Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

368
ARTHRITIS
CHAPTER 53
Catherine B. Custalow, MD, PhD
1. What are the signs and symptoms of arthritis?
Arthritis is the inflammation of a joint. The process may be monoarticular (involving a single
joint) or polyarticular (multiple joints). Patients typically report pain, swelling, redness, and
limitation of motion about the involved joint. On examination there may be tenderness,
swelling, effusion, erythema, and decreased range of motion. Preverbal children may present
with a limp or avoid using the extremity.
2. What are the common causes of acute arthritis?
Arthritis has many causes, including:
n
Infection (bacterial, fungal, or viral)
n
Trauma (fracture, overuse)
n
Hemorrhage (traumatic hemarthrosis, inherited coagulopathy, or anticoagulant induced)
n
Crystal deposition disease (gout or pseudogout)
n
Neoplasm (metastasis)
n
Inflammatory conditions (rheumatoid arthritis, rheumatic fever, lupus)
n
Degenerative conditions (osteoarthritis)
3. What is the difference between an intra-articular and a periarticular process?
In a true intra-articular process the inflamed synovium typically causes diffuse, generalized joint
pain, effusion, tenderness, warmth, swelling, and an increase in pain with active/passive range
of motion and axial loading. A periarticular processes, such as bursitis, tendinitis, or cellulitis,
tends to have a more localized area of tenderness, and no joint effusion. With a periarticular
process, moving a joint throughout the entire range of its motion may not reproduce the pain in
all directions. Instead the pain may be exacerbated only by stretching the specific muscles or
tendons over the areas that are affected.
4. What are some examples of diseases that are monoarticular, polyarticular, and
periarticular?
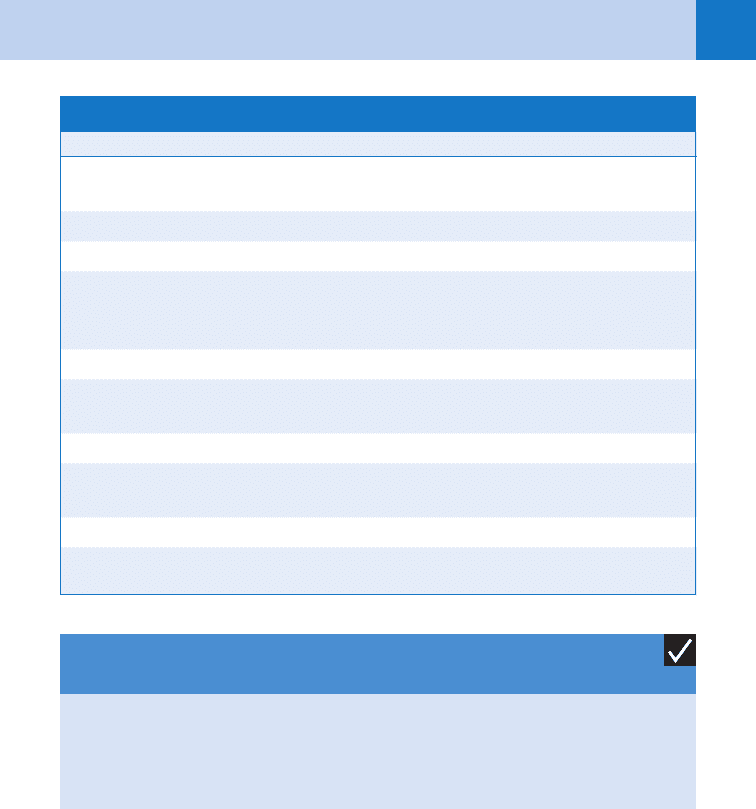
See Table 53-1 for a list of diseases by the number of joints involved.
5. What other physical findings may be helpful in diagnosing a patient with
arthritis?
A careful physical examination may provide additional clues to certain rheumatologic diseases.
Examples include genital ulcerations, purulent urethral discharge, and conjunctivitis in Reiter’s
syndrome; urethral or cervical discharge in gonococcal arthritis; tophi or concomitant renal
stones in gout; malar rash in lupus; swan-neck deformity in rheumatoid arthritis; erythema
chronicum migrans rash in Lyme disease; and high fever/chills in septic arthritis.
6. What does the location and distribution of the joint pain reveal about the
diagnosis?
Some diseases have a predilection for certain joints. Gout most frequently affects the first
metatarsophalangeal (MTP) joint. Rheumatoid arthritis commonly affects the
metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints. Osteoarthritis often
Chapter 53 ARTHRITIS 369
affects the distal interphalangeal (DIP) and the first metacarpophalangeal joints. In 45% of
cases septic arthritis attacks the knee.
