Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.


Chapter 95 ACUTE PSYCHOSIS658
6. Why is it important to control psychotic behavior immediately?
Patients who present in a psychotic state have no impulse control. They cannot distinguish
internal from external stimuli and are unable to prioritize their reactions to them. Because
of this dysfunction, they should always be considered a significant danger to themselves
or to others. The best way to deal with violent behavior is to prevent it. Emergency
physicians should recognize patients who are obviously confused, irrational, paranoid,
or excited. Emergency physicians must also develop an intuitive vigilance to detect the
possibility of violence in patients who present more rationally and less floridly psychotic.
Any history or comment that suggests violence should be taken seriously. The potential
for violence in general is particularly high in patients who are psychotic secondary to illicit
drug use.
7. Are there behavioral controls that can be used immediately for the psychotic
patient?
Yes. Recognizing the potential for violence and physical harm, definitive steps should be taken
to avoid confrontation:
n
Environmental: Keep the environment simple and stimuli-free, and minimize staff changes.
n
Interpersonal: Assume the role of patient advocate, and engage the patient in a calm and
self-assured voice. Recognize the patient’s right to privacy and dignity.
8. What options can be exercised if the patient becomes increasingly
disorganized, agitated, and violent?
See Chapter 97.
9. How do I obtain a history on a psychotic patient?
Because acutely psychotic patients may not be able to provide an adequate history, all
available sources for obtaining information must be explored. This may include speaking to
emergency medical services (EMS) personnel, family, friends, neighbors, and law enforcement
officers, as well as reviewing old medical records. A telephone conversation with caregivers
and significant others can also be helpful.
10. What historical information is important?
n
Onset. Did the behavior change suddenly or gradually?
n
Longitudinal course. What was the precipitating event? Is this the first such event? What
was the behavior like on previous events?
n
Psychosocial setting. Obtain some information regarding the patient’s support system.
n
Previous psychiatric disease, organic brain disease, the use or misuse of medication,
history of illicit drug use.
n
What are the current medications and have they been taken as prescribed?
11. How should my physical examination be tailored for a psychotic patient?
In retrospective reviews performed by Reeves, Tintinalli, and Riba, a high percentage of missed
organic diagnosis in psychotic patients was due to the lack of a complete history and physical
examination. Thus a complete and thorough physical examination, including a mental status
examination, is imperative. Always note the vital signs and pulse oximetry readings. In most
cases, emergency physicians will have built sufficient rapport with patients that they will
cooperate with the examination. Tell the patient exactly what you are doing and what you are
going to do during the examination. This helps to provide structure for the psychotic patient
and avoids confusion or misunderstanding.
12. What is the difference between organic and functional psychosis?
n
Organic psychosis refers to a reversible or nonreversible dysfunctional mental condition
that can be identified as a disturbance in the anatomy, physiology, or biochemistry of the
brain (i.e., dementia, withdrawal states and intoxications).
Chapter 95 ACUTE PSYCHOSIS 659
n
Functional psychosis refers to a dysfunctional mental condition identified as schizophrenia, a
major affective disorder, or other mental disorders with psychotic features (i.e., schizophrenia
and the affective disorders).
