Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.


increases blood glucose levels. The blood glucose test
involves feeding a standard 50-g lactose dose and
measurement of plasma glucose every 30 min over a
period of 2 h. In the presence of lactose maldigestion,
blood glucose increases less than 25 mg dl
1
above
the fasting level. Unfortunately, this test is mildly
invasive and with a relatively low reliability.
0014 Because of its ease, low cost, and noninvasiveness,
the breath hydrogen test is most widely used to diag-
nose lactose maldigestion. Undigested lactose remains
in the intestine and is fermented by colonic bacteria,
producing hydrogen gas, carbon dioxide, and me-
thane in some individuals. Bacterial fermentation is
the only source of molecular hydrogen in the body. A
portion of the hydrogen produced in the colon dif-
fuses into the blood and is excreted via the lungs. The
breath test measures the excretion of this hydrogen.
Typically, a subject is given an oral dose of lactose
following an overnight (12 h) fast. Breath samples
are collected at regular intervals for a period of 5–8h
and analyzed by gas chromatography. The historical
test used 50 g of lactose as a challenge dose, and an
increase of 20 parts per million (p.p.m.) or greater
above the fasting level as an indicator of lactose mal-
digestion. More recently, it has been shown that using
a sum of hydrogen from hours 5, 6, and 7 and a 15
p.p.m. above-fasting criterion for maldigestion
resulted in 100% sensitivity and specificity for carbo-
hydrate maldigestion.
Pathophysiology of Lactose Maldigestion
0015 A positive breath hydrogen test measures undigested
carbohydrate in the colon and is indicative of lactose
maldigestion. However, the correlation between lac-
tose maldigestion and intolerance symptoms, such as
flatulence, abdominal pain, and diarrhea, is unclear.
The lactose may or may not result in perceptible
symptoms depending on a number of factors, includ-
ing the amount of lactose entering the colon, the
metabolic activity of the colonic flora, the absorptive
capacity of the colonic mucosa for the end products
of lactose fermentation, and the ‘irritability’ of the
colon.
0016 Colonic bacteria metabolize lactose, thereby redu-
cing osmotic pressure in the colon. If the colonic
bacteria did not ferment undigested lactose, the os-
motic activity of even relatively small doses of lactose
could result in diarrhea. However, diarrhea is virtu-
ally never encountered when LNP subjects ingest a
cup of milk (12 g of lactose). Colonic bacteria ferment
lactose to short-chain fatty acids that are readily
absorbed by the colon. However, when massive
quantities of carbohydrate are maldigested, colonic
absorption of fatty acids may not keep up with
production. In this situation the bacteria may actually
enhance the osmotic activity and hence aggravate the
ensuing diarrhea.
0017In the fermentation process of lactose, appreciable
quantities of gas (carbon dioxide, hydrogen, and
sometimes methane) are also produced. The removal
of these gases is accomplished by bacterial utilization,
excretion in flatus, or by absorption through
the colon. With small doses of lactose, gas may be
removed as rapidly as it is produced and there will
be no symptoms. However, with large lactose loads
these removal mechanisms may not keep up with
production, and bloating, distention, and flatulence
result.
0018A final important factor that plays a role in the
development of gastrointestinal symptoms is the re-
sponse of the colon to the presence of gas and organic
acids. Subjects with an ‘irritable’ colon might perceive
symptoms whereas subject with a ‘nonirritable’ colon
might tolerate the same degree of distention without
symptoms. The intensity of symptoms may also vary
with the amount of lactose consumed, the degree of
colonic adaptation, and the physical form of the lac-
tose-containing food.
The Relationship Between Lactose
Maldigestion and Lactose Intolerance
0019The larger the dose of lactose, the greater the risk that
the LNP subject will perceive symptoms of lactose
intolerance. Early unblinded studies in which subjects
were fed milk or lactose and then asked if they had
symptoms suggested that over 45% had symptoms
following a glass of milk or its lactose equivalent
(12 g). The results of such studies have provided the
basis for claims that many subjects require a diet
severely restricted in milk and milk products or the
use of a variety of commercially available lactose-
digestive aids. However, tolerance to milk can be
affected by factors unrelated to its lactose content
and may be due to psychological factors or cultural
attitudes toward milk. There is a psychogenic com-
ponent to abdominal symptomatology, particularly
relating to the minor and nonspecific type of symp-
toms (bloating, distension), that may result from
ingested food. The true symptomatic potential of
milk (or other foods) can only be obtained with
rigidly controlled double-blind studies. Under these
controlled conditions, researchers have found that
lactose intolerance is less prevalent than commonly
believed. For example, in a well-controlled trial, 50 g
of lactose (the quantity in a quart (approx. 1l) of
milk), taken as a single dose caused symptoms in
most of LNP subjects. On the other hand, several
blinded studies indicated that LNP subjects tolerated
2638 FOOD INTOLERANCE/Lactose Intolerance

up to one cup (237 ml) of milk without experiencing
significant symptoms. However, the results of these
studies did not gain general acceptance, in part be-
cause of failure to utilize subjects with ‘severe’ lactose
intolerance. Some LNP individuals believe that small
amounts of lactose, such as the amount used with
coffee or cereal, cause gastrointestinal distress.
0020 In 1995, our group conducted a study in 30 self-
described ‘severely lactose-intolerant individuals.’