7. Are X-rays helpful in the diagnosis of arthritis?
Often the only radiographic evidence of inflammation is soft-tissue swelling; however, plain
radiographs may reveal foreign bodies, fractures, effusions, osteoporosis, or osteomyelitis.
The radiographic changes of degenerative arthritis include asymmetrical joint space
narrowing, marginal osteophytes, ligamentous calcifications, and subchondral sclerosis. In
advanced gout, there may be punched out subchondral and marginal erosions, joint space
narrowing, and periarticular calcified tophi.
8. Are the erythrocyte sedimentation rate (ESR) and peripheral white blood
count (WBC) useful for the evaluation of acute arthritis?
No. The ESR represents the body’s acute phase reaction to inflammation and infection.
Unfortunately, the ESR is neither sensitive nor specific enough to confirm or exclude any
particular disease. False-negative ESRs in septic arthritis can be as high as 20% to 30%.
Likewise, the peripheral WBC count does not contribute meaningfully to the diagnosis
of an inflamed joint as evidenced by one recent study in which 52% of patients with
septic arthritis had a peripheral WBC count less than 11,000 cells/mm
3
(normal).
Therefore, when clinical suspicion is high, a joint should be aspirated regardless of the
ESR or WBC count.
9. What is the most important diagnostic test for determining the etiology of
acute arthritis?
Arthrocentesis is the most important diagnostic procedure for evaluation of an acutely
inflamed joint. Synovial fluid analysis provides rapid, critical diagnostic information and
should be performed on all patients with an acute joint effusion who have no contrain-
dications. Other indications include drainage of a tense hemarthrosis and injection of
analgesic and inflammatory medications into the joint. The procedure is simple and safe,
and complications are rare when performed under sterile conditions and with proper
technique. If a prosthetic joint infection is suspected, an orthopedist should perform the
joint aspiration if possible.
10. How is arthrocentesis performed?
The detailed anatomic approach for each joint is beyond the scope of this chapter, but the
general steps are described here. Place the patient in a comfortable position with a cushion
supporting the joint if needed. Palpate the bony landmarks. Cleanse and prep the skin. Provide
anesthesia by local infiltration with an anesthetic solution such as 1% or 2% lidocaine. Using
a 19-gauge needle attached to a syringe, aspirate gently while carefully advancing the needle
Monoarticular Polyarticular Periarticular
Septic arthritis
Gout and pseudogout
Osteoarthritis
Hemarthrosis
Trauma
Systemic lupus erythematosus
Rheumatoid arthritis
Rheumatic fever
Osteoarthritis
Reiter’s syndrome
Lyme disease
Serum sickness
Cellulitis
Bursitis
Tendinitis
TABLE 53-1. JOINTS INVOLVED IN DISEASE

Chapter 53 ARTHRITIS370
into the joint. Avoid abrasion or puncture of the articular cartilage. Withdraw as much synovial
fluid as possible. If necessary, inject anesthetic solution into the joint for pain relief. Withdraw
the needle. Send the synovial fluid to the lab for analysis for WBC count, differential, crystals,
Gram stain, and culture.
11. What are some causes of arthritis with fever?
Diseases causing arthritis with fever include septic arthritis, Lyme disease, rheumatic fever,
Reiter’s syndrome, and toxic synovitis.
