Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.


Chapter 84 TRAUMATIC OPHTHALMOLOGIC EMERGENCIES588
overlooked aspect of therapy is the instillation of a cycloplegic agent, usually cyclopentolate
(Cyclogyl), to relieve the ciliary spasm that commonly accompanies this injury. Patients also
need evaluation for tetanus prophylaxis. Most should receive topical antibiotics, drops, or
ointment. Nonsteroidal anti-inflammatory eye drops have also been proven to be useful.
9. What is the role of an eye patch in treatment of corneal abrasions?
A pressure patch previously was considered the most important aspect of management of a
corneal abrasion. Patches were thought to increase comfort and hasten healing. It is now
known that not only are eye patches uncomfortable but also they do not increase healing and
may promote infection. They do not prevent the involved eye from moving and should not be
used for most superficial corneal abrasions. If you do use a patch, be sure to instruct the
patient not to drive because depth perception depends on binocular vision.
10. How does a corneal abrasion from a contact lens differ from other causes of
corneal trauma?
Corneal abrasions secondary to overuse of contact lenses are much more likely to have a
bacterial process involved, often Pseudomonas. These patients should receive topical
antibiotics effective against Pseudomonas organisms (tobramycin or gentamicin) and should
never be patched. If the emergency physician is unable to do a slit-lamp examination, early
ophthalmologic referral to rule out ulcerative keratitis (corneal ulcer) is indicated.
11. What is the most common location of an ocular foreign body?
Foreign bodies are often lodged just beneath the upper eyelid along the palpebral conjunctiva.
The eyelid needs to be everted with a cotton swab to examine this area adequately. Conjunctival
foreign bodies should be suspected when many vertical linear streaks are noted on the cornea
with fluorescein examination.
12. What is the proper treatment for a corneal foreign body?
First, topical anesthesia is applied, usually proparacaine. Nonembedded foreign bodies should
be removed with a sterile, moist cotton swab. Embedded foreign bodies are removed with a
27-gauge needle or an eye spud. Most metallic foreign bodies leave a residual rust ring that
should be removed in approximately 24 hours, after the cornea has softened.
13. What is an anterior hyphema?
A collection of blood in the anterior chamber of the eye; it is seen as a layering of cells that
pool along the bottom of the eye when the patient is sitting upright. When the patient is lying
down, a hyphema is not recognized easily; it may appear as a diffuse haziness of the anterior
chamber. Small hyphemas, termed microhyphemas, may be identified only with a slit lamp.
14. How is an anterior hyphema treated?
The standard in the past was to admit all patients for bed rest; today the dominant tendency is
toward outpatient management. The patient should be kept upright, the eye patched, and
ophthalmologic consultation initiated, at least by phone. Complications include rebleeding,
glaucoma formation (particularly in patients with sickle-cell trait), and corneal staining.
15. What physical findings lead to the suspicion of a blow-out fracture?
Classic findings with a blow-out fracture (fracture of the inferior orbital wall with herniation of
the global contents into the maxillary sinus) are (1) decreased sensation over the inferior
orbital rim, extending to the edge of the nose and ipsilateral upper lip, secondary to
compromise of the inferior orbital nerve; (2) enophthalmos, or a sunken appearance of the
eye, which may be masked by edema; and (3) paralysis or limitation of upward gaze
(manifested as diplopia), resulting from entrapment of the inferior rectus muscle.
16. What is traumatic mydriasis?
An efferent pupillary defect manifested by a dilated (in most instances irregular) pupil that
does not react to direct or consensual light, usually as a result of minor trauma to the eye.
Chapter 84 TRAUMATIC OPHTHALMOLOGIC EMERGENCIES 589
Because such a patient is at risk for other more serious eye injuries, a careful eye examination
is mandatory. The possibility of uncal herniation secondary to intracranial injury should be
considered if level of consciousness is decreased in the presence of a perfectly round,
nonreactive, unilateral, dilated pupil. If level of consciousness is unaltered, this is most likely
an isolated ocular injury.
