Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 55 LIGHTNING AND ELECTRICAL INJURIES388
lightning flash and the thunderclap in seconds divided by five is the distance in miles.
Further, you shouldn’t resume outdoor activities until at least 30 minutes after the last flash
of lightning is seen and the last clap of thunder is heard. “If you see it, flee it; if you hear it,
clear it.”
25. I want to appear as if I read this whole chapter. Is there one number to
memorize that will impress my friends and colleagues?
Sure, try 70%:
n
Thunderstorms that happen between noon and 6 pm: approximately 70%
n
Thunderstorms that happen in June, July, or August: 70% (June, 21%; July, 30%;
August, 22%)
n
Lightning victims who survive: approximately 70% (although this may be as high
as 90%)
n
Survivors with sequelae: approximately 70%
n
Singular victims: approximately 70% (fatal singular victims as high as 91%; victims in
couples, 15%; victims in groups of three or more, 15%)
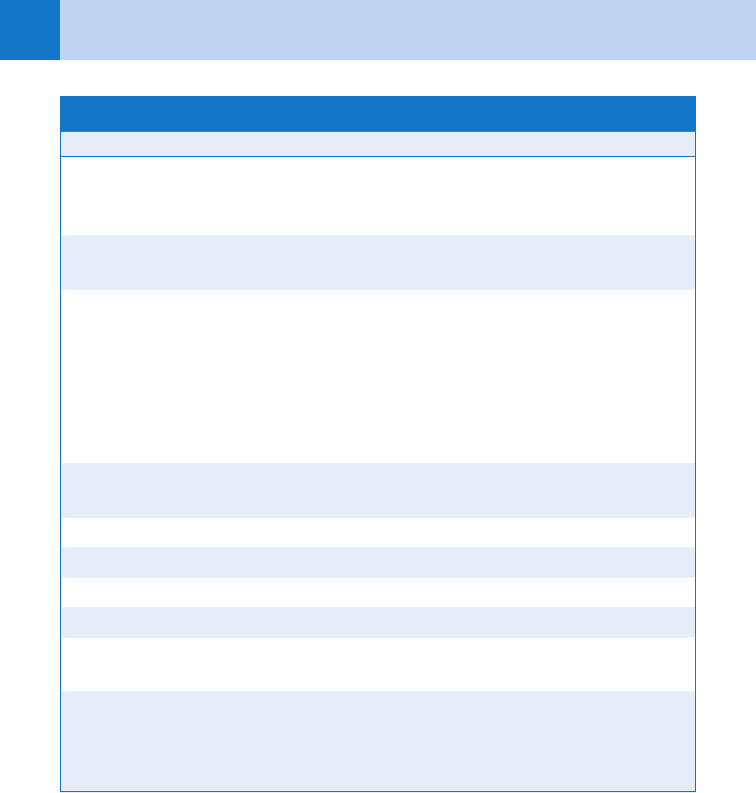
TABLE 55-3. LIGHTNING INJURIES BY ORGAN SYSTEM
System Injury
Cardiac Asystole, ventricular fibrillation (usually from hypoxia), nonspecific dysrhyth-
mias, myocardial stunning, nonspecific ST-T changes, ST elevation, T wave
inversion, hypertension, tachycardia, acute myocardial infarction (rare)
Respiratory Apnea from inhibition of the brainstem respiratory centers, hypoxia, pulmo-
nary contusions and hemorrhage, hemothorax, pneumothorax
Nervous Loss of consciousness, coma, transient aphasia, confusion, disorientation,
amnesia, autonomic dysfunction (with loss of pupillary function), coagulation
of brain substance, epidural and subdural hematomas, intraventricular
hemorrhage, skull fractures, seizures, transient or permanent paralysis,
EEG abnormalities, extrapyramidal symptoms, sensory disturbances, SIADH,
cerebral edema, ataxia, vertigo, cerebral artery thrombosis, spinal atrophic
paralysis, headaches
Psychiatric Hysteria, phobias, psychosis, depression, posttraumatic stress disorder,
“storm apprehension,” memory impairment, personality changes
Skin Feathering, linear burns, punctate burns, true thermal burns
Musculoskeletal Dislocations, fractures, muscle necrosis (rare)
Renal Myoglobinuria (rare)
Gastrointestinal Gastric atony, ileus, perforations (uncommon)
Ophthalmologic Mydriasis, loss of light reflex, anisocoria, Horner’s syndrome, cataracts
(in 20% of victims within 3 years)
Otologic Tinnitus, hearing loss, ruptured tympanic membranes
EEG, electroencephalographic; SIADH, syndrome of inappropriate antidiuretic hormone.