Initial breath hydrogen test measurements indicated
that approximately 30% (9 of 30) of the subjects
claiming severe lactose intolerance were digesters,
and thus, had no physiological basis for intolerance
symptoms. Among the true lactose maldigesters
there were no significant differences in symptoms
of bloating, flatulence, or number of flatus passages
during the period when conventional milk (lactose-
containing) versus lactose-hydrolyzed milk was
ingested. During both treatment periods, symptoms
were extremely mild. The triviality of these
symptoms with conventional (or lactose-hydrolyzed)
milk was particularly impressive given the subjects’
prestudy perception that symptoms would be so bad
that they would be compelled to withdraw from
the study. These findings further demonstrate how
strongly behavioral and psychological factors influ-
ence symptom reporting. Additional research is ne-
cessary to evaluate the psychological component of
symptom reporting in lactose maldigesters.
Lactose Digestion and Calcium
0021 Lactose maldigestion could potentially increase risk
of osteoporosis either by decreased milk, and there-
fore calcium, intake or by decreased calcium absorp-
tion. Lactose maldigestion has been associated with
lower calcium intakes and consequently a higher
prevalence of osteoporosis. A sizable fraction of
lactose maldigesters may unnecessarily restrict
their intake of lactose-containing, calcium-rich dairy
foods. Milk and milk products contribute 73% of the
calcium to the US food. A second potential relation-
ship between lactose maldigestion and osteoporosis is
that maldigestion of lactose decreases absorption of
calcium. Human and animal studies suggest that
lactose stimulates the intestinal absorption of
calcium. However, there is considerable disagreement
regarding the influence of lactose and lactose maldi-
gestion on calcium absorption in adults. Differences
in study methodology (milk versus water, dose of
lactose, and the choice of method for determining
calcium absorption) may explain contrasting results.
Physiologic doses of lactose (up to two cups (474 ml)
of milk) do not appear to have a significant impact on
calcium absorption. Therefore, increased prevalence
of osteoporosis in lactose maldigesters is most likely
related to avoidance of dairy foods and subsequently
inadequate calcium intake rather than impaired intes-
tinal calcium absorption.
Dietary Management for Lactose
Maldigestion
0022There are several dietary strategies that effectively
reduce or eliminate intolerance symptoms without
compromising nutritional status (Table 5).
Dose–Response to Lactose
0023There is a strong positive correlation between the
dose of lactose consumed and the symptomatic re-
sponse. In general, increasing the amount of lactose
consumed increases the number and severity of symp-
toms. In lactose maldigesters, 2 g of lactose is almost
completely absorbed, whereas 6 g of lactose results in
a minimal degree of maldigestion as measured by
breath hydrogen. On average, maldigesters absorbed
about half of a 12.5-g lactose load, whereas the other
half passes to the terminal ileum. Interestingly,
unblinded studies have frequently reported intoler-
ance symptoms after consuming only 12 g lactose. In
1995 a double-blind protocol demonstrated that
feeding 12 g of lactose (approximately one cup of
milk) with a meal resulted in minimal to no symptoms
in maldigesters who believed themselves to be
extremely intolerant to lactose. Further evidence
indicated that lactose-intolerant individuals could
consume two cups (474 ml) of milk daily with
divided doses at breakfast and dinner, without experi-
encing appreciable symptoms. Overall, a dose con-
taining 18–25 g of lactose has the potential to
produce symptoms (mostly flatulence) in approxi-
mately half of a population. However, the frequency
of symptoms varies from less than 40% to greater
than 90% of a subgroup. Thus, a first important
dietary strategy is to limit milk consumption to one
eight-ounce glass (12.5 g lactose) per meal. Doing so
will dramatically reduce the likelihood of intolerance
symptoms.
Factors Affecting Gastrointestinal Transit of
Lactose
0024A key explanation of the large variability in dose–
response studies is whether or not the lactose is fed
with a meal. Consuming milk with other foods slows
the intestinal transit of lactose. Slowing the intestinal
transit permits longer contact between residual
lactase in the small intestine and lactose, thus improv-
ing digestion and reducing the potential for symp-
toms. It is also possible that additional food in the
intestine may slow the rate at which lactose is delivery
FOOD INTOLERANCE/Lactose Intolerance 2639
in the colon. A slower entry of lactose into the colon
might also improve the fermentation and reduce the
potential for symptoms.
0025 Individual foods also affect lactose digestion and
tolerance. Whole milk, due to its greater fat
and energy content, may slightly decrease breath
hydrogen relative to skim milk. Whether this effect
is large enough to improve tolerance is unclear. Like-
wise, the addition of chocolate to milk may improve
lactose digestion and symptoms, possibly due to its
higher osmolality or energy content and/or the effect
of cocoa on intestinal transit. Thus, a second key
dietary recommendation is to consume milk and
other lactose-containing dairy foods with meals.
This strategy will also insure that adequate calcium
intake can be achieved without symptoms of intoler-
ance.
Yogurts
0026 Lactose that is found in yogurt with live active cul-
tures (Lactobacillus delbrueckii subsp. bulgaricus and
Streptococcus salivarius subsp. thermophilus)is
digested better than lactose in milk. As a result,
yogurt is well tolerated by lactose-intolerant individ-
uals. During the manufacture of yogurts, milk solids
are typically added to fluid milk to enhance the prod-
uct. During yogurt production, the bacteria reduce
the lactose level from around 6% to approximately
4%. Lactic acid bacteria in yogurt exhibit a very high
activity of b-galactosidase. This activity functions
during the manufacturing process, and most import-
antly also during gastrointestinal digestion of lactose
in vivo in the stomach and/or small intestine. Clinical
studies have showed that consumption of up to 18 g
lactose as yogurt (two cups of yogurt) is well toler-
ated, and results in few symptoms of intolerance.
