Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

594 Section VII • Pancreas
Cystojejunostomy
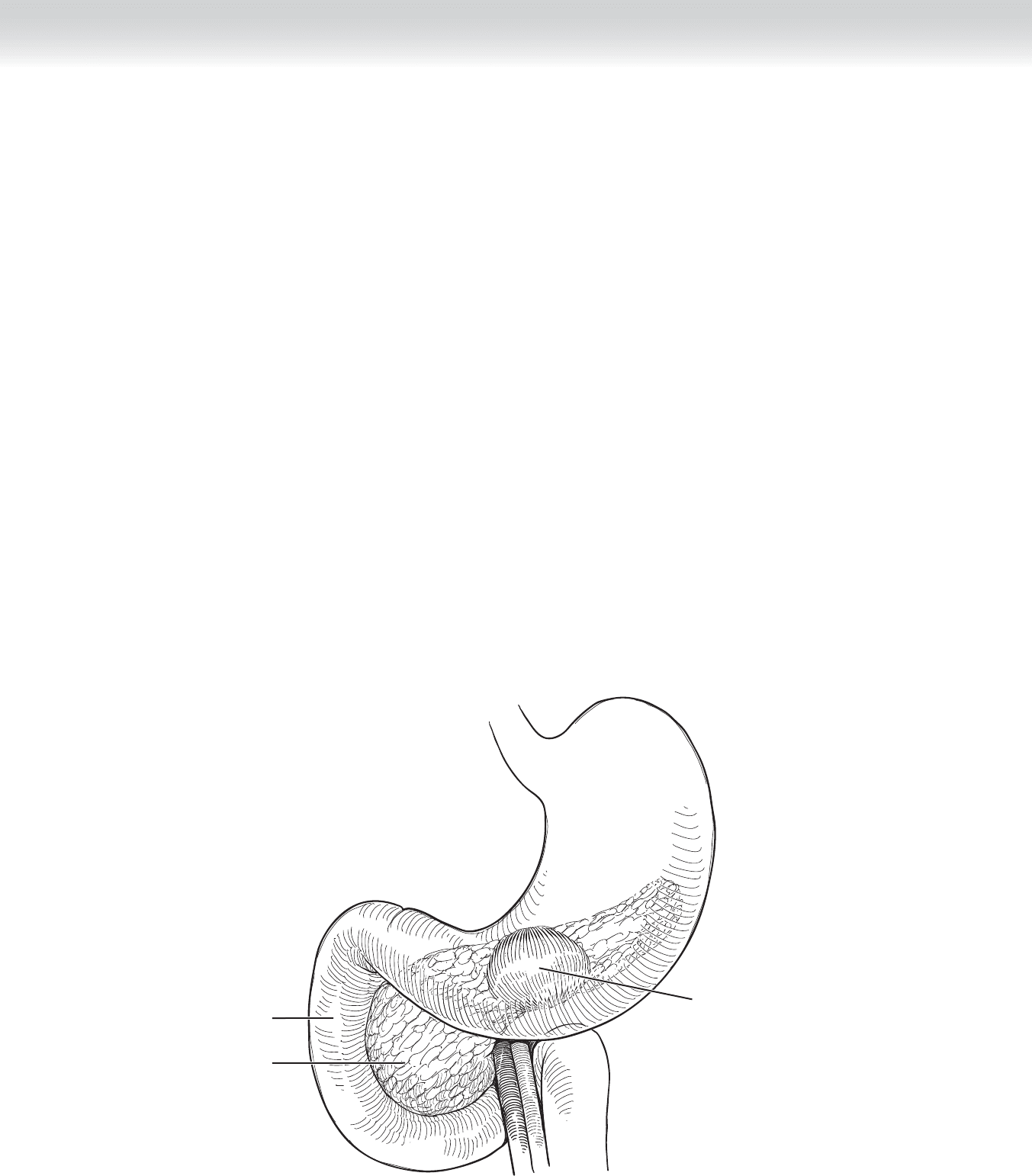
◆ When the decision is made to proceed to a cystojejunostomy (our procedure of choice), a
Roux-en-
Y reconstruction is required. Although this reconstruction can be used for pseudocysts
and any number of locations it really is the only option for pseudocyst in the mid-pancreas
without any clear shared plane with the posterior wall of the stomach (Figure 51-19).
◆ Once again, we typically perform this procedure by entering the lesser sac. This is achieved
by dividing the attachments between the gastrocolic omentum and the transverse colon.
