Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

638
CHAPTER 93
BURNS
Jeffrey S. Guy, MD
1. How should thermal burn patients be initially assessed in the ED?
Always start with the ABCs. Airway evaluation for inhalation injury is critical early in the
patient’s course. Assess respiratory status, and provide supplemental oxygen if necessary.
Evaluate for circulation and hemodynamic status with vital signs, pulses, and capillary refill.
The ABCs should be followed by a complete secondary survey including evaluation of burn
size and depth, associated trauma, and possible cervical spine injury. As with any ED patient,
past medical history, medications, allergies, and tetanus immunization status are also
important. Also, it is important to speak with the emergency medical service (EMS) transport
team to determine if the patient was trapped in an enclosed space or if exposure to toxic
substances is a concern.
KEY POINTS: TYPES OF BURNS COMMONLY SEEN IN THE ED
1. Thermal (most common)
2. Solar (i.e., sunburn)
3. Chemical
2. How do you evaluate for inhalation injury?
Risk factors for inhalation injury include flame burns, exposure to smoke in an enclosed
space, and associated trauma. Signs of possible inhalation injury are burns around the
face and mouth, soot in the nose or mouth, and carbonaceous sputum. Respiratory
symptoms such as dyspnea, hoarseness, wheezing, and stridor are highly suggestive of
inhalation injury.
3. How does smoke from a fire cause asphyxiation?
Two asphyxiates produced in fires include carbon monoxide (CO) and cyanide gas (CN)
(see Chapter 72). Both of these molecules cause cellular death from cellular hypoxia and
asphyxia. In these cases, the patient often has an airway and is capable of being ventilated,
but the tissues are not capable of utilizing the oxygen that is delivered to them. Portable
carbon monoxide monitors are available for use in the prehospital environment to aid in
the detection of CO. These monitors are helpful in evaluating both patients and firefighters.
Treatment of CO toxicity is removal from the source and administration of oxygen. When
the patient is placed on 100% oxygen, the half-life of CO-hemoglobin is reduced to 40 to
60 minutes.
Burning plastics and polyurethane produce cyanide gas. Patients with carbon
monoxide toxicity should be considered at risk for CN poisoning. A safe cyanide antidote,
hydroxocobalamin, is approved and available for prehospital and hospital use in the
United States and Europe.
4. Electrical
5. Radiation

Chapter 93 BURNS 639
4. What about thermal burns to the airway?
Because of the great capacity for heat dissipation in the oropharynx and nasopharynx, thermal
burns to the lower airways are uncommon except in the setting of steam inhalation. Direct
thermal burns to the airway are usually limited to the upper airway and present as mucosal
edema, erythema, and ulceration.
5. What are the indications for intubation in the burn patient?
Inhalation injury can produce a rapid progression of edema that can make orotracheal
intubation difficult or impossible. Evidence of airway involvement (voice changes, stridor,
wheezing, mucosal edema) or low oxygen saturation is an indication for observation in an
intensive care unit capable of providing advanced airway management or early intubation in
the ED. It should also be considered in patients with severe burns to the face and neck, even if
initial respiratory status is adequate.
6. Are there any specific issues related to intubation in the burn patient?
Again, early intubation is the key to avoiding complications of airway edema and possible crash
intubation. Orotracheal rapid-sequence intubation (RSI) is appropriate. Fiberoptic intubation can
be considered in the stable patient. Emergency cricothyrotomy may be necessary if airway edema
prevents orotracheal tube placement. Remember, many RSI drugs can contribute to hypotension.
Avoid complications with adequate fluid resuscitation and careful selection of RSI medications.
7. What about succinylcholine?
Succinylcholine is frequently reported as contraindicated in the burn patient due to changes in
muscle receptors that can cause hyperkalemia. These changes generally take place over the first
7 to 10 days after the burn. This is not a concern in the acute burn patient encountered in the ED.
8. What are some options for securing an endotracheal tube in a patient with
burns to the face?
Burned facial skin commonly shears off and weeps fluid, making adhesive tapes ineffective.
Loss of the airway in these patients can be catastrophic and require an emergent surgical
airway. Several commercial devices exist to secure these tubes. An effective alternative to
such commercial devices is to secure the endotracheal tube with umbilical tape or intravenous
tubing. The provider should use two ties to secure the tube. One tie should go over the ears
and one tie should drape under the ears. A common time for displacement of the airway is
with movement of the patient. For that reason, the position of the airway should always be
reconfirmed following each movement of the patient.