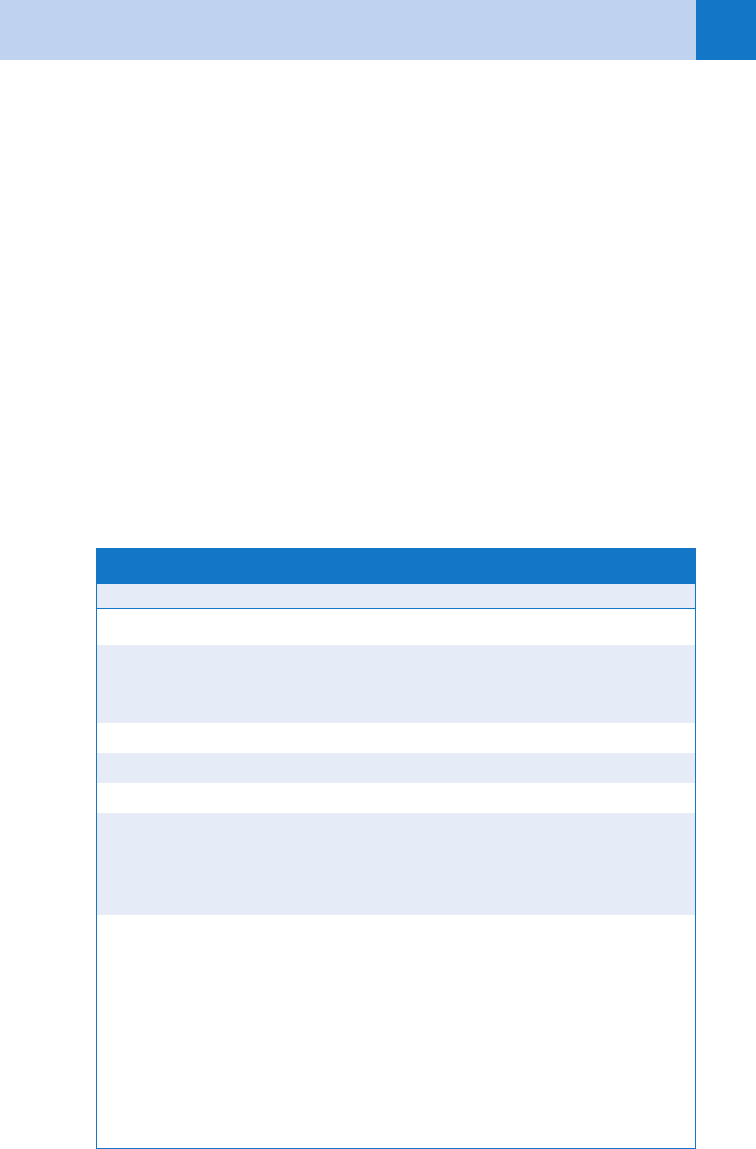
13. Summarize the key points to consider in the differentiation of organic from
functional psychosis.
See Table 95-1.
14. List the possible causes of alcohol-related organic psychosis.
n
Chronic alcoholism
n
Thiamine deficiency (i.e., diet, starvation, and emesis)
n
Alcohol-dependent withdrawal states
n
Comorbid substance abuse
n
Comorbid psychotic and mood disorder
n
Alcohol idiosyncratic intoxication (pathologic intoxication)
15. Is there a brief, self-limited, and nonorganic psychosis?
Yes. Some individuals may become acutely and briefly psychotic after exposure to an
extremely traumatic experience. If such a psychosis lasts for less than 4 weeks, it is termed a
brief psychotic disorder. Precipitants of the psychosis include the death of a loved one, a life-
threatening situation, such as combat or a natural disaster, or other life stressors. Patients
with hysterical, borderline, and narcissistic personalities are prone to brief psychotic disorder,
Organic Functional
M 5 Memory deficit Recent impaired Remote impaired
A 5 Activity Hyperactivity and hypoactivity
Tremor
Ataxia
Repetitive activity
Posturing
Rocking
D 5 Distortions Visual hallucinations Auditory hallucinations
F 5 Feelings Emotional lability Flat affect
O 5 Orientation Disoriented Oriented
C 5 Cognition Some lucid thoughts
Perceives occasionally
Attends occasionally
Focuses occasionally
No lucid thoughts
Unfiltered perceptions
Unable to attend
Unable to focus
S 5 Some other findings Age . 40
Sudden onset
Physical examination often
abnormal
Vital signs may be abnormal
Social immodesty
Aphasia
Consciousness impaired
Confabulation
Age , 40
Gradual onset
Physical examination
normal
Vital signs usually normal
Social modesty
Intelligible speech
Alert, awake
Ambivalence
TABLE 95–1. MADFOCS MNEMONIC

Chapter 95 ACUTE PSYCHOSIS660
and some studies support a genetic vulnerability. Emotional turmoil, confusion, and extremely
bizarre behavior and speech are common symptoms on presentation.