0027Pasteurization of yogurt increases the shelf-life but
decreases the number of active cultures that are partly
responsible for improved lactose digestion. However,
pasteurized yogurt is moderately well tolerated, pro-
ducing minimal symptoms. It is believed that the
physical form of the yogurt and the caloric density
are additional factors that improve tolerance to lac-
tose found in yogurt. Thus, a third dietary strategy is
to include yogurts as a part of a calcium-rich and
well-tolerated diet.
Lactase Supplements and Lactose-Reduced Milks
0028Pills, capsules, and drops that contain lactase deriv-
ed from yeast (Kluyveromyces lactis) or fungal
(Aspergillus niger, A. oryzae) sources have proved
effective for lactose digestion. Since 1984, these
over-the-counter preparations have been given the
status of generally recognized as safe (GRAS) by
the US Food and Drug Administration. Additionally,
milk that has been treated with lactase, resulting in a
70–100% reduction in lactose, is commercially avail-
able. Lactose-hydrolyzed milk typically has increased
tbl0005 Table 5 Dietary strategies for lactose intolerance
Factorsaffecting
lactosedigestion
Dietarystrategy References
Dose of lactose Consume a cup (237 ml) of milk or less at a time,
containing up to 12 g lactose
Suarez et al. 1995
Hertzler et al. 1996
Suarez and Savaiano 1997
Intestinal transit Consume milk with other foods, rather than
alone, to slow the intestinal transit of lactose
Solomons et al. 1985
Martini and Savaiano 1988
Dehkordi et al. 1995
Yogurts Consume yogurts containing active bacteria
cultures. A serving, or even more, should
be well tolerated. Lactose in yogurts
is better digested than the lactose in milks
Kolars et al. 1984
Gilliland and Kim 1984
Savaiano et al. 1984
Shermak et al. 1995
Pasteurized yogurts do not improve lactose
digestion. However, these products, when
consumed, produce little to no symptoms
Savaiano et al. 1984
Kolars et al. 1984
Gilliland and Kim 1984
Digestive aids Over-the-counter lactase supplement pills,
capsules, and drops may be used when
large doses of lactose (> 12 g) are
consumed at once
Moskovitz et al. 1987
Lin et al. 1993
Ramirez et al. 1994
Lactose-hydrolyzed milks are also well tolerated Nielsen et al. 1984
Biller et al. 1987
Rosado et al. 1988
Brand et al. 1991
Colon adaptation Consume lactose-containing foods daily
to increase the colon bacteria’s ability
to metabolize undigested lactose
Perman et al. 1981
Florent et al. 1985
Hertzler et al. 1996
2640 FOOD INTOLERANCE/Lactose Intolerance
sweetness, due to the presence of free glucose. Lactose
hydrolysis can be carried out by the consumer at
home, or products can be purchased already in low-
lactose form. A number of studies have evaluated the
effectiveness of these products. Doses of 3000–6000
FCC (Food Chemical Codex) units of lactase adminis-
tered just prior to milk consumption decrease both
breath hydrogen and symptom responses to lactose
loads ranging from 17 to 20 g. Thus, a fourth strategy
is to include lactose-reduced products and/or utilize
enzyme preparations if symptoms of intolerance are
present, despite adherence to simpler and more cost-
effective approaches.
Unfermented Acidophilus Milk
0029 Various strains of Lactobacillus acidophilus exist;
however strain NCFM (North Carolina Food Micro-
biology) has been most extensively studied and used
in commercial products. Unfermented acidophilus
milk tastes identical to unaltered milk since the
NCFM strain does not multiply in the product, pro-
vided that the storage temperature is below 40
F
(5
C). L. acidophilus strain NCFM is derived from
human fecal samples and contains b-galactosidase
(lactase). However unfermented acidophilus milk
does not enhance lactose digestion or reduce intoler-
ance symptoms in doses present in commercially
available products. It appears that the ingested bac-
teria are not disrupted by the bile acids, thus micro-
bial lactase is not released. However, when
acidophilus milk is sonicated, which destroys the
bacteria membrane, lactose digestion improves.
Colonic Fermentation and Bacterial Adaptation of
Lactose
0030 The colonic bacteria ferment undigested lactose and
produce short-chain fatty acids and gases. Historic-
ally, this fermentation process was viewed as a cause
of lactose-intolerance symptoms. However, it is now
recognized that the fermentation of lactose, as well as
other nonabsorbed carbohydrates plays an important
role in the health of the colon, and impacts the nutri-
tional status of the individual. The most compelling
evidence for colonic bacterial adaptation to lactose
comes from studies where the amount of lactose
is carefully controlled and gradually increased over
time. Increasing the daily lactose dose from 0.3 g kg
1
body weight up to 1.0 g kg
1
body weight over
a period of several days to 3 weeks results in a
several-fold increase in fecal b-galactosidase activity.