We begin this dissection to the left of the spine and extend it over to the hepatic fl exure
(Figure 51-20). If this access point is achievable, one may expose the anterior surface of the
pancreas, and in most cases, the pseudocyst will be identifi ed and palpable in this area. Care
should be taken if extensive adhesions are encountered between the posterior wall of the
stomach and the pseudocyst. However, it is not necessary to completely skeletonize the cyst
(Figure 51-21). Once an acceptable exposure of the cyst has been performed in the lesser sac,
one may then place an angiocatheter into the cyst to confi rm the presence of cyst fl uid.
Finally, an incision for a length of approximately 3 cm is performed transversely, and a large
amount of fl uid typically is removed.
◆ Any solid material in the cyst is removed and cultures are routinely obtained.
Duodenum
Pseudocyst
Stomach
Pancreas
FIGURE 51 –19
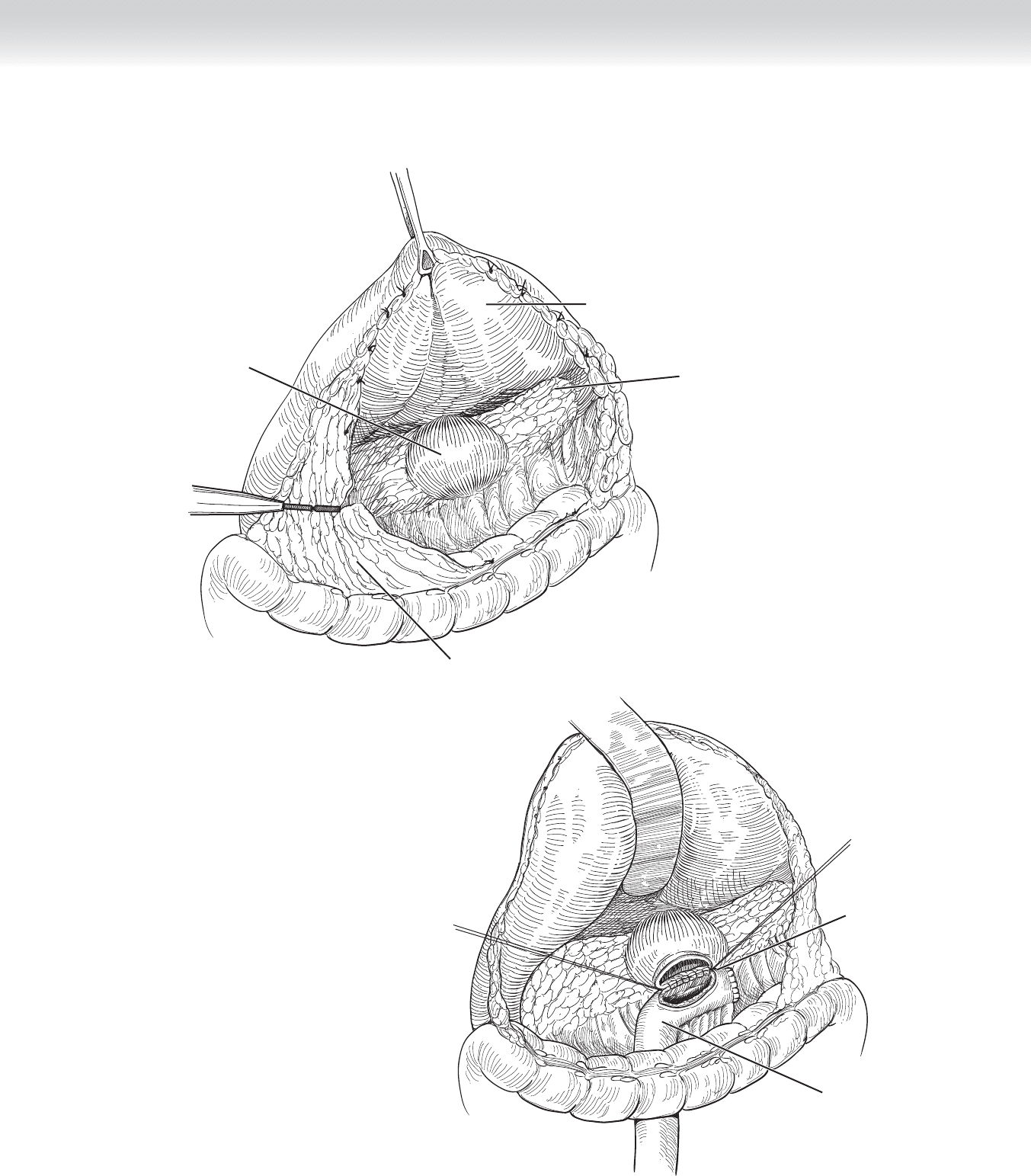
Pseudocyst
Gastrocolic attachments divided
Stomach
Pancreas
FIGURE 51 –20
Interrupted
3-0 sutures
Roux-en-Y limb
FIGURE 51 –21
CHAPTER 51 • Pseudocysts 595
596 Section VII • Pancreas
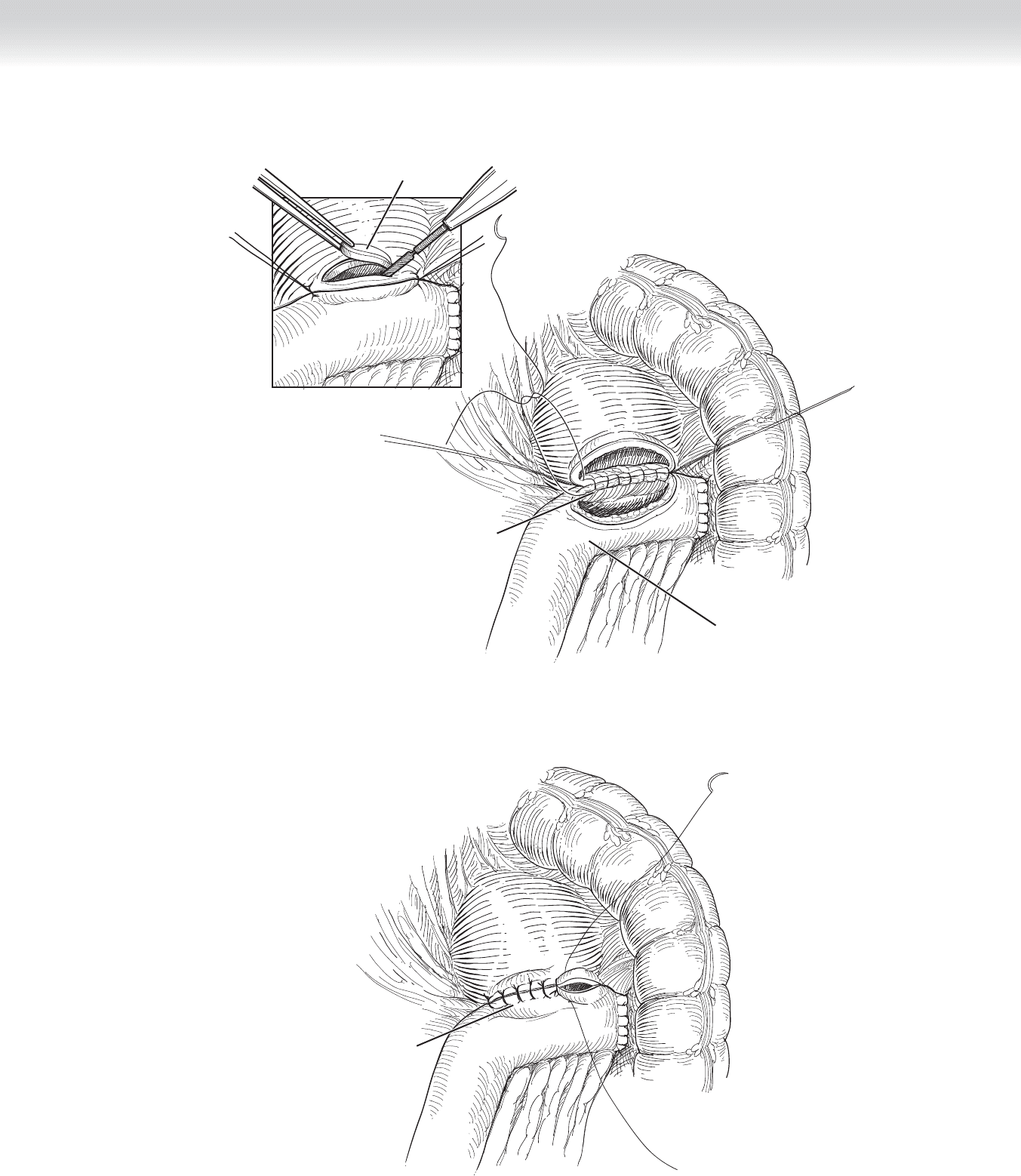
◆ An area is chosen in the proximal jejunum approximately 15 cm distal to the ligament of
Treitz. This is divided using a gastrointestinal anastomosis (GIA) stapling device, and mes-
entery is divided vertically toward the base of the mesentery to provide adequate length of
jejunum to reach the pseudocyst. The distal end of the divided jejunum is brought up to
the opening in the pseudocyst (see Figure 51-21). A single layer of 3-0 silk interrupted su-
ture is used to fi rst attach the jejunum to the inferior border of the open cyst before incising
the jejunum (see Figure 51-21), and subsequently the anterior edge is similarly closed
(Figure 51-22).