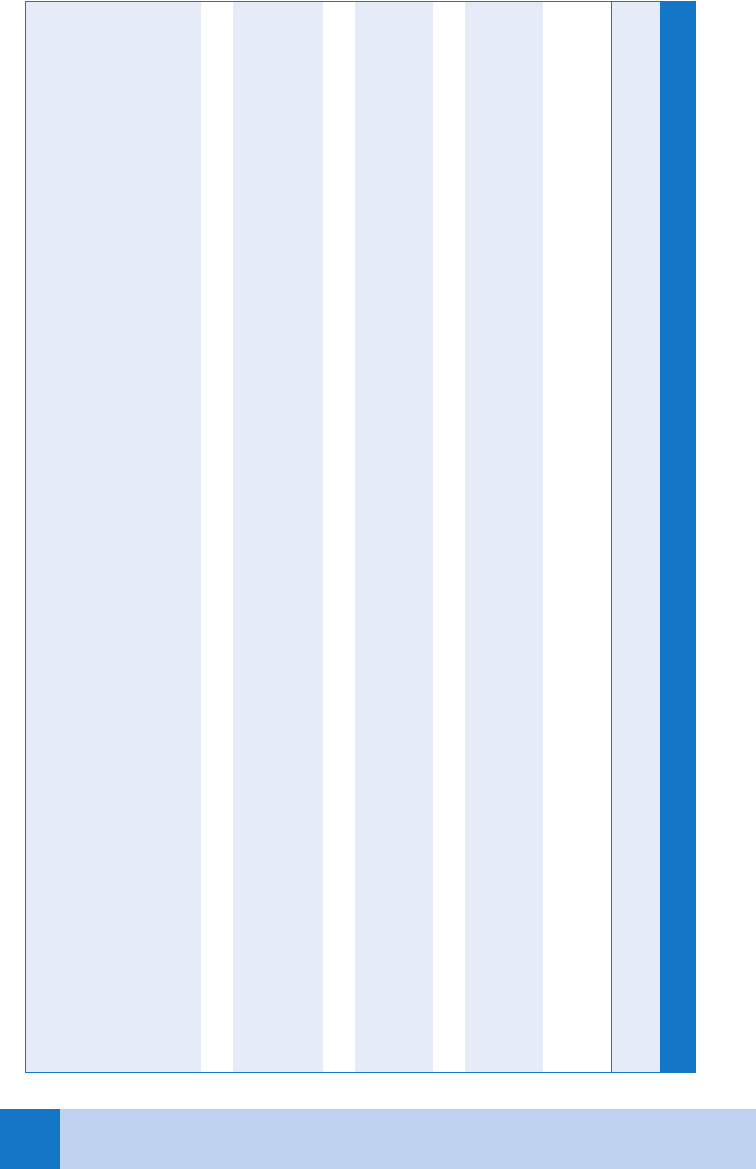
12. How do I interpret the results of the arthrocentesis?
See Table 53-2 for interpretation of synovial fluid analysis.
13. Does a synovial fluid white blood cell count of less than 50,000 cells/mm
3
completely rule out the diagnosis of a septic joint?
No. Typical synovial fluid counts in septic arthritis are greater than 50,000 WBC/mm
3
, with
predominantly polymorphonuclear neutrophilic (PMN) white blood cells, and a Gram stain
positive for bacteria. But a recent study showed that 36% of patients with septic arthritis had
synovial fluid counts less than 50,000 cells/mm
3
(168 cells in one patient). For this reason a
high index of suspicion should be maintained when a septic joint is in the differential and the
threshold for starting antibiotics must be low if the clinical examination suggests bacterial
arthritis.
14. What is the most serious cause of arthritis?
Bacterial arthritis is by far the most serious cause of acute monoarticular arthritis because
it can cause rapid cartilage destruction and significant in-hospital mortality. The most
important risk factor for septic arthritis is pre-existing joint disease, with almost half of
septic arthritis patients having previous joint problems. Permanent joint damage may
occur in as little as 7 days if untreated, and this can result in chronic disability and pain. In
children, septic arthritis can cause epiphyseal damage, resulting in growth impairment and
limb length discrepancy.
15. What organisms cause bacterial arthritis?
Staphylococcus aureus is the most common cause of septic arthritis overall. Methicillin-
resistant S. aureus (MRSA) causes 25% to 50% of septic arthritis cases with risk factors
including advanced age, comorbid medical conditions, and significant exposure to the
health care system (80% of patients hospitalized in the preceding 6 months). Other
causative organisms include Streptococcus agalactiae (group B streptococcus),
Streptococcus pneumonia, Neisseria gonorrhea, Escherichia coli, Pseudomonas
aeruginosa, Kingella kingae, and Haemophilus influenzae. In children the incidence of
septic arthritis due to H. influenza has decreased by 95% since widespread vaccination
against this organism.
