Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 56 SUBMERSION INCIDENTS398
16. Are glucocorticoids, barbiturate coma, or induced hypothermia indicated?
In the case of glucocorticoids and barbiturate coma, no. These therapies are unproven and
remain controversial. However, therapeutic hypothermia has recently been shown to be of
benefit in cardiac arrest, and case reports have suggested similar outcomes for victims of
submersion. In fact, Hein and colleagues reported on twin toddlers who suffered submersion
incidents, and the patient treated with induced hypothermia recovered without neurologic
deficit.
Investigators are also evaluating surfactant therapy as a new treatment for acute
respiratory failure secondary to submersion. Cubattoli and colleagues reported on two
submersion patients in acute respiratory failure who underwent bronchoscopy and instillation
of surfactant into both lungs with marked physiologic improvement.
17. What is unique about cold-water submersion?
Cases in which victims of prolonged submersion in cold water have been resuscitated
successfully without apparent neurologic sequelae are reported occasionally. The number
remains small, however. Sudden submersion in cold water theoretically induces the
mammalian diving reflex, in which blood is shunted from the periphery to the central core.
The induced hypothermia causes a decrease in metabolic demand, reducing potential hypoxic
injury from prolonged asphyxia. Cold water does have potentially deleterious effects. Most
significant are the induced cardiac irritability from hypothermia, exhaustion, and altered
mental status. Resuscitation of hypothermic near-drowning victims should be continued until
patients are adequately rewarmed or to the level required for therapeutic hypothermia (see
Chapter 57).
18. When should resuscitative efforts be withheld?
Generally, all patients should receive initial resuscitative efforts. One child recovered
successfully from a 66-minute submersion in cold water, and other studies have reported that
patients requiring cardiopulmonary resuscitation (CPR) in the field may make a full recovery.
When their core temperature has normalized and therapeutic efforts remain unsuccessful,
patients can be pronounced dead.
19. What is the disposition of a submersion victim?
All submersion victims with cardiac arrest deserve aggressive in-hospital resuscitation until
all reasonable efforts prove futile and the patient is near normothermic. All other submersion
victims require close observation. Some respiratory complications of drowning are delayed in
presentation and usually appear within 8 hours. A patient with any respiratory complaints or
symptoms, chest radiograph abnormalities, or a demonstrated oxygen requirement should be
monitored closely in a hospital for at least 24 hours. Similarly, any patient who received
resuscitative efforts or had a reported loss of consciousness, cyanosis, or apnea should be
monitored closely. Patients without any symptoms and completely normal evaluation may be
discharged after 6 to 8 hours of observation with instructions to return immediately if
respiratory distress ensues.
KEY POINTS: SUBMERSION INCIDENTS
1. Toddlers and teenagers are most at risk for death due to submersion.
2. Prehospital treatment is critical and directed at correcting underlying hypoxia.
3. A normal chest radiograph does not rule out pulmonary injury.
4. All asymptomatic victims of submersion must be observed at least 6 to 8 hours prior to
discharge.
5. Many submersion incidents are preventable.
Chapter 56 SUBMERSION INCIDENTS 399
20. What are the most important factors in estimating prognosis?
The most important factor in determining outcome is the patient’s response to resuscitation as
measured by serial neurologic examinations. Poor prognostic factors include:
n
A Glasgow Coma Scale score less than or equal to 5
n
Prolonged submersion (.5 minutes)
n
Delay in initiating CPR
n
pH less than 7.0
n
Water temperatures of greater than 10°C (77°F)
n
Asystole on arrival to the ED
Patients who arrive aware and alert have a 100% complete neurologic recovery, whereas 95%
of arousable patients with altered mentation have a complete neurologic recovery.
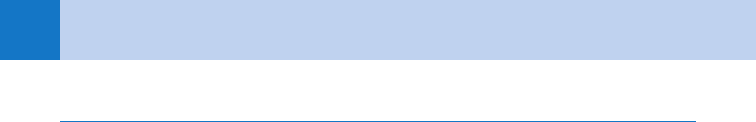
Szpilman has proposed a clinical classification based on the analysis of 1,831 cases of
submersion seen in Brazil over a 19-year period. The classification is based on clinical
findings in the field, and the mortalities are shown in Table 56-1.
