Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

CHAPTER 64 • Low Anterior Resection—Total Mesorectal Excision 737
Ureter
FIGURE 64–2
FIGURE 64–3
738 Section IX • Colon
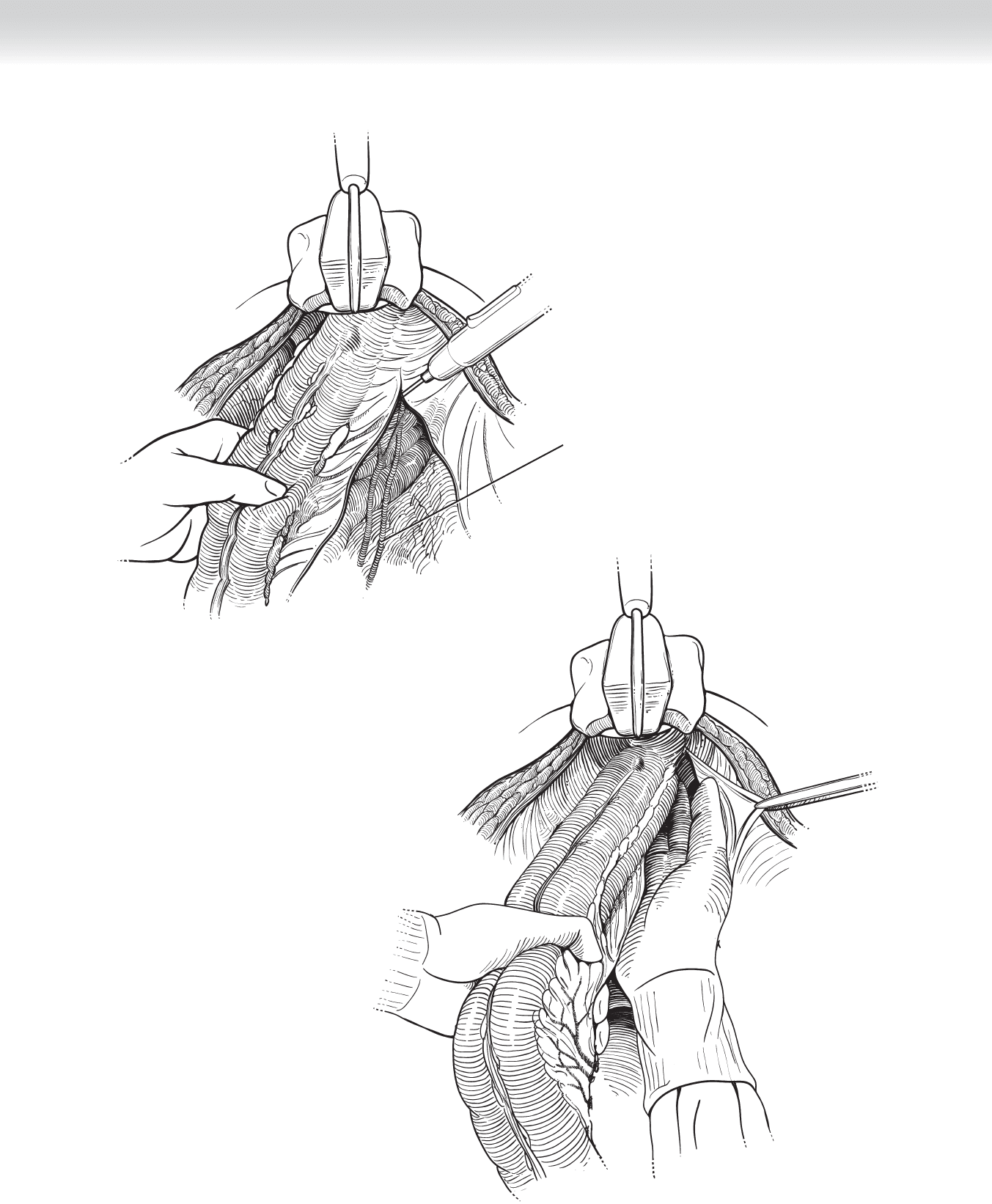
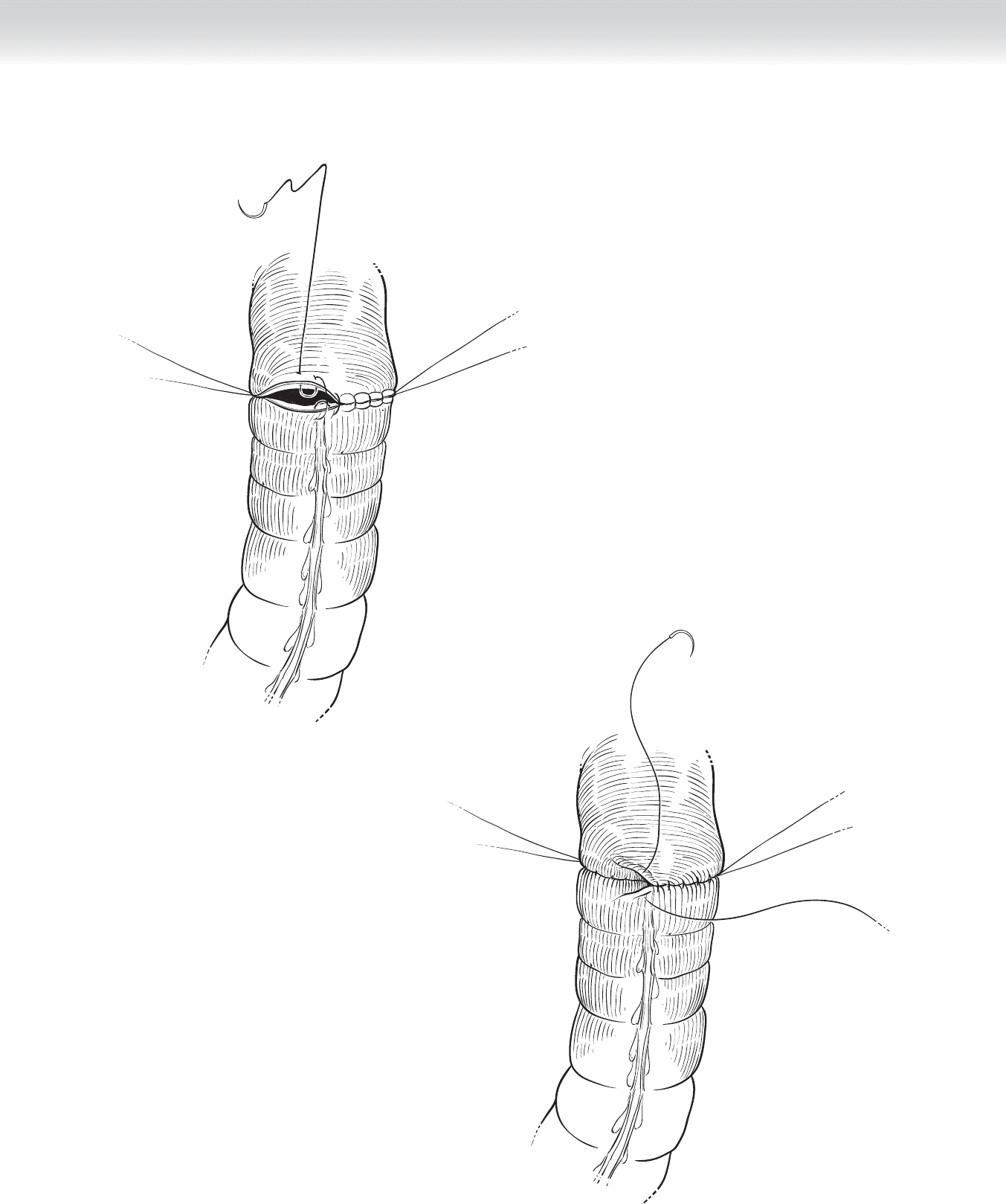
◆ The distal rectum is closed with a linear stapler approximately 2 to 5 cm distal to the tumor
(Figure 64-4). The rectum is clamped just proximal to the staple line and divided with a
scalpel. For low rectal tumors, a curved cutter stapler can help gain additional resection
margin by avoiding the need for applying a clamp.
◆ The sigmoid colon is divided just distal to the fi rst sigmoidal artery. The sigmoid colon is
clamped proximally with a purse-string applicator and distally with a linear clamp if a
stapled anastomosis is being performed (Figure 64-5) or with two linear clamps if a
hand-sewn anastomosis is being performed. Transection is completed with a scalpel
(Figure 64-6). The mesosigmoid is divided with clamps and sutures or with a vessel sealer
device.