Chapter 55 LIGHTNING AND ELECTRICAL INJURIES 389
ELECTRICAL INJURIES
26. What are the basic physics of electricity?
Electricity is simply the flow of electrons. The electromotive force moving those electrons
from high concentration to low concentration is voltage (V). The number of electrons flowing
is known as current or amperage (I). Resistance to the electron flow (R) is a property of the
medium through which they pass, measured in ohms (O). These three factors are related as
shown in Ohm’s law: I 5 V/R.
27. What factors determine nature and severity of the injury seen in electrical
accidents?
The most harmful effects of electricity on the body are thermal. The heat generated is related
to the current, tissue resistance, and duration of contact:
Heat 5 (amperage)
2
3 resistance 3 time
Because amperage is squared, it contributes the most to tissue injury. However, in real
accidents, the amperage is often unknown. Therefore, we use voltage as an approximate
indicator because high voltages are usually associated with high amperages. Voltages are
classified as:
n
High 5 1000 volts or more
n
Low 5 less than 1000 volts
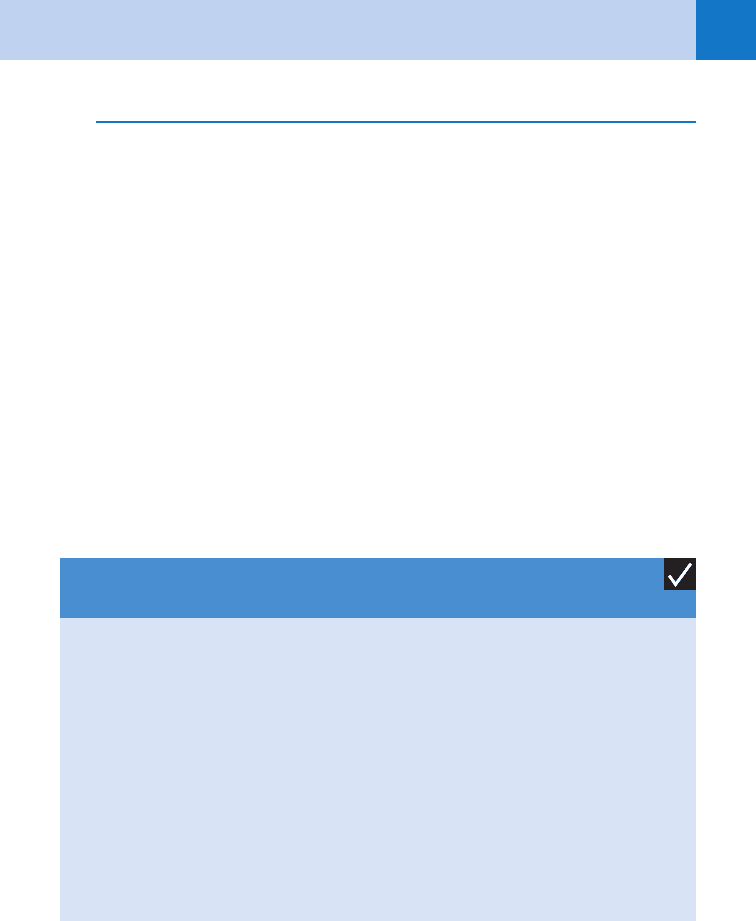
KEY POINTS: DIFFERENCES IN LIGHTNING AND HIGH-VOLTAGE
ELECTRICAL INJURIES
1. Duration: Instantaneous (lightning) versus prolonged contact (electrical)
2. Energy: 1 billion volts (lightning) versus 1,000 to 10,000 volts (electrical)
3. Current: DC (lightning) versus AC (electrical)
4. Shock wave: Present in thunder (lightning) versus absent (electrical)
5. Flashover: Present (lightning) versus absent (electrical)
6. Cardiac effect: Asystole (lightning) versus ventricular fibrillation (electrical)
7. Burns: Minor and superficial (lightning) versus deep (may appear benign or superficial)
(electrical)
8. Urinary failure: Rare (lightning) versus myoglobinuric (electrical)
9. Fasciotomy: Rarely indicated (lightning) versus common and early (electrical)
28. What is the epidemiology of electrical injuries?
There are about 800 to 1000 injuries from high-voltage electricity per year in the United States.