17. Why is a history of hammering metal on metal important in a patient
presenting with an eye complaint?
Often a small, high-velocity fragment penetrates the globe with minimal or no physical
findings. This injury, which can cause inflammation weeks later, is diagnosed with soft-tissue
radiographs of the orbit or a computed tomography (CT) scan of the globe.
18. Which eyelid lacerations should be repaired by an ophthalmologist or plastic
surgeon?
Those involving the:
n
Lid margin or gray line
n
Tear duct mechanism along the lower eyelid
n
Tarsal plate or levator muscle
19. When should penetration of the globe be suspected?
The pupil is usually misshapen, pointing in the direction of the penetration. The globe may
appear soft because of decreased intraocular pressure. Intraocular pressure should not be
tested if a penetrating injury is suspected because the pressure promotes extrusion of
aqueous humor.
20. List traumatic ophthalmologic injuries that require immediate ophthalmologic
consultation.
n
Chemical burns of the eye
n
Orbital hemorrhage with increased intraocular pressure
n
Perforation of the globe or cornea
n
Lacerations involving the lid margin, tarsal plate, or tear duct
n
Lens dislocation
21. Name two ophthalmologic injuries that require urgent ophthalmologic
consultation (within 12–24 hours).
Anterior hyphema and blow-out fracture.
22. What is solar keratitis?
Also known as flash burns or snow blindness, solar keratitis is a corneal injury secondary to
overexposure to ultraviolet light. Diagnosis is made with fluorescein staining, which shows
multiple punctate lesions of the cornea. Treatment consists of resting the eyes with adequate
narcotic analgesia. Spontaneous resolution can be expected in 12 to 24 hours.
23. What is the significance of a retro-orbital hematoma?
Bleeding behind the globe (retro-orbital hematoma) can lead to elevated orbital pressure,
which can be greater than the perfusion pressure of the retina and result in ischemia.
Treatment is a lateral canthotomy, which releases the canthus that holds the eye in its socket.
This allows for proptosis of the globe, which (temporarily) relieves the elevated retro-orbital
pressure, preserving blood flow to the retina.
24. What is the cause of a dilated pupil that fails to constrict with topical
pilocarpine?
A dilated pupil that fails to constrict with topical miotic agents is due to topical application of a
mydriatic agent often because of rubbing the eye after application of a scopolamine patch (for
motion sickness).
Chapter 84 TRAUMATIC OPHTHALMOLOGIC EMERGENCIES590
BIBLIOGRAPHY
1. McInnes G, Howes D: Lateral canthotomy and cantholysis: a simple, vision-saving procedure. Can J Emerg
Med 4:54, 2002.
2. Quinn SM, Kwartz J: Emergency management of contact lens associated corneal abrasions. Emerg Med J
21(6):755, 2004.
3. Turner A, Rabiu M: Patching for corneal abrasion. Cochrane Database Syst Rev (2) 264–270, 2006.
4. Weaver CS, Terrell KM: Evidence-based emergency medicine. Update: do ophthalmic nonsteroidal anti-
inflammatory drugs reduce the pain associated with simple corneal abrasion without delaying healing? Ann
Emerg Med 41(1):134–140, 2003.
1. Preservation of vision in a chemical burn is directly related from time of exposure to time
initiating irrigation; do not wait for the patient to arrive at the hospital.
2. Never patch a patient with an eye injury related to contact lens; a patch provides a perfect
environment for bacterial proliferation. These patients should be treated with aminoglycoside
ointment.
3. Diplopia on upward gaze is the hallmark of a blow-out fracture of the orbital floor.
KEY POINTS: OPHTHALMOLOGIC EMERGENCIES
591
CHAPTER 85
NECK TRAUMA
Jeffrey J. Schaider, MD
1. Why is neck trauma a complicated topic?
The lack of bony protection makes the anterior neck especially vulnerable to severe, life-
threatening injuries. The exposed anatomic structure of the neck, which contains many vital
structures of the vascular, airway, and gastrointestinal systems, provides a fertile ground for
debate and myriad opinions about modality of treatment.
