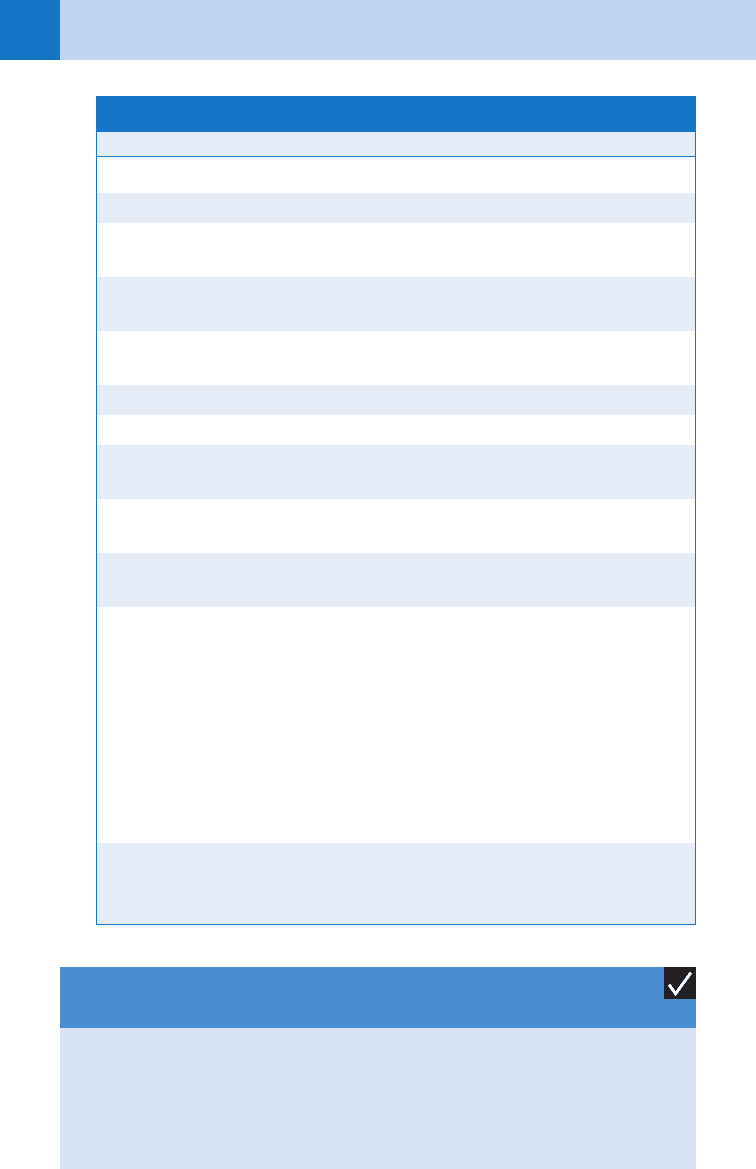
Adapted from Hockberger RS, Rothstein RJ: Assessment of suicide potential by non-psychiatrists using
the SAD PERSONS score. J Emerg Med 99:6, 1988. In Hockberger RS, Smith M: Depression and sui-
cide ideation In Wolfson A.B (ed): Clinical practice of emergency medicine, ed 4, Philadelphia, 2005,
Lippincott Williams & Wilkins, pp 637–639.
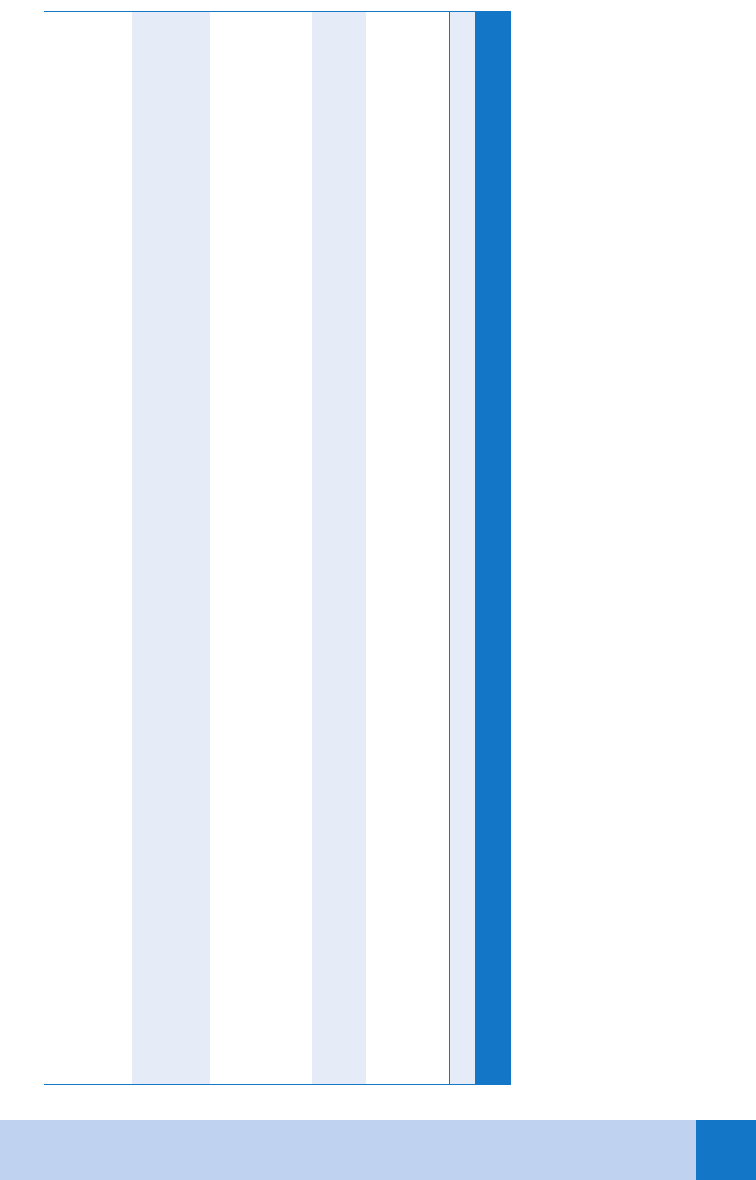
Mnemonic Characteristic Score
S Sex Male 1
A Age ,19 or .45 years 1
D Depression or hopelessness Admits to depression or decreased
concentration, appetite, sleep, libido
2
P Previous attempts or psychiatric
care
Previous inpatient or outpatient
psychiatric care
1
E Excessive alcohol or drug use Stigmata of chronic addiction or
recent frequent use
1
R Rational thinking loss Organic brain syndrome or psychosis 2
S Separated, widowed, or divorced 1
O Organized or serious attempt Well-thought-out plan or life-threatening
presentation
2