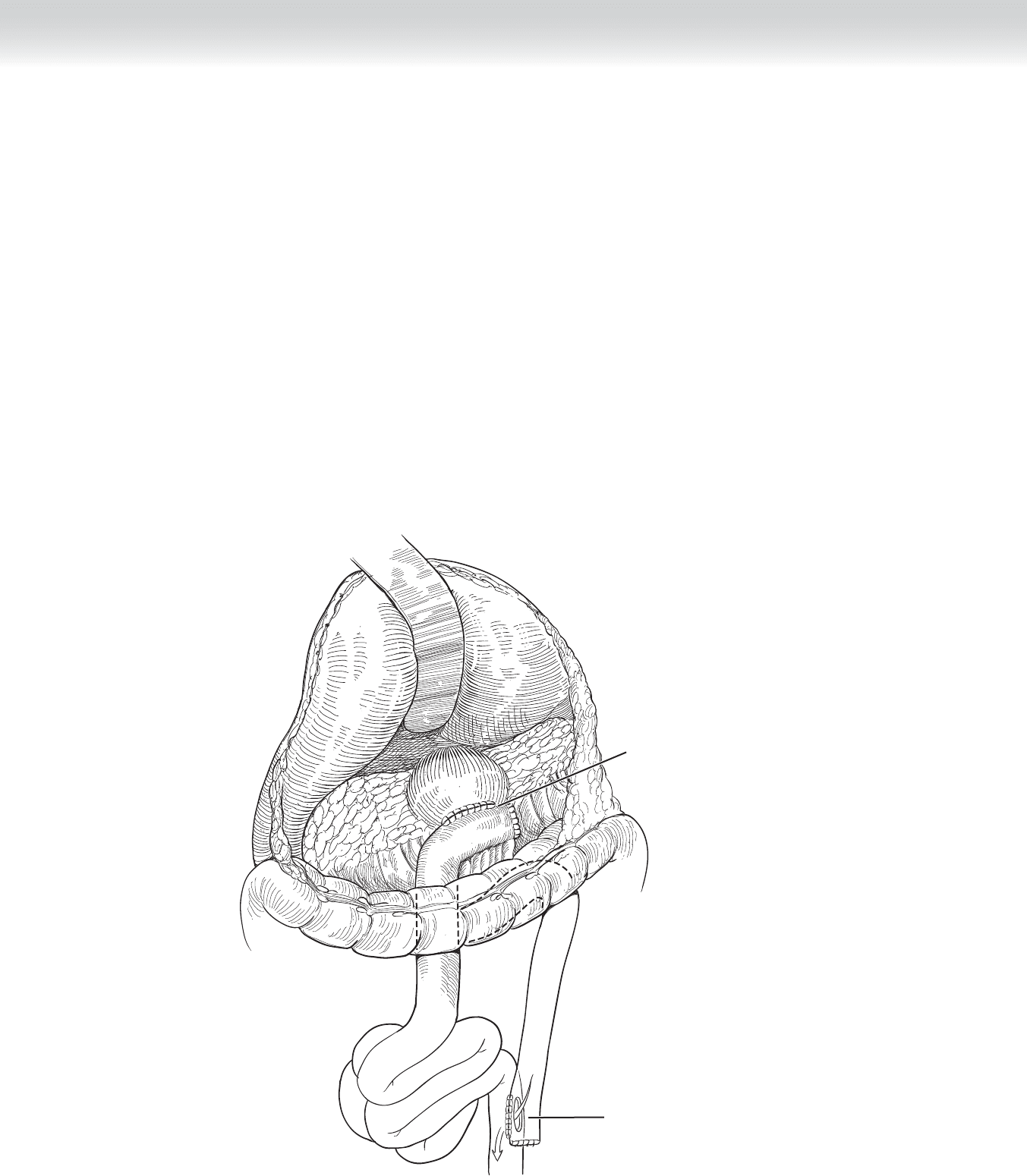
◆ After this has been completed, a jejunojejunostomy is performed approximately 40 cm dis-
tal to the cystojejunostomy in a side-to-side fashion in two layers, with an outer layer of
interrupted 3-0 silk stitch and an inner layer of running locking 3-0 Vicryl stitch on the
posterior wall. This is converted to a Connell type of stitch anteriorly. The rent in the mes-
entery, if one was used, is then reapproximated using 3-0 silk stitch, and any mesentery
defect created by the jejunojejunostomy limb is reapproximated using 3-0 silk stitch (see
Figure 51-22).