9. How is the burn injury evaluated?
Begin with a complete physical examination including the back and the perineum. Document
the locations burned and the depth of the burns.
n
First-degree burns involve only the epidermis and are erythematous and painful, without
blisters. They are usually described as looking like a sunburn. These do not count toward
the total body surface area (TBSA) when calculating the burn size.
n
Second-degree burns are characterized as superficial or deep partial-thickness burns. They
are painful, and their color can vary from red to mottled to pale. Blisters may be thin- or
thick-walled depending on the depth of the burn. Superficial partial-thickness burns are
erythematous and have thin-walled fluid-filled blisters. These usually heal in 2 to 3 weeks
without scarring. Deep partial-thickness burns extend further into the dermis, are usually
pale pink or mottled, and have thick-walled blisters. These burns will usually heal in 3 to
9 weeks but tend to develop hypertrophic scars; surgical treatment is usually necessary.
n
Third-degree burns involve all layers of the dermis. The skin is firm, white, or charred, and
is often described as “leathery.” This represents complete tissue destruction, and surgery is
necessary except in the smallest of third-degree burns.
n
Fourth-degree burns extend to deeper tissues including subcutaneous fat, muscle, and
bone. Significant debridement and reconstruction are required.
Chapter 93 BURNS640
10. What is so concerning about circumferential full-thickness burns?
As fluid leaks from damaged tissues into adjacent soft tissues, the leather-like full-thickness
burn prevents tissue expansion, thus causing compression of internal structures. Circumferential
burns of the neck can lead to compression of the jugular veins and increased intracranial
pressure or airway compromise. Circumferential burns of the chest can lead to decreased chest
wall compliance, increasing difficulty ventilating, and respiratory insufficiency. Circumferential
burns to the extremities can cause vascular compromise similar to compartment syndrome.
Evaluation of pulses and Doppler signals is absolutely necessary. Signs of poor perfusion to a
distal extremity are cyanosis, deep tissue pain, paresthesias, and cold skin. Prompt escharotomy
can be performed by the emergency physician or a surgeon.
11. After a thermal burn, what is the best method to stop the burning process?
The initial care of the burn patient is to stop the burning process. Remove clothing and jewelry
as these items will retain residual heat. The most effective cooling technique is irrigation with
copious amounts of room-temperature water. Immediate cooling with tap water (15º C) is
almost twice as effective in reducing temperature within burned tissue than application of a
product such as Melaleuca Alternifola hydrogel. Smaller burns that have been cooled have been
shown to have less cellular damage than those that are not cooled. Application of ice is
contraindicated. Ice will stop the burning process and provide analgesia but will increase the
extent of tissue damage. In fact, cooling the burn immediately with ice is more harmful than
application of tap water or no treatment at all. Too aggressive cooling will lead to tissue
damage, similar to what is experienced with frost bite. The hazard of cooling larger burns is
causing the patient to become hypothermic.