2. What are the most urgent concerns in the initial management of neck trauma?
Airway and hemorrhage control. Airway management comes before anything else discussed
in this chapter. Early endotracheal intubation is indicated for any patient with existing or
potential airway compromise. Delay in airway management increases the difficulty of
intubation because of swelling and compression of the anatomic structures. Bleeding should
be controlled with pressure rather than with blind clamping. The wound should be examined
to determine whether it has violated the platysma. Injudicious probing of the wound may be
dangerous, however, because a vascular structure that has ceased to bleed may resume with
disastrous consequences when its tamponade is released.
3. What is the preferred method to secure the airway?
Rapid-sequence induction (RSI) with oral tracheal intubation should be the initial airway
approach in patients with none to minimal distortion of their airway. Patients with airway
distortion with anticipated difficult bag-valve-mask ventilation should have their airway
managed with local airway anesthesia or sedative-assisted oral tracheal intubation. The
preferred sedative medications include versed and fentanyl because they are reversible or
ketamine because it does not depress spontaneous respirations. Although the risks of blind
nasal tracheal intubation include breaking away clots and damaging a distorted airway, a
recent study from Denver found that blind nasal tracheal intubation had a 90% success rate in
the prehospital phase. Surgical airway via cricothyrotomy should be employed if endotracheal
intubation is unsuccessful. Tracheostomy is preferred over cricothyrotomy if there is severe
damage to the larynx and cricoid cartilage.
4. What common findings indicate significant neck injury?
n
Injuries involving the vascular system result in hematomas, bleeding, pulse deficit, shock,
and neurologic deficit secondary to arterial interruption.
n
Laryngeal trauma causes voice alteration, airway compromise, subcutaneous emphysema,
crepitus, and hemoptysis.
n
Signs and symptoms of esophageal disruption include pain and tenderness in the neck,
resistance of the neck to passive motion, crepitus, subcutaneous emphysema, dysphagia,
and bleeding from the mouth or nasogastric tube. The diagnosis of esophageal disruption
is difficult because of injuries to other overlying structures. Ancillary testing must be used
to assist in the diagnosis of these injuries.
For more details, see Table 85-1.
5. What are the signs and symptoms of blunt carotid artery trauma?
Of patients with blunt carotid trauma, 25% to 50% have no external signs of trauma. Delayed
neurologic signs are the rule rather than the exception; only 10% of patients have symptoms
Chapter 85 NECK TRAUMA592
of transient ischemic attacks or strokes within 1 hour of injury. Most patients develop
symptoms within the first 24 hours, but 17% develop symptoms days or weeks after injury.
Carotid artery injuries may present with a hematoma of the lateral neck, bruit over carotid
circulation, Horner’s syndrome, transient ischemic attack, aphasia, or hemiparesis. The clinical
manifestations of vertebral artery injury include ataxia, vertigo, nystagmus, hemiparesis,
dysarthria, and diplopia.
6. Name the main controversy regarding management of penetrating neck
trauma.
The management of penetrating neck trauma that violates the platysma. In the 1990s,
physicians and surgeons changed from a mandatory exploration policy for penetrating neck
wounds to a selective management approach.
7. What is mandatory exploration for penetrating neck wounds?
All patients who have wounds that penetrate the platysma muscle in the neck are explored
surgically to determine the presence or absence of injury to the deeper structures in the neck.
Some ancillary diagnostic testing (i.e., angiography, esophagography, esophagoscopy, and
laryngoscopy) may be done preoperatively, depending on the location of the wound and the
stability of the patient.
8. What are the advantages and disadvantages of mandatory exploration for
penetrating neck wounds?