TA-55 stapler
Tumor
FIGURE 64 –4
CHAPTER 64 • Low Anterior Resection—Total Mesorectal Excision 739
FIGURE 64–6
FIGURE 64–5
740 Section IX • Colon
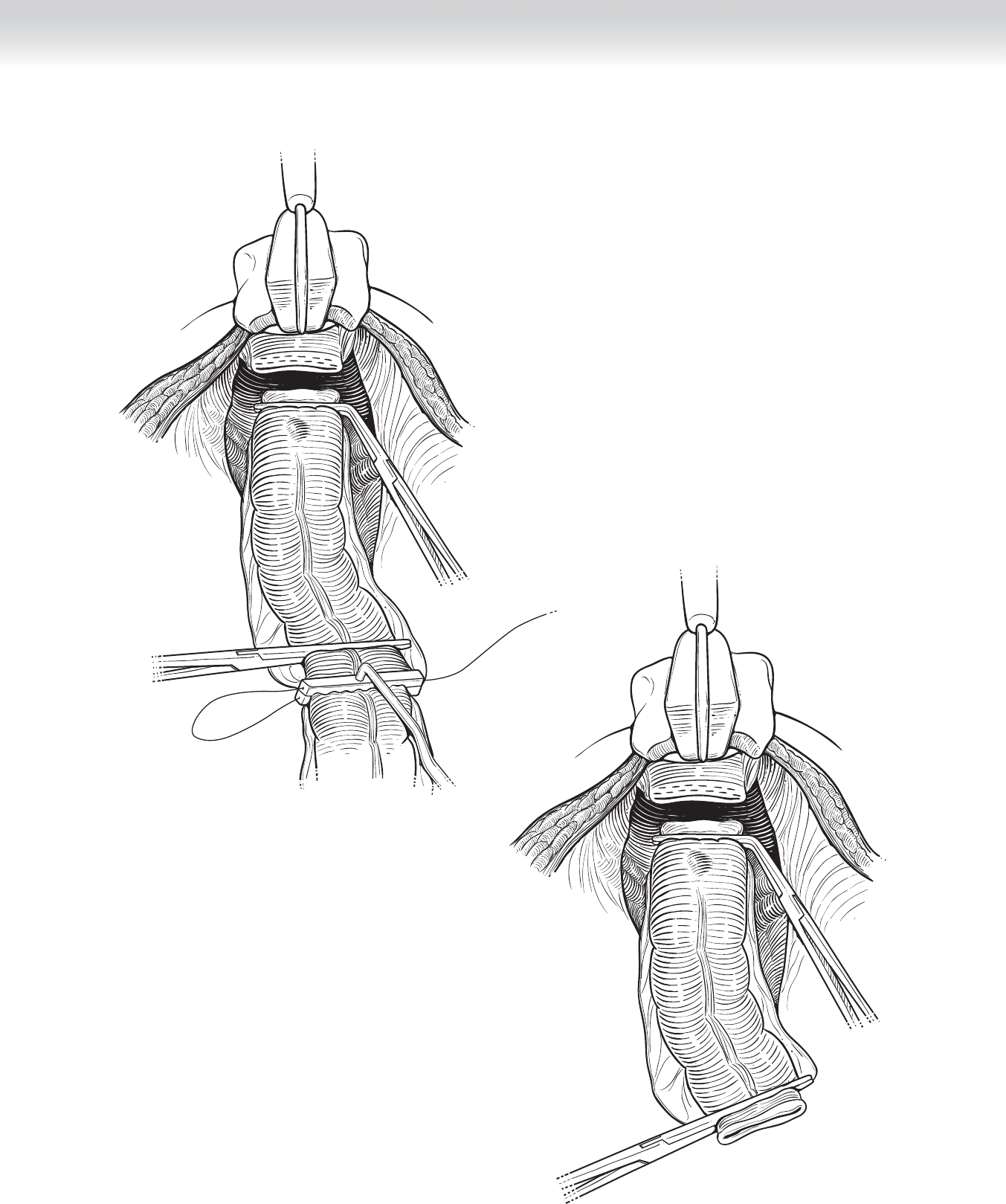
◆ A two-layer, hand-sewn colorectal anastomosis is performed by fi rst placing a posterior
layer of interrupted Lembert seromuscular sutures of 3-0 silk (Figure 64-7). Next, two
running full-thickness sutures of 3-0 Monocryl are placed by beginning at the mid-point
of the posterior layer (Figure 64-8). These sutures are continued anteriorly in a Connell
fashion (Figure 64-9) and fi nished by tying to each other to complete the inner layer.
Finally, an anterior layer of interrupted Lembert seromuscular sutures of 3-0 silk is placed
(Figure 64-10).