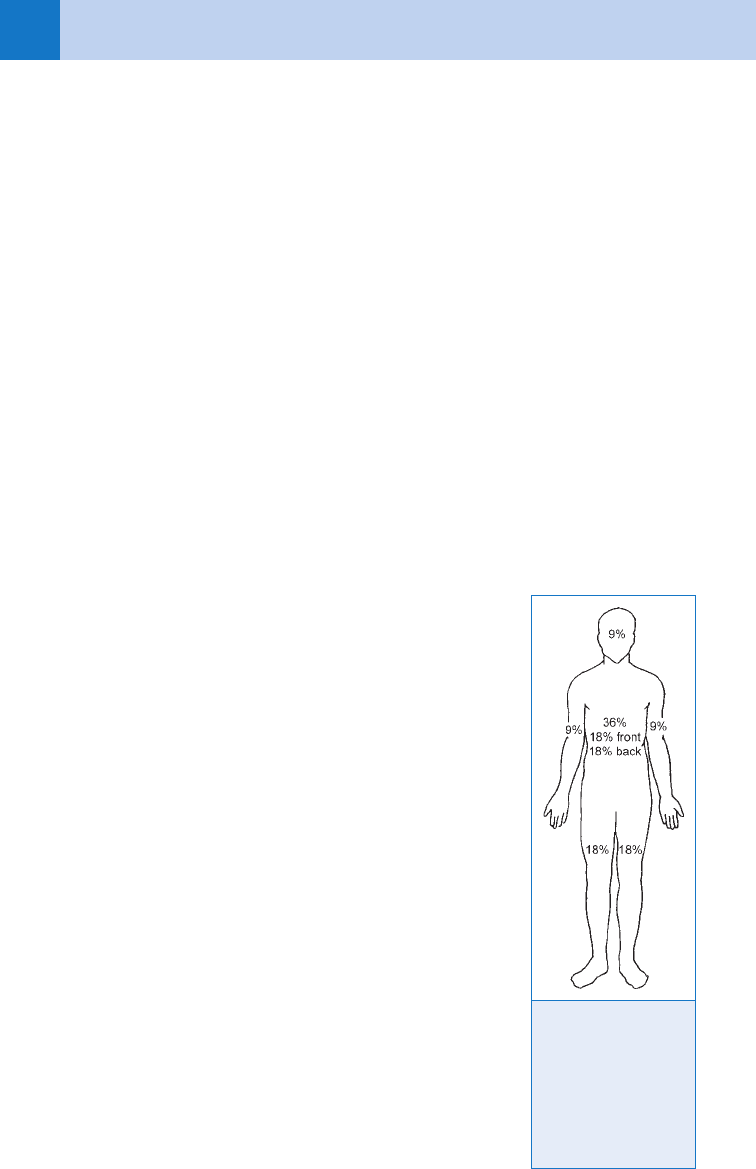
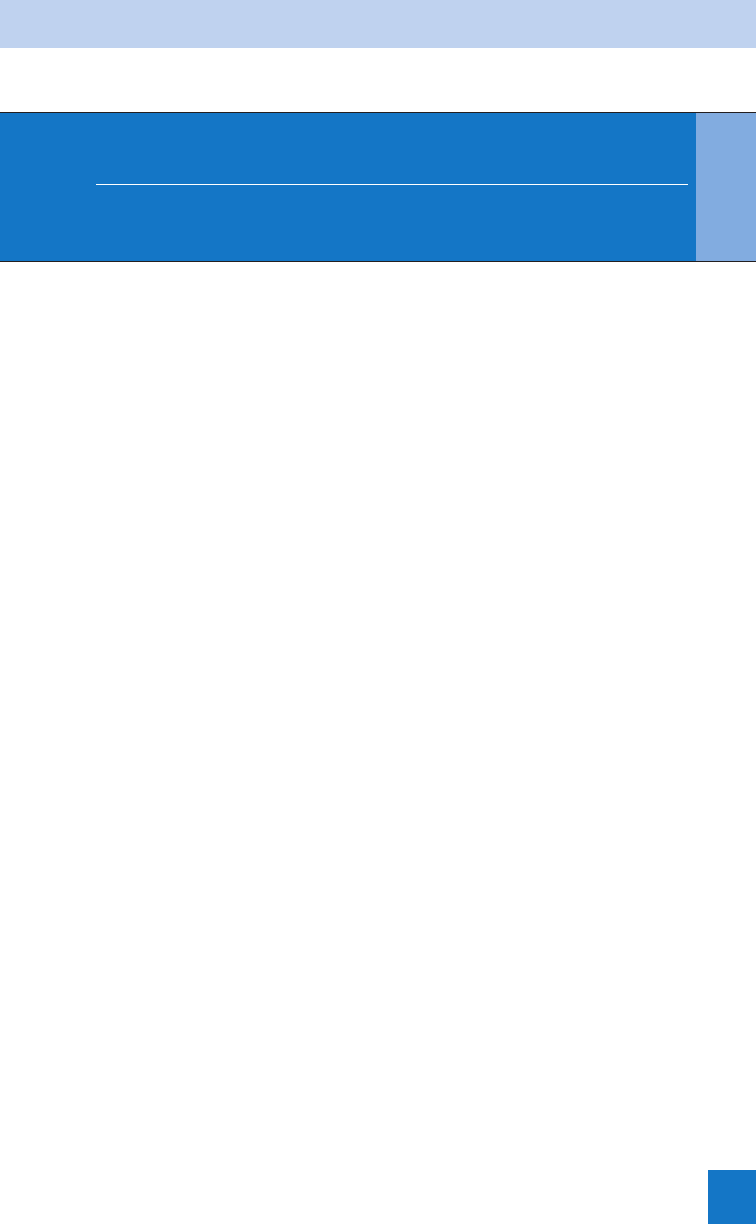
12. How is % TBSA burned calculated? Why is it important?
Estimation of the percentage of body surface area burned helps
direct fluid resuscitation, determines appropriate disposition of
the burn patient, and allows meaningful communication with
consultants and burn units. There are several methods to
estimate % TBSA burned. The rule of nines divides the regions
of the body into approximate percentages of total surface area
(Fig. 93-1). Due to differences in body proportions, the rule of
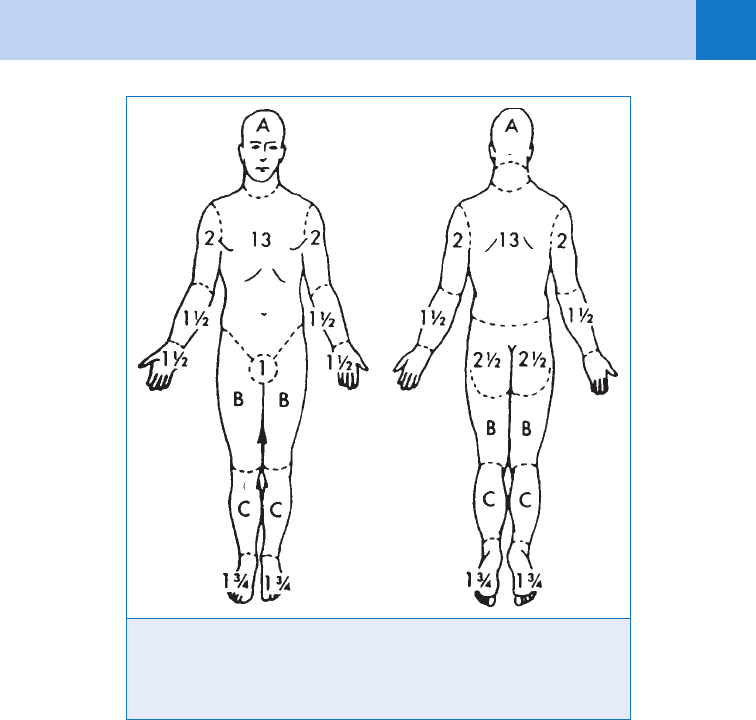
nines is not applicable to children. The Lund and Browder chart
has similar divisions but allows for variations in infancy and
childhood (Fig. 93-2). With either chart, document the areas of
second- and third-degree burns on the chart and calculate a total
percentage of TBSA burned.
13. What is burn shock?
Burn shock is a complex interaction of intravascular fluid loss
and release of vasoactive substances and inflammatory
mediators. Initial fluid loss is due to tissue destruction at the
burn site that causes increased vascular permeability. Fluid
