Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.

other factors such as age, physical exercise, stress, and
coexisting medical problems.
Gastrointestinal Tract
0012 Swelling and tingling of the lips, tongue, and throat
can present as initial symptoms of food allergy occur-
ring as the antigen comes into contact with these
organs. Nausea and vomiting are common acute
symptoms, and abdominal pain and diarrhea also
occur frequently.
0013 The pathological changes in the small intestine
which occur in food allergy have been characterized
from biopsy specimens. It is well documented that
mucosal damage can occur in cows’ milk protein al-
lergy and there is evidence that reactions to soya, egg,
fish, and chicken may also result in mucosal damage.
0014 More extensive intestinal mucosal damage is seen
in celiac disease in response to the ingestion of gluten.
Although abnormal immunological mechanisms are
believed to be partially responsible for this condition,
the exact mechanism remains uncertain. (See Celiac
(Coeliac) Disease.)
0015 Food allergy can also lead to inflammatory changes
in the large bowel and bloody diarrhea (proctocolitis)
in infants. However, in adults there is a lack of
evidence to suggest an immunological basis for large-
bowel disorders. (See Colon: Diseases and Disorders.)
Skin
0016Urticaria (an itchy raised skin rash also known as
nettle rash) and angiedema (swelling of the skin,
mucous membranes, and underlying tissues) are fre-
quently seen as manifestations of food allergy. There
is increasing evidence that food intolerance may be a
cause of eczema but the basic mechanism of the reac-
tion is still unclear. Infantile eczema is certainly more
common in children from atopic families. Such reac-
tions frequently occur in response to cows’ milk pro-
tein and may be ameliorated by dietary manipulation.
Respiratory Tract
0017Sneezing and rhinorrhea (running of the nose) can be
manifestations of food allergy, either in association
with gut or skin symptoms or alone. More rarely,
bronchoconstriction occurs when a food is ingested,
but food allergy is not a common cause of asthma.
Anaphylactic Shock
0018Although the majority of food-allergic reactions are
not life-threatening, a small proportion of reactions
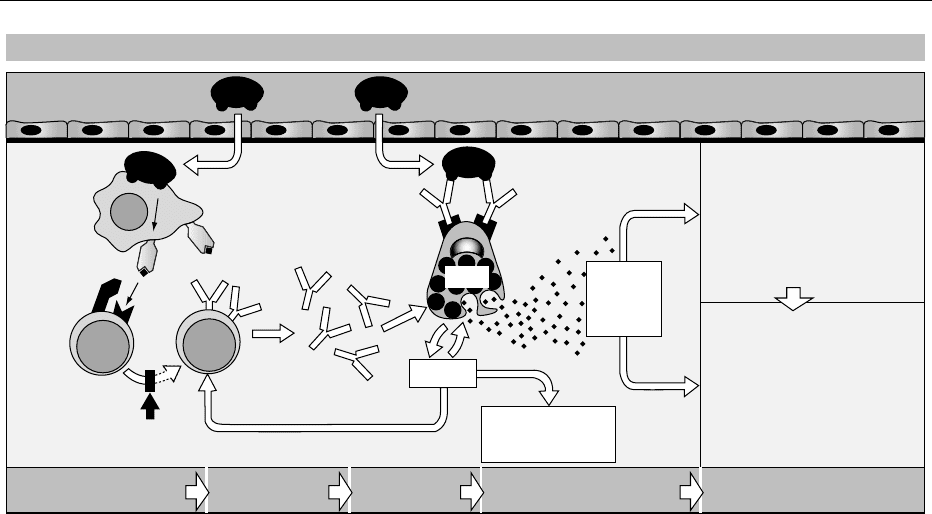
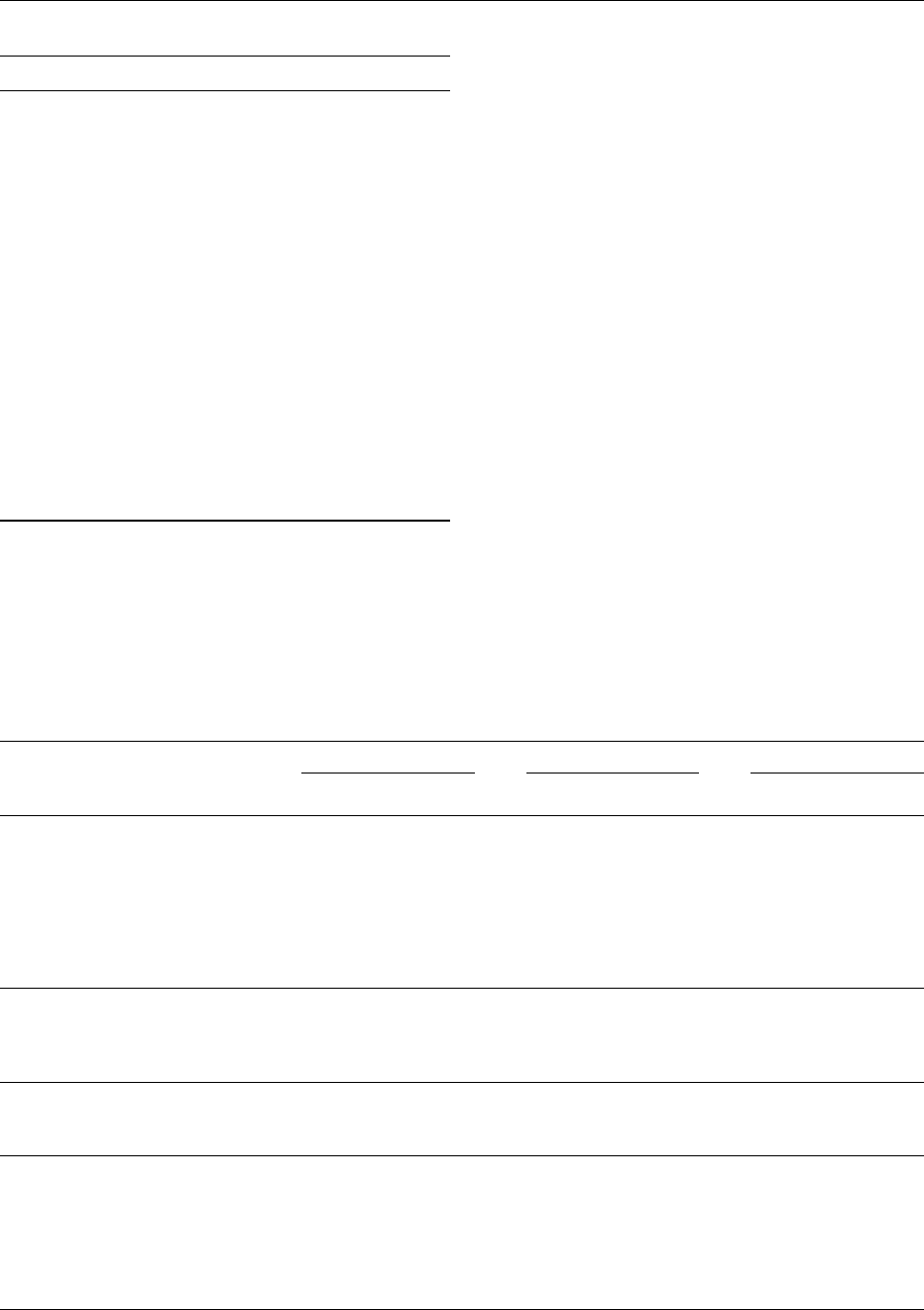
Antigen presentation IgE production
Mast cell
activation
Mediator release Clinical effects
IFN-γ
IL-4, IL-5, IL-6
Cytokines
GM-CSF, TNF-α
IL-8/9, inflammatory
cell activation
IL-3, IL-4,
Preformed
and newly
formed
mediators
Pharmacological effects
Blood vessels, airways, etc.