This elevated enzyme activity returns to baseline
levels with in a few days after the lactose-feeding
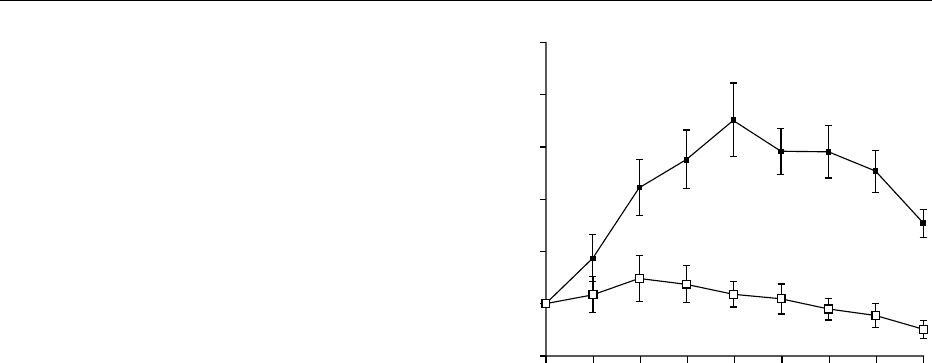
period. Furthermore, lactose feeding dramatically
decreases the breath hydrogen response to a lactose
challenge dose (Figure 1). In fact, after lactose
adaptation, the subjects may no longer appear to be
lactose maldigesters according to the breath hydrogen
test. The large doses of lactose fed during these adap-
tation periods (up to 70 g day
1
) result in only minor
symptoms. Additionally, the severity and frequency
of flatus symptoms in response to the lactose chal-
lenge dose are significantly reduced.
0031Thus it appears that colonic bacterial adaptation to
lactose does occur. Although the mechanisms that
cause colonic adaptation need further investigation,
it is clear that many lactose-intolerant individuals will
develop a tolerance to milk if they consume it regu-
larly. This may represent a simpler and less expensive
solution than the use of lactose digestive aids. Thus, a
final dietary recommendation to lactose-intolerant
individuals is not to avoid dairy foods, but rather to
include them in the diet on a daily basis. Daily con-
sumption of milk and dairy foods will enhance colon
bacterial adaptation and reduce the likelihood for
symptoms of intolerance.
Conclusion
0032Milk and milk products are important sources of
many nutrients, including calcium. The avoidance of
dairy products to prevent intolerance symptoms jeop-
ardizes bone density, thus increasing the risk for
osteoporosis. The inescapable conclusion to be
drawn from blinded studies is that virtually all
LNP subjects, including even those with severe
self-perceived intolerance, can drink milk or milk
−20
0
20
40
60
80
100
∆ Breath hydrogen (p.p.m.)
01234
Time (h)
567 8
fig0001Figure 1 Breath hydrogen response to a lactose challenge
after lactose (open squares) or dextrose (filled squares) feeding
periods. Data are the means + SEM, n ¼20. Reproduced from
Hertzler SR and Savaiano DA. Colonic adaptation to daily lactose
feeding in lactose maldigesters reduces lactose intolerance.
American Journal of Clinical Nutrition 64: 232–236, with permission.
FOOD INTOLERANCE/Lactose Intolerance 2641

products with minimal symptoms if taken in single
serving doses with meals. Thus, the role of the health
care provider is to convince the patient with self-
diagnosed or, less commonly, physician-diagnosed
lactose intolerance that various dietary strategies
effectively manage lactose intolerance by reducing
or eliminating gastrointestinal symptoms. However,
beliefs concerning lactose intolerance are not easily
reversed, and it may be very difficult to convince
patients that their abdominal symptoms are not
appreciably aggravated by ingestion of moderate
doses of lactose.
See also: Food Intolerance: Milk Allergy; Inborn Errors
of Metabolism: Overview; Lactic Acid Bacteria;
Lactose; Yogurt: The Product and its Manufacture;
Yogurt-based Products; Dietary Importance
Further Readings
Biller JA, King S, Rosenthal A and Grand RJ (1987) Effi-
cacy of lactase-treated milk for lactose-intolerant pedi-
atric patients. Journal of Pediatrics 111: 91–94.
Dehkordi N, Rao DR, Warren AP and Chawan CB (1995)
Lactose malabsorption as influenced by chocolate milk,
skim milk, sucrose, whole milk, and lactic cultures.
Journal of the American Dietary Association 95: 484–
486.
Florent C, Flourie B, Leblond A, Rautureau M, Bernier JJ
and Rambaud JC (1985) Influence of chronic lactulose
ingestion on the colonic metabolism of lactulose in man
(an in vivo study). Journal of Clinical Investment 75:
608–613.
Gilliland SE and Kim HS (1984) Effect of viable starter
culture bacteria in yogurt on lactose utilization in
humans. Journal of Dairy Science 67: 1–6.
Hertzler SR and Savaiano DA (1996) Colonic adaptation to
daily lactose feeding in lactose maldigesters reduces lac-
tose intolerance. American Journal of Clinical Nutrition
64: 232–236.
Kolars JC, Levitt MD, Aouji M and Savaiano DA (1984)
Yogurt – an autodigesting source of lactose. New Eng-
land Journal of Medicine 310: 1–3.
Lin M, Dipalma JA, Martini MC, Gross J, Harlander SK
and Savaiano DA (1993) Comparative effects of exogen-
ous lactase (B-galactosidase) preparations on in vivo
lactose digestion. Digestive Diseases and Sciences 38:
2022–2027.
Martini MC and Savaiano DA (1988) Reduced intolerance
symptoms from lactose consumed during a meal. Ameri-
can Journal of Clinical Nutrition 47: 57–60.
Moskovitz M, Curtis C and Gavaler J (1987) Does oral
enzyme replacement therapy reverse intestinal lactose
malabsorption? American Journal of Gastroenterology
82: 632–635.
Nielsen OH, Schiotz PO, Rasmussen SN and Krasilnikoff
PA (1984) Calcium absorption and acceptance of
low-lactose milk among children with primary lactase
deficiency. Journal of Pediatric Gastroenterology and
Nutrition 3: 219–223.