shifts into the extravascular space and is quickly lost through
the damaged skin.
14. How do you determine appropriate fluid resuscitation
in the burn patient?
Following a burn injury, the patient has profound shifts in
intravascular fluids and an initial reduction in cardiac output.
Several formulas exist for the determination of fluid resuscitation
needs; however, the Parkland formula is the most well known
and most widely applied. The Parkland formula provides an
estimate of the initial fluid needs of the severely burned patient.
The fluid requirement (of lactated Ringer’s solution) is calculated
Figure 93-1.
Percentages used in
determining extent of
burn by rule of nines.
(From Miller RH:
Textbook of basic
emergency medicine,
ed 2, St. Louis, 1980,
Mosby.)
Chapter 93 BURNS 641
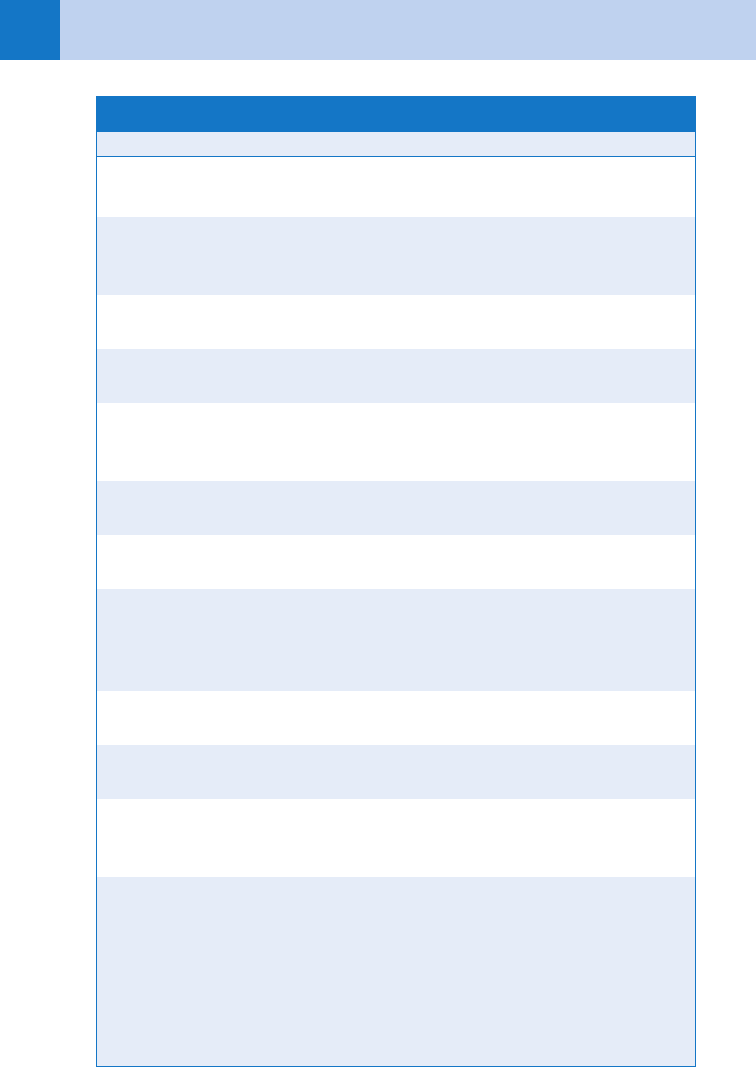
Figure. 93-2 Classic Lund and Bowden chart. The best method for determining
percentage of body surface burn is to mark areas of injury on a chart and then
compute total percentage according to patient’s age. (From Artz CP, Yarbrough DR
III: Burns: Including cold, chemical, and electrical injuries. In Sabiston DC Jr, editor:
Textbook of surgery, ed 11, Philadelphia, 1977, WB Saunders.)