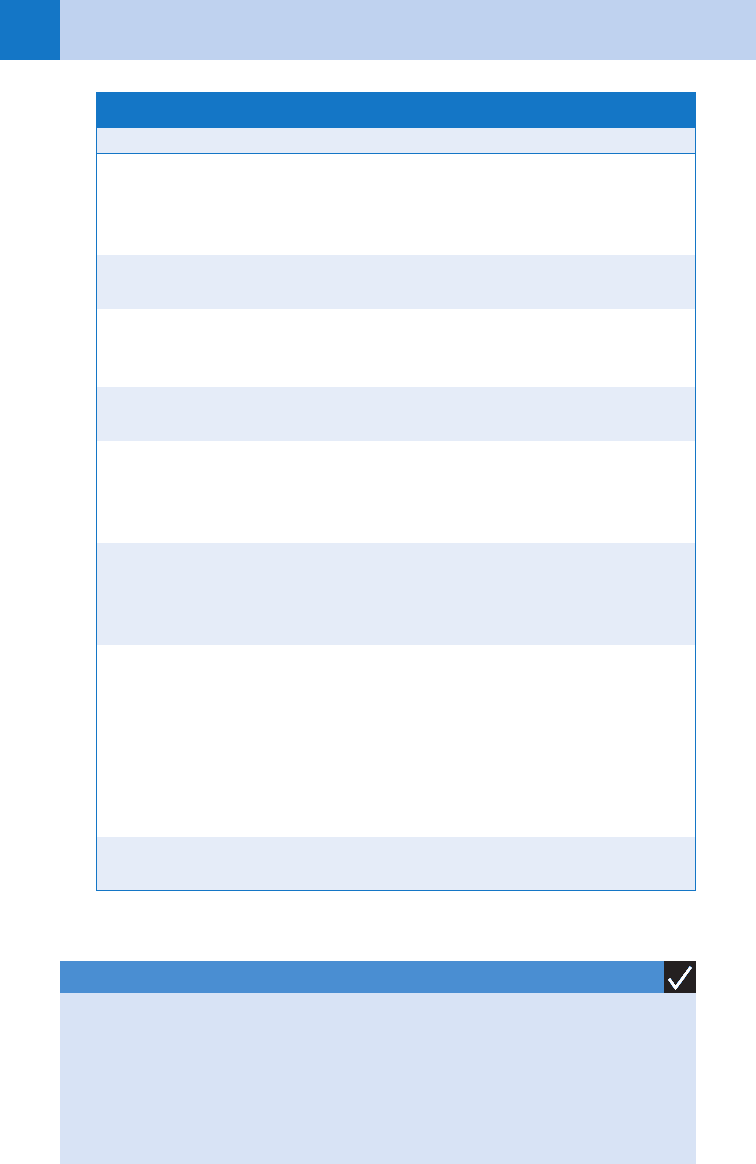
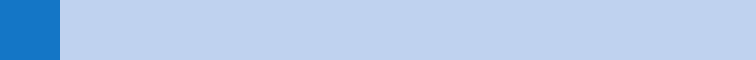
16. How is bacterial arthritis treated?
The patient should be admitted to the hospital and immediate orthopedic consultation
obtained for arthroscopic joint drainage, open joint drainage, or daily joint aspirations.
Intravenous (IV) antibiotics should be administered based on the Gram stain and culture of
the synovial aspirate if available and are generally continued for about 3 weeks. See Table 53-3
for a list of antibiotic recommendations for each organism. If the Gram stain is negative, then
empiric antibiotics can be administered according to the patient’s epidemiology. MRSA
coverage should be administered if the patient has risk factors such as being elderly, a recent
hospitalization, comorbid medical conditions, IV drug use, or living in a location with a high
prevalence of community-acquired MRSA.
17. What are some causes of arthritis with rash?
See Key Points.
Chapter 53 ARTHRITIS 371
Diagnosis Appearance
Total WBC
Count (per mm
3
) PMN (%)
Mucin Clot
Test
Fluid/Blood Glucose
(diff.) (mm/dL)
Miscellaneous
(Crystals/Organisms)
Normal Clear, pale 0–200 (200) ,10 Good NS —
Group I (noninflammatory; degenerative joint disease, traumatic arthritis)
Clear to
slightly
turbid
50–4,000 (600) ,30 Good NS —
Group II (noninfectious, mildly inflammatory; SLE scleroderma)
Clear to
slightly
turbid
0–9,000 (3,000) ,20 Good
(occasionally
fair)
NS Occasionally LE cell,
decreased complement
Group III (noninfectious, severely inflammatory)
Gout Turbid 100–160,000 (21,000) 70 Poor 10 Uric acid crystals
Pseudogout Turbid 50–75,000 70 (14,000) Fair-poor Insufficient data Calcium pyrophosphate
Rheumatoid arthritis Turbid 250–80,000 70 Poor 30 Decreased
Group IV (infectious, inflammatory)
Acute bacterial Very turbid 150–250,000 (80,000) 90 Poor 90 Positive culture for bacteria
Tuberculosis Turbid 2,500–100,000 (20,000) 60 Poor 70 Positive culture for
Mycobacterium tuberculosis
TABLE 53-2. SYNOVIAL FLUID ANALYSIS
LE, lupus erythematosus; NS, not significant; PMN, polymorphonuclear cells; SLE, systemic lupus erythematosus.