Between 3% and 4% of burn center admissions are for electric burns. Serious electrical burns
carry a 40% mortality. Electrical injuries follow a bimodal age distribution with a peak in
children younger than 6 years and another peak around age 20. The first peak represents
children exploring electrical cords, wall sockets, or extension cord outlets. This second peak
represents occupational accidents (one third of them are electric workers, and one third are
construction workers). In fact, electrocution is the fifth leading cause of occupational death.
See Table 55-4.
Chapter 55 LIGHTNING AND ELECTRICAL INJURIES390
29. What are some prehospital considerations in the treatment of electrical
injuries?
Scene safety for the rescuers is the first priority. Rescuers should not become victims—even
if that means taking time to turn off the power source before approaching a victim. The
essentials of resuscitation are the ABCs (airway, breathing, circulation). It is prudent to
assume traumatic injuries and immobilize the spine. Cardiac dysrhythmias are treated in the
standard manner. Two large-bore intravenous (IV) catheters should be established, and
aggressive fluid replacement should be started.
30. How is tissue resistance related to injury?
Nerves offer the least resistance and, therefore, allow the deepest penetration but the least
heat injury. Blood vessels have the next most resistance, then mucous membranes, muscle,
skin, tendon, and fat. The tissue with the greatest resistance is bone. Because of its high
resistance, it suffers the greatest heat injury but the least penetration.
Interestingly, the resistance of skin can be highly variable, depending on its thickness,
vascularity, and degree of hydration. The thick, dry skin of callused feet and hands is much
more resistant (100,000 ohms) than thin, wet skin (2,500 ohms). Immersion in water
further drops skin resistance to 1,500 ohms. When high-resistance skin is injured by
electricity, the heat produces burns. As the skin chars, it loses resistance and allows for
greater penetration.
31. Which organ systems can be damaged by electrical injury?
See Table 55-5.
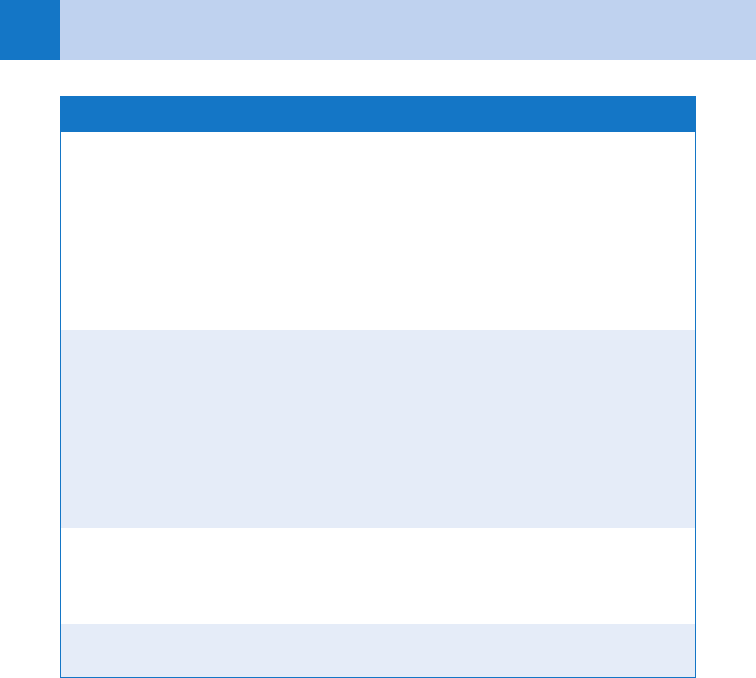
TABLE 55-4. ELECTRICITY GLOSSARY
Threshold for Sensation In contradistinction to DC, in which there is an unchanging direction
of current flow, AC is an electric source that changes its direction of
current flow as a particular frequency. Human tissues, particularly
muscles, respond well to AC frequencies between 40 and 150 Hz
(cycles per second). In the United States, homes are supplied with
exactly that: household current is 60 Hz, 110 to 120 volts. The
threshold for sensation is the minimum current that is perceptible,
about 1 to 4 mA.
“Let Go” Threshold “Let go” threshold is the current below which an individual can re-
lease their grip on the electricity source. The average child has a “let
go” threshold of approximately 3 to 5 mA. The average adult has a
“let go” threshold of approximately 6 to 9 mA. Between 8 and 22
mA, AC can cause tetanic muscle contractions to the degree that
one may not be able to let go of the electric source. The resulting
phenomenon is dangerous because it prolongs the time of contact,
thus producing more injury.
Ventricular Fibrillation
Threshold
This is the current at which ventricular fibrillation can be induced.