Cell infiltration and
accumulation
Clinical effects
Hayfever
Asthma
Eczema
Anaphylaxis
Mucosal surface
Processing
and presentation
Antigen
IgE
IL-4
IL-10
TH2
Bε
APC
Ca
2+
↑
Overview: induction and effector mechanisms in type I hypersensitivity
fig0002 Figure 2 Innocuous environmental antigens (allergens) enter via mucosal surfaces and are taken up by local antigen-presenting
cells (APCs), which process and present them to TH cells. TH2 cells secrete cytokines that induce B-cell proliferation and favor the
production of an allergen-specific immunoglobulin E (IgE) response. The IgE binds, via Fce receptors (FceRI), to mast cells, thus
sensitizing them. When allergen subsequently reaches the sensitized mast cell, it cross-links surface-bound IgE, causing an increase
in intracellular calcium (Ca
2þ
) that triggers the release of preformed mediators, such as histamine and proteases, and newly
synthesized, lipid-derived mediators such as leukotrienes and prostaglandins. These autocolds produce the clinical symptoms of
allergy. Cytokines are also released from degranulating mast cells and may augment the inflammatory and IgE responses. IL-4,
interleukin-4; IFN-g, interferor-g; GM-CSF, granulocyte – macrophage colony-stimulating factor. Adapted, with permission, from Roitt I,
Brostoff J and Male D (1998) Immunology, 5th edn. Sidcup: Mosby.
2628 FOOD INTOLERANCE/Food Allergies

can lead to anaphylactic shock (anaphylaxis), which
is severe and may be fatal. Anaphylaxis is an acute
allergic (IgE-mediated) reaction of rapid onset and
affecting many organ systems, including the cardio-
vascular system, the respiratory tract, the mouth, the
pharynx, and the skin, either individually or in com-
bination. It is characterized by swelling of the lips
and throat, shortness of breath, a rapid fall in blood
pressure, progressing to cardiovascular collapse and
severe shock. Treatment consists of intramuscular
injection of epinephrine (adrenaline), and without
this anaphylaxis may cause death. Anaphylactic reac-
tions are relatively rare, but there is evidence that
deaths from food-induced anaphylaxis are increasing.
In the UK and Europe, peanut is the most common
food reported to cause anaphylaxis, but other foods
that are known sometimes to cause the condition are
tree nuts, seeds, eggs, milk, and shellfish. Inadvertent
exposure to potential allergens in foods containing, or
contaminated with, minute amounts of the allergen
poses a major risk to the small number of people at
risk of anaphylaxis.
Predisposition to Food Allergies
0019 It is believed that genetic predisposition and immuno-
logical predisposition, notably elevated serum IgE
levels, are the most important determinants of allergic
disease. Environmental factors are secondary but may
still play an important role; they include nondietary
factors such as the level of allergen exposure, which
may be influenced by season of birth, maternal
smoking habit, exposure to pollutants, viral illness,
and the nutritional status of the individual.
0020 The importance of genetic factors in the etiology of
allergic disease and IgE production is evident from the
simple observation that allergic disease is more
common in the children of atopic parents. Children
from families where both parents are atopic have
more than a 50% chance of developing an allergic
disorder; where one parent is atopic, the chance is
about 30%. However, twin studies have shown that
concordance is far less than 100% in monozygotic
(identical) twins, indicating that environmental
factors are also important in the expression of atopic
disease.
0021 Research in atopic families and twins suggests that
total IgE levels are influenced by genetic factors. The
major control of antigen-specific IgE responses is be-
lieved to be linked to the human leukocyte antigen
(HLA) immune response genes. However, HLA-
linked genes do not appear to be responsible for
high IgE levels. There is evidence that general levels
of IgE may be determined by other genes, including
those responsible for cytokine production.
0022Inherited immune deficiency disorders, e.g., defi-
ciencies of complement or IgA, can also predispose
towards allergy. The presence of a specific type of
IgA, secretory IgA, in the gut is believed to reduce
antigen absorption. It might be deduced that IgA
deficiency could lead to increased antigen absorption
and IgE antibody stimulation. However, again the
explanation must be more complex, as not all such
people develop allergy.
0023As ingested food travels through the gut, it presents
the immune system with a vast array of foreign par-
ticles to distinguish. The intestinal mucosa itself is a
barrier which can protect against dietary antigens and
the secretion of mucus from intestinal goblet cells and
the production of secretory IgA are protective mech-
anisms which help to reduce antigen absorption. Dis-
ruption of the intestinal barrier, as occurs after
intestinal infection, and increased permeability of
the barrier, as in premature infants, the newborn, in
malnutrition, and in immune deficiency, may increase
the penetration of antigens.