21. Can we prevent submersion incidents?
Many of the factors contributing to death by submersion are preventable and can be directed
at those groups at risk, particularly children. Efforts include:
n
Fencing of private and public swimming pools
n
The use of personal flotation devices
n
Improving supervision of infants and young children near water
n
Increasing public knowledge of the risks of the day’s water conditions
n
Understanding the limitations of personal health conditions
n
Stressing the separation of alcohol from water-related activities.
WEBSITE
Drowning: http://emedicine.medscape.com/article/772753-overview
Grade Clinical Findings Mortality Rate (%)
1 Normal pulmonary auscultation 6 cough 0
2 Rales or crackles in some lung fields 0.6
3 Crackles in all fields without hypotension 5.2
4 Crackles in all fields with hypotension 19.4
5 Respiratory arrest without cardiac arrest 44
6 Cardiopulmonary arrest 93
TABLE 56-1. SZPILMAN CLASSIFICATION OF NEAR-DROWNING AND DROWNING
Chapter 56 SUBMERSION INCIDENTS400
BIBLIOGRAPHY
1. Cubattoli L, Franchi F, Coratti G: Surfactant therapy for acute respiratory failure after drowning: two children
victims of cardiac arrest. Resuscitation 80(9):1088–1089, 2009.
2. Hein OV, Triltsch A, von Buch C, et al: Mild hypothermia after near-drowning in twin toddlers. Crit Care Med
8(5):R353–R357, 2004.
3. Layon JL, Modell JH: Drowning: update 2009. Anesthesiology 110:1390–1401, 2009
4. Olshaker JS: Submersion. Emerg Med Clin North Am 22:357–367, 2004.
5. Richards DB, Knaut AL: Drowning. In Marx JA, Hockberger RS, Walls RM, et al, editors: Rosen’s emergency
medicine: concepts and clinical practice, ed 7, St. Louis, 2009, Mosby.
6. Salomez F, Vincent JL: Drowning: a review of epidemiology, pathophysiology, treatment, and prevention.
Resuscitation 63:261–268, 2004.
7. Schoene RB, Nachat A, Gravatt AR, et al: Submersion incidents: drowning and near-drowning. In Auerbach PS,
editor: Wilderness emergency medicine, ed 5, St. Louis, 2007, Mosby.
8. Szpilman D: Near-drowning and drowning classification: a proposal to stratify mortality based on the analysis
of 1,831 cases. Chest 112:660–665, 1997.
9. Williamson JP, Illing R, Gertler P, et al: Near-drowning treated with therapeutic hypothermia. Med J Aust
181:500–501, 2004.
401
HYPOTHERMIA AND FROSTBITE
CHAPTER 57
Daniel F. Danzl, MD, and Mary Nan Mallory, MD
HYPOTHERMIA
1. What is accidental hypothermia?
An unintentional decrease in core temperature to less than 35°C (95°F). The preoptic anterior
hypothalamus normally maintains a diurnal temperature variation within 1°C.
2. What factors are important in the epidemiology of hypothermia?
Primary accidental hypothermia results from direct exposure to the cold. Secondary
hypothermia is a natural complication of many systemic disorders, including sepsis, cancer,
and trauma. The mortality of secondary hypothermia is much higher. Although outdoor
exposure is common, many elderly victims are found indoors.
3. How is body temperature normally regulated?
The normal physiology of temperature regulation is activated by cold exposure, producing
reflex vasoconstriction and stimulating the hypothalamic nuclei. Heat preservation mechanisms
include shivering, autonomic and endocrinologic responses, and adaptive behavioral responses.
Although acclimatization to heat stress is efficient, humans can’t acclimate to a three-dog night.
KEY POINTS: COMMON MECHANISMS OF HEAT LOSS
1. Radiation
2. Conduction
3. Convection
4. Respiration
5. Evaporation
4. Describe the common findings in mild, moderate, and severe hypothermia.
■
Mild hypothermia (32.2°C–35°C [90°F–95°F]) depresses the central nervous system and
increases the metabolic rate, pulse, and amount of shivering thermogenesis. Dysarthria,
amnesia, ataxia, and apathy are common findings.