(From Wyngaarden JB, Smith LH, editors: Cecil textbook of medicine, ed 18, Philadelphia, 1988, W. B. Saunders, p 1994, with permission.)
Chapter 53 ARTHRITIS372
g, gram; h, hour; IV, intravenously; mU, million units; q, every.
Organism Gram Stain Antibiotics Dosage
Methicillin-sensitive
Staphylococcus
aureus
Gram-positive
cocci clusters
cefazolin or nafcillin
or oxacillin
cefazolin 2 g
IV q 8
nafcillin 2 g IV q 4
oxacillin 2 g IV q 4
Methicillin-resistant
S. aureus
Gram-positive
cocci clusters
vancomycin vancomycin
15 mg/kg IV q 12
Streptococcus
pneumonia
Gram-positive
cocci chains
penicillin G or
ampicillin
penicillin G 12–18
mU IV q day
divided
Penicillin sensitive Ampicillin
2 g IV q 4 h;
S. pneumonia
Penicillin resistant
Gram-positive
cocci chains
ceftriaxone or
cefepime
ceftriaxone
1 g IV q 24 h
cefepime
2 g IV q 8 h
Neisseria gonorrhea Gram-negative
cocci
ceftriaxone or
cefepime
ceftriaxone
1 g IV q 24 h
cefepime
2 g IV q 8 h
Pseudomonas
aeruginosa
Gram-negative
rods
ceftazidime or ce-
fepime plus gentami-
cin or tobramycin
ceftazidime 2 g IV
q 8cefepime
2 g IV q 8 h
gentamicin 5 mg/
kg IV q 24
tobramycin 5 mg/
kg IV q 24
TABLE 53-3 ANTIBIOTIC TREATMENT FOR SEPTIC ARTHRITIS
KEY POINTS: CAUSES OF ARTHRITIS WITH A RASH
1. Lyme disease: Erythema chronicum migrans
2. Reiter syndrome: Keratoderma blennorrhagicum
3. Disseminated gonococcal infection: Pustular rash
4. Psoriatic arthritis: Psoriatic lesions
5. Systemic lupus erythematosus: Malar rash
Chapter 53 ARTHRITIS 373
18. What is the difference between gout and pseudogout?
Gout develops when sodium urate crystals precipitate in a joint and pseudogout develops
when calcium pyrophosphate crystals precipitate in the joint. Both are released from the cells
lining the synovium and initiate an inflammatory reaction. Under polarized light microscopy,
gout crystals are needle shaped and negatively birefringent, whereas pseudogout crystals are
rhomboid in shape and positively birefringent.
19. What are the risk factors for gout and which joints are most commonly affected?
Risk factors for gout include obesity, hypertension, diabetes, dietary excess, alcohol
consumption, proximal loop diuretics, increased uric acid levels, and stress (illness or
surgery). Middle-aged men and postmenopausal women are at an increased risk for gout. The
MTP joint of the great toe is the most frequently affected joint (up to 75%). In this joint gout
is known as podagra. Other commonly involved joints are the tarsal joints, the ankle, and the
knee. Gout is polyarticular in as many as 40% of patients.
20. What medications can be used to treat gout emergently?
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the primary agents used to treat gout.
Indomethacin is commonly used at a dose of 75 to 200 mg/day for several days and tapering
off as inflammation decreases. Colchicine inhibits microtubule formation, which results in a
decreased inflammatory response and is also effective in treating acute attacks. It may be
administered orally at a dosage of 0.5 to 0.6 mg every hour until symptoms improve, until
diarrhea or vomiting develops, or until the maximum dose of 6 mg has been reached. A single
IV dose of 1 to 2 mg of colchicine administered over 10 minutes may also be quite effective.
Once bacterial infection has been ruled out, oral corticosteroids may also be administered,
such as prednisone at a dose of 40 mg/day for 3 days and then tapering off. Drugs that alter
serum uric acid levels such as allopurinol and probenecid should not be administered acutely
because changing serum uric acid levels can exacerbate the condition.
21. Which tick-borne infection causes arthritis?
See Chapter 52.
BIBLIOGRAPHY
1. Burton JH: Acute disorders of the joints and bursa. In Tintinalli JE, GD Kelen, JS Strapczynski, et al editors:
Tintinalli’s emergency medicine: a comprehensive study guide, ed 5, New York, 2000, McGraw-Hill, pp 1891–1899.