During the 1940s, mandatory exploration was instituted for all penetrating wounds that violate
the platysma. This policy reduced mortality significantly and remained the only mode of
therapy until the mid-1970s. Proponents of mandatory exploration warn of the catastrophic
complications from delayed treatment and missed injuries. Neck exploration is relatively
simple, and a negative exploration has low morbidity and mortality. However, because the
negative exploration rate (no injuries found at surgery) is 50%, the cost of the operation and
the added length of hospital stay are unwarranted. Many of these operations could be avoided
with the selective approach to neck exploration.
Vascular Aerodigestive
Hematoma Respiratory distress
Hemorrhage Stridor
Neurologic deficit Cyanosis
Pulse deficit Hemoptysis
Horner’s syndrome (carotid injury) Tracheal deviation
Hypovolemic shock Subcutaneous emphysema
Vascular bruit or thrill Pneumothorax
Altered sensorium Sucking wound
Harsh, machinery-like precordial
murmur (air embolism)
Dysphonia, aphonia, hoarseness
Dysphagia
Odynophagia
TABLE 85–1. SIGNS AND SYMPTOMS OF SYSTEM INJURIES
Chapter 85 NECK TRAUMA 593
9. Describe the theory behind the selective surgical management of penetrating
neck wounds.
With the improved sensitivity and specificity of ancillary diagnostic testing (angiography,
carotid duplex scanning, computed tomography [CT], esophagography, esophagoscopy,
laryngoscopy), a nonoperative approach to a select group of patients, based on physical
examination and results of ancillary tests, is safe. The selective approach has reduced the
negative exploration rate from 50% to 30%.
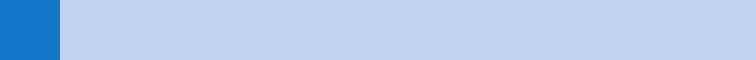
10. What are the three anatomic zones of the neck?
n
Zone I is the area below the cricoid cartilage.
n
Zone II extends from the cricoid cartilage to the angle of the mandible.
n
Zone III extends from the angle of the mandible to the base of the skull.
Figure 85-1 illustrates the zones of the neck.
11. Why is the neck divided into three zones?
The location of the injury plays a major role in assessing the need for angiography:
n
All zone I injuries require angiography to determine the integrity of the thoracic outlet
vessels. In stable but symptomatic patients needing surgery, angiography should be
done preoperatively because positive findings necessitate a thoracotomy before neck
exploration.
n
The familiar anatomy of zone II, coupled with relative ease of surgical exposure, minimizes
the need for angiography in symptomatic patients undergoing surgery. For patients without
clinical signs of significant injury, most recommend helical CT angiography of the neck or
carotid duplex scanning on asymptomatic patients to detect occult injuries and involvement
1. Manage airway early before airway distortion occurs.
2. Use oral tracheal intubation with RSI as initial airway management option.
3. Do not paralyze patients with significant airway distortion who cannot be ventilated.
4. Tracheostomy may be necessary as rescue airway if there is a hematoma over or damage to
cricoid cartilage.
KEY POINTS: EARLY AIRWAY MANAGEMENT FOR NECK
INJURIES
Figure 85-1. Zones of the neck.
Chapter 85 NECK TRAUMA594
of vertebral vessels before observation. Some clinicians observe asymptomatic patients
with penetrating injuries without any imaging.
n
The management of zone III injuries is controversial because of the complex anatomy of
the area and the difficulty in obtaining adequate exposure. Most clinicians agree that for
asymptomatic patients not undergoing surgery, angiography is necessary to assess the
status of the internal carotid artery and the intracerebral circulation. For symptomatic
patients, preoperative angiography is helpful because high internal carotid artery injuries
are difficult to visualize at operation and may require carotid artery ligation and concomitant
extracranial-intracranial bypass.
12. Can carotid duplex scanning or computed tomographic angiography (CTA)
replace angiography for detection of vascular injuries in penetrating neck
injuries?
With experienced operators, carotid duplex scanning approaches 100% sensitivity for
excluding zone II and III vascular injuries in stable, asymptomatic patients with penetrating
neck injuries. Because carotid duplex scanning has a lower specificity (85%–95%), positive
carotid duplex scanning should be followed by carotid angiography before making a decision
regarding surgical intervention.