■
Moderate hypothermia (27°–C32.2°C [80°F–90°F]) progressively depresses the level of
consciousness and the vital signs. Shivering is extinguished, and dysrhythmias commonly
develop. The QT interval is prolonged, and a J wave (Osborn wave) may appear at the
junction of the QRS complex and ST segment. Patients become poikilothermic and cannot
rewarm spontaneously. A cold diuresis results from an initial central hypervolemia, which is
caused by the peripheral vasoconstriction.
■
Severe hypothermia (, 27°C [80°F]) results in coma and areflexia with profoundly
depressed vital signs. Carbon dioxide production decreases 50% for each 8°C fall in
temperature; there is little respiratory stimulation.

Chapter 57 HYPOTHERMIA AND FROSTBITE402
5. What three factors predispose to hypothermia?
■
Decreased heat production
■
Increased heat loss
■
Impaired thermoregulation
6. What decreases heat production?
Decreased heat production is common:
■
At the age extremes
■
With inadequate stored fuel
■
With endocrinologic or neuromuscular inefficiency
Neonates are poorly adapted for cold, even without being subjected to emergent deliveries
and resuscitations. The elderly have progressively impaired thermal perception. Anything
from simple hypoglycemia to more severe malnutrition represents a threat to the core
temperature. Examples of endocrinologic failure include myxedema, hypopituitarism, and
hypoadrenalism.
7. What are the common causes of increased heat loss?
Increased heat loss results mainly from exposure or dermatologic problems that interfere with
the skin’s integrity. Iatrogenic causes include emergency childbirth, cold infusions, and
heatstroke treatment.
8. How is thermoregulation impaired?
Impairment is via central, peripheral, metabolic, or pharmacologic mechanisms. A variety of
central nervous system processes affect hypothalamic function. Traumatic or neoplastic
lesions and degenerative processes induce hypothermia. Acute spinal cord transection
extinguishes peripheral vasoconstriction, which prevents heat conservation. The abnormal
plasma osmolality common with metabolic derangements, including diabetic ketoacidosis and
uremia, is an additional cause. Innumerable medications and toxins can impair central
thermoregulation when present in either therapeutic or toxic doses.
9. When should hypothermia be suspected?
The diagnosis is simple when a history of exposure is obvious. The history may not be
available or helpful, however, and subtle presentations are far more common in urban
areas. Ataxia and dysarthria may mimic a cerebrovascular accident or intoxication. The
only safe way to avoid missing the diagnosis is to routinely measure the patient’s
temperature.
10. Are there decoys that confuse the physical examination?
If there is tachycardia disproportionate for the temperature, suspect hypoglycemia, an
overdose, or hypovolemia. Most patients with vasodilation require volume administration.
Hyperventilation during moderate or severe hypothermia suggests a central nervous system
lesion or one of the systemic acidoses, such as diabetic ketoacidosis or lactic acidosis. A
cold-induced rectus spasm and ileus may mask or mimic an acute abdomen. Suspect an
overdose, ETOH intoxication, or central nervous system insult whenever the decreased level of
consciousness is not consistent with the temperature.
11. What options are available to measure the core temperature?
Rectal, esophageal, tympanic, and bladder sites can be measured. The rectal temperature may
lag or be falsely low if the probe is in cold feces. Esophageal temperature is falsely elevated
during heated inhalation. The reliability of tympanic measurements is unclear.
12. How does temperature depression affect the hematologic evaluation of
patients?
Anemia is masked because the hematocrit increases 2% per 1°C drop in temperature. Do
not rely on leukocytosis to predict sepsis because the leukocytes often are sequestered.
Chapter 57 HYPOTHERMIA AND FROSTBITE 403
There are no safe predictors of values. The increased viscosity seen with cold hema-
glutination often results in either thrombosis or hemolysis, and a type of disseminated
intravascular coagulation syndrome can occur. Coagulopathies are not reflected by the
deceptively normal international normalized ratio because this test is done routinely on blood
rewarmed to 37°C.
13. Should arterial blood gases be corrected for temperature?
No. Correction implies acidosis is beneficial. An uncorrected pH of 7.4 and pCO
2
of 40 mm Hg
confirm acid-base balance at all temperatures.
14. What is the key decision regarding rewarming?
The primary initial decision is whether to rewarm the patient passively or actively. Passive
rewarming is noninvasive and involves simply covering the patient in a warm environment.
This technique is ideal for previously healthy patients with mild hypothermia.