Completed
cystojejunostomy
End-to-side
jejunostomy
FIGURE 51 –22
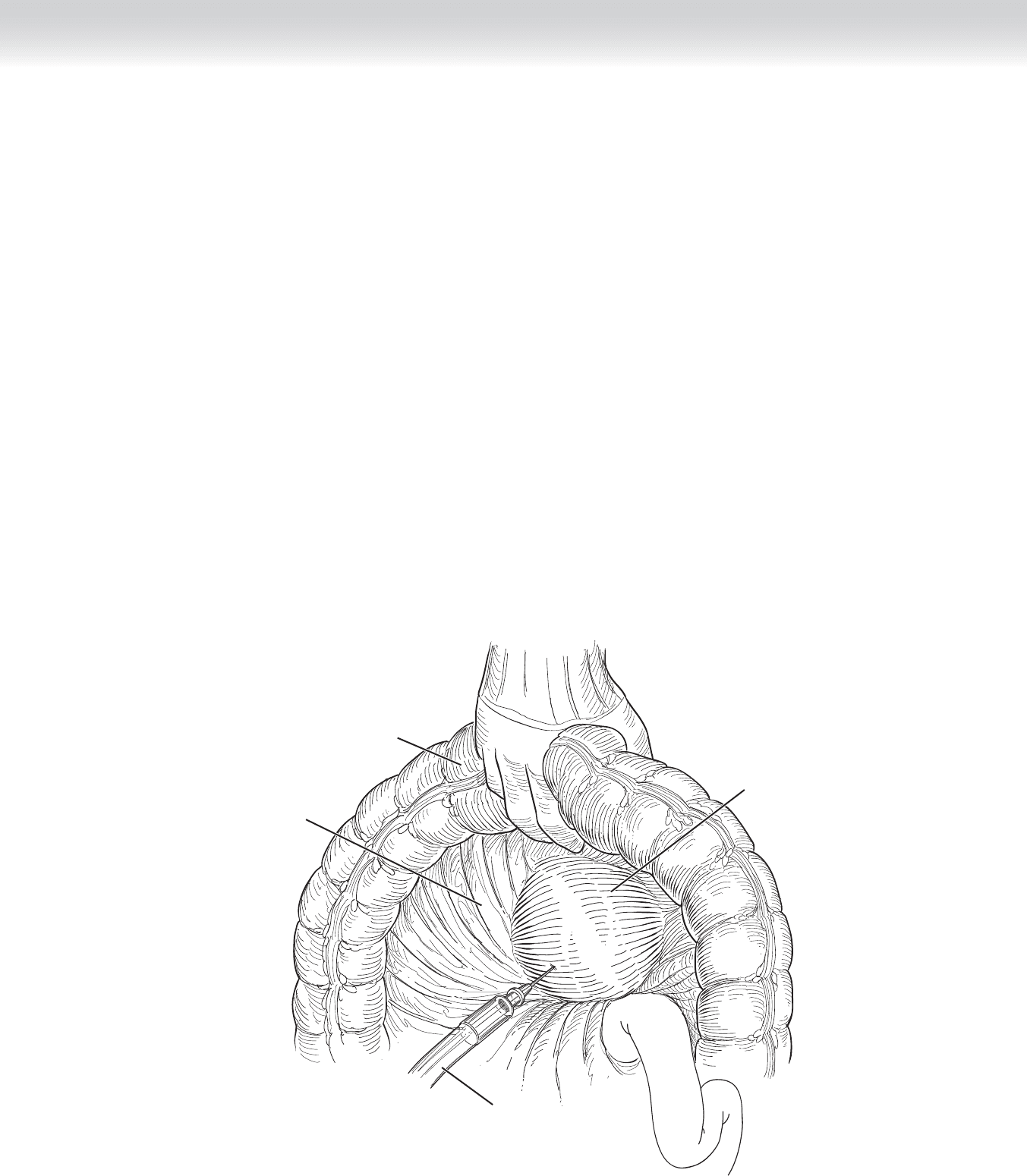
◆ In the event that one cannot easily access the lesser sac, we will occasionally resort to an
incision through the transverse mesocolon into the cyst. We will at times use intraoperative
ultrasound to facilitate this access point (Figure 51-23).