In recent studies using multidetector helical CT scanners, CTA had sensitivities of 90% to
100%, a specificity of 100%, a positive predictive value of 100%, and a negative predictive
value of 98% in detecting carotid artery injuries. The limitations and pitfalls of the helical CTA
include artifacts produced by the shoulders of large patients or by bullet fragments and other
metallic foreign bodies. Streak artifacts can simulate an intimal tear. In cases with inadequate
studies or doubtful CTA results, the study should be considered nondiagnostic, and the
patients must undergo conventional angiography. CTA examinations have only a 1.1%
reported incidence of nondiagnostic results.
13. What diagnostic testing is preferred in detection of blunt vascular injuries?
n
Blunt vascular injuries were found in 27% of high-risk patients screened for blunt
vascular injury (combination of injury mechanism [cervical hyperextension or
hyperflexion, direct cervical blow, near-hanging] and injury pattern [carotid canal,
midface, and cervical spine fracture]). Angiography is the study of choice in acutely
injured and symptomatic patients. Of lesions, 90% occur at the bifurcation of carotids
or higher. Four-vessel angiography is recommended because multiple vessel injuries
occur in 40% to 80%. With the improved sensitivity of CT, angiography is shifting to a
therapeutic role.
n
The diagnostic accuracy of CTA has improved with the use of better CT technology. Using a
16 slice CT, Eastman found that CTA had a 97% sensitivity and 100% specificity. CTA has
been shown to decrease significantly the time to diagnose the injury.
n
Color flow Doppler ultrasound provides rapid identification and quantification of arterial
dissection, but it is unable to assess distal upper extracranial and intracranial internal
carotid artery and is operator dependent. With an experienced operator, ultrasound can be
used as a screening test in lower-risk patients.
n
Magnetic resonance angiography (MRA) accurately detects carotid and vertebral artery
injuries with a sensitivity and specificity greater than 95% for carotid artery dissection. It is
ideal for follow-up or for stable patients; MRA is difficult to perform in an acutely injured
unstable patient.
14. What is the appropriate management of blunt vascular injuries?
Carotid and vertebral artery dissections causing neurologic deficits should be treated with
endovascular stent-placement. Asymptomatic dissections are at risk for extension of the
dissection and thromboembolic events but often heal with observation and anticoagulation
therapy alone.
Chapter 85 NECK TRAUMA 595
15. Which diagnostic studies are important in suspected laryngeal injuries?
n
Soft-tissue cervical radiographs may show a fractured larynx, subcutaneous air, or
prevertebral air.
n
CT accurately identifies the location and extent of laryngeal fractures. CT should be done
when the diagnosis of a laryngeal fracture is still suspected despite a negative examination
of the endolarynx or when flexible laryngoscopy cannot be done (e.g., intubated patient).
n
Flexible laryngoscopy provides valuable information regarding the integrity of the
cartilaginous framework and the function of the vocal cords.
16. Are diagnostic studies necessary in suspected esophageal injuries?
Yes. Soft-tissue cervical radiographs may show subcutaneous emphysema or an increased
prevertebral shadow. Chest radiograph findings include pleural effusion, pneumothorax,
mediastinal air, and mediastinal widening. Esophageal contrast studies should be done initially
with radiopaque contrast medium (Gastrografin); if negative, studies should be repeated with
barium to increase diagnostic yield. Radiographic imaging is difficult because of the high
false-negative rate. Esophagography has a 30% to 50% false-negative rate and should be
followed by esophagoscopy in patients with suspected esophageal injury. Rigid endoscopy is
more sensitive than flexible endoscopy. No one study can exclude esophageal perforation; a
combination of physical signs, plain and contrast radiographs, and esophagoscopy should be
used to make the diagnosis. Isolated esophageal injuries after blunt injury are extremely rare.
BIBLIOGRAPHY
1. Biffl WL, Moore EE: Identifying the asymptomatic patient with blunt carotid arterial injury. J Trauma
47:1163–1164, 1999.