The ventricular fibrillation threshold (50–100 mA) is not much
higher than the “let go” threshold.
AC, alternating current; DC, direct current.
Chapter 55 LIGHTNING AND ELECTRICAL INJURIES 391
TABLE 55-5. ORGANS DAMAGED BY ELECTRICAL INJURY
System Injury
Skin Thermal burns such as entrance and exit wounds (typically in AC
burns, the entrance and exit burns look similar; in DC burns, the
entrance is smaller than the exit), flexor crease burns, mouth
commissure burns (risk of delayed bleeding from labial artery when
the eschar separates)
Cardiac (the most
frequent causes of
immediate death from
electrical injury)
Cardiac arrest from asystole (DC) or ventricular fibrillation (AC), atrial
and ventricular ectopy, atrial fibrillation, first-degree and second-degree
heart blocks, bundle-branch blocks, and QT interval prolongation,
nonspecific ST-changes (common), acute myocardial infarction (rare)
Vascular Hemorrhage, arterial and venous thrombosis, ischemia, progressive
necrosis (from “skip” lesions in which the current, presumably, skips
from traveling within the blood column to traveling within the wall of
the vessel)
Nervous CNS or peripheral; immediate or delayed, loss of consciousness,
amnesia, confusion, disorientation, concentration and memory
problems, apnea or respiratory depression, seizures, paralysis,
paresthesias, motor nerves more commonly injured than sensory,
poor rate of recovery
Musculoskeletal Muscular pain, muscle necrosis (rhabdomyolysis), compartment
syndrome, tendon rupture, dislocations (one of the few mechanisms
for posterior shoulder dislocations), fractures, “electroporation”
or the formation of cell membrane pores in bone, aseptic necrosis,
periosteal burns, “bone pearls” (osteo schisis)
Respiratory Inhibition of the brainstem respiratory centers
Gastrointestinal Hollow visceral and solid visceral injury (both rare), stress ulcers
Renal Acute tubular necrosis (from rhabdomyolysis and myoglobinuria),
renal failure, hyperkalemia, hypocalcemia, hyperglycemia, acidosis
Ophthalmologic Cataracts (6–24 months after the incident), corneal burns, intraocular
hemorrhage and thrombosis, retinal edema, retinal detachment,
uveitis, optic nerve atrophy
Pregnancy Spontaneous abortion (fetal death rate is 73%), oligohydramnios,
IUGR (amniotic fluid and fetal tissues conduct 200 times more than
dry, intact adult skin)
AC, alternating current; CNS, central nervous system; DC, direct current; IUGR, intrauterine growth retardation.
Chapter 55 LIGHTNING AND ELECTRICAL INJURIES392
32. My patient is a 24-year-old, 75-kg man who was working on a high-voltage line
when he received a shock. He has a burn on his palm where it contacted a
wire and another burn on his knee where it was in contact with a ladder.
These two burns together are about 2% of his total body surface area (TBSA).
How much IV fluid should he receive?
Traditional burn formulas for calculating volume repletion, such as the Parkland formula
(4 mL 3 weight in kg 3 %BSA), are not applicable to electrical injuries because the surface
damage does not reflect the degree of deeper tissue damage. The surface burn is just the “tip
of the iceberg.” For this reason, electrical injuries correlate more with crush injuries than they
do with thermal burns. IV fluids should be administered at a rate to ensure a urine output of
1 to 2 mL/kg/h (for this patient 75–150 mL of urine per hour). The objective of early,
aggressive fluid resuscitation is to prevent renal failure secondary to rhabdomyolysis.
33. When should I include a computed tomography (CT) of the brain in my work-up?
A brain CT scan should be considered as part of the diagnostic procedure in every case of high-
voltage electrical injury presenting with signs of central nervous system (CNS) involvement
during or after the event. Due to the low resistance of neural tissue, subarachnoid hemorrhage
needs to be ruled out, as well as other sources of traumatic intracranial hemorrhage.
34. True or false: One should treat high-voltage electrical victims as one would
lightning victims?
False. Lightning and high-voltage electrical injuries can have very different effects and require
different treatment approaches. For example, high-voltage injuries often produce deep burns
that may require fluid resuscitation and even fasciotomy. These victims often have renal failure
from myoglobinuria. If they are in cardiac arrest, it is often ventricular fibrillation. In contrast,
lightning victims rarely have deep burns that need fluid resuscitation and fasciotomy. Their
kidneys are rarely affected. If the lightning strike victim is in cardiac arrest, it is typically
asystole (unless he or she is also hypoxic).