N No social supports No close family, friends, job, or active
religious affiliation
1
S Stated future intent Determined to repeat attempt or
ambivalent
2
Scoring: A positive answer to the presence of depression or hopelessness, lack of rational
thought processes, an organized plan or serious suicide attempt, and affirmative or ambivalent
statement regarding future intent to commit suicide are each scored 2 points. Each other
positive answer is scored 1 point.
Score
,6
6–8
.8
Risk
Low
Intermediate
High
TABLE 96–1. MODIFIED SAD PERSONS SCALE
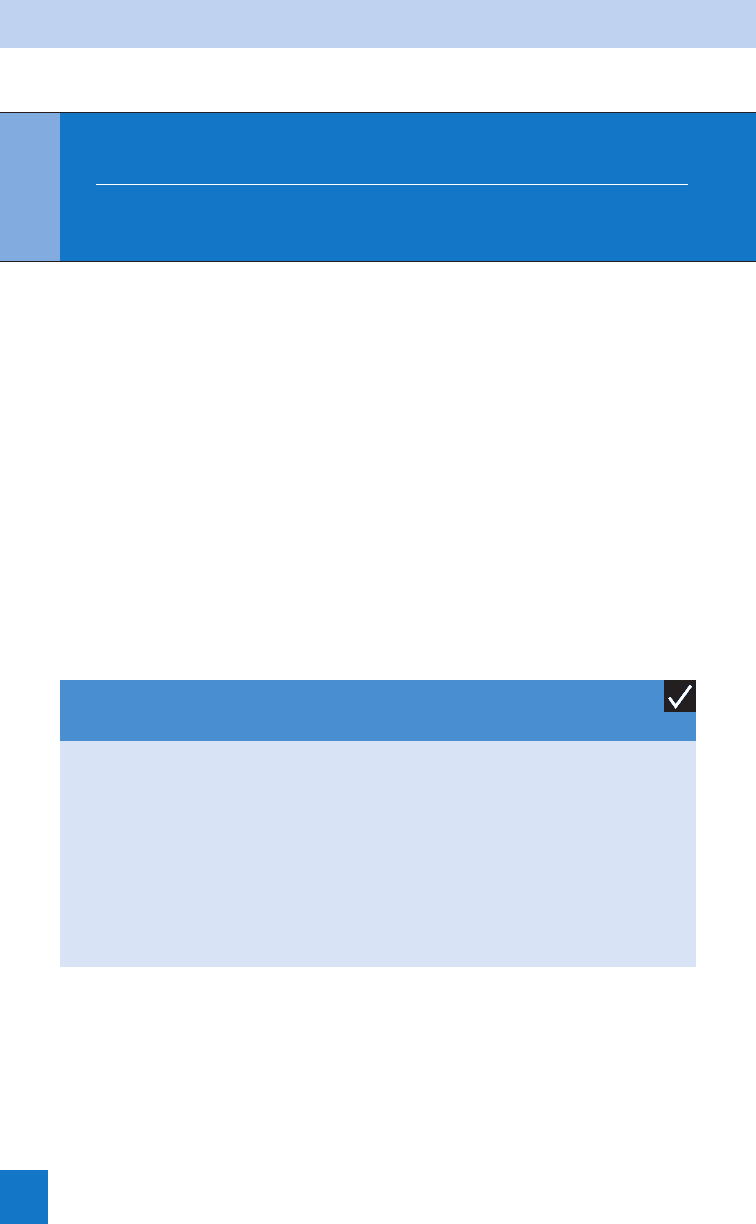
1. Violent, near-lethal, preplanned attempt
2. Psychotic patient
3. Elderly patient
4. Expression of continued wish to die by suicide
KEY POINTS: POINTS: INDICATIONS FOR SUICIDE
PRECAUTIONS AND PSYCHIATRIC CONSULTATION

Chapter 96 DEPRESSION AND SUICIDE 669
BIBLIOGRAPHY
1. Chiles, JA, Strosahl KD: Clinical manual for assessment and treatment of suicidal patients. Washington DC,
2005, American Psychiatric Publishing, Inc.