16. Summarize the potentially reversible causes of psychosis.
DEMENTIA mnemonic:
D 5 Drug toxicity
E 5 Emotional disorders
M 5 Metabolic disorders
E 5 Endocrine disorders
N 5 Nutritional disorders
T 5 Tumors and trauma
I 5 Infection
A 5 Arteriosclerotic complications
17. Name the life-threatening causes of acute psychosis.
WHHHIMP mnemonic:
W 5 Wernicke’s encephalopathy
H 5 Hypoxia or hypoperfusion of the central nervous system
H 5 Hypoglycemia
H 5 Hypertensive encephalopathy
I 5 Intracerebral hemorrhage
M 5 Meningitis/encephalitis
P 5 Poisonings
18. List pharmacologic agents that can cause acute psychosis.
n
Digitalis
n
Corticosteroids
n
Isoniazid (INH)
n
Disulfiram (Antabuse)
n
Tricyclics
n
Anticonvulsants
n
Cimetidine
n
Benzodiazepines
n
Amphetamines and related drugs
n
Antidysrhythmics
n
Narcotics
n
Barbiturates
n
Methyldopa
n
Nonsteroidal anti-inflammatory drugs
n
Anticancer agents
n
Recreational drugs: alcohol, cocaine, amphetamines
19. Is laboratory screening necessary in the work-up of an acute psychotic patient?
Patients, with established psychiatric diagnosis, presenting to the ED with psychiatric chief
complaints, benign histories, and normal physical examinations have a low likelihood of
clinically significant laboratory findings. Therefore, routine laboratory tests are not
recommended. If a patient presents with their first psychotic episode, then laboratory studies
are indicated to distinguish functional versus organic psychosis. The following tests are
recommended: complete blood count, electrolytes, toxicology screens, pregnancy test, thyroid
function tests and computed tomography (CT) scan of the brain.
20. Are there any other clinical rules of thumb in the work-up of the acute
psychotic patient?
Fever and psychosis 5 meningitis
Acute psychosis and alcoholism 5 Wernicke’s encephalopathy
Chapter 95 ACUTE PSYCHOSIS 661
Headache and psychosis 5 tumor or intracranial hemorrhage
Abdominal pain and psychosis 5 porphyria
Sweating and psychosis 5 hypoglycemia or delirium tremens
Autonomic signs and psychosis 5 toxic or metabolic encephalopathy
21. When should hospitalization be recommended?
If this is the patient’s first psychotic episode
If the patient is a danger to self or others
If the patient is unable to care for self appropriately
If the patient has no social support system
If the functional psychotic patient is not sufficiently clear after initial ED tranquilization
If an acute organic psychosis does not clear while the patient is in the ED
22. How do I treat the acutely psychotic patient in the ED?
See Chapter 97.
KEY POINTS: ACUTE PSYCHOSIS
1. Definition: delusions or prominent hallucinations
2. Least restrictive restraint: isolation; restraints; psychotropic medication
3. Complete and thorough history and physical examination, including mental status examination,
is imperative
4. Organic versus functional disorder
BIBLIOGRAPHY
1. American College of Emergency Physicians: Clinical policy for the initial approach to patients presenting with
altered mental status. Ann Emerg Med 33:251–281, 1999.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, ed 4, Washington, DC,
2000, American Psychiatric Association.
3. Bresler RE, Klinger BI, Erickson BJ: Acute intoxication and substance abuse among patients presenting to a
psychiatric emergency service. Gen Hospital Psychiatry 18:183, 1996.
4. Broderick KB, Lerner EB, McCourt JD, et al: Emergency physician practices and requirements regarding the
medical screening examination of psychiatric patients. Acad Emerg Med 9:88–92, 2002.