35. What medications should I consider using for lightning and electrical injuries?
There are no specific pharmacotherapeutics for lightning injuries. Patients with electrical
injuries and rhabdomyolysis with myoglobinuria may benefit from forced diuresis with
mannitol or furosemide. Consideration should also be given to the use of sodium bicarbonate
for urine alkinalization because this may increase myoglobin clearance. Finally, nonsteroidal
anti-inflammatory agents have been shown to be effective in treating electrical injuries and
may be indicated in lightning injuries as well (although this has not been studied).
36. What should be the disposition of lightning and electrical victims?
All patients with cardiac abnormalities (including abnormal electrocardiograms [ECGs]),
neurologic findings, or significant burns require hospital admission. Current guidelines
recommend 24-hour telemetry monitoring for all patients with high-voltage injuries and for
patients with low-voltage injuries who have an abnormal initial ECG. The American Burn
Association burn unit referral criteria include any electrical burns and lightning injuries.
Patients with associated trauma or burns may need admission, depending on the extent of the
injury. All others may be discharged. It is prudent to arrange for ophthalmology follow-up in 6
months and otolaryngology and psychiatry follow-up, as needed.
37. What about children who get injured by a household electrical cord or
appliance?
In contrast to adults who typically sustain electrical injuries in the workplace, children often
sustain electrical injuries in the home; these injuries are usually associated with electrical
cords (60%–70%) and wall outlets (15%–20%). Healthy children exposed to common
household currents (120–240V) without any water contact, who are asymptomatic at ED
presentation and without a ventricular dysrhythmia or cardiac arrest in the field, are at very
low risk for developing cardiac dysrhythmias. Patients with a normal initial ECG do not
Chapter 55 LIGHTNING AND ELECTRICAL INJURIES 393
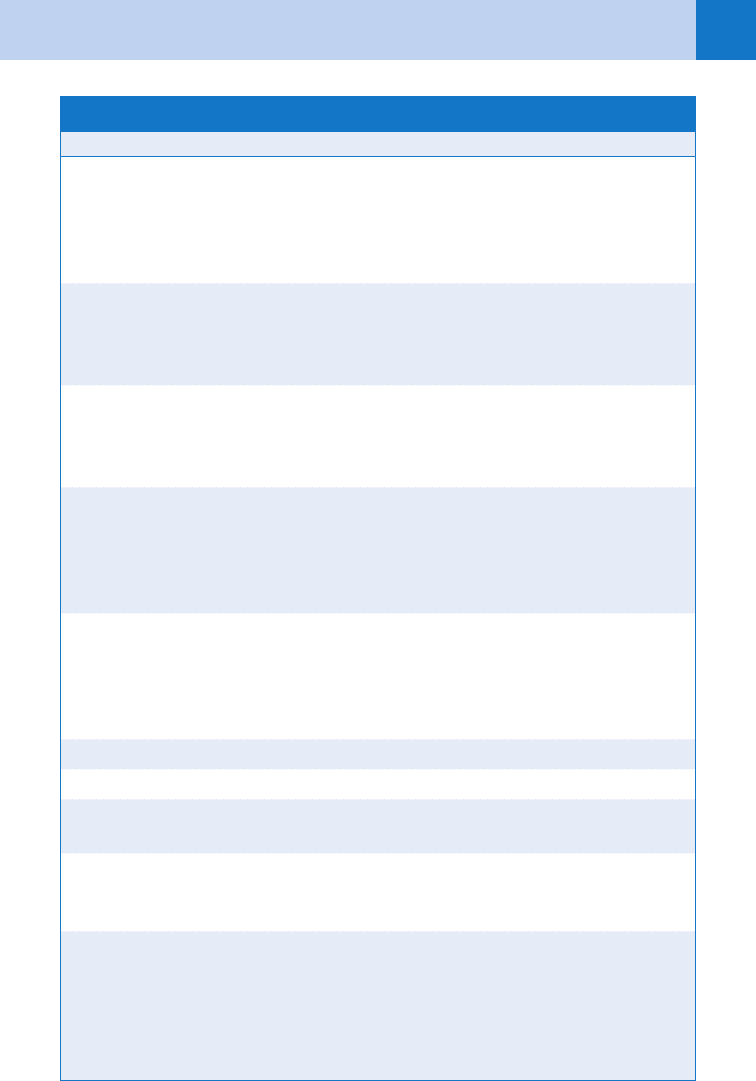
Table 55-6. CRITERIA FOR ADMISSION AND DISCHARGE
Admit (Consider Burn or Trauma Center) Discharge*
Major burns, circumferential burns, significant
hand burns
Patients requiring CPR
High voltage, especially transthoracic path
Abnormal ECG, dysrhythmias
Loss of consciousness
Neurologic abnormalities
Hypoxia, myoglobinuria
Mouth commissure burns (because of problems
with feeding and bleeding from the labial artery)
OB consultation is recommended for all
pregnant patients
Asymptomatic low-voltage injury
No ECG findings
No significant burns
*Ophthalmology follow-up in 6 months
*ENT, psychiatry follow-up as needed
CPR, cardiopulmonary resuscitation; ECG, electrocardiogram; ENT, ear, nose, and throat; OB, obstetric.