for the first 24 hours. One half of this is administered over the first 8 hours. The second half
is administered over the following 16 hours.
Fluid required 5 body weight(kg) 3 %TBSA burn (second and third degree) 3 4 mL
Remember, this is an estimate. Monitor adequacy of fluid resuscitation by following vital
signs and urine output. Goal urine output is 30 mL/hr in adults and 1 to 2 mL/kg/hr in children.
(Do not forget the Foley catheter.)
15. Can you give me an example of using the Parkland formula?
Let’s use an example of an 80-kg patient who has sustained a 30% body surface area burn.
24-hour fluid total 5 4 mL/kg/% TBSA burn
5 4 mL/kg/% TBSA burn 3 80 kg 3 30% TBSA burn
5 9,600 mL
n
Once you have calculated the 24-hour fluid requirement, divide that number by two. Half
of that fluid should be given in the first 8 hours from injury, and the second half in the
next 16 hours.
n
Fluids given in the first 8 hours: 9,600 mL/2 5 4800 mL
n
To determine the hourly rate for the first 8 hours, divide this number by 8.
n
Fluid rate in first 8 hours 5 4,800 mL/8 hours 5 600 mL/hr
n
The fluid rate for hours 8 to 24 is calculated by dividing 9,600 mL by 16.
n
Fluid rate for hours 8 to 245 4,800 mL/16 hours 5 300 mL/hr
Chapter 93 BURNS642
16. Are there any pitfalls with using the Parkland formula?
Yes, there are some common pitfalls with fluid resuscitation. The first is that a formal
Parkland fluid resuscitation is not required for burns less than 20% TBSA. Another detail
concerns those patients who may present to the ED several hours after injury. For example,
if the patient presented earlier were to arrive to the ED 2 hours after injury not having
received any resuscitative fluids, then the provider would need to recalculate the fluid rate
for the fluid to be given for the first 8 hours after injury. The first half of the fluids should
be administered within 8 hours from the time of the injury, not from the time after
presentation. Therefore, if the patient presents two hours after injury, the initial fluid
requirement would now have to be given over the remaining 6 hours, and the rate for fluid
resuscitation would be:
n
Fluid resuscitation hours 2 to 85 4,800 mL/6 hours 5 800 mL/hr
n
The fluid rate for remaining 16 hours would remain at 300 mL/hr
17. How do you manage a patient with burns and trauma?
Patients with combined burns and trauma are at greater risk for morbidity and mortality
than either alone. These patients are at higher risk for inhalation injury and tend to require
greater fluid resuscitation than isolated burn patients. Generally, aggressive burn
resuscitation should be started, and life-threatening traumatic injuries should be treated
initially. Transfer to a burn unit can be delayed until the traumatic injuries have been
stabilized.
18. What are the criteria for referral to a burn center?
The American Burn Association has developed a list of criteria that warrant referral to a
specialized burn unit. Their website also contains a list of verified burn centers. Referral does
not always require transfer to the burn unit but may include instruction in wound treatment or
plans for follow-up.
n
Partial-thickness burns . 10% TBSA
n
Burns that involve the face, hands, feet, genitalia, perineum, or major joints
n
Third-degree burns
n
Electrical burns, including lightning injury
n
Chemical burns
n
Inhalation injury
n
Burns in patients with preexisting medical disorders that could complicate management,
prolong recovery, or affect mortality
n
Any patient with burns and concomitant trauma in which the burn injury poses the greatest
risk of morbidity or mortality
n
Burned children in hospitals without qualified personnel or equipment for the care of
children
n
Burn injury in patients who will require special social, emotional, or long-term rehabilitative
intervention
19. Are there any burns that can be managed in the outpatient setting?
Partial-thickness burns involving less than 10% TBSA or full-thickness burns involving less
than 2% TBSA without risk of functional or cosmetic complications can usually be treated as
an outpatient.