◆ After adequately palpating through the transverse mesocolon, one will use an angiocatheter
to confi rm the access to the cyst and, by palpation, will determine that there are no signifi -
cant mesenteric vessels in the line of dissection. In this case, some of the fat of the mesen-
tery may be carefully divided, and after palpating the wall of the cyst, one may make an in-
cision into the cyst following the path of the angiocatheter. A length of approximately 3 cm
is achieved.
Mesocolon
Angiocatheter
Transverse colon
Pseudocyst under
mesocolon
FIGURE 51 –23
CHAPTER 51 • Pseudocysts 597

598 Section VII • Pancreas
◆ Once again a limb of jejunum is chosen approximately 15 cm distal to the ligament of Treitz.
The limb of jejunum is brought to the incision in the cyst, and a side-to-side anastomosis is
begun to approximate the jejunum to the cyst (Figure 51-24). Again, a cystojejunostomy is
performed in one layer using interrupted 3-0 silk stitch. If not yet performed, a biopsy is
taken of the wall of the cyst and sent for frozen section evaluation (see Figure 51-24).
◆ Although we do not advocate a two-layer anastomosis to the pseudocyst, this variation has
been described. In this case, both layers will be nonabsorbable suture. The inner layer is
placed, and then a second layer of interrupted 3-0 silk is placed. Finally, the entire two-
layer anastomosis is completed (Figure 51-25).
◆ No drains are applied. The fascia is closed in the normal fashion. The skin is closed using
subcuticular stitches.
STEP 4: POSTOPERATIVE CARE
◆ Pain management may be a signifi cant issue in some patients, and this at times will require
epidural analgesia.
◆ Patients should be monitored for hemorrhage or for glucose intolerance in the fi rst 24 hours.
◆ A nasogastric tube will typically be used but will be removed on the fi rst day. Liquid diet
will be advanced to regular diet.
◆ We do not advocate continued antibiotics, although it should be understood that many re-
ports on the surgical management of pseudocysts quote rather high rates of complications,
many infectious. So certainly a level of surveillance for signs of infection should be used.
Interruped
3-0 sutures
Biopsy
Roux-en-Y limb
Interrupted
3-0 sutures
FIGURE 51 –24
FIGURE 51 –25
CHAPTER 51 • Pseudocysts 599

600 Section VII • Pancreas
STEP 5: PEARLS AND PITFALLS
◆ As stated before, we advocate several precepts in arriving at the decision to proceed to
intervention.
◆ We particularly point out the signifi cance of time since development of the pseudocyst. The
literature on nonoperative modalities often describes interventions earlier than 4 weeks after
the initial event. The reason to avoid such a decision early is that the texture of the pseudo-
cyst will be unsuitable for holding a suture. We further believe that a percentage of these
patients will have complete resolution of the pseudocyst if given enough time to do so.
◆ Once the decision is made to proceed to intervention, we advocate obtaining pancreatic
ductal anatomy defi ned by either endoscopic retrograde cholangiopancreatography (ERCP)
or magnetic resonance cholangiopancreatography (MRCP). We have developed a system to
categorize the ductal changes seen in patients with pseudocyst; and type II (stricture),
type III (complete obstruction), and type IV (chronic pancreatitis) are likely best managed
by surgery, whereas type I (normal duct) is ideally suited to nonoperative interventions.
◆ We advocate cystojejunostomy and infrequently use cystoduodenostomy.
◆ Be prepared that some pseudocysts will be diffi cult to locate during operation. Intraopera-
tive ultrasound can be very helpful in this situation. If in doubt, always aspirate with a fi ne
needle before attempting to incise the wall of the presumed pseudocyst.
◆ We have published the observation that persistent fl uid collections after acute necrotizing
pancreatitis are often rigid-walled and irregular in contour. These have been called “orga-
nized pancreatic necrosis,” although the terminology is still evolving. Because of the rigid
wall, these fl uid collections will not collapse when drained. In our experience, this has re-
sulted in a higher frequency of postoperative infection and in a prolonged period before all
symptoms resolve. If you are managing such patients, the radiographs will always be read
as pseudocyst, and the surgeon must be prepared to make that distinction based on the his-
tory of each individual patient.