2. Colucciello SA, Hockberger RS: Suicide. In Marx JA, Hockberger RS, Walls RM, editors: Emergency medicine:
concepts and clinical practice, ed 5, St. Louis, 2002, Mosby.
3. Kishi Y, Robinson RG, Kosier JT: Suicidal ideation among patients with acute life threatening physical illness in
patients with stroke, traumatic brain injury, myocardial infarction and spinal cord injury. Psychosomatics
42:382–390, 2001.
4. Olfson M, Marcus SC, Druss B, et al: National trends in the outpatient treatment of depression. JAMA 287:
203–209, 2002.
5. Placidi GP, Oquendo MA, Malone KM, et al: Anxiety in major depression, relationship to suicide attempts. Am J
Psychiatry 157:1614–1618, 2000.
6. Simon RI: Assessing and managing suicide risk: guidelines for clinically based risk management. Washington
DC, 2004, American Psychiatric Publishing, Inc.
7. Stahl SM: Essential psychopharmacology: the prescribers guide. Cambridge, 2005, Cambridge University Press.
8. Zametkin AJ, Alter MR,Yemini T: Suicide in teenagers: Assessment, management and prevention. JAMA
286:3120–3125, 2001.
National Mental Health Association: www.nmha.org
WEBSITE
670
CHAPTER 97
MANAGEMENT OF THE VIOLENT PATIENT
Douglas Ikelheimer, MD, MA
1. Is violence a problem in the emergency department (ED)?
Yes. Only a small percentage of ED patients are violent, disruptive, or abusive to staff yet they
require disproportionate staff attention and resources. About 4% of patients in the ED need
restraints during their stay. According to a prospective observational study from an urban ED,
29.2% of restraint episodes were for violent and disruptive behavior, 25.2% for agitation, and
7.4% for alcohol or drug intoxication. Restraints were less frequently used for confusion
(6.4%) or dementia (1.7%), but note that 40% of the patients who were restrained had
multiple reasons for restraints. Approximately 30% of agitated patients require a combination
of physical and chemical restraint.
2. Why did the patient become violent in the first place?
Common causes of violence and agitation include acute intoxication, acute withdrawal and
associated delirium, metabolic disorders, trauma, infectious disease, sepsis, cardiovascular
disorders, psychiatric disorders, hypoxia, or intracranial processes such as stroke or
hemorrhage. Note that the rate of violence is the same between patients with mental illness
and those without mental illness. Better predictors of violence include recent history of
violence and the presence of personality disorder or substance abuse.