5. Frame DS, Kercher EE: Acute psychosis: Functional vs. organic. Emerg Med Clin North Am 9:123–136, 1991.
6. Hillard JF: Emergency treatment of acute psychosis. J Clin Psychiatry 59:57, 1998.
Consensus guidelines on the medical clearance examination for the evaluation and management
of the psychiatric patient in the emergency department: www.macep.org/site/index.php?option5
com_content&task5view&id557&Itemid574
WEBSITE
ACKNOWLEDGMENT
The editors gratefully acknowledge the contributions of Eugene E. Kerchner, MD, author of this
chapter in the previous edition.

Chapter 95 ACUTE PSYCHOSIS662
7. Kercher EE: Acute psychosis. In Rund DA, Barkin RM, Rosen P, Sternbach GL, editors: Essentials of
emergency medicine, ed 2, St. Louis, 1996, Mosby, pp 647–655.
8. Reeves RR, Pendarvis EJ, Kimble R: Unrecognized medical emergencies admitted to the psychiatric units.
Am J Emerg Med 2000. 18:390–393.
9. Riba M, Hale M: Medical clearance: fact or fiction in the hospital emergency room. Psychosomatic 1990.
31:400–404.
10. Tintinalli JE, Peacock FW, Wright MA. Emergency medical evaluation of psychiatric patients. Ann Emerg Med
1994. 23:859–862.
11. Yildiz A, Sachs GS, Turgay A: Pharmacological management of agitation in emergency settings. Emerg Med J
20:339–346, 2003.
12. Zun LS, Leikin JB, Stotland NL, et al: A tool for the emergency medicine evaluation of psychiatric patients. Am
J Emerg Med 14:329–333, 1996.
663
CHAPTER 96
DEPRESSION AND SUICIDE
Douglas A. Rund, MD, and Radu V. Saveanu, MD
DEPRESSION
1. What are the symptoms of depression?
The cardinal symptoms of depression are a dysphoric or sad mood or a loss of interest
or enjoyment. To diagnose depression, one of these must be present nearly every day
over a 2-week period. There must also be at least four of the following symptoms during
this same period: sleep disturbance, feelings of guilt or worthlessness, lack of energy,
decreased concentration or ability to make decisions, appetite disturbance (usually
diminished), psychomotor changes (agitated or slowed), and suicidal thinking. The
mnemonic SIG E CAPS can be remembered by thinking of what you want to do for
depressed patients (figuratively): prescribe energy capsules.
Five of the following are necessary for the diagnosis of depression, one of which must be
the I, loss of interests or depressed mood:
S 5 Sleep disturbance
I 5 Interests/mood
G 5 Guilt
E 5 Energy
C 5 Concentration
A 5 Appetite disturbance
P 5 Psychomotor changes
S 5 Suicidal thinking
2. Why is depression considered a mood disorder?
Mood refers to a person’s internal state, as subjectively experienced and reported by that
person. Affect is a person’s outward appearance, as objectively experienced by another. The
term mood disorder has essentially replaced affective disorder in much of the psychiatric
literature and communications. The main mood disorders are:
n
Major depression (or unipolar disorder), which is exclusively depression
n
Manic depression (or bipolar disorder), which is depression with a history of at least one
manic episode
3. What is the difference between primary and secondary depression?
Major depression is classified as primary if the symptom complex appears before or is
causally unrelated to any other significant medical or psychiatric illness. It is considered
secondary when it follows and is causally related to another medical or psychiatric
illness.
4. List medical conditions that might cause secondary depression.
Endocrine disorders
n
Hypothyroidism
n
Diabetes mellitus
n
Cushing’s syndrome
Neurologic disorders
n
Cerebrovascular accidents
n
Subdural hematoma
n
Multiple sclerosis
n
Brain neoplasm
n
Parkinson’s disease
n
Seizure disorder
n
Dementia
Connective tissue diseases
n
Systemic lupus erythematosus
Neoplasms
n
Pancreatic cancer

Chapter 96 DEPRESSION AND SUICIDE664
5. List medications that might cause secondary depression.
n
Antihypertensives (b-blockers)
n
Hypnotics and sedatives (benzodiazepines and barbiturates)
n
Corticosteroids
n
Cimetidine
n
Ranitidine
6. Why should the clinician always inquire about alcohol use when evaluating
depression?