0024The significance of increased gut permeability in
the etiology of food allergic disease is nevertheless
uncertain. It has been demonstrated that antigens
can cross the gut wall in both allergic and nonallergic
individuals, and that immune complexes may circu-
late in the blood of nonallergic individuals without ill
effect. This underlines the complexity, as well as the
gaps in our understanding, of the ways in which
genetic and environmental factors may interact to
cause allergic disorders.
Vulnerability of the Newborn to Food
Allergy
0025It is evident from clinical experience that the newborn
is vulnerable to food allergens. For example, there is
clear evidence that infants exposed to unmodified
cows’ milk within the first few weeks of life are
particularly susceptible to the development of symp-
toms of allergy to cows’ milk such as eczema. How-
ever, our knowledge of the pathogenesis of food
allergic disease and the relative importance of the
various contributory factors in the neonatal period
is still limited.
0026The immunological response to feeding a ‘foreign
protein’ may result from the immaturity of neonatal
digestive and absorptive functions and early penetra-
tion of the antigens. It has also been suggested that
because newborn infants are temporarily deficient in
IgA – secretory IgA does not appear until the age of
2–4 weeks – the gut mucosa is particularly vulnerable
to antigen penetration.
0027The influence of maternal diet during pregnancy
and lactation, the protective role of breast-feeding,
FOOD INTOLERANCE/Food Allergies 2629

and the timing and introduction of solids at
weaning may all play their part in the pathogenesis
of food allergic disease. The coincident occurrence
of infection with the introduction of a specific
antigen may also be a crucial factor. (See Pregnancy:
Safe Diet.)
0028 The idea that breast-feeding might protect against
allergic disease has existed for some 50 years. Al-
though there are many studies that support this idea,
there are many that do not. Such conflict appears to
result from the difficulty in controlling studies on
infants and differences in methodology. (See Infants:
Breast- and Bottle-feeding.)
0029 On balance, it appears that breast-feeding de-
creases the likelihood of allergic disease in children
who are ‘at risk’ because of family history. To some
extent this is due to the late introduction of foreign
protein but it is also attributable to the presence of
protective immunological factors, such as IgA, in col-
ostrum and breast milk. Breast milk protects against
infection, and breast-feeding should help to maintain
the integrity of the gastrointestinal mucosa in the
neonatal period.
0030 The level of total IgE in umbilical cord blood is
believed to be predictive of allergic disease. The influ-
ence of maternal diet on cord blood immunoglobulin
levels and the placental transfer of antibodies to spe-
cific food proteins in atopic and nonatopic mothers
are subjects of active research at the present time. As
yet the influence of maternal diet on allergic outcome
in the offspring remains uncertain.
0031 The current view is that sensitization in utero does
occur. However, the influence of dietary manipula-
tion of the mother in pregnancy in preventing food
allergy in the infant is contentious and in need of
further research before it can be recommended.
0032 Food antigens pass into breast milk in small
amounts and these are significant in immunological
terms. It is believed that this may lead to sensitization
in susceptible infants. Therefore the exclusion of spe-
cific foods from the mother’s diet during lactation
may be beneficial for at-risk infants. Again, this is
the subject of research.
0033 The potential severity of the reactions associated
with peanut allergy has led to the recommendation, in
the UK, that pregnant and breast-feeding women
from atopic families (whether they are themselves
atopic or if the father or any other sibling has atopic
disease) should avoid peanuts and peanut products in
order to reduce the risk of peanut allergy developing
in their offspring. However, the scientific basis for
this recommendation is still open to debate and
other countries have not made similar recommenda-
tions. (See Food Intolerance: Types.)
0034Particularly important for at-risk infants is the
timing of weaning and the nature of the foods intro-
duced early on. Exclusive breast-feeding, for at least 4
and preferably 6 months, and avoidance of the early
introduction of foods commonly known to cause al-
lergies, e.g., cows’ milk and its products, eggs, wheat,
fish, nuts, and citrus fruits, would seem to be the best
preventive approach. However, more research is
needed on the links between weaning and subsequent
development of food allergic disorders. (See Infants:
Weaning.)
Prevalence of Food Allergies
0035It is difficult to arrive at a precise estimate of the
prevalence of food allergic disease because of the dif-
ferent testing procedures and diagnostic criteria used
in research studies. Figures ranging from 1% to 20%
have been cited, but the true prevalence is currently
estimated to be towards the lower end of this range,
at about 2%. Our present state of knowledge suggests
that food allergy is far less common than food intol-
erances (with a nonimmunological basis), and less
common than allergic reactions to pollen and house
dust. However, as yet there are no systematic data to
permit the accurate calculation of the incidence and
prevalence of food allergic reactions, either in the UK
or elsewhere.
See also: Allergens; Colloids and Emulsions; Colon:
Diseases and Disorders; Food Intolerance: Types;
Immunology of Food; Infants: Breast- and Bottle-
feeding; Weaning; Pregnancy: Safe Diet;
Prostaglandins and Leukotrienes
Further Reading
British Nutrition Foundation (2002) Adverse Reactions to
Food. Report of the British Nutrition Foundation Task
Force. Oxford: Blackwell Science.
Cant AJ (1991) Food allergy and intolerance. In: Mclaren
DS et al. (eds) Textbook of Paediatric Nutrition, 3rd
edn, pp. 204–221. London: Churchill Livingstone.
Food Standards Agency (2000) Adverse Reactions to Food
and Food Ingredients. Report from the Committee on
Toxicity of Chemicals in Food, Consumer Products and
the Environment. London: TSO.
Roitt I, Brostoff J and Male D (1998) Immunology, 5th edn.
Sidcup: Mosby.
2630 FOOD INTOLERANCE/Food Allergies
Milk Allergy
S L Taylor and J Kabourek, University of Nebraska,
Lincoln, NE, USA
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Introduction
0001 Cows’ milk is one of the most common causes of
adverse reactions in foods and can occur through
several mechanisms. True cows’ milk allergy (CMA)
occurs through an immunoglobulin E (IgE) mediated
mechanism. The prevalence of allergy to cows’ milk is
reported to be about 2% of the general pediatric
population in developed countries. Treatment of
CMA involves the strict avoidance of cows’ milk
and products containing cows’-milk proteins. Educa-
tion of both the affected child and parents is also vital
to successful management of CMA.