2. Custalow CB: Arthrocentesis. In CB Custalow, editor: Color atlas of emergency department procedures,
Philadelphia, 2005, Elsevier, 2005, pp 1–11.
3. Frazee BW, Fee C, Lambert L: How common is MRSA in adult septic arthritis? Ann Emerg Medi 54(5):
695–700, 2009.
4. Heffner AC: Monoarticular arthritis. In Wolfson AB, Hendey GW, Hendry PL, et al, editors: The clinical practice
of emergency medicine, ed 4, Philadelphia, 2005, Lippincott Williams & Wilkins, pp 563–568.
5. Li SF, Henderson J, Dickman E, et al: Laboratory tests in adults with monoarticular arthritis: can they rule out
a septic joint? Acad Emerg Med 11:276, 2004.
6. Lowery DW: Arthritis. In Marx JA, RS Hockberger, RM Walls, et al, editors: Rosen’s emergency medicine:
concepts and clinical practice, ed 5, St. Louis, 2002, Mosby, pp 1925–1943.
7. Nuermberger E: Septic arthritis, community-acquired. In Bartlett JG, Auwaerter PG, Pham P, editors:
http://prod.hopkins-abxguide.org.
8. Ross JJ, Davidson L: Methicillin-resistant Staphylococcus aureus septic arthritis: an emerging clinical
syndrome. Rheumatology 44:1197, 2005.
9. Schwartz DT, Reisdorff EJ: Fundamentals of skeletal radiology. In Schwartz DT, Reisdorff EJ, editors:
Emergency radiology, New York, 2000, McGraw-Hill, pp 22–24.
10. Thomas HA Jr, Hartoch RS: Polyarticular arthritis. In Wolfson AB, Hendey GW, Hendry PL, et al, editors: The
clinical practice of emergency medicine, ed 4, Philadelphia, 2005, Lippincott Williams & Wilkins, pp 568–572.
374
SKIN DISEASES
CHAPTER 54
Lela A. Lee, MD, and Joanna M. Burch, MD
1. How are skin lesions best described?
It is helpful to remember dermatologic terms (Table 54-1). Describing in plain English how the
lesions appear is acceptable, however. Communication with other care providers may be
improved by the use of plain but accurately descriptive terms.
Characteristics helpful in establishing a diagnosis include the following: location and
distribution, color, size, presence or absence of scale, contour (e.g., raised, depressed, or
pitted), tactile characteristics (e.g., firm, spongy, fluctuant, blanchable, or nonblanchable), and
apparent depth (e.g., superficial, dermal, or subcutaneous).
2. What categories of skin conditions are life-threatening or associated with
life-threatening disease?
n
Diseases resulting in extensive compromise to the cutaneous barrier
n
Skin signs of systemic infection (e.g., meningococcemia)
n
Cancers (e.g., melanoma)
n
Urticaria or angioedema with airway compromise or anaphylaxis
n
Skin signs of vascular compromise (including hemorrhage, emboli, thrombi, and
vasculitis)
n
Skin findings of an introduced toxin (e.g., venomous snake bite)
n
Skin signs of physical abuse
3. List some cutaneous red flags (i.e., skin signs indicating an increased
likelihood of disease requiring emergency attention).
n
Extensive blisters or denuded areas of skin
n
Acute total-body erythema, particularly in the elderly or frail
n
Extensive erythematous eruption in a person who is febrile and systemically ill
n
Petechiae, purpura, and ecchymoses
n
Necrosis
n
Urticaria
n
Isolated, abnormal-appearing mole
4. What types of skin diseases result in potentially life-threatening compromise
to the skin barrier?
Most of these are blistering diseases. When the blister breaks, the barrier is removed,
and the individual is at risk for infection, fluid and electrolyte imbalance, and difficulties
with heat regulation. Skin conditions that can be associated with an extensively
compromised barrier include toxic epidermal necrolysis (TEN), Stevens-Johnson
syndrome (SJS), pemphigus and pemphigus-like chronic blistering diseases, and burns.
Patients with erythroderma (total or near-total body erythema) also may have problems
with infection, fluid and electrolyte balance, and heat regulation, particularly patients
who have significant chronic health problems, such as congestive heart failure. Lesions
of the oral cavity may compromise life if they are severe enough to prevent food or fluid
intake.