20. How are outpatient burns treated in the ED?
All burns should be cleaned with saline or water and a mild cleanser. Ruptured blisters should
be débrided. There is controversy in the burn community over treatment of intact blisters;
most sources recommend débridement of the blister or aspiration of the fluid to prevent
infection of the blister fluid. Topical antibiotics such as bacitracin ointment or silver
sulfadiazine should be applied liberally and covered with a nonadhesive dressing and a bulky
bandage. The patient should follow up in 24 hours in the ED or with a physician experienced
Chapter 93 BURNS 643
in burn care. If there are any questions concerning outpatient management, consultation with
a burn center is appropriate.
21. Is there anything special about facial burns?
Facial burns should not be treated with silver sulfadiazine because it can cause pigmentation
changes in the healing tissue. Antibiotic ointment alone, without dressings, is adequate for
facial burns. Again, follow-up in 24 hours is recommended.
22. What about pain control?
Burns are painful, and large doses of narcotics are sometimes necessary. Intravenous
narcotics can be started in the field and repeated if needed. Adequate pain control may require
substantial doses of pain medications. These should only be withheld if administration is life
threatening due to hemodynamic status. Also, don’t forget to provide adequate oral analgesics
for outpatient management. Superficial partial-thickness burns can be the most painful.
23. Should I check tetanus immunization status?
Always check the status of tetanus immunization and update if needed.
24. What are the special considerations in burn care in children?
Children younger than 2 years have increased morbidity and mortality from burns. Consider
admission even in minor burns in this age group. Do not forget the possibility of
nonaccidental trauma. Twenty percent of pediatric burns are the result of intentional burn
injury. Ask about conditions around the home, and assess for safety. The reliability of the
parents is another consideration in evaluating need for inpatient management of a pediatric
burn. Do not forget that any suspicion of child abuse must be reported to child protective
services.
25. How can I recognize intentional burns in children?
The most common form of intentional burn injury in children is forcible immersion. These
types of injuries commonly occur when an adult places a child in hot water as a form of
punishment, often associated with toilet training. These children will commonly have second-
and third-degree burns of the hands and feet in a glove or stocking type pattern. These
injuries are especially suspicious when the burns are symmetrical and lack splash patterns.
When a child is lowered into hot water, the child will assume a defensive posture tightly
flexing their arms and legs. These burns will produce sparing of the flexion creases in the
antecubital fossa, popliteal fossa, and groins.
Contact burns are the second most common form of burn-related child abuse. Accidental
contact burns typically have irregular burn depth and edges. This is because dropped hot
objects will often strike and deflect off the curvature of the various body surfaces. With
intentional contact burns, the instrument causing the burn is typically pressed onto the body
surface. This therefore produces a burn pattern that has sharp lines of demarcation.
26. What are the special considerations in adults?
Past medical history is important. Patients with HIV, immune suppression (transplants,
steroids), diabetes, cardiac disease, chronic obstructive pulmonary disease (COPD), or
substance abuse may all require inpatient management of minor burns to monitor and treat
complications of the chronic disease. Also, burn patients older than 60 years are at increased
risk of morbidity and mortality from their injuries.
WEBSITE
American Burn Association: www.ameriburn.org
Chapter 93 BURNS644
BIBLIOGRAPHY
1. American Burn Association: Guidelines for the Operations of Burn Units, Resources for Optimal Care of the
Injured Patient: Committee on Trauma, American College of Surgeons, 1999.
2. Chadwick DL: The diagnosis of inflicted injury in infants and young children. Pediatr Ann 21:477, 1992.
3. de Camara DL, Robinson MC: Ultrastructure aspects of cooled thermal injury. J Trauma 21: 911–919, 1981.
4. Edlich RF, Bailey TL, Bill TJ: Thermal burns. In Marx JA, Hockberger RS, Walls RM, et al, editors: Rosen’s
emergency medicine: concepts and clinical practice, ed 5, St. Louis, 2002, Mosby, pp 801–812.
5. Hight DW, Bakalar HR, Lloyd JR: Inflicted burns in children: recognition and treatment, JAMA 242:517, 1979.
6. Holmes JH, Heimbach DM: Burns. In Brunicardi FC, Andersen DK, Billiar TR, et al, editors: Schwartz’s
principles of surgery, ed 8,. New York, 2004, McGraw Hill, pp 189–204.
7. Houeto P, Borron SW, Sandouk P, et al: Pharmacokinetics of hydroxocobalamin in smoke inhalation victims.
J Toxicol Clin Toxicol 34:397, 1996.