Milk Allergy
0002 Cows’ milk is one of the most common causes of
adverse reactions in foods and can occur through
several mechanisms. True CMA or hypersensitivity
is indicative of an adverse reaction to bovine milk
proteins that produces symptoms and where an im-
munologic mechanism may be implicated. CMA is
mainly an IgE-mediated, type I immediate hypersen-
sitivity reaction, although type III and IV reactions
have also been implicated. CMA is considered the
most severe form of intolerance because the threshold
dose for elicitation of a reaction is low, and symptoms
can be severe in some affected individuals.
0003 Classified by Coombs and Gell, hypersensitivity
reaction mechanisms are divided into four types:
I–IV. The first three types are antibody-mediated,
whereas the fourth type is mediated by T cells and
macrophages.
0004 Type I (anaphylactic) reaction is immediate and
is due to interaction of antigen (allergen) with IgE-
sensitized mast cells and basophils, resulting in
histamine and mediator release from these cells.
0005 Type II (cytotoxic) reaction involves both IgG and
IgM antibodies. A specific cell or tissue is targeted,
activating the complement cascade and causing
cytotoxic cells to damage membranes.
0006 Type III hypersensitivity (immune complex) in-
volves an antigen–antibody complex, causing an
inflammatory response with fixation of complement.
0007 Type IV (cell-mediated) hypersensitivity involves T
cells producing cytokines that recruit phagocytes and
other inflammatory cells. Continued stimulation of
these cells causes tissue damage.
0008In true IgE-mediated CMA, exposure of susceptible
individuals to one or more of several cows’-milk al-
lergens (naturally occurring proteins) elicits the pro-
duction of allergen-specific IgE antibodies. These IgE
antibodies become fixed to the membranes of mast
cells in the tissues and basophils in the blood. This
symptomless process is called allergic sensitization.
Upon subsequent exposure to cows’ milk, the specific
cows’-milk allergen cross-links two IgE antibodies on
the membrane surface of the sensitized mast cells and
basophils. This interaction triggers the release of a
host of bioactive mediators from the mast cells and
basophils, including histamine, leukotrienes, and
prostaglandins. These mediators are responsible for
the range of symptoms experienced in an allergic
reaction.
0009Cows’-milk protein intolerance (CMPI), not to
be confused with IgE-mediated CMA, is generally a
nonimmune-mediated reaction against cows’-milk
proteins. CMPI is probably a cell-mediated inflam-
matory reaction that damages the absorptive function
of the intestinal tract. Symptoms are primarily gastro-
intestinal (nausea, abdominal cramps, and diarrhea)
and delayed, appearing several days after milk inges-
tion. Generally, CMPI is a disorder occurring in
infancy that is frequently outgrown.
0010Lactose intolerance refers to inadequate diges-
tion of lactose, the major carbohydrate found
in milk, usually from a deficiency or low levels
of b-galactosidase (lactase) enzyme. Lactose
intolerance produces gastrointestinal symptoms,
including cramps, bloating, gas, diarrhea, and/or
nausea. In contrast to CMPI and CMA, lactose in-
tolerance primarily affects adults.
Composition
0011Cows’ milk is a nutrient-dense food consisting of
varying amounts of carbohydrate, fat, and protein.
The major constituents of cows’ milk are water
(87.4%) and milk solids (12.6%), which includes
vitamins, minerals, carbohydrate, fat, and protein.
Cows’ milk is known to contain many nutrients,
including varying concentrations of fat and water-
soluble vitamins, minerals, trace elements, and
salts. The principal carbohydrate in milk is lactose.
The lactose content of milk varies by species. Cows’
milk contains about 4.8% lactose (12–12.5 g lactose
per cup), whereas human milk has 7% lactose.
In addition to lactose, minor quantities of glucose,
galactose, and oligosaccharides are present. Milk
fat is a complex lipid existing as an oil-in-water
emulsion. Milk lipids are mainly triacylglycerols
or fatty acid esters with glycerol, of which more
than 400 have been identified. Phospholipids,
FOOD INTOLERANCE/Milk Allergy 2631

sterols, waxes, and free fatty acids have also been
identified.
0012 Cows’ milk is a heterogeneous mixture of at least
20 proteins. Eighty percent of the total protein is
casein proteins and 20% is whey proteins. Caseins
are relatively heat-stable, whereas whey proteins are
more labile. Casein can be fractionated into four
major components: alpha, beta, kappa, and gamma
casein. The whey proteins consist of a-lactalbumin, b-
lactoglobulin, bovine serum albumin, and several
minor proteins, including lactoferrin and lactoper-
oxidase.
0013 Great variability of the human IgE response to
cows’ milk exists. Many patients are allergic to
more than one milk protein. The major allergens of
cows’ milk are a-
s1
casein and b-lactoglobulin. a-
Lactalbumin is also involved in some patients. IgE
antibodies directed to minor cows’-milk proteins,
such as bovine serum albumin and lactoferrin, have
been identified in a few patients but their role in CMA
is not firmly established.
Prevalence
0014 CMA and CMPI are primarily diseases of infancy.
CMA has become one of the most common food
allergies in early childhood since cows’ milk is usually
one of the first foreign antigens encountered in large
quantities in infancy. Most infants develop symptoms
before 1 month of age, often within 1 week of
introduction. Onset of CMA after 1 year of age is
extremely rare. Major risk factors for CMA are a
positive family history of CMA or other atopic dis-
ease and early cows’-milk protein exposure. The
onset of disease in most cases is closely related to
the time of introduction of cows’-milk products.
The prevalence of allergy to cows’ milk is reported
to be about 2% of the general pediatric population in
developed countries. CMA occasionally occurs in
adults, affecting less than 1% of the adult population;
however, good prevalence estimates for CMA in
adults are not available.
Prevention
0015 Because cows’ milk is usually one of the first foreign
antigens encountered in infancy, preventive measures
are ideally employed during this time period, particu-
larly in children of atopic parents. Although conflict-
ing data exist and no single prevention method is
completely effective, protective effects have been
seen with breast-feeding and delaying introduction
of cows’ milk.