Alcohol use and abuse is an extremely common comorbid condition with depression and
should always be queried for several reasons. First, alcohol use can be disinhibiting with regard
to behavior, putting a depressed and suicidal person at increased risk of impulsively acting on
suicidal tendencies. Second, depression cannot be treated effectively if there is ongoing alcohol
abuse. Third, alcohol is a depressant and is a common cause for depression, a problem known
as alcohol-induced mood disorder. It may be that the patient’s depression is secondary to
alcohol use and is treated best by abstaining from alcohol, rather than by administering an
antidepressant. This situation is suggested when the onset of the mood disturbance occurs
during an extended period of regular (usually daily) alcohol use, rather than before it.
7. When should I suspect depression when a patient presents with what seems
to be a medical complaint?
Screen for depression when patients present with nonspecific complaints, such as “sick all
over,” “weak and dizzy,” or “just feeling bad.” Using the SIG E CAPS mnemonic (see Question 1)
aids in diagnosis. Often depression is expressed in physical rather than emotional terms.
Nonspecific physical complaints, such as fatigue, exhaustion, headache, gastrointestinal
complaints, muscle aches, and nonspecific pain, are common. Anxiety is seen commonly with
depression and can manifest as shortness of breath, nervousness, irritability, and difficulty
swallowing, among other symptoms. Panic attacks, a severe form of anxiety that often occurs in
the context of depression, are a common cause of ED presentations of atypical chest pain.
8. Are psychotic features ever a manifestation of depression?
Sometimes. If psychotic symptoms accompany depression, it signifies a more severe and
dangerous form of depression. When this is the case, psychiatric consultation and often
psychiatric hospitalization are indicated. Common psychotic symptoms are hearing guilt-
provoking or self-critical voices, called auditory hallucinations, and fixed, false beliefs that can
be persecutory or paranoid in nature, referred to as delusions. Patients with psychotic
depression are at higher risk for suicide, especially when they have auditory hallucinations
commanding them to harm themselves.
9. Name therapies available for treatment of depression.
Antidepressant medications, psychotherapy, and electroconvulsive therapy.
10. What antidepressant medications are used to treat depression?
Tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) are the two oldest
classes of antidepressants, both of which have fallen into relative disuse because of their side
effects and dietary restrictions (in the case of MAOIs). Serotonin reuptake inhibitors are still the
most commonly prescribed class of antidepressants, mainly because of comparable efficacy,
greater ease of use, and fewer adverse effects. These are fluoxetine (Prozac), paroxetine (Paxil),
sertraline (Zoloft), citalopram (Celexa), fluvoxamine (Luvox), and Escitalopram (Lexapro).
Newer and perhaps better medications that act on multiple neurotransmitter systems are now
available, and also have better side-effect profiles than the older TCAs or MAOIs. These include:
n
Venlafaxine (Effexor)
n
Bupropion (Wellbutrin)
n
Mirtazapine (Remeron)
n
Duloxetine (Cymbalta)
Lithium, psychostimulants, and thyroid hormone are common adjunctive treatments.
Chapter 96 DEPRESSION AND SUICIDE 665
11. What are some psychotropic-related emergencies or precautions?
n
MAOIs in combination with sympathomimetic agents can cause hyperadrenergic crisis, and
their combination with meperidine (Demerol) or dextromethorphan can cause
cardiovascular instability and central nervous system excitability.
n
Neuroleptics can cause dystonias, including laryngeal spasm and neuroleptic malignant
syndrome (delirium, rigidity, fever, and autonomic abnormalities), both medical emergencies.
n
Anticholinergic toxicity may occur because many psychotropics have anticholinergic
properties and often are used in combination; these include benztropine mesylate
(Cogentin); trihexyphenidyl (Artane); diphenhydramine (Benadryl); TCAs; and low-potency
and mid-potency neuroleptics.
n
Many other commonly used agents have dose-related toxic side effects, particularly the mood
stabilizers, which include lithium and the anticonvulsants valproic acid and carbamazepine.