*If discharged, these follow-up arrangements should be provided.
develop late dysrhythmias. Those with nonfatal dysrhythmias or nonspecific ECG
abnormalities typically resolve spontaneously within 24 hours. As such, literature supports
safely discharging these patients without an initial ECG evaluation or inpatient cardiac
monitoring after a common household current exposure.
KEY POINTS: LIGHTNING AND ELECTRICAL INJURIES
1. Rescuers should not become victims.
2. Assume the presence of occult trauma and remember the tip of the iceberg phenomenon.
3. Typically, only high-voltage electric victims need aggressive hydration.
4. Lightning MCI priority goes to the dead, (i.e., reverse triage).
38. Who gets admitted, and who goes home?
See Table 55-6.
WEBSITES
American Burn Association: www.ameriburn.org/
Lightning Injury Research Program: www.uic.edu/labs/lightninginjury/
Lightning and Atmospheric Electricity Research at GHCC: http://thunder.msfc.nasa.gov/primer/
National Lightning Safety Institute: www.lightningsafety.com/
Chapter 55 LIGHTNING AND ELECTRICAL INJURIES394
BIBLIOGRAPHY
1. Adekoya N, Nolte KB: Struck by lightning deaths in the United States. J Environ Health 67:45–50, 2005.
2. Arnoldo BD, Purdue GF, Kowalske K, et al: Electrical injuries: a 20-year review. J Burn Care Rehabil 25:479–
784, 2004.
3. Chen EH, Sareen A: Do children require ECG evaluation and inpatient telemetry after household electrical
exposures? Ann Emerg Med 49(1):64–67, 2007.
4. Domart Y, Garet E: Lichtenburg figures due to a lightning strike. N Engl J Med 343:1536, 2000.
5. Duff K, McCaffrey RJ: Electrical injury and lightning injury: a review of their mechanisms and
neuropsychological, psychiatric, and neurological sequelae. Neuropsychol Rev 11:101–116, 2001.
6. Espaillat A, Janigian R Jr, To K: Cataracts, bilateral macular holes, and rhegmatogenous retinal detachment
induced by lightning. Am J Ophthalmol 127:216–217, 1999.
7. Fish RM: Electric injury. Part I: treatment priorities, subtle diagnostic factors, and burns. J Emerg Med
17:977–983, 1999.
8. Liao W, Lin J: High-Voltage Electrical Brain Injury. J Trauma 64(3):843–845, 2008.
9. O’Keefe Gatewood M, Zane RD: Lightning injuries. Emerg Med Clin North Am 22:369–374, 2004.
10. Pham TN, Gibran NS: Thermal and electrical injuries. Surg Clin North Am 87:185–206, 2007.
11. Rivera J, Romera KA: Severe stunned myocardium after lightning strike. Crit Care Med 35:280–285, 2007.
12. Zafren K, Durrer B, Herry JP, et al. Lightning injuries; prevention and on-site treatment in mountains and
remote areas. Resuscitation 65:369–372, 2005.
13. Zimmermann C, Cooper MA, Holle RL: Lightning safety guidelines. Ann Emerg Med 39:660–664, 2002.
ACKNOWLEDGMENT
The editors gratefully acknowledge the contributions of Lee W. Shockley, MD, author of this chapter
in the previous edition.
395
SUBMERSION INCIDENTS
CHAPTER 56
Jedd Roe, MD, MBA, FACEP
1. Define terms associated with submersion accidents.
Traditional nomenclature applied to submersion incidents has included the following:
n
Drowning is death by suffocation from submersion in liquid.
n
Near-drowning is survival (at least temporarily) after a submersion event.
n
Immersion syndrome is sudden death after submersion in very cold water, probably
secondary to vagal nerve mediated asystolic cardiac arrest.
n
Wet drownings are those in which aspiration of water occurred during the event; 80% to
90% of drownings are classified as wet drownings.
n
Dry drownings are those in which asphyxia is caused by laryngospasm without aspiration.