SELECTED REFERENCES
1. Nealon WH, Walser E: Main pancreatic ductal anatomy can direct choice of modality for treating pancre-
atic pseudocysts (surgery vs. percutaneous drainage). Ann Surg 2002;235:751-758.
2. Nealon WH, Walser E: Duct drainage alone is suffi cient in the operative management of pancreatic pseu-
docysts in patients with chronic pancreatitis. Ann Surg 2003;237:614-622.
3. Nealon WH, Bhutani M, Riall TS, et al: A unifying concept: Pancreatic ductal anatomy both predicts and
determines the major complications resulting from pancreatitis. J Am Coll Surg 2009;208:790-799.

602
STEP 1: SURGICAL ANATOMY
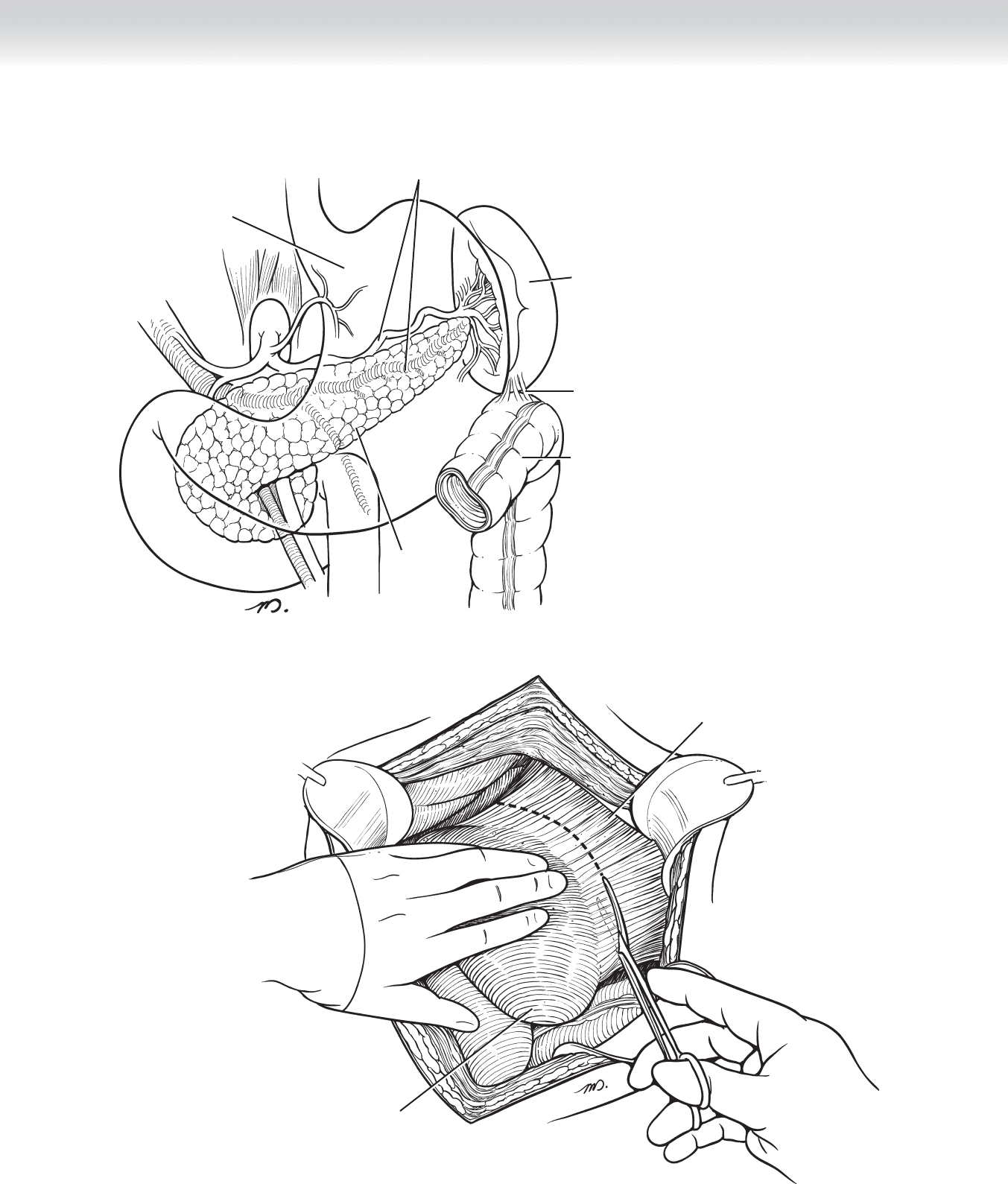
◆ The vascular supply of the spleen is composed primarily of the splenic artery and vein and
the short gastric vessels. Primary anatomic consideration in treating spleen injuries is related
to mobilization of the retroperitoneal attachments of the spleen, the splenocolic, splenorenal,
and splenophrenic ligaments (Figures 52-1 and 52-2).