8. Jandera V, Hudson DA, de Wet PM, et al: Cooling the burn wound: evaluation of different modalities. Burns
26:265–270, 2000.
9. Kao CC, Garner WL: Acute burns. Plast Reconstr Surg 105:2482–2493, 2000.
10. Mellins RB, Park S: Respiratory complications of smoke inhalation in victims of fires. J Pediatr 87:1, 1975.
11. Santaniello JM, Luchette FA, Esposito TJ, et al: Ten year experience of burn, trauma, and combined burn/
trauma injuries comparing outcomes. J Trauma 57:696–701, 2004.
12. Sauer SW, Keim ME: Hydroxocobalamin: improved public health readiness for cyanide disasters, Ann Emerg
Med 37:635, 2001.
13. Sawada Y, Urushidate S, Yotsuyanagi T, et al: Is prolonged and excessive cooling of a scalded wound
effective? Burns 23(1):55–58, 1997.
14. Schwartz LR, Balakrishnan C: Thermal burns. In Tintinalli JE, Kelen GD, Stapczynski JS, editors: Emergency
medicine: a comprehensive study guide, ed 6, New York, 2004, McGraw-Hill, pp 1220–1226.
15. Sheridan RL: Burns. Crit Care Med 30(11 suppl):S500–S514, 2002.
16. Sheridan RL: Burn care: results of technical and organizational progress. JAMA 290:719–722, 2003.
ACKNOWLEDGMENT
The editors thank Michelle Tartaglia, MD, for her contributions to this chapter in the previous edition.
645
CHAPTER 94
WOUND MANAGEMENT
Maria E. Moreira, MD, and Vincent J. Markovchick, MD, FAAEM, FACEP
1. Why is wound management important?
Annually, approximately 12 million traumatic wounds are treated in EDs across the United States
constituting about 10% of all ED visits. Patients often judge the competency of a physician
based on the ultimate functional or cosmetic result of the wound repair and the development of
complications.
2. What is the difference between functional and cosmetic closure?
Functional closure is closure of a wound prioritizing returning the injured part to full function.
A cosmetic repair prioritizes obtaining the least amount of scarring.
3. How do I remember what steps to take when repairing a wound?
Use the mnemonic LACERATE:
L 5 Look. Evaluate the wound to determine the most appropriate closure. Examine thoroughly
for movement, sensation, and pulsation distal to the wound.
A 5 Anesthetize.
C 5 Clip and clean. Clipping hair leads to less infection than shaving. Methodical irrigation is
the best way to decrease infection risk.
E 5 Equipment. Have everything needed for repair at the bedside, including laceration kit,
sterile gloves, suture material, and dressing.
R 5 Repair. Perform the repair. Devitalized tissue may need to be débrided.
A 5 Assess results. Reevaluate the wound when the repair is near completion to determine
the need for additional sutures.
T 5 Tetanus. Give tetanus prophylaxis for dirty or contaminated wounds when the patient
has not had a booster in 5 years or for clean wounds when the patient has not had a
booster in 10 years.
E 5 Educate. Educate the patient on how to care for the wound, signs of infection, and the
timing of suture removal.
4. Which factors increase the visibility of scars and compromise wound healing?
How are they minimized?
See Table 94-1.
5. What aspects of history should be obtained in a patient with a traumatic wound?
The time, setting, and mechanism of injury are essential to determine whether the wound is
contaminated, the possibility of foreign body, or the potential for infection. The patient’s
current medications and immune status (AIDS, diabetes, chemotherapy), the patient’s
occupation, and dominant hand if a hand injury has occurred are important. The patient’s
tetanus immunization history and allergies (specifically regarding anesthetics, antibiotics, or
latex gloves) must be obtained.
6. What are the most important aspects of the physical examination?
To perform an adequate examination, it is important to be familiar with underlying anatomy,
especially in the regions of the face, neck, hands, and feet. Examination of the injured site
should begin with identification of any motor, sensory, and vascular deficits. With extremity
Chapter 94 WOUND MANAGEMENT646646
From Markovchick V: Suture materials and mechanical after care. Emerg Med Clin North Am 10:
673–689, 1992.