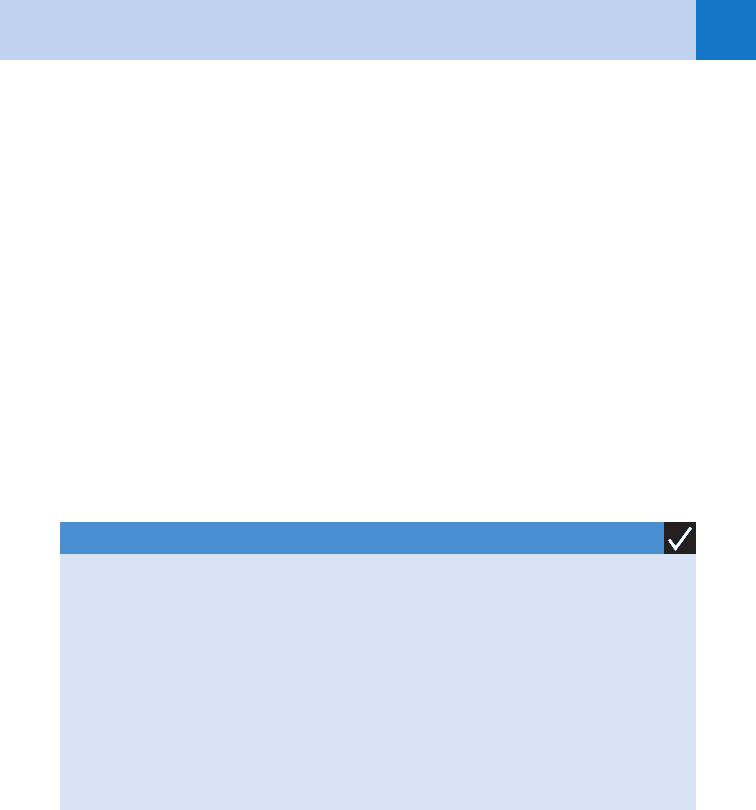
1. Hypoxia
2. Hypoglycemia
3. Acute intoxication or withdrawal syndromes
4. Meningoencephalitis
5. Intracranial injury or bleed
6. Hyponatremia or hypernatremia
7. Drug side effects
KEY POINTS: COMMON MEDICAL CONDITIONS THAT
MANIFEST AS VIOLENT BEHAVIOR
3. What can hospitals do to decrease the risk of violence?
n
Limit hospital access to only a few entrances staffed and monitored by trained security
personnel.
n
Metal detectors should be used to screen patients and visitors for weapons.
n
Continuous surveillance or closed-circuit television monitors should be used to help ensure
safety in the parking areas and the immediate grounds of the hospital.
n
Multiple methods of summoning police or security must be available to the ED without
having to go through the hospital operator.
Chapter 97 MANAGEMENT OF THE VIOLENT PATIENT 671
4. What can be done to preempt a violent episode?
n
Be aware of early signs of impending violent behavior, such as agitation, intoxication,
delirium, abusive language, and challenges to authority.
n
Completely undress all patients and place in a gown; remove from reach any items that
may be used as a weapon.
5. What is the initial approach a physician can take to control an agitated or
violent patient?
The first approach should be verbal redirection. The physician should appear calm and in
control but empathetic while explaining to the patient that he or she is in a safe environment
and that the ED staff is there to help. Active listening may go a long way toward calming the
patient. Keep hands in a neutral position, not crossed across your chest or behind your back.
Make an attempt to make the patient more comfortable by offering a drink or a warm blanket.
Be clear that violence will not be tolerated and that ED staff must maintain a safe environment
for treating patients. Security officers in the patient’s presence may dissuade further
inappropriate behavior. It may be beneficial to offer nicotine replacement such as gum or a
patch or other voluntary meds for agitation including oral haloperidol, lorazepam, olanzapine,
or ziprasidone (see section on medications). Care providers must be aware of their own
emotions when dealing with agitated patients; yelling or exchanging threats with the patient
only further escalates the situation.