12. When should the emergency physician prescribe antidepressant therapy?
Because antidepressants generally take weeks to begin working and often require monitoring of
side effects and dose titration, prescribing them in the ED should be avoided whenever
possible. Exceptions include a patient who is already on treatment and needs a refill or a patient
who is initiating new treatment after an emergent consultative evaluation by a psychiatrist.
Ideally, in both of these cases, a 1- to 2-week supply of medication can be prescribed, and the
patient should follow up with outpatient psychiatric care.
13. What is the most serious complication of depression?
Suicide. Major depression accounts for an estimated 50% of all suicides.
14. Which patients should be hospitalized for depression?
Depressed patients who express suicidal intent or have a plan for suicide should be
hospitalized. Psychotically depressed patients should usually be admitted. Also, patients who
have just made a violent suicide attempt, have tried to avoid rescue, or are refusing help
should be admitted for further observation. Do not forget to institute suicidal precautions
while these patients are in the ED.
SUICIDE
15. What is the proper approach to a patient who has attempted suicide?
Medical management of any life-threatening condition precedes psychiatric evaluation. It is
important, however, that as the treatment proceeds, the ED team maintain a nonjudgmental
approach. Punishment or ridicule is neither therapeutic nor proper conduct for medical
professionals. Nearly all patients who attempt suicide are at least ambivalent about the wish to
live or die. Demeaning or harsh treatment of such patients, especially by health professionals
who are symbols of medical authority, worsens the already low self-esteem and may make
subsequent psychiatric care more difficult.
16. Describe suicide precautions.
Because some patients have been known to repeat a suicide attempt while in the ED, suicide
precautions are necessary. Such precautions include searching the patient and recovering
weapons, pills, or other potential means of self-injury; keeping the patient under close
observation; recovering any potential dangerous items from the immediate care area (e.g.,
needles, scalpels, glass, razors); and not allowing the patient to go anywhere (e.g., bathroom)
unaccompanied. When constant staff observation is not possible, physical restraints may be
necessary to protect the severely suicidal patient from further self-harm.
17. Are accidents ever suicide attempts?
It is important to remember that victims of trauma may have actually attempted suicide.
Single-victim accidents, such as a car driven at high speed into a concrete structure, a
pedestrian hit by a high-speed vehicle, or a fall from a height, are classic examples of suicide
Chapter 96 DEPRESSION AND SUICIDE666
attempts presenting as trauma. Medical management should be followed by an assessment of
suicide intent, including a discussion with family members and perhaps psychiatric
consultation.
18. What psychiatric disorders are associated with attempted suicide?
Major depression, alcohol and drug dependence, schizophrenia and other thought disorders,
personality disorders, panic disorder, adjustment disorders, and organic brain syndromes.
19. How do I evaluate the risk of a subsequent suicide in someone who attempted
suicide?
The following elements are part of an emergency assessment of suicide risks: age, gender,
marital status, social supports, physical illness, previous attempts, family history of suicide,
risk of the attempt versus likelihood of rescue, secondary gain, nature of any psychiatric
illness, alcohol or drug abuse, attitude (hopelessness, impulsivity) affect, and future plans of
the suicide attempter. If, after reviewing these factors, the emergency physician is still unsure
of the patient’s risk, psychiatric consultation is often helpful.
20. How does age relate to suicide risk?
Older patients (especially . 65 years) are statistically more likely to complete suicide than
younger patients. Such patients may experience loss of spouse, loneliness, physical illness, or
economic hardship in addition to depression. A worrisome increase in suicide among younger
persons has emerged, however. Suicide is now the third leading cause of death in youth and
young adults (19–24 years of age).
21. What role does gender play?
The rates of completed suicide in men are higher than those for women, whereas the rates
of attempted suicide are higher for women than for men. This difference has to do with the
lethality of the means. Men attempt suicide more often by violent means, such as shooting,
stabbing, hanging, or jumping from a height, whereas women typically use less violent and
less lethal methods, such as drug overdose.
22. What is the relationship of marital status to risk of successful suicide?
Never having been married carries the highest risk, followed in decreasing magnitude of risk
by being widowed, separated, divorced, and married.