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ Nonoperative management of spleen injuries is applicable to most patients who present in
hemodynamically stable condition, and the diagnosis of injury is most often made as a re-
sult of computed tomographic (CT) scanning. Under these conditions the success rates for
nonoperative therapy is very high, more than 80% in most modern series. Bed rest in the
intensive care unit (ICU) should be prescribed, serial complete blood counts obtained, and
serial abdominal examinations performed in an ICU for 24 to 48 hours. Hemodynamic de-
terioration or the development of peritonitis is typically considered indications to alter to
an operative treatment mode. Some centers have reported success in controlling hemor-
rhage from both liver and spleen injuries with angioembolization, but this requires prompt
availability of the interventional radiologists, which may not be applicable in many situa-
tions. There is no clear defi nition of what transfusion requirement merits abandonment of
nonoperative treatment or how far to allow the hemoglobin to fall in these cases before
transfusion and/or operative intervention. In most instances, however, persistent hemor-
rhage is manifest in the fi rst 24 hours, with progressive reduction in hemoglobin levels at 6,
12, and 18 hours after injury or episodes of hypotension. The development of peritonitis is
another clear indication for operative intervention.
◆ Because most patients with spleen injuries who undergo surgery are those who present he-
modynamically unstable with severe hemorrhage or have failed attempts at nonoperative
management, the approach to surgery is generally of an emergent nature and requires direct
and rapid control of hemorrhage. The torso should be widely prepped and draped, and a
generous midline incision carried from the xiphisternum to just above the pubis. The use of
fi xed self-retaining retractors (e.g., Upper Hand, Omni-Tract, Thompson, or Buchwalter)
can aid in retraction of the costal margin and exposure.
CHAPTER
52
Splenectomy/Splenic Repair
William J. Mileski
CHAPTER 52 • Splenectomy/Splenic Repair 603
Splenic artery and vein
Spleen
Stomach
Pancreas
Colon
Splenocolic ligament
Lateral, posterior, and superior
retroperitoneal ligaments dissected
Spleen retracted medially
and caudally
FIGURE 52 –1
FIGURE 52 –2

604 Section VIII • Spleen
◆ In some patients, opening of the peritoneum may result in decompression of a degree of
tamponade and result in severe hypotension; temporary compression of the aorta at the dia-
phragmatic hiatus, either manually with an aortic compression device or with the end of a
small Richardson retractor, can provide temporization while the anesthesiologists restore in-
travascular volume. Upon evacuation of the hemoperitoneum, the right upper and left up-
per quadrants of the abdomen can be initially packed with laparotomy pads and the source
of hemorrhage determined.
STEP 3: OPERATIVE STEPS
1. INCISION AND MOBILIZATION OF THE SPLEEN
◆ Through a midline incision the spleen is retracted caudally and medially by the surgeon’s
left hand, and the assistant retracts the abdominal wall laterally (see Figure 52-2).
2. DISSECTION
◆ The lateral, posterior, and superior retroperitoneal attachments are rapidly released by sharp
dissection with a long Metzenbaum scissor (see Figure 52-2).
◆ A retropancreatic/prenephric plane can then be manually dissected, allowing the spleen to
be retracted anteriorly and medially into the midline incision (Figure 52-3).
◆ Active bleeding can be easily controlled with manual compression of the splenic hilum or
application of vascular clamps to the hilum. If clamps are used, it is important to exercise
care to avoid injury to the tail of the pancreas, which may be close by.
◆ Several laparotomy pads should be packed behind the spleen to tamponade bleeding and
support the spleen while the lesser sac is opened on the proximal aspect of the greater
curve of the stomach, and the short gastric vessels are ligated. While ligating the short gas-
tric vessels, care should be taken to avoid incorporating the gastric wall in the ligatures,
which can later lead to necrosis and a gastric fi stula. At this point the spleen can be freely
mobilized along with the tail of the pancreas to the midline (Figure 52-4).