0016 Prolonged breast-feeding in all infants is the ideal
source of nutrition, providing immunological factors,
developing intestinal maturation, and enhancing
infant–mother bonding. The protective effect of
breast-feeding may be due, in part, to avoidance
of high doses of cows’-milk proteins or an inherent
protective effect of human milk. Support for the
benefits of breast-feeding in preventing or delaying
the development of CMA has been seen in
prolonged breast-feeding practice of at least 6
months. In addition to breast-feeding, delaying the
introduction of cows’ milk until 6 months of age
also has a preventive effect. If breast-feeding is not
possible or during weaning, an extensively hydro-
lyzed formula in combination with delayed milk
introduction may be protective. Partially hydrolyzed
infant formulas (PHF) are also available. These
formulas appear beneficial in the prevention of
sensitization to cows’ milk and are more palatable
than extensively hydrolyzed formula (EHF). But the
partial hydrolysates can provoke allergic reactions
in previously sensitized infants. There may be a pre-
ventive effect of maternal avoidance of common
allergenic foods during lactation but there has been
no protective effect shown for an altered diet
during pregnancy. Occasionally, CMA seems to de-
velop in exclusively breast-fed infants, ostensibly
from exposure to small amounts of cows’-milk pro-
teins secreted into the breast milk and arising from
the mother’s diet. However, cows’ milk is so import-
ant in the nutrition of lactating women that avoid-
ance of cow’s milk during the lactation period is not
often recommended. Similarly, the practice of cows’
milk avoidance during pregnancy should not be sug-
gested because it may put the health of the mother as
well as the fetus in jeopardy of nutritional compli-
cations or deficiencies.
Symptoms/Manifestation
0017Clinical manifestations and severity of symptoms of
CMA vary widely from one individual to another.
Symptoms arise involving the skin, gastrointestinal
or respiratory tracts. The majority of patients have
greater than two symptoms affecting greater than two
organs/systems. CMA in individuals exhibiting gas-
trointestinal symptoms and/or dermatitis usually re-
solves early in life, whereas individuals with urticaria,
angioedema, respiratory symptoms, or anaphylaxis
may persist with CMA into adult life.
0018Individuals with immediate reactions often exhibit
systemic anaphylaxis and/or dermatological symp-
toms. Anaphylaxis is a systemic, multiorgan reaction
associated with IgE-mediated hypersensitivity. It may
progress slowly or rapidly and can involve hypoten-
sion, bronchospasm, edema, and cutaneous symp-
toms. Treatment for anaphylaxis involves the use of
2632 FOOD INTOLERANCE/Milk Allergy

epinephrine (adrenaline) given intramuscularly, anti-
histamines, and steroids. Although severe reactions to
cows’ milk are rare, deaths have been documented.
Dermatological features may include urticaria,
angioedema, and eczema (dermatitis).
0019 Intermediate reactions occurring from 1 to 24 h
after ingestion may involve gastrointestinal symp-
toms, including vomiting, diarrhea, reflux, colic,
and bleeding.
0020 Symptoms appearing more than 24 h after cows’-
milk ingestion often affect the respiratory tract and
skin. Respiratory symptoms may involve nasal stuffi-
ness, coughing, wheezing, tachypnea, and rhinitis.
Atopic dermatitis is a rather common manifestation
of CMA involving the skin; it can be a chronic
condition.
Diagnosis
0021 Differentiation between CMA and CMPI cannot
be based on clinical symptoms alone, nor is there a
lone clinical test. The first step in evaluation of some-
one with a history of possible adverse reactions is to
take a detailed food history. Along with identifying
the suspected food, the quantity of food needed to
produce symptoms and the frequency with which
reactions occur need to be reported. Physical exams
may be helpful in revealing a chronic skin condition
such as atopic dermatitis. However, other physical
signs, such as respiratory symptoms, may be present
but are not necessarily a result of food hypersensitiv-
ity and may be attributed to other conditions. Gastro-
intestinal complaints, in particular, can have
numerous causes.
0022 Diagnosis is usually based on cows’-milk protein
elimination and challenge tests. Open, controlled
cows’-milk challenges are recommended for in-
fants 0–1 year. In children older than 1 year and
adults, double-blind placebo-controlled challenges
(DBPCFC) are performed. These tests determine if
cows’ milk is the cause of symptoms but do not
identify the mechanism.
0023 Several methods, including skinprick test and radio-
allergosorbent test (RAST), are available as diagnostic
tools in identifying immunological-mediated CMA.
Recent advances in RAST have improved the diag-
nostic value of these tests and lessened the need to
perform DBPCFCs. Milk-specific IgE is seen in some
milk-hypersensitive individuals but not all. CMPI
may be suspected if symptoms are restricted to the
gastrointestinal tract and have delayed onset,
especially in cases where specific IgE antibodies are
absent.
0024 Presently, allergic sensitization to cows’-milk pro-
teins usually occurs during the first few years of life,
often disappearing thereafter. The majority of
children outgrow CMA and CMPI and will acquire
tolerance, with an estimated remission rate of 85–
90% before 3 years of age. However, an early in-
creased IgE response to cows’ milk proteins is associ-
ated with an increased risk of persisting allergy to
cows’-milk proteins, development of asthma or rhi-
noconjuctivitis, or development of atopic disorders
later in life.
Treatment/Management
0025Treatment of CMA and CMPI involves the strict
avoidance of cows’ milk and products containing
cows’-milk proteins. Because even a minute amount
of allergen has the potential to trigger sensitization
and/or symptoms, awareness is key in treatment.
Breast milk is the ideal source of nutrition. If breast-
feeding is not possible, numerous formulas are avail-
able as cows’-milk substitutes.
0026Soy protein formulas can be well tolerated by some
individuals. However, soy is also a commonly aller-
genic food and has been reported to cause symptoms
in some CMA individuals due to the development of
soy allergy.
0027Meat-based formulas from sources such as chicken
or lamb may be used but have also been shown to
cause symptoms on rare occasions. Also, a formula
based on goats’ milk contains b-lactoglobulin and
often causes symptoms in CMA individuals.