23. What about other social support?
Unemployment, loneliness, loss of home, and relative isolation increase the risks of suicide.
Church, family, or community support helps to mitigate suicide risk.
24. Is there a relationship between physical illness and suicide risk?
Yes. Patients with a medical illness, especially a painful, incurable one, may seek a “way out”
through suicide. The most common nonpsychiatric diagnoses associated with suicide are
chronic medical conditions, such as cancer, chronic obstructive pulmonary disease, and
chronic pain. Renal dialysis patients have a suicide rate 400 times higher than the general
population, and HIV patients also have a higher than average rate.
25. Does a history of prior suicide attempts signify increased risk?
Yes, especially if each subsequent attempt escalates in severity. The risk of completed suicide
is more than 100 times the average in the first year after an attempt—200 times greater for
people older than 45 (National Mental Health Association: www.nmha.org). An exception may
exist if the previous attempts all have been minor and considered to be manipulative acts.
26. What is the relationship of family history to suicide risk?
Patients with a family history of suicide, alcoholism, or depression have a higher suicide risk
than patients without such a family history. A family history of suicide in first-order relatives
(e.g., parent or sibling) should cause particular concern.
Chapter 96 DEPRESSION AND SUICIDE 667
27. How does the risk of the suicide attempt and the likelihood of rescue affect a
suicide evaluation?
In general, a more serious or risky attempt is considered a more likely predictor of subsequent
attempts than a minor attempt. An attempt carried out in such a way that rescue is probable is
associated with a lower risk of subsequent successful suicide. The patient’s belief about the
lethality of the attempt is at least as important as the physician’s assessment of the
seriousness of it.
1. Patients thought what they did in their attempt to commit suicide was likely to kill them.
2. They did it in such a way as to have a low chance of being rescued.
3. They are not talking much about how they are feeling now.
4. They have little social support and are unwilling to reach out to others or accept help from
available resources.
5. They still want to die.
KEY POINTS: SERIOUS SUICIDE ATTEMPTS
28. What is secondary gain as it applies to suicide attempt?
Sometimes a suicide attempt seems to have a goal other than death. This goal, which is
termed secondary gain, may be increased attention from parents, friends, or lovers. In
attempts with no expected gain other than death, the potential for subsequent successful
suicide is great. With the increase in successful suicides among the young, the physician
must be careful in ascribing suicide attempts to the desire for attention or secondary gain until
a reasonably thorough evaluation can be completed.
29. What is the value of assessing the suicidal patient’s attitude and affect?
The patient who appears exhausted, helpless, hopeless, or lonely represents high risk. The
patient who attempts suicide because of anger or in an effort to gain revenge has a much
better prognosis than one who appears quiet, sad, fatigued, or apathetic.
30. Why is it important to inquire about a specific plan?
Never hesitate to ask the patient about any plans regarding suicide. The patient who continues
to express suicidal ideation after one attempt is at risk for a subsequent attempt. The risk is
highest if the plan is detailed, violent, or feasible.
31. What is the SAD PERSONS Scale?
In 1983, Patterson et al. used known high-risk characteristics to develop the mnemonic SAD
PERSONS Scale. The scale was designed to be used by nonpsychiatrists to assess the need
for hospitalization in suicidal patients. Hockberger and Rothstein modified the scale to
facilitate use in the ED (see Table 96-1). A score of 5 or less indicates that a patient probably
can be discharged safely. Scores of 6 or more require psychiatric consultation, and a score of
9 or more indicates the probable need for psychiatric hospitalization.
32. In general, which suicidal patients should be hospitalized?
n
Absolute indications for hospitalization after suicide attempts (involuntarily, if necessary)
usually include the following: presence of psychosis; a violent, nearly lethal preplanned
attempt; and continued suicidal ideation with definite plans for a repeated attempt.
n
Relative indications include age older than 45; high risk-to-rescue ratio; serious mental
illness; alcoholism; drug addiction; living alone with poor social support; and hopelessness,
helplessness, or exhaustion.