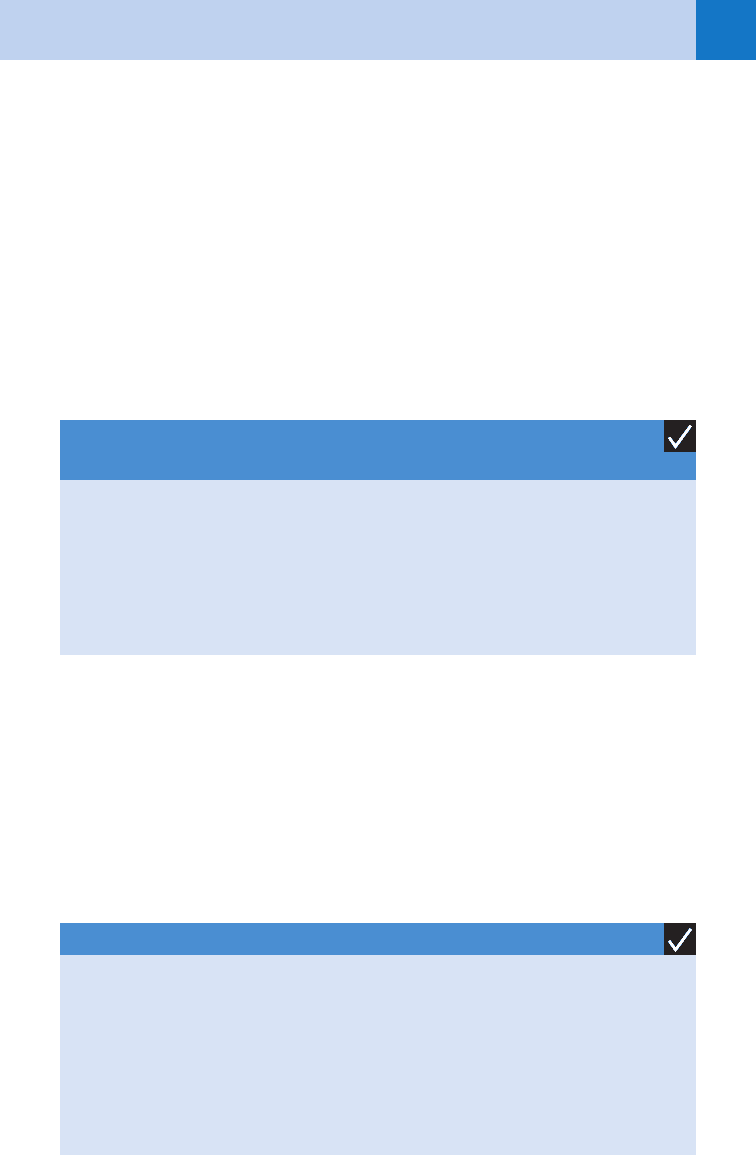
KEY POINTS: DE-ESCALATING A VIOLENT PATIENT
1. Use verbal redirection.
2. Use nonconfrontational body language.
3. Reassure the patient’s safety.
4. Use empathy.
5. Maintain and emphasize control over the ED.
6. Be honest and direct.
7. Offer nicotine replacement, food, water, or blanket.
8. Offer voluntary meds for agitation.
6. What if that doesn’t work?
When aggressive behavior cannot be managed by verbal de-escalation and a patient becomes
an increasing risk of violence or elopement, physical or chemical restraint may be indicated.
Physical restraint usually involves four-point locking leather cuffs (both wrists and both
ankles). A team of five staff members should place the restraints—one care provider for each
limb and one at the head of the patient to provide an ongoing explanation to the patient of
what is happening and why. The physician should not be involved in this action because it
may further jeopardize his or her therapeutic relationship with the patient. Soft restraints or
two-point restraints may be best for the disoriented patient at risk of pulling lines and tubes.
When the patient becomes calm, he or she is often brought down to two-point restraints or
released from restraints completely.
7. What do I need to remember when physically restraining a patient?
Restraints must be snug enough to control the patient but not impede circulation. There
should be enough room to allow one finger to move easily between the patient’s skin and the
cuff. Ensure that side rails are up. Due to risk of suffocation, never restrain a patient in the

Chapter 97 MANAGEMENT OF THE VIOLENT PATIENT672
prone position and any patient at risk of aspiration should be positioned on his or her side.
Patients in restraints must be monitored directly and continuously. As the agitation resolves,
restraining measures can be downgraded or discontinued. Documentation is required
regarding the patient’s behavior and mental status, attempts at less restrictive measures, and
monitoring of vital signs. The Joint Commission has specific guidelines for use of physical
restraints. There are additional hospital protocols regarding restraints, and the physician
should be familiar with all of these guidelines.
8. Am I legally allowed to restrain someone?
Yes. Chemical or physical restraint is indicated when patients become imminently dangerous
and less restrictive measures have failed. The courts have held both physicians and hospitals
liable for injuries that have occurred when violent or otherwise incapacitated patients escaped
hospital grounds or are discharged. The ED staff must therefore prevent certain patients from
leaving until they can be examined and thoroughly evaluated. If the patient elopes, avoid
personal heroics and instead call the local authorities. Regarding a patient’s right to refuse
medications, this does not apply to patients who exhibit violent or acutely psychotic behavior
in the ED. Courts have routinely held that physicians may involuntarily administer medications
to patients who would otherwise present an imminent risk of dangerous behavior.
9. What medications are recommended for chemical restraint?
Three primary classes of drugs are used for chemical restraint: (1) benzodiazepines, such
as lorazepam and diazepam; (2) traditional antipsychotics such as haloperidol and
chlorpromazine; and (3) atypical antipsychotics such as olanzapine, risperidone, and
ziprasidone.
Benzodiazepines: These are useful in agitation, mania, psychosis, alcohol withdrawal,
benzodiazepine withdrawal, and sympathomimetic toxidromes like cocaine or amphetamine
toxicity. Doses of 1 to 2 mg intramuscularly (IM) or intravenously (IV) of lorazepam may be
given every hour as needed. Diazepam may be given as follows: 5 to 10 mg PO, IV, IM, or per
rectum (PR) every hour as needed. Another choice is midazolam alone or in combination with
haloperidol. Midazolam, 5 mg IM, has been shown to have a more rapid onset than lorazepam
or haloperidol and also has the benefit of having a shorter time to arousal.
Traditional Antipsychotics: Although the antipsychotic effects of these medications may
take days to achieve, their usefulness in the acute setting with any patient (with or without
psychosis) is due to their sedating properties. Haloperidol in doses of 5 to 10 mg per os (by
mouth; PO), IM, or IV can be an effective medication for controlling agitation due to
psychosis, delirium, or intoxication. These doses may be repeated every hour until the patient
is calm; maximum recommended daily dose of haloperidol is 30 mg. Chlorpromazine at a
dose of 100 mg PO or 50 mg IM may be given hourly as needed. In 2001, the Food and Drug
Administration (FDA) issued a black box warning for droperidol, citing a risk of QTc
prolongation and torsades de pointes. However, the evidence for this is in dispute and many
practitioners believe that the risks associated with use of droperidol are outweighed by the
beneficial effects, particularly when routine electrocardiogram (ECG) screening is employed.
Whenever using a traditional antipsychotic such as haloperidol, it is advisable to provide
protection from possible extrapyramidal symptoms (EPS) by coadministration of an
anticholinergic agent such as diphenhydramine at a dose of 50 mg PO, IM, or IV, or
benztropine at a dose of 1 mg PO, IM, or IV.