Perman JA, Modler S and Olson AC (1981) Role of pH in
production of hydrogen from carbohydrates by colonic
bacterial flora. Studies in vivo and in vitro. Journal of
Clinical Investment 67: 643–650.
Ramirez FC, Lee K and Graham DY (1994) All lactase
preparations are not the same: results of a prospective,
randomized, placebo-controlled trial. American Journal
of Gastroenterology 89: 566–570.
Rosado JL, Morales M, Pasquetti A, Nobara R and
Hernandez L (1988) Nutritional evaluation of a lac-
tose-hydrolyzed milk-based enteral formula diet. I. A
comparative study of carbohydrate digestion and clin-
ical tolerance. Rev Invest Clin 40: 141–147.
Savaiano DA, AbouElAnouar A, Smith DE and Levitt MD
(1984) Lactose malabsorption from yogurt, pasteurized
yogurt, sweet acidophilus milk, and cultured milk in
lactase-deficient individuals. American Journal of Clin-
ical Nutrition 40: 1219–1223.
Shermak MA, Saavedra JM, Jackson TL, Huang SS, Bayless
TM and Perman JA (1995) Effect of yogurt on symp-
toms and kinetics of hydrogen production in lactose-
malabsorbing children. American Journal of Clinical
Nutrition 62: 1003–1006.
Solomons NW, Guerrero AM and Torun B (1985) Dietary
manipulation of postprandial colonic lactose fermenta-
tion: I. Effect of solid foods in a meal. American Journal
of Clinical Nutrition 41: 199–208.
Suarez FL and Savaiano DA (1994) Lactose digestion and
tolerance in adult and elderly Asian-Americans. Ameri-
can Journal of Clinical Nutrition 59: 1021–1024.
Elimination Diets
C M Carter, Great Ormond Street Hospital for
Children, London, UK
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Definitions and Aims
0001An elimination diet is one which excludes one or
more foods or food additives. The aim of an elimin-
ation diet is to diagnose and/or treat food-allergic
disease. Food-allergic disease is an intolerance to
food(s) resulting from an abnormal immunological
response. The title ‘food allergy and intolerance’ is
often used because an immunological basis cannot
always be demonstrated. This article discusses the
indications for the use of an elimination diet and the
dietary manipulations involved.
Indications and Contraindications
0002The symptoms of food allergy or intolerance may
come on quickly or slowly (Table 1). Symptoms may
2642 FOOD INTOLERANCE/Elimination Diets
appear immediately after a very small amount of food
has been consumed and are usually associated with
immunoglobulins of the immunoglobulin E (IgE)
class. The gut, skin, and/or respiratory tract may be
involved and symptoms are listed in Table 1. Skin
symptoms include urticaria (also known as nettle
rash or hives, an itchy reaction characterized by the
appearance of raised red patches or wheals) and
angiedema (localized swelling of parts of the face,
mainly lips, eyes, and throat) The most serious reac-
tion is known as anaphylaxis, which is a state of
shock induced by antigen–antibody (mainly IgE) re-
action. It can be life-threatening unless epinephrine
(adrenaline) is administered rapidly. People who have
these very severe reactions to foods tend to be asth-
matic. First signs may be tingling of the lips, tongue,
and throat, sneezing, pallor, and feeling unwell and
light-headed. Skin rashes, angiedema, and urticaria
may or may not occur. First signs are quickly followed
by upper or lower airway obstruction, low blood
pressure, and cardiac arrhythmia.
0003 On the other hand, symptoms may come on
slowly after hours or days and only when a con-
siderable amount of the food has been consumed.
Gut, skin, and respiratory reactions are well docu-
mented and are likely to be T-cell-mediated without
IgE being involved (Table 1). However there is
some evidence for a ‘late-phase’ IgE response. Less
well-documented reactions to food include migraine,
epilepsy with migraine, attention deficit hyperactivity
disorder (ADHD), and rheumatoid arthritis. There is
much difference of opinion as to the role of
diet, although the small amount of research carried
out indicates that the idea that food is
involved should be taken seriously, but etiology is
not known.
Immediate IgE-mediated Food Allergy
0004The presence of specific IgE antibodies can be dem-
onstrated quantatively with skinprick tests (SPT) or in
the serum with radioallergosorbent tests (RAST).
Although the negative predictive accuracy of SPTs is
95%, the positive predictive accuracy is only about
50%. This means that a negative result virtually pre-
cludes the possibility of an IgE-mediated allergic
reaction, while a positive result indicates an allergic
person, but an elimination diet cannot be based on
the results of these tests. RAST tests are no more
accurate.
0005However, people (or parents of children) who have
immediate reactions to foods usually have no doubt
as to the problem food and will need to avoid it.
Those who have severe or anaphylactic reactions to
food will need to avoid even the smallest trace and
this is difficult to do in practice. Any food may be a
trigger but the most common provoking foods are
peanut, tree nut, milk, egg, wheat, soya, fish, and
shellfish. Such elimination diets are hard to achieve
for the following reasons:
tbl0001 Table 1 Symptoms of food allergy and intolerance
Part of body involved Usually IgE-mediated Probably non-IgE-mediated
Immediate onset Delayed onset
Within 2 h Within a few hours to 3 days
After small amount of food After larger amount of food
Gut Swelling of lips, mouth Reflux vomiting
Oral allergy syndrome Abdominal pain, bloating
Vomiting Small-bowel enteropathy
Colic Failure to thrive
Allergic colitis, rectal bleeding
Diarrhea
Constipation
Skin Urticaria Eczema
Angiedema Urticaria (rarely)
Skin rashes
Lung Cough/wheeze/sneeze Asthma
Laryngeal edema
Bronchospasm
Systemic Cardiac arrhythmia
Hypotension
Anaphylaxis
Controversial Migraine
Migraine with epilepsy
Attention deficit hyperactivity disorder
Rheumatoid arthrititis
IgE, immunoglobulin E.