2. Demetriades D, Theodorou D, Cornwell E, et al: Evaluation of penetrating injuries of the neck: prospective
study of 223 patients. World J Surg 21:47–48, 1997.
3. Deshaies EM, Nair AK, Boulos AS, et al: Blunt traumatic injuries to the carotid and vertebral arteries of the
neck and skull base. Contemp Neurosurg 30:1–6;2008.
4. Eastman AL, Chason DP, Perez CL, et al: Computed tomographic angiography for the diagnosis of blunt
cervical vascular injury: is it ready for prime time? J Trauma 60:925–9, 2006.
5. Fry WR, Dort JA, Smith RS, et al: Duplex scanning replaces arteriography and operative exploration in the
diagnosis of potential cervical vascular injury. Am J Surg 168:693–695, 1994.
6. Knaut AL, Kendall JL: Penetrating neck trauma. In Wolfson AB, Hendey GW, Hendry PL, et al, editors: Clinical
practice of emergency medicine, ed 4, Philadelphia, 2005, Lippincott, Williams & Wilkins, pp 956–962.
7. LeBlang SD, Nunez DB: Noninvasive imaging of cervical vascular injuries. Am J Roentgenol 175:1269–1278, 2002.
8. Múnera F, Cohn S, Rivas LA: Penetrating Injuries of the neck: use of helical computed tomographic
angiography. J Trauma 58:413–418, 2005.
9. Múnera F, Soto JA, Palacio D, et al: Diagnosis of arterial injuries caused by penetrating trauma to the neck:
comparison of helical CT angiography and conventional angiography. Radiology 216:356–362, 2000.
10. Schaider JJ, Bailitz J: Neck trauma: don’t put your neck on the line. Emerg Med Pract 5:1–23, 2003.
11. Tishman SA, Bokhari F, Collier B, et al: Clinical practice guideline: penetrating zone II neck trauma. J Trauma
64:1392–1405; 2008.
12. Weitzel N, Kendall JL, Pons P: Blind nasotracheal intubation for patients with penetrating neck trauma. J Trauma
56.1097–1101, 2004.
596
CHAPTER 86
CHEST TRAUMA
Susan Brion, MD, MS, and Justin C. Chang, MD
1. What is the initial approach to the patient with chest trauma?
Specific life-threatening conditions should be suspected based on mechanism of injury. Key
injuries that should be diagnosed and treated during the initial standard survey include airway
obstruction, tension pneumothorax, cardiac tamponade, massive hemothorax, open
pneumothorax, and flail chest.
n
Inspection. Completely undress the patient and visually inspect the entire chest,
which necessitates rolling over a supine patient. Look for a flail chest (paradoxical
movement of the chest wall) and sucking chest wounds. Identify the exact location,
number, and type (i.e., penetrating or blunt) of wounds. Look for distended neck veins,
swollen face or neck (indicating damage to the mediastinum or underlying subcutaneous
emphysema).
n
Auscultation. Initial auscultation should focus on the axillae where breath sounds are
most readily heard. If breath sounds are equal bilaterally, the major bronchi are
probably intact. Listen for diminished or absent breath sounds and bowel sounds in the
chest. The presence of bowel sounds high in the chest may be the first indication of
diaphragmatic injury. Decreased breath sounds usually indicate pneumothorax or
hemothorax, although in an intubated patient this may also occur with the endotracheal
tube being in too deep. Bony crepitus indicates a rib or sternal fracture with the
potential for intrathoracic injury.
n
Palpation. It is important to palpate the chest wall gently at first to detect bony crepitus
and subcutaneous emphysema. Crepitus indicates a major blow to the chest with rib
fractures and the potential for underlying organ damage (e.g., pulmonary contusion), and
subcutaneous emphysema, depending on location, indicates pneumothorax or
pneumomediastinum.