Contributing Factors Methods to Minimize Scarring
Direction of wound (e.g., perpendicular
to lines of static and dynamic tension)
Layered closure; proper direction in
elective incisions of wound
Infection necessitating removal of
sutures débridement, resulting in healing
by secondary intention and a wide scar
Proper wound preparation; irrigation and
use of delayed closure in contaminated
wounds
Wide scar secondary to tension Layered closure; proper splinting and
elevation
Suture marks Removal of percutaneous sutures within
7 days
Uneven wound edges resulting in
magnification edges and of scar by
shadows
Careful, even approximation of wound
top layer closure to prevent differential
swelling of edges
Inversion of wound edges Proper placement of simple sutures or
use of horizontal mattress sutures
Tattooing secondary to retained dirt or
foreign body
Proper wound preparation and
débridement
Tissue necrosis Use of corner sutures on flaps, splinting,
and elevation of wounds with marginal
circulation or venous return; excise
nonviable wound edges before closure
Compromised healing secondary to
hematoma
Use of properly conforming dressing
and splints
Hyperpigmentation of scar or abraded
skin
Use of 15 or greater SPF sunblock for
6 months
Superimposition of blood clots between
healing frequent wound edges
Proper hemostasis and closure; H
2
O
2
swabbing; proper application of com-
pressive dressings
Failure to align anatomic structures
properly such as vermilion border
Meticulous closure and alignment;
marking or placement of alignment
suture before distortion of wound edges
with local anesthesia; use of field block
TABLE 94–1 MINIMIZING FACTORS THAT INCREASE VISIBILITY OF SCARS
Chapter 94 WOUND MANAGEMENT 647
injuries, examination can be conducted in the absence of hemorrhage by temporarily inflating
a sphygmomanometer or placement of a finger tourniquet proximal to the injury. Palpation of
the bones adjacent to the site of injury may detect instability or point tenderness from an
underlying fracture. Direct inspection and visualization always should be performed when
there is a suspicion of a tendon or joint capsule injury or presence of a foreign body.
7. What is the most important step I can take to prevent infection?
1. For all traumatic wounds, irrigation with normal saline at least 8 psi should be done with an
18- or 19-gauge needle and a 30-mL syringe. The optimal volume of irrigant has not been
determined; however, 50 mL to 100 mL per centimeter of wound length has been used as a
guideline. In the presence of gross contamination, copious irrigation should be done and
débridement considered. Tap water is a reasonable alternative for wound irrigation.
Detergents, hydrogen peroxide, and concentrated povidone-iodine should not be used for
irrigation because they are toxic to tissues. Exploration; débridement when indicated;
hemostasis; and proper repair, dressing, and immobilization are essential adjuncts for proper
wound management. Antibiotics have no proven prophylactic benefit in the normal host. For
contaminated or dirty extensive wounds, a mechanical irrigation device should be used to
remove all dirt and decrease the bacterial count. A stiff brush such as a toothbrush or sharp
débridement should be used to remove dirt that remains after irrigation.
8. Which anesthetic agent should be used for local anesthesia?
Selection of an appropriate anesthetic depends on many factors, including age of the patient,
underlying health, prior drug reactions, wound size and location, and practice environment in
the ED. Lidocaine traditionally has been the standard agent for local anesthesia in the ED;
however, bupivacaine has advantages over lidocaine, related mainly to duration of anesthesia.
Patients receiving bupivacaine experience significantly less discomfort during the 6-hour
postinfiltration period. Also, in a busy ED, use of bupivacaine may prevent the need to
reanesthetize a wound when repair has been interrupted by the arrival of a higher acuity
patient.
9. What causes the pain of local anesthetic infiltration, and how can it be
prevented?
Pain from anesthetic infiltration is caused by distention of tissue from too-rapid injection with
too large a needle directly into the dermis. The acidity of the agent also contributes to the
pain. Pain from infiltration can be minimized by injecting slowly, subcutaneously, with a small,
25- or 27-gauge needle, directly through the wound margins. Buffering the anesthetic agent
with 1 mL of sodium bicarbonate for every 10 mL of lidocaine also can help to reduce pain.
However, bupivacaine does not lend itself to buffering because it precipitates as its pH rises.
Another efficacious and inexpensive method of decreasing the pain of infiltration is by
warming the anesthetic.
10. What is the toxic dose of lidocaine and bupivacaine?
Table 94-2 summarizes the maximum dose and duration of action of lidocaine, bupivacaine,
and procaine, alone and in combination with epinephrine. When calculating the dose of
milligrams infiltrated, 1 mL of 1% lidocaine 5 10 mg of lidocaine and 1 mL of 0.25%
bupivacaine 5 2.5 mg of bupivacaine. Lower maximal doses should be used for patients with
chronic illness, for very young or very old patients, or when infiltrating highly vascular areas
or mucosa.
11. Describe the presentation of lidocaine toxicity.
In general, toxicity should not occur unless the recommended dosing is met or exceeded. The
caveat to that statement is that toxicity may take place at lower than maximal doses when
infiltrating highly vascular areas or mucous membranes or in patients who are at the extremes
of age or chronically ill. The main effects are on the central nervous and cardiovascular
systems. Central nervous system effects present as lightheadedness, nystagmus, and sensory