FIGURE 64–7
FIGURE 64–8
CHAPTER 64 • Low Anterior Resection—Total Mesorectal Excision 741
Lembert sutures
FIGURE 64–10
Connell sutures;
anterior anastomosis
FIGURE 64–9
742 Section IX • Colon
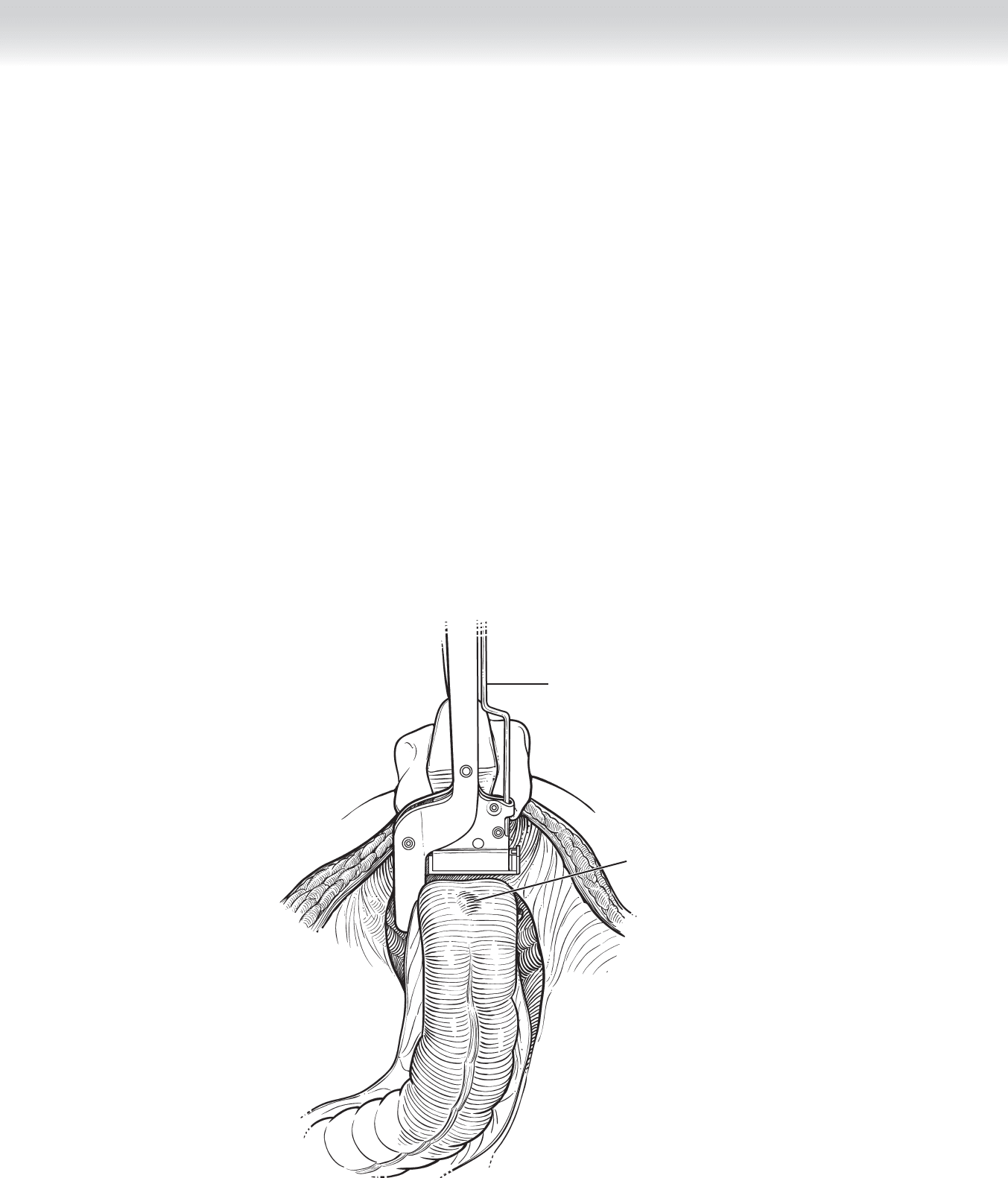
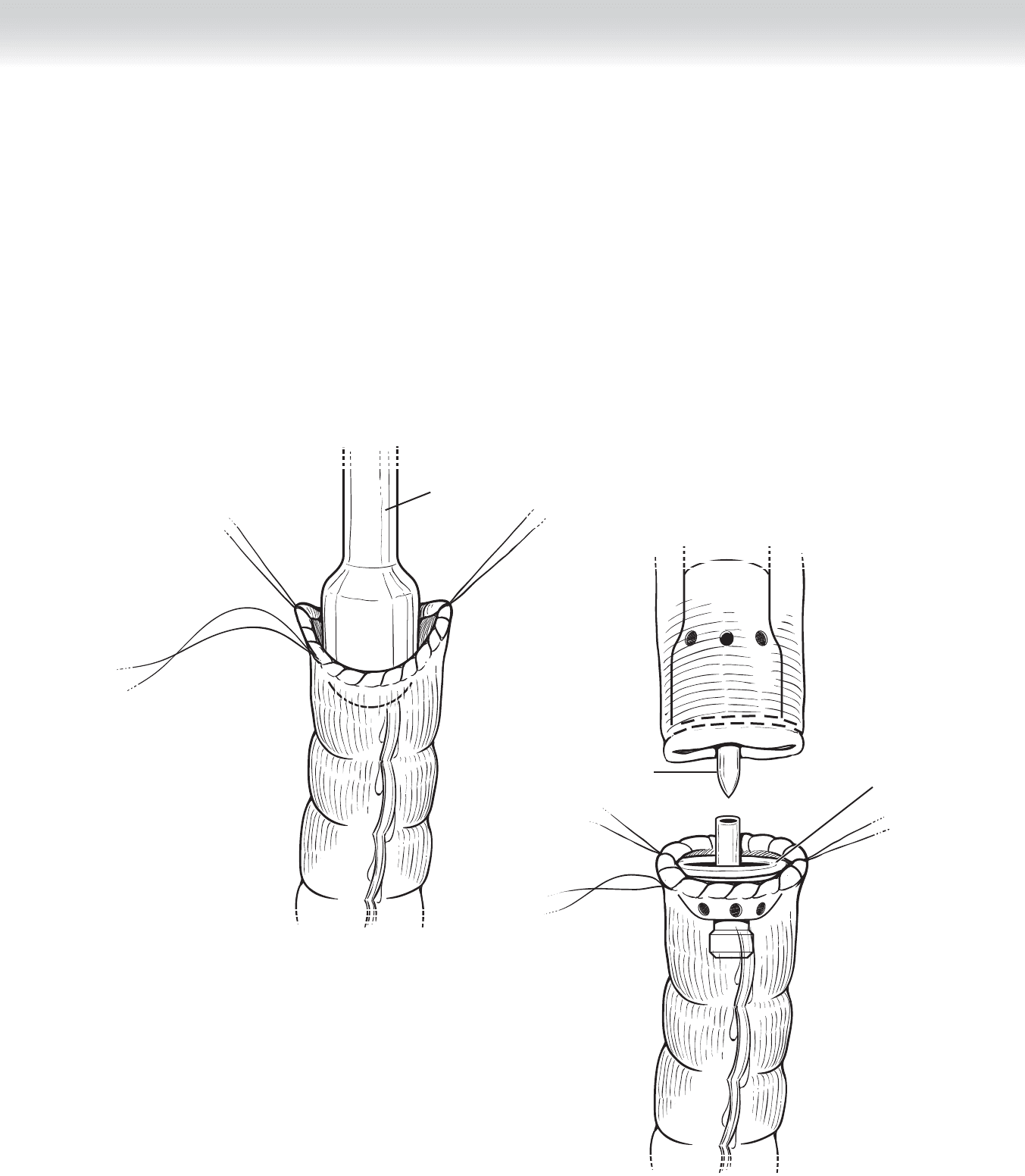
◆ Alternatively, a stapled colorectal anastomosis can be performed. After a purse-string appli-
cator is used, the proximal sigmoid colon is dilated with increasing size of dilators, which
also serves to determine the appropriate size of the stapler (Figure 64-11). Similarly, the
distal rectum is sized with the dilators.
◆ The anvil of the circular stapler is inserted into the proximal sigmoid colon, and the purse-
string is secured (Figure 64-12). The handle of the circular stapler is brought through the
distal rectal staple line transanally (see Figure 64-12).