15. What conditions mandate active rewarming?
■
Cardiovascular instability
■
Temperature , 32.2°C (90°F)
■
Age extremes
■
Neurologic or endocrinologic insufficiency
16. What is core temperature afterdrop?
The commonly observed continued drop in core temperature after initiation of rewarming.
There are two causes:
■
Temperature equilibration between tissues
■
The circulatory return of cold peripheral blood to the core
17. Are there unique considerations with active external rewarming?
The external transfer of heat to a patient is accomplished most safely when the heat is applied
directly to the trunk. In chronically hypothermic patients, rapidly rewarming the
vasoconstricted extremities may overwhelm a depressed cardiovascular system and result in
cardiovascular collapse. Forced heated air rewarming blankets and circulating water blankets
are commonly used. Monitoring in a heated tub can be difficult, and vasoconstricted skin is
burned easily by electric blankets.
18. What constitutes active core rewarming?
Techniques that deliver heat directly to the core. Options include heated inhalation, heated
infusion, lavage, and extracorporeal rewarming.
19. When is airway rewarming indicated?
Heated, humidified oxygen can be administered via mask or endotracheal tube. Heat transfer
is not as significant by mask, but respiratory heat loss is eliminated while the patient is
rewarmed gradually.
20. What are the techniques for heated irrigation?
Heat transfer from irrigation of the gastrointestinal tract is minimal. Irrigation should be
considered only in severe cases and in combination with other techniques. Thoracostomy
tube irrigation with two tubes is a more efficient alternative in severe cases. Intravenous
(IV) fluids heated to 40°C to 42°C are particularly helpful during major volume
resuscitations.
21. When should heated peritoneal lavage be considered?
Double-catheter peritoneal lavage can efficiently rewarm seriously hypothermic patients. This
invasive technique generally should be reserved for severely hypothermic and unstable
patients, or in patients with certain overdoses. Infuse 2 L of isotonic dialysate at 40°C to 45°C,
and suction after 20 minutes dwell time.
Chapter 57 HYPOTHERMIA AND FROSTBITE404
22. When is extracorporeal rewarming indicated?
Cardiopulmonary bypass, continuous arteriovenous and venovenous rewarming, and
hemodialysis can be life-saving in cardiac arrest situations. Patients with completely frozen
extremities, severe rhabdomyolysis, and major electrolyte fluxes are also easier to manage in
this manner.
23. What are the contraindications to cardiopulmonary resuscitation (CPR) in
accidental hypothermia?
CPR should be initiated unless do-not-resuscitate status is verified, lethal injuries are
identified, no signs of life are present, or the chest wall is frozen and cannot be compressed.
Because a profoundly hypothermic patient may appear dead, and because vital signs may be
difficult to obtain, a cardiac monitor should be applied for 30 to 45 seconds to ensure that
there are no signs of life.
24. Are there unique pharmacologic considerations during hypothermia?
Protein binding increases as body temperature drops, and most drugs become ineffective.
Pharmacologic manipulation of the pulse and blood pressure generally should be avoided.
25. What is the significance of atrial and ventricular dysrhythmias?
Atrial dysrhythmias normally have a slow ventricular response. They are innocent and should
be left untreated. Pre-existent ventricular ectopy may resurface during rewarming and confuse
the picture. Ventricular dysrhythmia treatment is problematic because the cold heart may be
unresponsive to cardiovascular agents. If the patient is in ventricular fibrillation, only one
defibrillation attempt (2 J/kg) is indicated until the core temperature exceeds 30°C to 32°C.
FROSTBITE
26. What is frostbite?
Frostbite is the most common freezing injury of tissue. It occurs whenever the tissue
temperature decreases to less than 0°C. Ice crystal formation damages the cellular
architecture, and stasis progresses to microvascular thrombosis.
27. Which factors predispose to frostbite?
Tissue rapidly freezes when in contact with good thermal conductors, including metal, water,
and volatiles. Direct exposure to cold wind (wind-chill index) quickly freezes acral areas (e.g.,
fingers, toes, ears, nose). A variety of conditions can impair the peripheral circulation and
predispose to frostbite. Constrictive clothing and immobility reduce heat delivery to the distal
tissues. Vasoconstrictive medications, including nicotine, can exacerbate cold damage,
especially when coupled with underlying vascular conditions, such as atherosclerosis.