FOOD INTOLERANCE/Elimination Diets 2643

1.0006 Problems with manufactured food labeling. In
Europe and other parts of the world (except the
USA and Canada) there is a ‘25% rule’ which
means that if a product has a compound ingredient
which forms less than 25% of the finished prod-
uct, its ingredients do not have to be declared. For
example, the ingredients of salami on a pizza
would not have to be declared. Many food manu-
facturers are disregarding this rule for peanuts and
tree nuts and it is to be hoped that this will happen
for milk and wheat also. Another aspect of food
labeling involves the use of many terms for one
food item. Table 2 shows the many different terms
which denote the presence of milk.
2.
0007 Factory contamination. Many manufactured
foods are not produced on designated lines so
there is the possibility of food being contaminated
from a previous run or other factory contamin-
ation. For this reason most chocolate in the UK
and many other manufactured foods carry a ‘may
contain nuts’ label. This precludes a large array
of manufactured food for peanut- and tree nut-
allergic people.
3.
0008 Eating out. Although attempts are being made to
educate the catering industry, there are reports of
people eating in restaurants or purchasing take-
aways being told food was free of the requested
items when it was not. There is the possibility of
contamination when eating out (or at home)
when, for example, a sandwich for a nut-allergic
person may be made with an unwashed knife
which was previously used for a peanut-butter
sandwich. Alternatively a serving spoon could be
contaminated with food dished up previously.
Cross-contact may also occur through shared
grilling surfaces, food containers, and frying oil.
0009Children often grow out of allergies to milk, egg,
soya, and wheat but this is much less likely for aller-
gies to peanuts, tree nuts, and fish. Although SPTs
may give an indication, the only way to know if an
allergy has been outgrown is to perform a food chal-
lenge. For people who are at risk of severe reactions
challenges are performed in hospital where graded
doses of food are given over several hours and resusci-
tation equipment is available.
Delayed-onset Food Allergy or Intolerance
0010In the case of delayed reactions to foods, it is much
less likely that people know which foods are upsetting
them. Indeed, problems with foods which are eaten at
nearly every meal such as wheat and milk tend to
go completely unnoticed. SPTs and RAST tests are
not helpful. Claims of alternative diagnostic tests
have not been validated. Although the small-bowel
biopsy can be a useful tool in the diagnosis of gastro-
intestinal disease, it does not indicate which foods are
the problem.
0011The elimination diet is therefore the only available
‘diagnostic’ tool for suspected delayed-onset food al-
lergy or intolerance. The severity of symptoms should
be taken into account before deciding whether or not
to embark on an elimination diet. For example, it is
inappropriate to use such a diet for eczema unless the
child has failed to respond to the optimum skin treat-
ment and the eczema is severe enough to warrant diet
intervention. Diets can be socially disruptive and
nutritionally inadequate unless supervised properly
and may cause more problems than the disease it is
intended to treat. However, if symptoms are severe
and foods are suspected as being implicated (although
this is not a prerequisite), a ‘diagnostic’ elimination
diet is indicated. In the case of severe symptoms, it is
important that other more serious disease has been
ruled out before embarking on the diet approach.
Elimination Diet Strategy
0012Diagnosis of food allergy/intolerance by elimination
diet involves several phases. The first is an appro-
priate elimination diet which, if successful, results
in relief of some or all the symptoms. The second
phase involves sequential reintroduction of foods to
identify those foods that cause problems, and a third
phase is the final maintenance diet excluding all foods
that were demonstrated to have caused problems on
open introduction.
0013Phase 1: elimination diet This may be a diet exclud-
ing only one or two foods, a diet omitting a large
tbl0002 Table 2 Words denoting milk used in ingredient lists on
manufactured food labels
Nonfat milk solids
Skimmed milk powder
Casein
Whey
Cheese
Cream
Yogurt
Butter
Ghee
Butterfat
Buttermilk
Caseinates
Dry milk solids
Lactose
Hydrolyzed milk protein
Rennet casein
Sour cream
Whey protein concentrate
2644 FOOD INTOLERANCE/Elimination Diets

number of foods, or even a diet consisting of a
hypoallergenic formula only.
0014 The empirical exclusion diet An empirical diet is
used where food allergy/intolerance is suspected,
causative agents are not known, and one or several
of the most commonly provoking foods are avoided.
Studies with children who have delayed reactions to
food indicate anecdotally that the most common pro-
voking foods are similar to those listed for immediate
reactions to foods, except that intolerance to some
food additives and chocolate appears more common
and intolerance to fish and nuts less common.
0015 In under 1-year-olds the most frequent offender is
cows’ milk-based infant formula, so a cows’ milk-free
diet is often used. Diet avoiding egg and milk together
with any known problem foods is sometimes used for
eczema. It is not unusual for pediatric gastroenterol-
gists to use a diet free of milk, egg, wheat, rye, and
possibly soya for children with gastrointestinal symp-
toms. Several adult centers use a diet free of all grains
(someinclude rice),egg, milk, chocolate, and additives.
This is sometimes known as a ‘hunter gatherer’ diet.