0028More commonly, modified-protein formulas are
the treatment of choice. Protein hydrolysates are
classified as PHF or EHF and may be derived from
casein or whey. For the most part, however, these
EHFs are generally tolerated and are a good alterna-
tive for CMA management. A few CMA infants will
respond adversely to trace amounts of milk proteins
or peptides present in EHF.
0029PHF were developed for the purpose of dietary
prevention of CMA and are not recommended for
individuals who already have CMA. EHF have been
in use for over 50 years as a therapeutic diet in
CMA management and are the recommended treat-
ment. However, palatability of EHF is an issue, and
EHF can be quite costly. In severely sensitive indi-
viduals, hypoallergenic, nutritionally complete
infant formula composed of individual amino acids
(elemental formula) may be the only effective substi-
tute.
0030Hypoallergenic formula or breast-feeding should
be the recommended dietary options for infants with
CMA for the first 6 months of life. From 6 months
of age, solid foods may be introduced. Generally,
highly allergenic foods such as egg, soy, peanut, fish,
and wheat are also avoided until the age of 1 year.
FOOD INTOLERANCE/Milk Allergy 2633
Reintroduction of cows’-milk protein may be per-
formed in 3–6-month intervals after the age of
1 year; with infants having severe CMA, pediatric
advice should be sought before attempting reintro-
duction.
0031 Education of both the affected child and parents
is vital to successful management of CMA. Both
the physician and dietitian can provide guidance
and recommend ways for introducing foods in
childhood. This helps guarantee a cows’-milk pro-
tein-free diet as well as a nutritionally complete diet.
Dietitians are also very useful in teaching how to read
labels on food packages and identifying milk-derived
products.
See also: Food Intolerance: Types; Food Allergies;
Lactose Intolerance; Elimination Diets; Infant Foods:
Milk Formulas
Further Reading
American Academy of Pediatrics Committee on Nutrition
(2000) Hypoallergenic infant formulas. Pediatrics 106:
346–349.
Exl B-M, Mu
¨
ller-Teicher G and Vandenplas Y (2000) Pre-
ventative possibilities within the context of cow’s milk
allergy. Allergy and Clinical Immunology International
12: 68–76.
Hosking CS, Heine RG and Hill DJ (2000) The Melbourne
milk allergy study – two decades of clinical research.
Allergy and Clinical Immunology International 12:
198–205.
Novembre E and Vierucci A (2001) Milk allergy/intoler-
ance and atopic dermatitis in infancy and childhood.
Allergy 56(suppl. 67): 105–108.
Pelto L, Salminen S, Lilius E-M, Nuutila J and Isolauri E
(1998) Milk hypersensitivity – key to poorly defined
gastrointestinal symptoms in adults. Allergy 53:
307–310.
Savilahti E, Kuitunen P and Visakorpi JK (1981) Cow’s milk
allergy. In: Lebenthal E (ed.) Textbook of Gastroenter-
ology and Nutrition in Infancy, pp. 689–708. New York:
Raven Press.
Sicherer SH (2000) Determinants of systemic manifest-
ations of food allergy. Journal of Allergy and Clinical
Immunology 106: S251–S257.
Sprikkelman AB, Heymans HS and Van Aslderen WMC
(2000) Development of allergic disorders in children
with cow’s milk allergy or intolerance in infancy. Clin-
ical and Experimental Allergy 30: 1358–1363.
Wal J-M (1998) Cow’s milk allergens. Allergy 53:
1013–1022.
Zeiger RS (2000) Dietary aspects of food allergy prevention
in infants and children. Journal of Pediatric Gastroenter-
ology and Nutrition 30: S77–S86.
Lactose Intolerance
F Suarez, Abbott Laboratories, Columbus, OH, USA
C Shannon, The Toledo Hospital, Toledo, OH, USA
S Hertzler, The Ohio State University, Columbus, OH,
USA
D Savaiano, Purdue University, West Lafayette, IN,
USA
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Introduction
0001Lactose intolerance is best defined as the development
of gastrointestinal symptoms after the consumption
of the ‘milk sugar’ lactose. Symptoms of intolerance
can occur in most humans and all mammals if the
amount of lactose consumed exceeds the ability of the
gastrointestinal tract to digest this lactose. Thus, lac-
tose intolerance is intermittent since it depends on
both the dose of lactose and the response of the
gastrointestinal tract. Lactose, a carbohydrate unique
to milks and dairy foods, is a disaccharide composed
of glucose and galactose, synthesized in the mammary
glands of almost all mammals. Young mammals have
a large capacity to digest lactose due to a very high
activity of a digestive enzyme (a lactase) found on the
lining of the small intestine. Most humans and all
mammals exhibit a reduced level of this lactase
enzyme (and thus a reduced capacity to digest lactose)
as they mature past infancy. Interestingly, approxi-
mately 25% of the human population maintains a
high level of lactase activity and therefore a large
capacity to digest lactose throughout life. These indi-
viduals are called lactose-tolerant or lactose digesters.
A more scientific name for this group is lactase-per-
sistent since the enzyme activity is maintained or
persists. The majority of lactose digesters come from
northern European, central African and Middle East-
ern backgrounds. The remaining 75% of the world’s
population, including almost all Asians, Native
Americans, and many Africans and Latinos, are thus
described as lactose-intolerant or lactase-nonpersis-
tent. The regulation of intestinal lactase activity is
under genetic control.
0002The belief that lactase-nonpersistent individuals
will always have abdominal symptoms, such as flatu-
lence, abdominal pain, and diarrhea, following dairy
food consumption has resulted in many individuals
eliminating dairy products from their diet in an effort
to prevent symptoms. However, dairy products pro-
vide key nutrients and the majority of calcium found
in the food supply. The elimination of milk and milk
products from the diet makes it very difficult to obtain
the recommended dietary allowance of calcium
from natural dietary sources. The average American
2634 FOOD INTOLERANCE/Lactose Intolerance

woman consumes only 50–60% of the 1000–1500 mg
recommended for maximum retention of body cal-
cium. Inadequate calcium intake compromises bone
structure and may eventually result in osteoporosis.