28. What peripheral circulatory changes precede frostbite?
Humans possess a life-versus-limb mechanism that helps prevent systemic hypothermia.
Arteriovenous anastomoses in the skin shunt blood away from acral areas to limit radiative
heat loss.
29. Before frostbite occurs, what other cutaneous events take place in the
prefreeze phase?
As tissue temperatures decrease to less than 10°C, anesthesia develops. Endothelial cells leak
plasma, and microvascular vasoconstriction occurs. Crystallization is not seen as long as the
deeper tissues conduct and radiate heat.
30. What happens during the freeze phase of frostbite?
The type of exposure determines the rate and location of ice crystal formation. Usually, ice
initially forms extracellularly, causing water to exit the cell and inducing cellular dehydration
hyperosmolality, collapse, and death.
Chapter 57 HYPOTHERMIA AND FROSTBITE 405
31. Immediately after thawing, what may occur?
In deep frostbite, progressive microvascular collapse develops. Sludging, stasis, and cessation
of flow begin in the capillaries and progress to the venules and the arterioles. The tissues are
deprived of oxygen and nutrients. Plasma leakage and arteriovenous shunting increase tissue
pressures and result in thrombosis, ischemia, and necrosis.
32. What is progressive dermal ischemia?
This is an additional insult to potentially viable tissue that is partially mediated by
thromboxane. Arachidonic acid breakdown products are released from underlying damaged
tissue into the blister fluid. The prostaglandins and thromboxanes produce platelet
aggregation and vasoconstriction.
33. What delayed physiologic events occur?
Edema progresses for 2 to 3 days. As the edema resolves, early necrosis becomes apparent if
nonviable tissue is present. Final demarcation often is delayed for more than 60 to 90 days.
Hence the aphorism, “Frostbite in January, amputate in July.”
34. What are the symptoms of frostbite?
Sensory deficits are always present, affecting light touch, pain, and temperature perception.
Frostnip produces only a transient numbness and tingling. This is not true frostbite because
there is no tissue destruction. In severe cases, patients report a “chunk of wood” sensation
and clumsiness.
35. What imaging techniques might help assess frostbite severity?
Routine radiography at presentation and later at 4 to 10 weeks post-injury may demonstrate
specific abnormalities. Scintigraphy may predict tissue loss and monitor the efficacy of
treatment. Magnetic resonance angiography can also predict tissue demarcation.
36. What is chilblain (PERNIO)?
Repetitive exposure to dry cold can induce chilblain (cold sores), especially in young women.
Pruritus, erythema, and mild edema may evolve into plaques, blue nodules, and ulcerations.
The face and dorsa of the hands and feet are commonly affected.
37. What is trench foot?
Prolonged exposure to wet cold above freezing results in trench foot (immersion foot).
Initially, the feet appear edematous, cold, and cyanotic. The subsequent development of
vesiculation may mimic frostbite. Liquefaction gangrene is a more common sequela, however,
with trench foot than with frostbite.
38. How should frostbite be classified?
Classification by degrees as is done with burns is unnecessary and is often prognostically
incorrect. Superficial or mild frostbite does not result in actual tissue loss; deep or severe
frostbite does.
39. What do the various signs of frostbite indicate?
The initial presentation of frostbite can be deceptively benign. Frozen tissues appear yellow,
waxy, mottled, or violaceous-white. Favorable signs include normal sensation, warmth, and
color after thawing. Early clear bleb formation is more favorable than delayed hemorrhagic
blebs. These result from damage to the subdermal vascular plexi. Lack of edema formation
also suggests major tissue damage.
40. How should frozen tissues be thawed?
Rapid, complete thawing by immersion in 40°C to 41°C circulating water is ideal. Reestablishment
of perfusion is intensely painful, and parenteral narcotics are needed in severe cases. Premature
termination of thawing is a common mistake because an incomplete thaw increases tissue loss.
Never use dry heat or allow tissues to refreeze. Rubbing or friction massage may be harmful.
Chapter 57 HYPOTHERMIA AND FROSTBITE406
41. What steps should immediately follow thawing?
■
Handle tissues gently, and elevate the injured parts to minimize edema formation.
■
If cyanosis is still present after thawing, monitor the tissue compartment pressures.
■
Consider streptococcal and tetanus prophylaxis.