0016 The empirical diet may be followed for up to 6
weeks before a decision is made as to whether it has
helped or not. Unhelpful diets must be abandoned.
0017 Problems occur with empirical diets when excluded
foods are inadvertently replaced by others which are
equally capable of causing adverse reactions. For
example, a child on a milk-free diet may drink soya
milk or orange juice instead and it is possible to be
equally intolerant to these foods. Failure to respond
to an empirical diet does not rule out the possibility of
food intolerance. More restricted diets therefore have
a role to play.
0018Few-foods diet There are considerable difficulties in
teaching people how to avoid a large number of
foods. For very restricted diets it is easier to decide
on which foods the child can eat and teach the diet in
terms of which foods are allowed rather than concen-
trating on those that are forbidden. This is the basis
for the few-foods diet and 3–4 weeks is the longest
time one should consider using a very restricted diet,
although improvement may occur in a shorter time.
0019The few-foods diet may consist of no more than 5–
10 foods, all of which are least likely to cause prob-
lems. Different people working in this field have
achieved this in several ways. The simplest few-
foods diet consists of lamb, pears, and spring water
only. Although an adult may manage this, a child
would have great difficulty. Diets using one meat,
one carbohydrate source, one fruit, and one vegetable
have been used. If no improvement occurs, a second
diet containing a different set of foods can be used.
This is an ideal diet in theory but, because of compli-
ance problems, especially in children, it is not uncom-
mon to double up and allow two meats, two
carbohydrate sources, etc. (Table 3). The diet should
be individualized to some extent in that it cannot
tbl0003 Table 3 Few-foods diet and modifications
Few-foods diet Possible variationsand/oradditions
Meats Turkey, lamb Pork, chicken, rabbit
Starches Rice, potato Sweet potato, corn/maize
Vegetables Two from:1. Brassica
2. Carrot, parsnip
3. Cucumber, marrow, courgette
4. Onion, leek, asparagus
5. Swede, turnip
All vegetables except tomato
Include pulses
Fruit Two from:1. Peaches and apricots
2. Pears
3. Pineapple
4. Melon
5. Grapes
Allow all fruits listed on the left
Drinks Tap/bottled water Hypoallergenic formula for under 2s
Juice from allowed fruits
Miscellaneous Sunflower or olive oil Spices
Whey-free margarine
Small amount of sugar
Jam from allowed fruits
Salt, herbs
Vitamin/mineral supplements Not essential in short term
May be needed in the long term
Rice can be given as Thai rice noodles, puffed rice cakes, homemade rice cookies, rice ‘drink,’ boiled and fried rice, and risotto. Potatoes can be
prepared in many ways, including plain crisps/chips.
FOOD INTOLERANCE/Elimination Diets 2645

include known problem foods, disliked foods, or
foods which are craved and usually eaten in large
amounts. Table 3 gives ideas for variations or slightly
enlarging the diet to make it more practical. Allergy/
intolerance can occur with any food and the few-
foods diet is really a ‘guesswork’ diet using those
foods least likely to be implicated.
0020 The few-foods diet can be difficult to follow and
should only be adopted if symptoms are frequent and
severe. The diet should be carefully taught and the
patient given ideas for menus and packed lunches and
provided with recipes for cooking with the foods
allowed. Close professional support is essential.
0021 Hypoallergenic formula only For such a diet, the
only food allowed is a nutritionally complete formula
which has no intact protein, the protein source being
supplied by either peptides derived from hydrolyzed
protein or synthetic amino acids. Such formulas are
available for infants and children and adults.
0022 This may be the first choice of diet for the infant
but it is very much a last resort for children and adults
and it probably means tube feeding (these products
do not have a good taste).
0023 Phase 2: reintroduction of foods If the elimination
diet has resulted in a worthwhile improvement, foods
are reintroduced sequentially in an effort to identify
provoking foods. If the effect of the diet is unclear or
if there is no improvement it should be abandoned or
another type of elimination diet tried. New foods
should be given in normal amounts for a week before
they are incorporated into the diet. During the period
of reintroduction, which may take months, the nutri-
tional adequacy of the diet must be monitored. Vita-
min and/or mineral supplements may be required. If
staple foods must be avoided, e.g., milk and wheat,
alternatives should be found.
0024 If there is a risk of a severe immediate reaction to a
food, it should either be avoided or reintroduced in
hospital as described. Some children with multiple
symptoms and multiple food intolerances have imme-
diate reactions to some foods and delayed reactions to
others.
0025 Some people’s symptoms are triggered by inhaled
substances, e.g., house dust mite, or by contact with
substances, e.g., grass as well as food. It can some-
times be difficult during the reintroduction phase to
know whether an adverse reaction is due to a food or
other allergens in the environment.
0026 Phase 3: maintenance diet Once all foods (and addi-
tives) have been introduced and those foods causing
problems avoided, the patient has arrived at a main-
tenance diet which will need to be adhered to.
0027Children have a tendency to grow out of their
problems so the possibility of reintroducing avoided
foods should be discussed every 6 months to a year.
This may happen in an unsupervised way as a result
of an accidental or a deliberate break in the diet.
0028If the maintenance diet excludes many foods it may
be necessary to compromise. During the introduction
phase some foods have an adverse effect after normal
amounts are consumed regularly over several days. It
may be possible to allow these foods from time to
time with no adverse effect.
Outcome Assessment
0029It is extremely helpful for patients (or parents) to keep
a daily symptom score diary beginning at least 1 week
before the diet starts and continuing during the open
reintroduction of foods. It can report on severity of
symptoms, dietary indiscretions, and other factors
that may be relevant. Diet manipulation is a very
crude form of diagnosis and a diary may make it
more objective.