Thus, it is important to provide clear dietary manage-
ment that allows lactase-nonpersistent individuals
to consume adequate amounts of essential nutrients,
including calcium, while avoiding symptoms of
intolerance.
0003 Lactose intolerance must not be confused with milk
allergy. Milk allergy is caused when the immune
system reacts against one or more of the proteins
found in milk. Milk allergy usually develops in early
infancy, before 1 year of age. In developed countries,
the incidence in infancy is estimated at 5% and
the remission rate is about 90% before 3 years of
age. Gastrointestinal symptoms are reported in ap-
proximately 50% of infants with milk allergy while
cutaneous symptoms are more common and respira-
tory symptoms less so. In contrast, lactose intolerance
has no immunological bases, only follows the loss of
intestinal lactase activity, which occurs around 3–5
years of age, and is limited to gastrointestinal symp-
toms.
0004 To understand the dietary management of lactose
intolerance, it is important to recognize that multiple
factors affect the body’s ability to digest and tolerate
lactose. These factors include: (1) the amount of lac-
tose ingested; (2) the level of the residual lactase
activity that remains after maturation; (3) gastro-
intestinal transit time; and (4) the capacity of the
colonic microflora to ferment (digest) lactose. This
article will review these factors in order to describe
a dietary approach to eliminate symptoms of intoler-
ance while consuming adequate calcium, as well as to
correct the perception that lactose intolerance is a
frequent and severe problem.
Lactose Digestion and Lactase Activity
0005 Lactose is present in varying degrees in all mamma-
lian milk, with the exception of the milk of the
sea lion. Mammary glands have a unique capability
to synthesize lactose via the enzyme lactose synthe-
tase. Lactose sythetase links the two monosaccharides
(simple sugars) glucose and galactose by a beta 1–4
bond, forming the disaccharide lactose. Cows’ milk
contains about 50 g l
1
of lactose, whereas human
milk contains one of the highest concentrations, up
to 75 g l
1
. Table 1 lists the lactose content of
common dairy foods. Fluid milk products have the
highest concentration of lactose. When cheese is
manufactured, lactose remains with the whey. Thus,
hard cheeses contain very small amounts of lactose
since the whey is removed in the elaboration process.
Lactose may also be found in medications in biologic-
ally insignificant amounts (milligrams) due to its
excellent tablet-forming properties.
0006Dietary lactose cannot be absorbed intact directly
across the small intestinal mucosa; it must first be
hydrolyzed. The enzyme lactase-phlorizin hydrolase
(commonly called lactase), a disaccharidase located
on the brush border of the intestinal epithelium,
breaks the chemical bond between glucose and gal-
actose. These monosaccharides are absorbed across
the intestine and transported to the liver for utiliza-
tion. The lactase enzyme is found must abundantly
in the proximal ileum and specifically only hydrolyzes
lactose. Human infant lactase is the last of the dis-
accharidases to appear during fetal production. The
gene responsible for the synthesis of lactase has been
located in humans on chromosome 2. Lactase activity
can be detected as early as 8 weeks after conception
and increases to that of only one-third of a full-term
infant by 34 weeks’ gestation. During late gestation
(35–38 weeks), lactase activity reaches approxi-
mately three-quarters of that of a full-term infant.
Lactase synthesis and activity are high in nearly all
full-term infants and remain high throughout the first
4 years of life.
0007At some point after weaning, a genetically
programmed reduction of lactase synthesis occurs,
in approximately three-fourths of the world’s
population, to a residual level of 5–10% that of in-
fancy. This loss of intestinal lactase activity is not a
disease, but rather a normal pattern in human physi-
ology and is transmitted by a recessive gene. The
decline in lactase activity is known as lactase-
nonpersistence (LNP) or primary acquired hypo-
lactasia and cannot be modified by continued expos-
ure to milk or lactose.
0008In humans there appears to be a mosaic pattern
of lactase activity in the jejunal enterocytes. In LNP
individuals, some jejunal enterocytes produce high
amounts of lactase while others, even those sharing
the same villus, do not produce lactase. Thus,
rather than a uniform reduction in lactase production
among all enterocytes, a hypolactasic individual
may have a patchy distribution of lactose-producing
enterocytes that are low in number relative to the
nonlactase-producing enterocytes. Current evidence
suggests that the regulation of lactase is accomplished
primarily at the level of transcription, although post-
transcriptional factors may still be elucidated.
0009Congenital lactose intolerance is an extremely rare
inborn error in metabolism in which detectable levels
of lactase are absent at birth (0–10 IU g
1
protein)
and remain abnormal throughout life. An infant
with congenital lactase deficiency will have severe
diarrheal illness beginning a few days after birth.
FOOD INTOLERANCE/Lactose Intolerance 2635
Treatment with a lactose-free diet eliminates symp-
toms and promotes normal growth and development.
0010 Because lactase enzyme protrudes from the mem-
brane of the epithelial cell and the greatest activity is
found at the tip of the intestinal villi, lactase is ex-
tremely vulnerable to intestinal disease or insult. Sec-
ondary hypolactasia is a temporary condition caused
by damage to the enterocytes via disease, poisons
such as alcohol, medications, surgery, or radiation
to the gastrointestinal tract (Table 2). This condition
is relatively common in developing countries, but
most common in Third-World countries where
chronic intestinal infections are prevalent. Once the
causative disease is resolved and the epithelium heals,
lactase activity returns to normal. Total resolution of
the insufficiency may require up to 6 months or more
of diet therapy.
Assessment of Lactase Levels and
Lactose Maldigestion
0011Lactase level can be ascertained with a modest degree
of accuracy simply from the determination of the
subject’s heritage, because prevalence varies among
ethnic and racial groups (Table 3). Individuals of
African, Asian, middle Eastern, Mediterranean
(Jews, southern Italians, Greeks, Arabs), and Native
American origin have a greater than 70% chance of
being LNP. Subjects of Scandinavian and middle
European origin have about a 5% and 15% chance
of being LNP, respectively.