Dilator
EEA stapler
Anvil
FIGURE 64–11
FIGURE 64–12
CHAPTER 64 • Low Anterior Resection—Total Mesorectal Excision 743
FIGURE 64–13
FIGURE 64–14
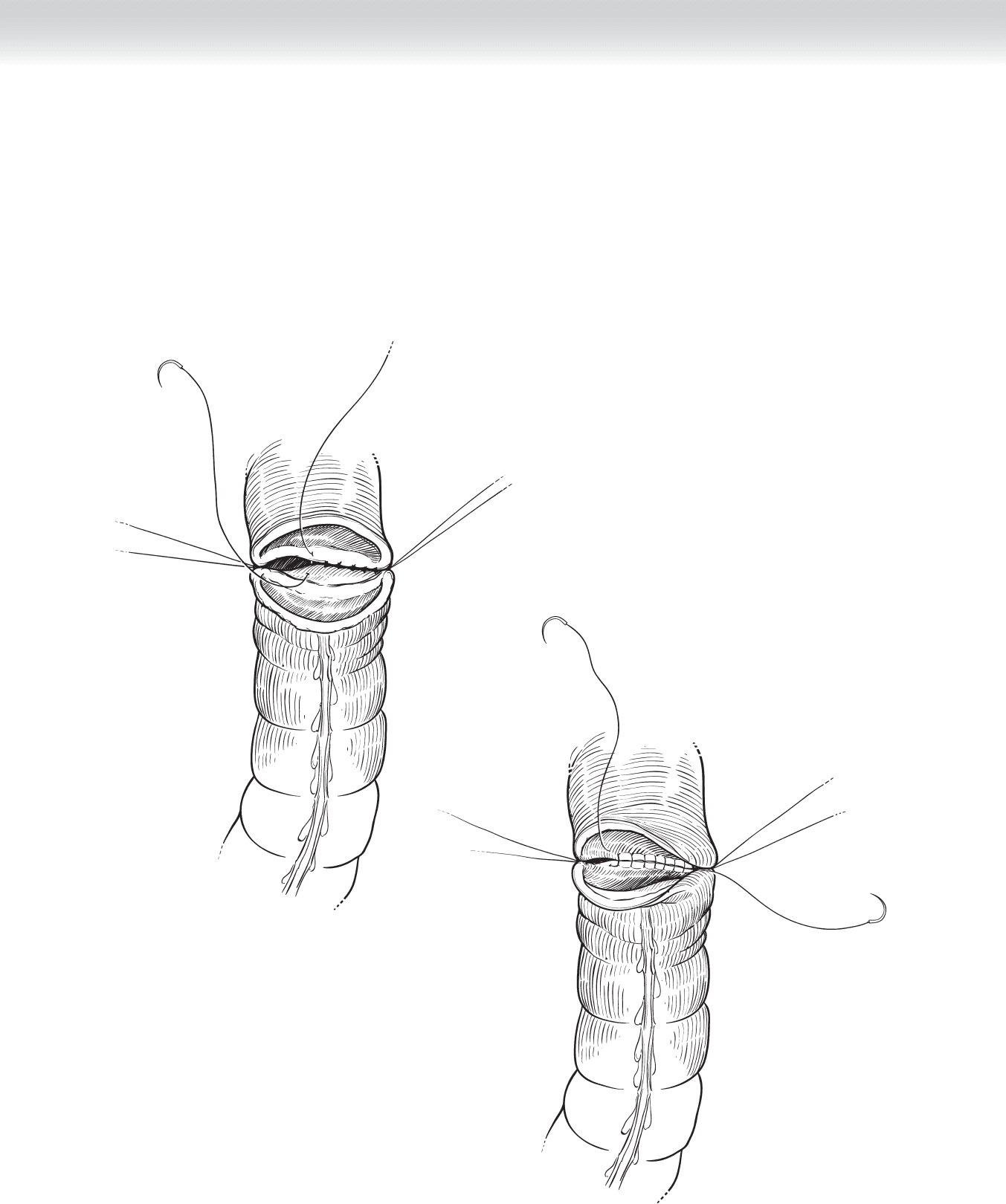
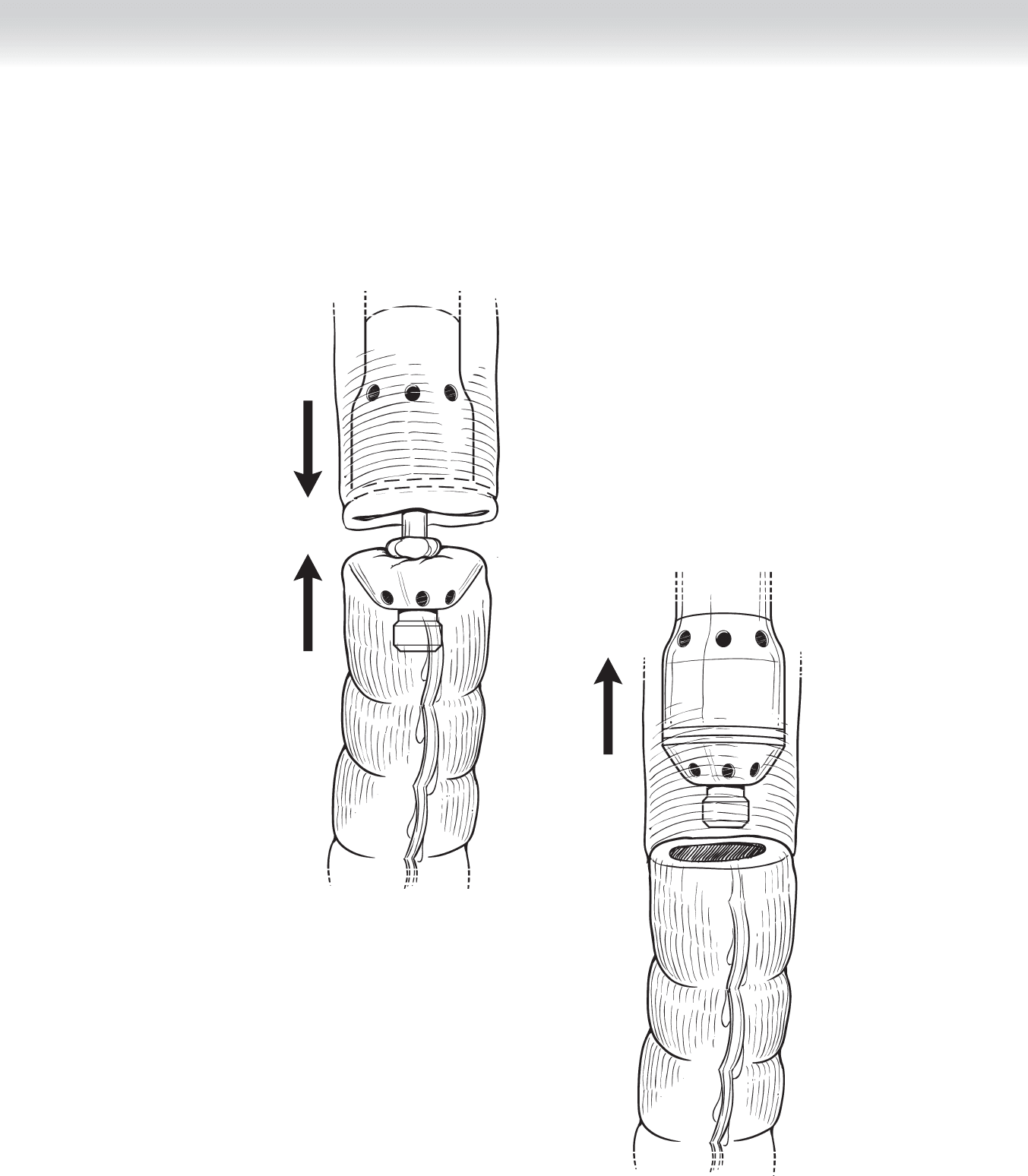
◆ The circular stapler is closed to appropriate tension and deployed (Figure 64-13). The circu-
lar stapler is opened partially and removed transanally (Figure 64-14). The stapler is then
examined to ensure that there are an intact ring of sigmoid colon in the anvil and an intact
ring of rectum in the stapler handle.
744 Section IX • Colon
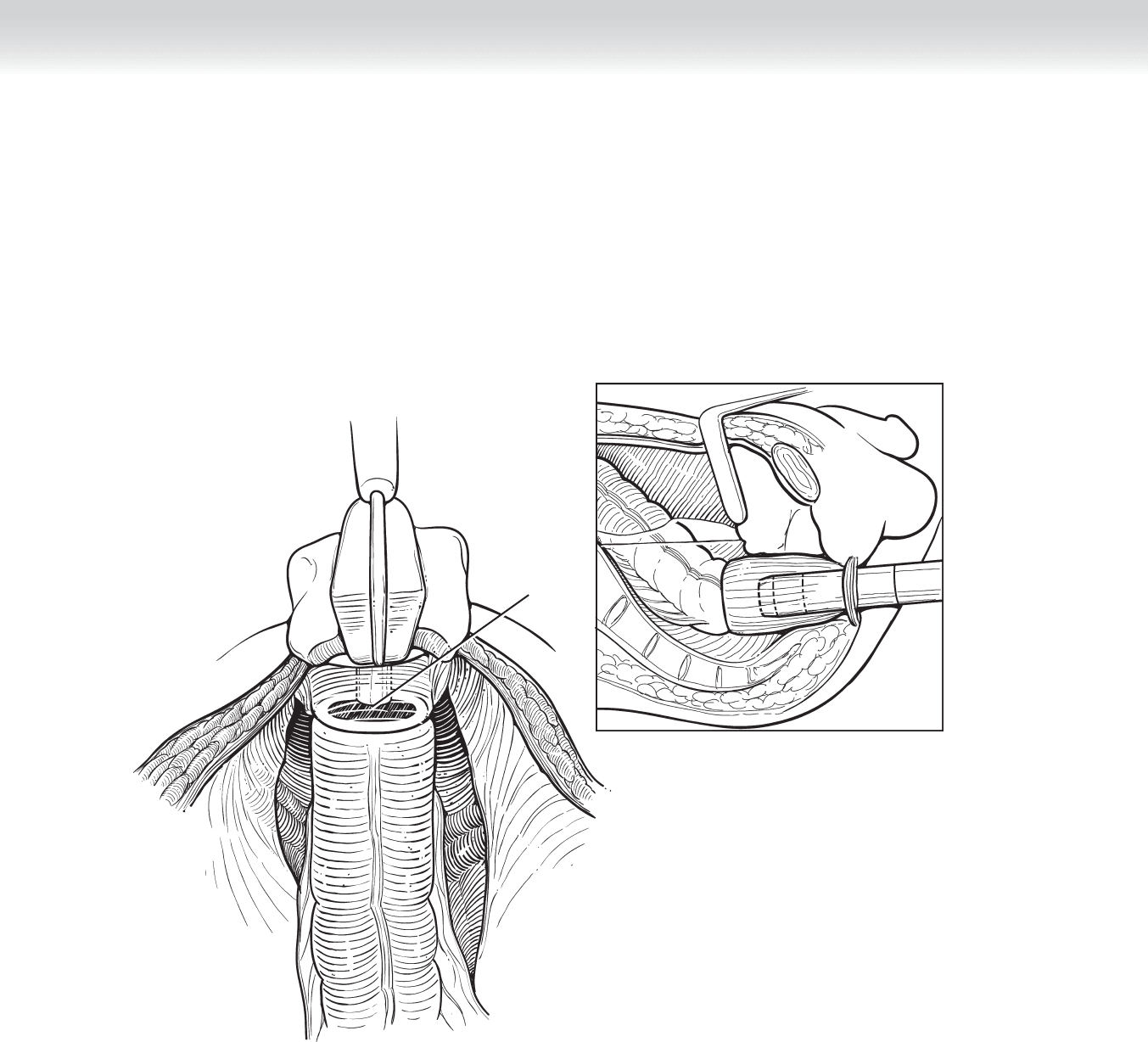
◆ The “bubble test” is performed to test the integrity of the colorectal anastomosis. The pelvis
is fi lled with saline, and a rigid proctoscope is inserted into the rectum distal to the anasto-
mosis. The lumen is gently distended by pumping air into the rectum, and absence of bub-
bles indicates an intact anastomotic line (Figure 64-15).
Scope
Testing the integrity of low rectal anastomosis with saline