Atypical Antipsychotics: Although the atypicals can be more expensive, they are effective at
controlling agitation without overly sedating the patient, thus offering potential benefits with
regard to more expedient disposition of the patient. Risperidone 2 to 4 mg PO or olanzapine
10 to 20 mg PO or 10 mg IM can be effective in controlling agitation. Ziprasidone 80 to 120 mg
PO or 10 to 20 mg IM (with or without lorazepam) is also indicated for acute agitation. Be
advised that coadminstration of benzodiazepines with IM olanzapine is not recommended
due to risk of respiratory depression.
Chapter 97 MANAGEMENT OF THE VIOLENT PATIENT 673
10. What if two doses of haloperidol have not sedated the patient?
Don’t give a third dose. Supplement the haloperidol with a benzodiazepine; the two together
have a synergistic effect. If you used haloperidol 5 mg IM and repeated this once, try adding
lorazepam 2 mg IM or IV or diazepam 5 mg IM or IV. Alternatively, add an atypical
antipsychotic such as ziprasidone, risperidone, or olanzapine.
11. How do you use chemical restraint for sedation in a pediatric patient?
Very few of the psychotropic medications used for restraint in adults have been approved for
use in children. The most frequently used medication for rapid sedation in children is
lorazepam due to its rapid onset, short half-life, and multiple routes of administration (see
doses), but be wary of dysinhibition/paradoxical agitation. Haloperidol is a safe and effective
alternative and may be given IM or PO (see Table 97-1). Intravenous haloperidol has not been
approved by the FDA but may be effective. Haloperidol and lorazepam may be mixed together
in one syringe; this combination is safe and effective in the pediatric and adult population but
may lead to prolonged sedation.
1. Haloperidol 5 to 10 mg PO or IM; may repeat every hour as needed; max 30 mg; consider
adding diphenhydramine 50 mg PO or IM twice a day to reduce risk of EPS. Consider adding
lorazepam 1 to 2 mg PO or IM.
2. Olanzapine 10 to 20 mg PO or 10 mg IM; do not combine intramuscular olanzapine with
lorazepam due to risk of respiratory depression.
3. Lorazepam 1 to 2 mg PO, IM, or IV; may repeat hourly as needed.
KEY POINTS: PREFERRED DRUGS FOR CHEMICAL
RESTRAINT
KEY POINTS: MAJOR SIDE EFFECTS OF HALOPERIDOL
1. Akathisias
2. Dystonic reactions
3. Neuroleptic malignant syndrome (rare)
4. Anticholinergic effects
5. Hypotension
6. Lowered seizure threshold
12. Summarize the main side effects to watch for with these drugs.
Benzodiazepines may rarely cause hypotension and respiratory depression. The traditional
antipsychotics may cause hypotension and extrapyramidal or other dystonic symptoms (EPS).
Hypotension is rare, but EPS occurs in approximately 1% of patients. The most common
dystonic reactions are oculogyric crisis, torticollis, and opisthotonos, which are irregular
movements of the eyes, neck, and back, respectively. These symptoms may be prevented or