Formulas for Infants with Cows’ Milk
Allergy
0030The infant who is not breast-fed and who is allergic to
the usual infant formulas which are based on cows’
milk protein will require an alternative.
0031Formulas based on whole soya protein isolate have
been available for many years. Infants with immedi-
ate IgE-mediated allergies often do well on these for-
mulas, although about 15% will be allergic to soya
also. Infants with gastoenteropathic symptoms are
much more likely to be intolerant of soya and these
formulas should not be used.
0032As previously mentioned, there are several infant
formulas available where the protein has been exten-
sively hydrolyzed to form small peptides. These for-
mulas are usually tolerated by cows’ milk-allergic
infants but a few highly allergic ones cannot manage
these either. A formula where the protein consists of
pure synthetic amino acids is most useful in these
circumstances.
Proof by Blind Food Challenge
0033Since diet treatment may have a powerful placebo
effect, the only way to prove that there is a physical
rather than purely psychological basis for the im-
provement on diet is to administer the foods ‘blind’,
i.e., when the subject is unaware that he or she is
consuming it. This is achieved by offering the chal-
lenge food hidden in other food known to be toler-
ated. On a second occasion, in random order with the
2646 FOOD INTOLERANCE/Elimination Diets

first, material is given which looks and tastes like the
challenge but does not contain challenge material.
When the observer is also blind to the order of ad-
ministration the procedure is known as a double-
blind placebo-controlled food challenge (DBPCFC).
This is regarded as the ‘gold standard’ for proof of
food allergy or intolerance.
0034 The DBPCFC has been used in many research stud-
ies. Over the last 25 years or so, American workers
have used the DBPCFC as an integral part of investi-
gations into immediate allergic reactions to food.
Researchers used incremental doses of food over 2–
5 h so that placebo and challenge could be completed
in one day. They have been recommended as a diag-
nostic tool outside the research area but are very little
used in the UK.
0035 The DBPCFC has also been used to investigate
more controversial slow-onset reactions to foods
such as ADHD. However, open reintroductions of
foods into an apparently successful elimination diet
tend to reveal that many people relapse after several
days of eating normal amounts of food. This makes a
DBPCFC much more difficult to design. One would
need to provide challenge and placebo material for a
week each with a 2-week washout period in between.
This has to be organized on an individual basis and
the following crititeria must be fulfilled:
1.
0036 Enough of the provoking food must be given for a
sufficient length of time. The amount will have
been established during open reintroduction.
2.
0037 The challenge food must be disguised in food
known to be tolerated in the amount to be given.
3.
0038 The two must be indistinguishable from one
another.
4.
0039 For children in particular, the material must be
acceptable in taste and quantity.
5.
0040 The challenge food should be provided in the same
form as that which caused symptoms on open
reintroduction. For example, dried powdered
milk may not have the same effect on a subject as
fresh pasteurized milk.
Although DBPCFCs may be an essential part of re-
search, they are rarely performed in clinical practice.
For the more controversial areas of food allergy or
intolerance they are time-consuming and difficult to
design. They are perhaps best reserved for those cases
in which there are serious doubts about the diagnosis.
Elimination Diets for Prevention of Food
Allergy
0041 There is much interest in the possibility of preventing
the onset of allergies in babies born into allergic fam-
ilies (sibling or parent with allergic disease). Results
of research studies are not clear-cut but some tenta-
tive guidelines may be drawn.
Diet During Pregnancy
0042Although research is ongoing in this field there is not
enough evidence to suggest that women who are
expecting ‘at-risk’ infants should alter their diets
during pregnancy.
Diet of the Mother During Lactation
0043There is little evidence to suggest that the diet of the
mother during lactation has any effect in the long
term on her child. However, there is some evidence
that in the short term this may be helpful. Indeed,
some highly allergic breast-fed children develop aller-
gic symptoms which can be controlled if their mother
avoids certain foods. For mothers who wish to do so,
a milk- and egg-free diet could be followed, provided
the mother has professional support and will need at
least a calcium supplement.
Careful Weaning of the Potentially Allergic Child
0044Breast-feeding should be encouraged for all children.
The ‘at-risk’ infant should have nothing but breast
milk for at least the first 4–6 months. If breast milk is
not available the best alternative is probably an infant
formula where the protein has been highly hydro-
lyzed. It is not known whether soya formula has a
protective effect. It would seem prudent to begin the
weaning process with pure baby rice, vegetables,
fruits, and meats, and wait until nearer 1 year old to
introduce milk, egg, and wheat. There are no specific
guidelines on this. Introduction of nuts should be
delayed until at least 3 years.
Conclusion
0045Elimination diets can be expensive, are socially dis-
ruptive, and run the risk of being nutritionally inad-
equate. They should be reserved for individuals with
troublesome symptoms who have not responded to
symptomatic treatment. The ideal place for this type
of treatment is in specialized clinics with interested
doctors and dietitians who have the necessary expert-
ise. Immediate reactions to foods can occasionally be
very severe or even life-threatening so very careful
advice must be given. Despite all these problems,
elimination diets can be of great benefit to many
people.
See also: Allergens; Food Additives: Safety; Food
Intolerance: Types; Food Allergies; Milk Allergy; Lactose
Intolerance; Infant Foods: Milk Formulas; Migraine and
Diet
FOOD INTOLERANCE/Elimination Diets 2647