In an effort to simplify classification, the use of the term submersion incident has been
adopted to encompass any adverse event sustained by a patient as a result of submersion in a
liquid.
2. How many people drown each year?
Each year in the United States, more than 8,000 people die from drowning (an estimated
500,000 worldwide). It is the third leading cause of accidental death in all ages. Drowning is
the fourth leading cause of accidental death, and an estimated 50,000 persons annually
survive a submersion event.
3. Who drowns and why?
The incidence of drowning peaks in two groups—teenagers and toddlers. In teenagers
(ages 15–24), nearly 80% of drowning and submersion victims are male. Teenage boys are
victims because of risk-taking behavior during swimming, boating, diving, or other water-
related activities. Alcohol is a contributing factor in more than 60% of all teenage drownings.
Of all drowning victims, 40% are younger than 4 years. Toddlers are at risk because of
their inherently inquisitive nature and their physical inability to extricate themselves from
hazards such as pools, buckets, tubs, toilets, or washers. Inadequate supervision, even for
brief moments, is the primary cause of drowning in toddlers. One always must consider the
possibility of abuse when evaluating a child drowning victim because inflicted submersions
account for 1.5% to 8% of all events for children younger than age 5. An estimated 59% of
drownings in people younger than 1 year of age occur in bathtubs, and 56% of these are a
result of child abuse.
Other risk factors in all age groups are as follows:
n
Inability to swim
n
Hypothermia
n
Seizures
n
Cardiovascular or cerebrovascular disease
n
Trauma
n
Child abuse/neglect
n
Ethanol
n
Diabetes
n
Hyperventilation
n
Suicide
n
Substance abuse
n
Hot tubs/spas

Chapter 56 SUBMERSION INCIDENTS396
In the United States, 50,000 new pools are added annually to the 4.5 million pools that
already exist. The increasing prevalence of hot tubs, pleasure craft, and outdoor sports has
increased greatly the number of people at risk of drowning. Of drownings, 90% occur
tantalizingly close to safety, within 10 yards.
4. What kills a drowning victim?
Historically, emphasis has been placed, incorrectly, on the significance of drowning in salt
water versus fresh water because of presumed differences in the pathophysiology of the
aspirated water. In fresh-water aspirations, the hypotonic fluid was thought to diffuse into the
circulation, increasing blood volume and decreasing the concentration of serum electrolytes.
This also causes a loss of surfactant and results in alveolar collapse. Sea water was thought
to pull fluid into the alveoli, decreasing the blood volume and increasing the electrolyte
concentrations. This transudated fluid would cause a pathologic effect on pulmonary alveolar
membranes, leading to noncardiogenic pulmonary edema. In fact, such pathologic changes
have rarely been seen in patients who have survived to hospital arrival. It has been suggested
that a person must ingest 22 mL/kg to cause electrolyte changes, and it is unusual for
submersion victims take in more than 3 to 4 mL/kg.
Of submersion victims, 10% to 20% have not aspirated water, and most victims of
submersion do not aspirate enough fluid to cause a significant alteration in blood volume or
electrolytes or a life-threatening pulmonary shunt secondary to perfusion of fluid-filled alveoli.
Death is most often the result of asphyxia caused by laryngospasm and glottis closure.
Although this mechanism is less common, more successful resuscitations (80%–90% of all
patients) occur in this group of patients. The aspirated water is a significant pulmonary irritant
and contaminant that may increase intrapulmonary shunting, resulting in hypoxemia.
5. What happens in a drowning?
The first event is an unexpected or prolonged submersion. The victim begins to struggle and
panic. Fatigue begins and air hunger develops. Reflex inspiration ultimately overrides breath
holding. The victim swallows water, and aspiration occurs, causing laryngospasm that may last
for several minutes. Hypoxemia worsens, and unconsciousness ensues. If the victim is not
rescued and resuscitated promptly, central nervous system damage begins within minutes.
6. Describe the presenting symptoms of near-drowning victims.
The presenting pulmonary symptoms are varied. The patient may be completely
asymptomatic, have a mild cough, show mild dyspnea and tachypnea, or be in fulminant
pulmonary edema. The clinical spectrum of central nervous system findings may range from
confusion or lethargy to coma. Some patients may be found in cardiac arrest.