■
Avoid compressive dressings, and use daily whirlpool hydrotherapy.
■
Consider phenoxybenzamine (a-blocker that reduces vasoconstriction) in severe cases.
■
Whenever possible, defer surgical decisions regarding amputation until clear demarcation
is demonstrated.
■
Magnetic resonance angiography may predict demarcation earlier than clinical demarcation.
42. How are blisters treated?
Clear blisters may temporarily be left intact or sterilely aspirated. After debridement, apply
antibiotic ointment or a specific thromboxane inhibitor, topical aloe vera. When coupled with
systemic ibuprofen, this strategy can minimize accumulation of arachidonic acid breakdown
products. In contrast, hemorrhagic blisters should be left intact to prevent tissue desiccation.
43. Are any ancillary treatment modalities really helpful?
A variety of vasodilatory treatment regimens, including medical and surgical sympathec-
tomies, dextran, heparin, and a variety of anti-inflammatory agents, do not conclusively
increase tissue salvage. In select cases, with less than 6 hours of warm ischemia time,
thrombolytic therapy may decrease the need for amputation.
KEY POINTS: COMMON SEQUELAE OF FROSTBITE
1. Paresthesias
2. Hyperhidrosis
3. Thermal misperception
4. Epiphyseal damage
5. Nail deformities
BIBLIOGRAPHY
1. Danzl DF: Accidental hypothermia. In Marx JA, Hockberger RS, Walls RM, editors: Rosen’s emergency
medicine: concepts and clinical practice, ed 7, Philadelphia, 2009, Mosby Elsevier, pp 1868–1881.
2. Danzl DF: Frostbite. In Marx JA, Hockberger RS, Walls RM, editors: Rosen’s emergency medicine concepts and
clinical practice, ed 7, Philadelphia, 2009, Mosby Elsevier, pp 1861–1867.
WEBSITES
www.emedicine.com
www.hypothermia.org,
www.uptodate.com
407
HEAT ILLNESS
CHAPTER 58
Christopher B. Colwell, MD, and Gina Soriya, MD
1. How does the body regulate temperature?
The hypothalamus controls thermoregulation. The posterior region functions to conserve heat
and the preoptic region is involved in heat dissipation. This is a critical function as human
body systems operate under a narrow range of temperatures.
2. What are the four mechanisms for cooling the body?
n
Conduction: the transfer of thermal energy between objects in direct contact with each
other due to a temperature gradient; heat moves from the warmer to the cooler object,
equalizing the temperature difference.
n
Convection: heat transfer in a gas or liquid by the circulation of currents from one region to
another.
n
Radiation: energy emitted by one body travels through a medium or space to be absorbed
by another body.
n
Evaporation: molecules in a liquid state spontaneously become gaseous, such as sweat
into the ambient air.
3. Which mechanism is the most effective for heat loss?
Evaporation is the most effective means of cooling the body.
4. How does the relative humidity of the atmosphere affect the normal body
mechanisms of cooling?
The moisture gradient has to be such that the air is dryer than the body. As humidity rises,
evaporation becomes less effective. Heat is removed from the body at a slower rate, causing
greater heat retention.
5. How does heat cause damage to the body?
Heat is directly toxic to cells, causing protein denaturation, as well as breakdown of cellular
membranes and nuclei, leading to cell apoptosis and necrosis. Stress from heat causes the
release of several inflammatory cytokines, which can precipitate a severe systemic
inflammatory response. In addition, heat directly injures the vascular endothelium, causing
increased vascular permeability, activation of the coagulation cascade, and disseminated
intravascular coagulation. Heat also may accelerate biochemical reactions, which in turn may
cause metabolic abnormalities.
Temperatures above 41.6°C (106.9°F) are considered to be above the critical thermal
maximum for humans and can cause cellular damage within hours of exposure. Temperatures
above 49°C (120°F) cause nearly immediate cell death and necrosis. Lower temperatures over
longer periods of time can cause the same degree of damage as higher temperatures over
shorter periods of time.
6. List the spectrum of heat illnesses and briefly describe.
n
Heat edema—transient swelling of hands, feet, and ankles due to water retention in a
nonacclimated person
n
Heat rash—prickly heat; maculo-papular rash caused by excessive sweating and blockage
of the sweat ducts; primarily occurs on parts of the body covered by tight clothing