2. What is the differential diagnosis for blunt versus penetrating chest
trauma?
n
Blunt injury: Simple pneumothorax, tension pneumothorax, hemothorax, rib fractures, flail
chest, sternal fracture, pulmonary contusion, pneumomediastinum, cardiac contusion/blunt
myocardial injury, and aortic injury.
n
Penetrating injury: Open pneumothorax, cardiac and great vessel injury
3. What is the best way to diagnose simple pneumothorax?
Recent literature supports the use of bedside transthoracic ultrasound in the hands of
experienced emergency medicine physicians as a superior modality for the diagnosis of
pneumothorax in comparison to plain chest X-ray, particularly in the supine patient. If plain
chest X-ray is used, a posterior-anterior (PA) film in full expiration should be used to detect a
small pneumothorax. Computed tomography (CT) of the thorax remains the gold standard for
diagnosis.
4. When is a pneumothorax likely to cause severe symptoms?
Severe symptoms may be seen if the pneumothorax is greater than 40% of the hemithorax
(approximately 2.5 cm from the chest wall in an adult), in patients with shock or pre-existing
cardiopulmonary disease, or if it is a tension pneumothorax.
Chapter 86 CHEST TRAUMA 597
5. How is tension pneumothorax diagnosed?
Tension pneumothorax is a clinical rather than radiographic diagnosis. Clinical signs include
dyspnea, distended neck veins, diminished or absent breath sounds on the affected side,
tracheal deviation to the opposite side, hyperresonance to percussion, and hyperexpansion of
the chest wall on the affected side. If hypotension is present, jugular venous distention may
not be noted. Tachycardia, absent breath sounds, and hypotension are the most reliable and
easiest to appreciate signs of tension pneumothorax. If a chest X-ray is obtained, a
hyperlucent, overexpanded hemithorax with an evident pneumothorax and a mediastinal shift
to the opposite side would be observed.
6. What is the treatment for tension pneumothorax?
If tension pneumothorax is suspected, immediate reduction of the intrapleural pressure by
placement of a 14-gauge intravenous catheter over the fourth or fifth rib in the midaxillary
line, followed by aspiration with a 50-mL syringe, will convert the tension pneumothorax into
an open pneumothorax. This should be followed immediately by a tube thoracostomy after
vital signs improve. Lack of improvement following decompression indicates another cause of
hypoperfusion should be sought immediately.
1. Tension pneumothorax should be a clinical diagnosis.
2. Tachycardia, absent breath sounds, and hypotension are the most reliable means of diagnosis.
3. Immediately decompress the chest with a 14-gauge intravenous catheter whenever tension
pneumothorax is suspected.
4. Look for other sources of hypotension if there is no immediate improvement after
decompression.
KEY POINTS: TENSION PNEUMOTHORAX
7. What is the definition of massive hemothorax?
Massive hemothorax in an adult is defined as 1500 mL or more, about two thirds of the
available space in the hemithorax, occupied by blood. Patients with hemothorax will
occasionally continue to bleed. If there is evidence of ongoing hemorrhage after initial
drainage exceeding 600 mL over 6 hours, a massive hemothorax equivalent is diagnosed.
8. What is flail chest?
A flail chest occurs when a segment of the chest wall becomes unattached from the rest of the
chest. It occurs in one of three settings:
n
Two or more ribs are broken in two or more places.
n
More than one rib is fractured in association with costal cartilage disarticulation.
n
The costal cartilages on both sides of the sternum are disarticulated, resulting in a sternal
or central flail segment.
The significance of a flail chest lies in the tremendous force that caused it and the near
certainty of associated intrathoracic injuries.
9. What is the treatment for flail chest?
The primary treatment should be supportive, including analgesia, coughing, chest
physiotherapy, prevention of fluid overload, and subsequent pulmonary edema. If the patient
is in respiratory distress either clinically or as indicated by blood gas analysis or oxygen
saturation measurements, intubation and positive-pressure ventilation should be initiated.
Indications for early ventilatory support include shock, three or more associated injuries,
severe head injury, comorbid pulmonary disease, fracture of eight or more ribs, and age older
than 65 years.