7. What is the pulmonary pathophysiology?
The central clinical feature of all submersion incidents is hypoxemia caused by laryngospasm
or aspiration. The PO
2
decreases; the PCO
2
increases, and there is a combined respiratory and
metabolic acidosis. If the patient is successfully resuscitated, the recovery phase often is
complicated by aspirated water or vomitus. Aspiration can cause airway obstruction by
particulates, bronchospasm by direct irritation, acute respiratory distress syndrome (ARDS)
due to pulmonary edema from parenchymal damage, atelectasis from loss of surfactant, and
pulmonary bacterial infections. Some patients may later develop pulmonary abscesses or
empyema.
8. How is the cardiac system affected in drowning?
Cardiac decompensation and dysrhythmias are caused by hypoxemia and complicated by the
ensuing acidosis. The heart is relatively resistant to hypoxic injury, and successful resumption
of cardiac activity is common, but severe central nervous system damage often occurs.
Response of the heart to therapy, particularly antiarrhythmic medications, may be limited by
hypoxia, acidosis, and hypothermia. Primary therapy is aimed at reversal of these three
problems.
Chapter 56 SUBMERSION INCIDENTS 397
9. What is the prehospital treatment?
The most important part of treatment of a near-drowning victim is delivered in the prehospital
phase with immediate resuscitation. If a submersion victim has appropriate airway
management and ventilation is rapidly established, anoxic brain injury is avoided, and prompt
and full recovery is anticipated. The patient without rapid airway management and ventilation
suffers irreversible anoxic brain injury and either is unresponsive to resuscitation or has a
progressively deteriorating course after initial resuscitation. Therapy must correct hypoxia,
associated acidosis, and hypotension as rapidly as possible. Establish a patent airway using
appropriate cervical spine precautions if indicated because diving injuries often are associated
with cervical spine injury. Apply a nonrebreather oxygen mask to patients with spontaneous
respirations. Initiate bag-mask breathing or endotracheal intubation if indicated. Correct hypoxia
and acidosis by hyperventilation with 100% oxygen. Intravenous (IV) access is needed.
NOTE: There is no convincing evidence for the effectiveness of postural drainage
maneuvers, and their use is not recommended.
10. When is endotracheal intubation indicated?
Any person with altered mentation or an inability to protect the airway needs intubation. In the
initially stable patient, an inability to maintain a pO
2
greater than 60 to 90 mm Hg with high
flow oxygen by nonrebreather mask indicates that extensive pulmonary compromise or ARDS
may exist, and early airway management with positive-pressure ventilation and positive end-
expiratory pressure is appropriate to decrease intrapulmonary shunting.
One important point is to determine if the submersion event may have occurred as a result
of diving into water. In these cases, the patient may have sustained a cervical spine injury, and
appropriate precautions should be taken with in-line stabilization of the neck during intubation.
11. If aspiration is suspected, what treatment is needed?
Pulmonary treatment is supportive. Close observation for signs of a developing pulmonary
infection or ARDS is needed. Some cases with significant aspiration may require
bronchoscopy to remove particulate matter and tenacious secretions. Bronchodilator therapy
with b-agonists is appropriate if bronchospasm is evident.
12. Does a normal chest radiograph rule out pulmonary injury?
No. A normal chest radiograph may be seen in 20% of cases early in their course. Typical
X-ray findings include perihilar infiltrates and pulmonary edema, although these classic
descriptors of ARDS (noncardiogenic pulmonary edema) may take hours to develop.
13. Is there a role for prophylactic antibiotics?
When contaminated water is involved (e.g., sewage), prophylactic antibiotics may be
considered. In all other instances, prophylactic antibiotics are of no proven benefit.
14. Is there an indication for the use of sodium bicarbonate during resuscitation?
No. Respiratory and metabolic acidosis should be treated by mechanical ventilation and
hyperventilation.
15. Discuss the approach to patients with a decreased level of consciousness or
coma.
Hypoxic injury leads to cerebral edema and a concomitant rise in intracranial pressure.
Although there was initial enthusiasm for treatment of presumed elevated intracranial pressure
with the usual modalities of muscle paralysis, hyperventilation, mannitol, barbiturate coma,
hypothermia, and steroids, more recent studies have shown no improvement in outcome with
these therapies. Supportive care is the mainstay of therapy. Be attentive to the possibility of
cranial or spinal injuries in all boating or diving injuries in patients with altered level of
consciousness. Do not forget the possibility of suicide or child abuse. If the history is in
doubt, assume a cranial and a cervical injury. The possibility of toxicologic conditions also
should be investigated with appropriate toxicologic screens performed.