reversed with diphenhydramine or benztropine. Neuroleptic malignant syndrome (NMS) is a
medical emergency characterized by rigidity, hypertension, hyperthermia, and altered mental
status and can been seen after administration of antipsychotics. Treatment for NMS involves
supportive care and dantrolene.
Chapter 97 MANAGEMENT OF THE VIOLENT PATIENT674
Medication Adult Dose Pediatric Dose Onset Duration Side Effects
Benztropine 1–4 mg PO/IM/IV bid prn EPS 0.02–0.05 mg/kg/dose
n
IV 5–15 mins
n
IM 15–30 mins
n
PO 30–60 mins
6–12 hours Anticholinergic effects
Chlorpromazine 100 mg PO q 60 min prn or
50 mg IM q 60 min prn
n
PO 30–60 mins
n
IM 20–40 mins
4-6 hours Akathisia, NMS, EPS
Diazepam 2–10 mg PO/IM/IV q 30–60 min
prn
n
IV 1–5 mins
n
IM 20–30 mins
n
PO 30–40 mins
30–60 mins Respiratory depression, paradoxical
agitation, dysinhibition
Diphenhydramine 25–50 mg PO/IM/IV q 6 h prn
EPS
1.25 mg/kg/dose
n
IV 5–15 mins
n
IM 15–30 mins
n
PO 30–60 mins
4–6 hours Anticholinergic effects
Droperidol* 2.5–10 mg IM/IV q
60 min prn
0.03–0.07 mg/kg/dose
(max 2.5 mg)
n
IV 2–10 mins
n
IM 5–10 mins
2–3 hours Dystonias, akathisia, NMS hypotension,
QTc elevation, lower seizure threshold,
anticholinergic effects, hypotension
TABLE 97–1. QUICK REFERENCE FOR DOSING AND ADMINISTRATION OF MEDS FOR AGITATION
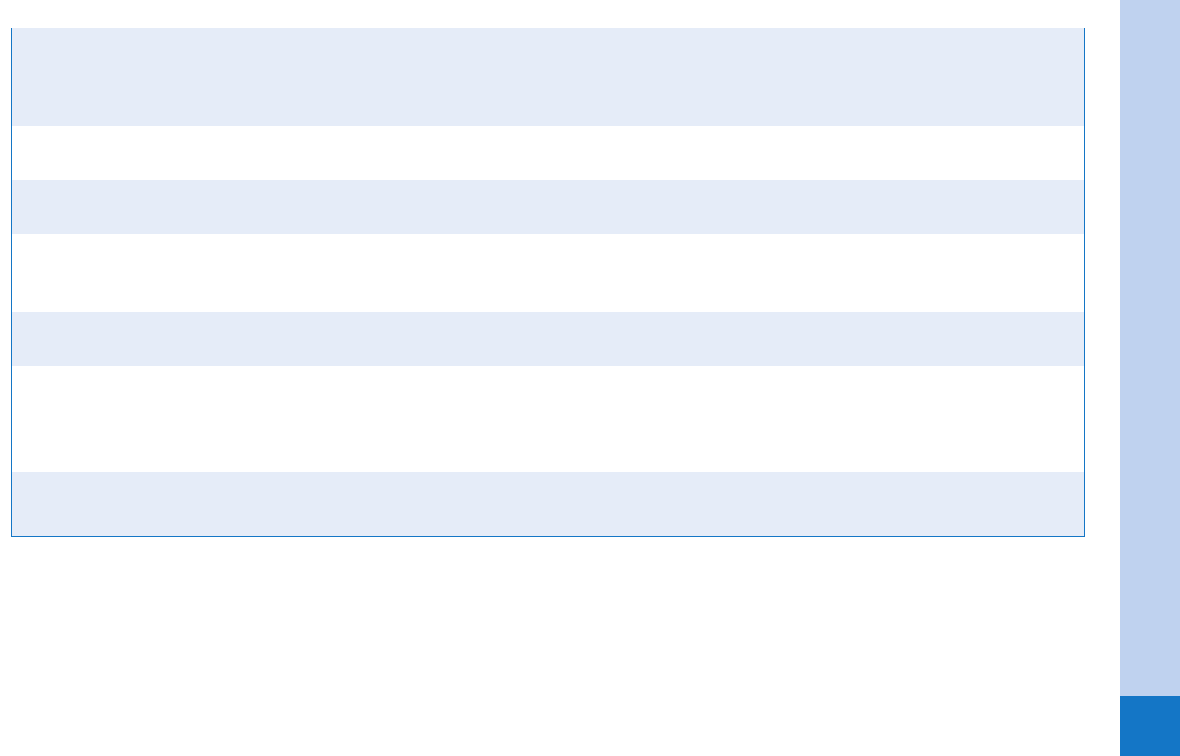
Chapter 97 MANAGEMENT OF THE VIOLENT PATIENT 675
*FDA Black Box Warning
EPS, extrapyramidal symptoms; IM, intramuscularly; IV, intravenously; NMS; neuroleptic malignant syndrome; PO, orally; PRN, as needed; q, every.
Haloperidol 2–10 mg PO/IM/IV q
30–60 min prn (max 30 mg)
0.025–0.075 mg/kg/dose
n
IV 2–5 mins
n
IM 30–40 mins
n
PO 30–60 mins
2–4 hours Dystonias, akathisia, NMS, hypoten-
sion, QTc elevation, lower seizure
threshold, anticholinergic effects
Lorazepam 0.5–4 mg PO/IM/IV q
30–60 min prn
0.05–0.1 mg/kg/dose PO/IV
n
IM/IV 5–10 mins
n
PO 30–40 mins
4–6 hours Respiratory depression, paradoxical
agitation, disinhibition
Midazolam 1–5 mg IM/IV q 60 min
prn
0.05–0.1 mg/kg/dose IV
(max 1.0 mg)
n
IV 1–5 mins
n
IM 15–20 mins
1–2 hours Respiratory depression, paradoxical
agitation, disinhibition
Olanzapine 5–20 mg PO/SL q 60 min prn or
2.5–10 mg IM tid prn
(max 30 mg daily)
n
PO/SL
30–60 mins
n
IM 20–40 mins
2–4 hours NMS, akathisia; do not mix intramus-
cular preparation with benzos
Risperidone 2-4 mg PO q 4 h (max 16 mg
daily)
n
PO 30–60 mins 2-4 hours Akathisia, NMS
Ziprasidone 80–120 mg PO bid or
10–20 mg IM q 4 h (max IM
dose 5 40 mg)
n
PO 30–60 mins
n
IM 20–40 mins
2–4 hours Akathisia, QTc elevation
Chapter 97 MANAGEMENT OF THE VIOLENT PATIENT676
13. Give a quick reference on dosing and administration.
See Table 97-1.
14. How should restrained patients be monitored?
Continuous pulse oximetry is indicated due to possible respiratory compromise, particularly
when ethanol-intoxicated patients receive chemical restraint. The Joint Commission requires
that physically restrained patients be directly and continuously monitored by trained staff.