Chapter 54 SKIN DISEASES 375
5. Describe the skin findings in meningococcemia, Rocky Mountain spotted
fever, toxic shock syndrome, and necrotizing fasciitis.
n
In meningococcemia, lesions may be irregularly shaped petechiae or purpura with dusky
centers, located most commonly on the trunk and extremities. The lesions may involve the
palms and soles.
n
In Rocky Mountain spotted fever, skin lesions appear on about day 4 of the acute febrile
illness. Lesions begin on the distal extremities, may involve the palms and soles, and
spread centripetally. After a few days, the lesions become petechial or purpuric. In practice,
this eruption may be difficult to distinguish from that of meningococcemia.
n
Patients with toxic shock syndrome may have a scarlatiniform eruption, edema of the face
and extremities, conjunctival erythema, and erythema of the oral or genital mucosa. There
is desquamation of the hands and feet 1 to 2 weeks later.
n
Necrotizing fasciitis is characterized by a rapidly progressive painful erythema with
development of duskiness and frank necrosis. There may be blisters. The overlying skin
change is often mild compared with the necrosis occurring underneath.
KEY POINTS: PHYSICAL FINDINGS OF LIFE-THREATENING
DISEASES WITH COMPROMISE TO SKIN BARRIER
1. Extensive blistering
2. Erythroderma
3. Extensive oral erosions preventing food or fluid intake
Skin Lesion Description Example
Macule Flat, circumscribed color change (nonpalpable)
,1 cm
Café-au-lait spot
Patch Flat color change .1 cm Vitiligo
Papule Raised lesion ,1 cm Molluscum contagiosum
Plaque Elevated, flat-topped lesion .1 cm. Lesions with
epidermal changes (e.g., scale) would be
considered plaques.
Psoriasis
Nodule Raised lesion with a deeper palpable portion Erythema nodosum
Vesicle Raised, usually dome-shaped lesion filled with
fluid and ,1 cm
Varicella
Bulla Fluid-filled lesion .1 cm Bullous pemphigoid
Pustule Raised lesion filled with exudative fluid, giving it a
yellow appearance
Folliculitis
Cyst Nodule filled with semisolid-to-solid material Epidermoid cyst
Wheal Flat-topped, firm, raised, edematous lesion; a hive Urticaria
TABLE 54-1. BASIC DERMATOLOGIC TERMS
Chapter 54 SKIN DISEASES376
6. Describe the skin findings of common or distinctive childhood exanthems.
n
Scarlet fever occurs in children between the ages of 2 and 10 years. Red macules and
papules start on the neck and usually spread to the trunk and extremities. The skin may
have a rough sandpaper feel on palpation and sometimes can be petechial. Erythema is
usually most intense in the axillae, groin, and abdomen. Patients may exhibit Pastia’s lines,
which are petechiae in a linear pattern along the major skin folds. Palms and soles
characteristically are spared. The face appears flushed with circumoral pallor.
Desquamation usually occurs as the eruption resolves in 1-3 weeks.
n
Staphylococcal scalded skin syndrome begins as faint erythema on the face, neck, axilla,
and groin in a child younger than 5 years, usually following upper respiratory symptoms.
The skin is tender, and crusting typically occurs around the mouth, eyes, and skin folds.
The skin separates through the epidermis with even slight rubbing, leaving a red, moist
surface underneath (Nikolsky’s sign). Mucous membranes are not involved. In neonates,
the entire body is involved, whereas in infants and children the upper body is affected
preferentially.
n
Varicella (chickenpox) presents with abrupt onset of crops of faint macules that progress
through several stages. The macules become edematous papules, then vesicles over 24 to
48 hours. Often there is a small vesicle on a larger erythematous macule, described as a
“dew drop on a rose petal.” The vesicles develop moist crusts and leave shallow erosions.
Lesions tend to begin centrally and spread to the extremities. The palms, soles, and
mucous membranes frequently are involved. Characteristically, lesions in multiple stages of
development (i.e., macules, papules, vesicles, crusts, erosions) are present in the same
patient. The number of lesions ranges from 10 to 1,500 (average 300). The lesions are
usually pruritic. In general, lesions heal without scarring, although scarring may occur in
some instances.
n
Erythema infectiosum (fifth disease) is a parvovirus B19 infection that results in intense
erythema on the bilateral cheeks (slapped cheeks). In some patients, after the facial
erythema, a diffuse pink-to-red macular eruption develops with a reticular or lacy
appearance. The macular eruption tends to reappear with stimulation of cutaneous
vasodilation, such as warm baths, exercise, or sun exposure. This can last for 4 months.