in the pelvis and insufflation of air from a sigmoidoscope
FIGURE 64–15

3. CLOSING
◆ The peritoneal cavity is irrigated with saline, and hemostasis is obtained. The midline fascia
is closed in one layer with two running absorbable sutures of loop 0 polydioxanone (PDS)
beginning at the cranial and caudal end of the incision. The skin is reapproximated with
staples.
◆ No intraperitoneal drains are indicated.
◆ The nasogastric tube is removed before the patient emerges from anesthesia.
STEP 4: POSTOPERATIVE CARE
◆ Clear liquids are started on postoperative day 1, and diet is advanced as tolerated.
◆ Postoperative antibiotics are not necessary.
◆ The urinary catheter is left in place for 3 or 4 days to decrease the risk of urinary retention
after pelvic dissection.
STEP 5: PEARLS AND PITFALLS
◆ The mesorectal dissection should be performed sharply under direct vision and not bluntly
with the hand.
◆ The colorectal anastomosis must be tension free, and this may require division of the sig-
moid artery at its origin and mobilization of the splenic fl exure of the colon.
◆ In T3 and T4 rectal cancers, preservation of the pelvic autonomic nerves may not be possible.
◆ In most patients, the 29-mm circular stapler works well. Using the maximum-size circular
stapler may create radial tension, leading to anastomotic leak.
◆ If the anastomosis fails the “bubble test,” the anastomotic defect must be identifi ed and
repaired primarily. A protection loop ileostomy may be indicated for diffi cult or low anasto-
mosis (⬍5 cm) and for patients who underwent preoperative chemoradiation treatment.
CHAPTER 64 • Low Anterior Resection—Total Mesorectal Excision 745

746 Section IX • Colon
SELECTED REFERENCES
1. Havenga K, Grossmann I, DeRuiter M, Wiggers T: Defi nition of total mesorectal excision, including the
perineal phase: Technical considerations. Dig Dis 2007;25:44-50.
2. Fry RD, Mahmoud N, Maron D, et al: Colon and rectum. In Townsend CM Jr, Sabiston DC (eds):
Sabiston Textbook of Surgery, 18th ed. Philadelphia, Elsevier Saunders, 2008, pp 1348-1432.