15. Does the ED staff need any treatment?
The effect of violence on ED employees can be devastating; physical and psychological
trauma may have a long-lasting impact and such episodes may affect future job performance.
A comprehensive program patterned after the critical incident stress debriefing model should
be established to provide immediate and long-term psychological support, and staff should
be encouraged to avail themselves of this support when the need arises.
WEBSITE
Restraints: www.emedicine.com
BIBLIOGRAPHY
1. American Psychiatric Association: Seclusion and restraint, Task Force Report No. 22. Washington, DC, 1984,
American Psychiatric Association.
2. Battaglia SA, Ownby RL, Penalver A, et al: Haloperidol, lorazepam, or both for psychotic agitation? A
multicenter, prospective, double-blind, ED study. Am J Emerg Med 15:335–340, 1997.
3. Buckley PF, Noffsinger SG, Smith DA, et al: Treatment of the psychotic patient who is violent. Psychiatr Clin
North Am 26:231–272, 2003.
4. Chase PB, Biros MH: A retrospective review of the use and safety of droperidol in a large, high-risk, inner-city
ED patient population. Acad Emerg Med 9:1402–1410, 2002.
5. Hill S, Petit J: Psychiatric emergencies. Emerg Med Clin North Am 18:201–315, 2000.
6. Kao LW, Moore GP, Jackimczyk KC, et al: The combative patient: chemical restraints. In Marx JA, Hockberger
RS, Walls RM, et al, editors:: Rosen’s emergency medicine: concepts and clinical practice, ed 5, Mosby, 2002,
St. Louis, pp 2595–2599.
7. Lavoe FW: Consent, involuntary treatment and the use of force in an urban ED. Ann Emerg Med 21:25–32,
1992.
8. Nobay F, Simon DC, Levitt MA, et al: A prospective, double-blind, randomized trial of midazolam versus
haloperidol versus lorazepam in the chemical restraint of violent and severely agitated patients. Acad Emerg
Med 11:744–749, 2004.
9. Sorrentino A: Chemical restraints for the agitated, violent, or psychotic pediatric patient in the ED:
controversies and recommendations. Curr Opin Pediatr 16:201–205, 2004.
10. Zun LS: A prospective study of the complication rate of use of patient restraint in the ED. J Emerg Med
24:119–124, 2003.
ACKNOWLEDGMENT
The editors thank Danielle Raeburn, MD, and Katherine M. Bakes, MD for their contributions to this
chapter in previous editions of this text.
677
CHAPTER 98
INTIMATE PARTNER VIOLENCE
Debra Houry, MD, MPH
1. Isn’t intimate partner violence more of a law enforcement issue than it is a
health issue?
No. Research shows that up to one fourth of all women presenting to EDs for care have
experienced partner violence within the past year. Injuries and illnesses caused by abuse affect
their lives more frequently than diseases such as hypertension, cancer, or diabetes. Survivors
of intimate partner violence have higher rates of physical and mental health problems than
their peers.
2. Define domestic violence.
Domestic violence, in a broad sense, refers to all violence occurring within a family unit. By
this definition, partner abuse, child abuse, and elder abuse are subsets of domestic violence.
Intimate partner violence (IPV) is a more specific term, and it is used in this chapter. IPV
includes physical acts, such as battering and sexual assault, and nonphysical acts, such as
emotional abuse, economic abuse, threats to harm children and property, and prevention of
access to health care or prenatal care. Most battered women state that the nonphysical abuse
is more humiliating and distressing to them than physical beatings.
3. What are the risk factors for IPV?
IPV occurs in all socioeconomic classes and in all races. Women at greatest risk include
those with male partners who abuse alcohol or use drugs; are unemployed; have mental
health issues; have a history of pet abuse; have less than a high school education; or are the
former husband, estranged husband, or former boyfriend of the woman. Women who are
younger than 30 years; who are single, divorced, or separated; or who abuse drugs or
alcohol classically have been viewed as being at increased risk for IPV. It is unclear, however,
if some of these risk factors lead to the partner abuse or are a result of living in an abusive
situation.
4. Are men ever victims of partner abuse?
Yes, men do experience partner violence, but this is less often battering. Men may be
embarrassed to disclose IPV or worried that they may be the ones arrested if they go for help.
However, male IPV is not as lethal: a woman is 13 times more likely to be injured and 30%
more likely to be killed.
5. If IPV is so common, why have none of my patients experienced it?
Many of your patients may be experiencing partner abuse. Often, physicians do not know
because they do not ask about it.
6. What is the result of a missed diagnosis of IPV?
Failure to diagnose IPV may return the woman to a dangerous situation and increase her risk
of future injury. It also furthers the victim’s sense of entrapment and helplessness.
Inappropriate medications may be prescribed (tranquilizers and antidepressants) without a
search for the underlying causes of these symptoms. Patients may be labeled as being
hysterical, paranoid, and irrational.