Some patients develop a petechial eruption of the distal hands and feet with parvovirus B19
infection. This is the purpuric gloves and socks syndrome.
n
Roseola (exanthem subitum) is a disease of infants and toddlers caused by infection with
human herpesvirus 6. After 2 to 3 days of sustained fever, abrupt defervescence is followed
by a pink maculopapular eruption. Periorbital edema is sometimes seen.
n
Hand-foot-and-mouth disease caused by Coxsackieviruses exhibits an abrupt onset of a
few scattered papules that progress to oval or linear vesicles with an erythematous rim. As
the name suggests, most lesions occur on the oral mucosa, palms, and soles. The oral
lesions appear as small, discrete, whitish-gray erosions.
n
Kawasaki disease is typified by an irritable child with conjunctival injection and slightly
swollen, distinctly red lips. The hands may be edematous or desquamating. The skin
findings are nonspecific and variable, ranging from macules to maculopapules to vesicles.
The child must meet the clinical criteria of fever for 5 or more days plus four of five of the
following:
a. Nonpurulent conjunctivitis
b. Mucosal changes
c. Edema or desquamation of the distal extremities
d. Exanthema
e. Cervical lymphadenopathy
7. What is erythema multiforme (EM)?
EM is usually an eruption of acute onset that is characterized by multiple, fixed red papules.
Because the keratinocyte is the target of inflammatory insult, there is keratinocyte necrosis
or apoptosis, manifest clinically as a central dusky center. The characteristic lesion is the
Chapter 54 SKIN DISEASES 377
target lesion: a papule with a central dusky zone and an outer zone of erythema. The
majority of EM lesions are erythematous, whereas typically only a few lesions are truly
target-like. Some lesions may develop vesicular changes in the center, due to intense
necrosis.
EM frequently follows herpes simplex (HSV) infection. Mucous membranes are usually
spared or affected mildly. Lesions are found on the dorsal hands and extensor extremities, and
palms and soles frequently are involved. Patients with HSV-associated EM are not generally
ill-appearing, and although the eruption can be quite impressive, it can be managed on an
outpatient basis. The eruption lasts 10 to 14 days and may recur after subsequent episodes of
HSV. Antiviral therapy is useful only as suppressive therapy to prevent HSV recurrences.
Treatment is usually reassurance or oral antihistamines to treat any associated burning and
itching. Topical or oral steroids are not indicated.
8. Which disease is most often mistaken for EM?
Acute urticaria. Urticarial lesions may be annular with concentric color changes and may
occur on the palms and soles. Usually, urticarial lesions have a pale edematous center with an
erythematous border, whereas EM lesions tend to have dusky centers. Lesions in urticaria are
transient (,24 hours), whereas the target-like lesions of EM are fixed and can be present for
one week or more. Urticarial lesions clear with subcutaneous epinephrine, whereas EM lesions
do not.
9. What is the most common clinical presentation of a cutaneous adverse drug
reaction?
Exanthematous (morbilliform, maculopapular, or urticarial) eruptions are the most
common presentation of a cutaneous adverse drug reaction. The eruption is characterized
by erythematous macules and papules that are usually widespread and symmetrically
distributed. Lesions can sometimes show central clearing, often leading to the incorrect
diagnosis of EM. The eruptions usually begin 7 to 14 days after the onset of the new
medication, but in the cases of rechallenge, time to onset can be shorter. Treatment
includes stopping the offending drug and prescribing antihistamines for symptomatic relief
of pruritus.
10. What drugs are most often implicated in exanthematous drug eruptions?
Aminopenicillins, sulfonamides, cephalosporins, and anticonvulsants.
11. What is the main diagnosis in the differential of exanthematous drug
eruptions?
Viral exanthems are often clinically and histologically indistinguishable from morbilliform
drug eruptions. History of recent drug administration or symptoms of viral illness will help
distinguish. Peripheral blood eosinophilia favors drug eruption. In children, 10% to 20% of
exanthematous eruptions are drug induced, whereas 50% to 70% are drug induced in adults.
Skin biopsy will not distinguish viral from drug exanthematous eruptions and is not helpful to
distinguish which drug is the cause.
12. What clinical signs should prompt consideration of a more serious adverse
drug reaction?
Facial edema; marked peripheral blood eosinophilia; hepatosplenomegaly; hemorrhagic and
tender mucous membrane lesions; painful, dusky papules or plaques; or blistering and
sloughing of the skin should prompt consideration of the serious drug reactions.
13. Describe the signs and symptoms of the most serious drug eruptions.
Three severe adverse drug reactions that can result in death are SJS, TEN, and drug reaction
with eosinophilia and systemic symptoms (DRESS) (See Table 54-2). Urticaria and angioedema
can also be life-threatening if the airway is compromised.