0012The geographical and racial distribution of lactase
persistence has led to the hypothesis that three separ-
ate gene mutations occurred several thousands of
years ago in places where dairy foods had become
tbl0001 Table 1 Lactose and calcium content of selected milks, milk products, and substitutes
Product Serving size Lactose (g perserving) Calcium (mg)
Milk 1 c (237 g) 11 291
Low-fat milk, 2% fat 1 c (237 g) 9–13 297
Lactaid milk, 1% fat, 70% lactose-reduced 1 c (237 g) 3.6 300
Skim milk 1 c (237 g) 12–14 302
Chocolate milk 1 c (237 g) 10–12 280
Sweetened, condensed whole milk 1 c (306 g) 35 868
Dried whole milk 1 c (128 g) 48 1168
Nonfat dry milk, instant 1.5 c (91 g) 46 1120
Buttermilk, fluid 1 c (245 g) 9–11 285
Whipped-cream topping 1 tbs (3 g) 0.4 10
Light cream 1 tbs (15 g) 0.6 14
Half and half 1 tbs (15 g) 0.6 16
Low-fat yogurts 1 c (227–258 g) 11–15 314–415
Cheese
Blue 1 oz (28 g) 0.7 150
Camembert 1 oz (28 g) 0.1 110
Cheddar 1 oz (28 g) 0.4–0.6 204
Colby 1 oz (28 g) 0.7 194
Cream 1 oz (28 g) 0.8 23
Gouda 1 oz (28 g) 0.6 198
Limburger 1 oz (28 g) 0.1 141
Parmesan, grated 1 oz (28 g) 0.8 390
Cheese, pasteurized, processed
American 1 oz (28 g) 0.5 174
Pimento 1 oz (28 g) 0.5–1.7 174
Swiss 1 oz (28 g) 0.4–0.6 219
Cottage cheese 1 c (210 g) 5–6 126
Cottage cheese, low-fat, 2% fat 1 c (226 g) 7–8 155
Butter 2 pats (10 g) 0.1 2
Oleomargarine 2 pats (10 g) 0 1
Ice cream
Vanilla, regular 1 c (133 g) 9 176
French, soft 1 c (173 g) 9 226
Ice milk, vanilla 1 c (131 g) 10 176
Sherbet, orange 1 c (193 g) 4 103
Ice, orange 100 g 0 0
c, cup; tbs, tablespoon.
2636 FOOD INTOLERANCE/Lactose Intolerance
an important component of the adult diet. Darwinian
theory suggests that mutation yielded a survival ad-
vantage to subjects provided they were drinking
milk. Herding animals and the use of mammalian
milk as a human food originated in northern Europe,
the Middle East, and central Africa several thousand
years ago. Interestingly, it is in these populations that
lactase persistence also appeared. Thus, the current
view is that selective advantage in these populations
led to the maintenance of a genetic mutation in each
of these three populations. Inheritance has spread the
persistence trait to other populations. Table 4 shows
that approximately 200 million individuals in the
USA are lactase-persistent.
0013Lactase levels can be measured directly or indir-
ectly. Directly assaying the lactase activity requires a
mucosal biopsy from the jejunum, since the enzyme is
attached to the brush border of the small intestinal
mucosa. Such biopsies can be obtained at endoscopies
or via the use of a variety of tubes equipped with
biopsy capsules. While this test can accurately meas-
ure lactase activity, it is an expensive, invasive, and
time-consuming test and is therefore rarely used clin-
ically. Thus, lactase activity is usually assessed indir-
ectly from measurements of lactose absorption via
blood or breath tests. Digested lactose results in free
glucose, which is absorbed rapidly, and ultimately
tbl00 02 Table 2 Potentialcausesofsecondaryhypolactasia
Diseases
Small-bowelMultisystem
HIVenteropathyCarcinoidsyndrome
Regionalenteritis
(e.g.,Crohn’sdisease)
Cysticfibrosis
Diabeticgastropathy
Sprue(celiacandtropical)Protein-energymalnutrition
Whipple’sdisease
(intestinallipodystrophy)
Zollinger–Ellisonsyndrome
Alcoholism
AscarislumbricoidesinfectionIrondeficiency
Blind-loopsyndrome
Giardiasis
Infectiousdiarrhea
Shortgut
Iatrogenic
Chemotherapy
Radiationenteritis
Surgicalresectionofintestine
Medications
Colchicine(antigout)
Neomycin(antibiotic)
Kanamycin(antibiotic)
Aminosalicylicacid(antibiotic)
Adaptedfrom:SrinivasanRandMinochaA(1998)Whentosuspectlactose
intolerance:symptomatic,ethnic,andlaboratoryissues.Postgraduate
Medicine(1988)104:109–123;ScrimshawNSandMurrayEB(1988)The
acceptabilityofmilkandmilkproductsinpopulationswithahigh
prevalenceoflactoseintolerance.AmericanJournalofClinicalNutrition48:
1083–1159;SavaianoDAandLevittMD(1987)Milkintoleranceand
microbe-containingdairyfoods.JournalofDairyScience70:397–406.
HIV,humanimmunodeficiencyvirus.
tbl00 03 Table 3 Projectionsoflactosemaldigestionaroundtheworld(inmillions)
Area%Lactose
maldigesters
(LM)
199020002020
PopulationLMPopulationLMPopulationLM
Africa756294728056041172879
Asia100318631863688368845784578
Europe 20 721 144 729 146 722 144
Latin America 70 442 309 520 364 645 452
North America 25 278 70 307 77 363 91
Oceania 25 27 7 31 8 38 10
World 5283 4188 6080 4887 7518 6154
(79%) (80%) (82%)
GeoHive,2002ONLINE.Availablehttp://www.geohive.com/global/index.php[2002].
tbl0004 Table 4 Projections of lactose maldigestion in the USA (in millions)
% Lactose
maldigesters
(LM)
19 9 0
millions of
people
LM
millions of
people
2000
millions of
people
LM
millions of
people
2025
millions of
people
LM
millions of
people
African-Americans 75 30 23 34 25.5 44 33
Asian-Americans 100 7 7 11 11 20.5 20.5
Caucasian 20 188 28 197 39.4 209 41.8
Hispanic (all races) 60 22 13 31 18.6 60 36
Native Americans 100 2 2 2 2 2.5 2.5
Total 29 249 72 275 96.5 336 133.8
(% of population) 29% 35% 40%
Source: US Department of Commerce; 1990 census and estimates.
FOOD INTOLERANCE/Lactose Intolerance 2637
