Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

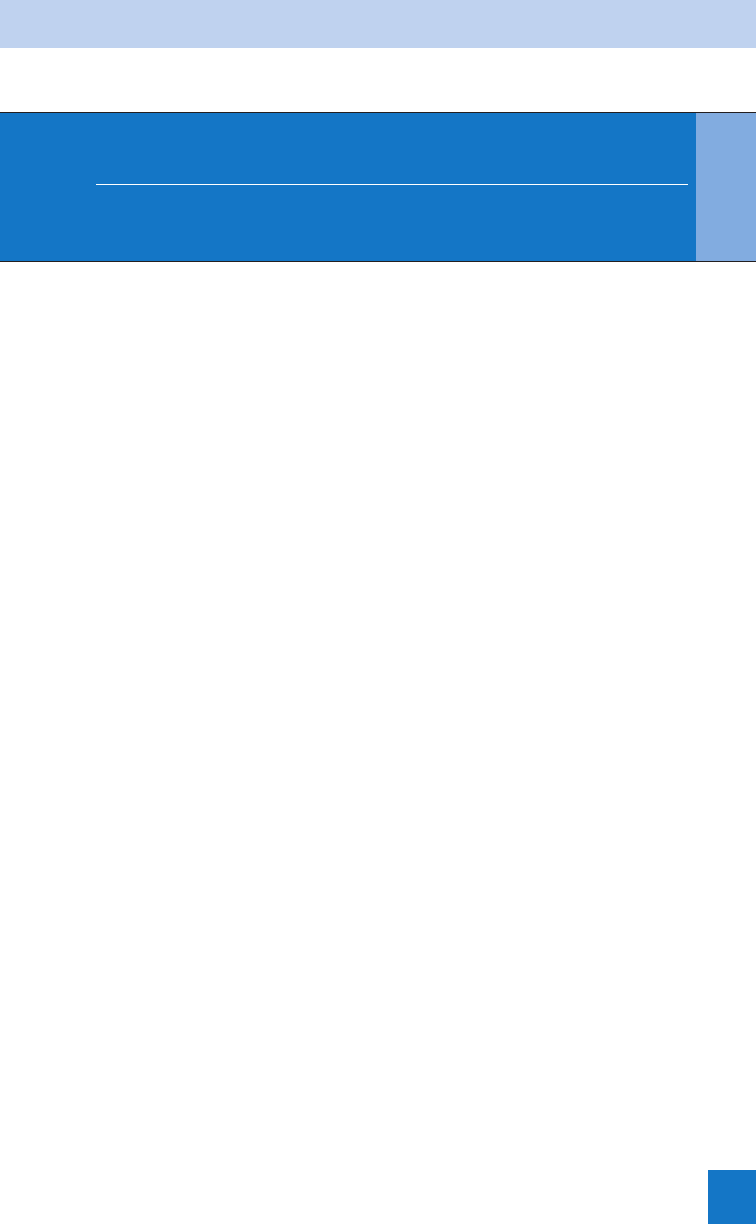
Chapter 88 PELVIC FRACTURES AND GENITOURINARY TRAUMA608
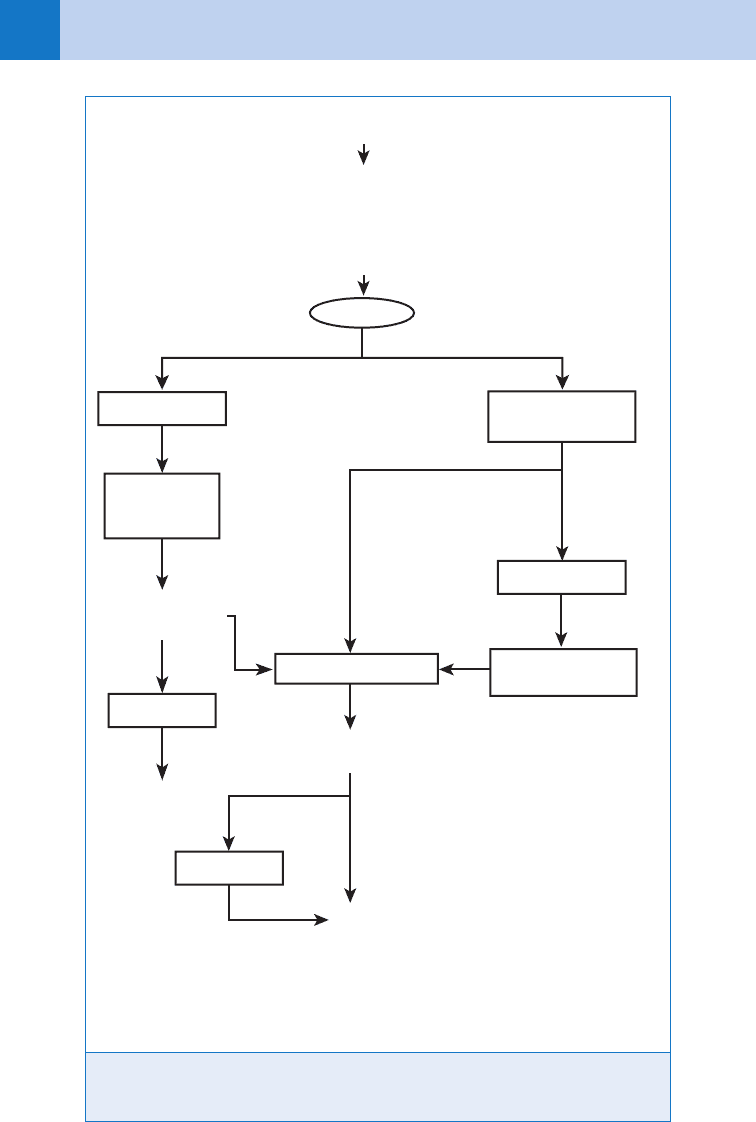
Figure 88-1. Management of patients with a pelvic fracture. CVP, central venous pressure; DPL,
diagnostic peritoneal lavage; FFP, fresh frozen plasma; PLTs, platelets; PRBCs, packed red blood
cells; TICU, trauma intensive care unit.
HD unstableHD stable
Yes
Yes
No
No
Angiography
Angiography
SICU
SICU
SICU +/- CT scans**
Ongoing transfusion
requirements?
Positive
FAST exam
2 units PRBCs/ED
trauma bay
Operating room
Operating room
Hemodynamically
stable?
Negative
Pelvic fixation
and pelvic packing
** Normalize coagulation status, consider Factor VIIA if recalcitrant.
Abdominal CT scan if no laparotomy done.
Laparotomy,
pelvic fixation,
pelvic packing
Resuscitate with 2 L crystalloid-place CVP line-measure base deficit-
R/O thoracic source (portable chest x-ray)
If beginning to transfuse PRBCs, start thinking about pelvic packing
Transfuse PRBC and FFP 1:1; 1 apheresis unit PLT for each 5 U PRBC
Immediate notification: attending trauma surgeon,
attending orthopaedic surgeon, blood bank resident, IR fellow
Pelvic Fracture Clinical Pathway:
Patients with hemodynamic instability and ANY pelvic fracture
Chapter 88 PELVIC FRACTURES AND GENITOURINARY TRAUMA 609
Vertical shear injuries consist of displaced fractures of the anterior rami and posterior
columns, including SI dislocation.
5. What are the sources of bleeding from major pelvic fractures?
The most frequent source is of venous origin, but arterial bleeding can lead quickly to
hemodynamic compromise. Massive bleeding is often associated with vertical shear or APC
fractures. The internal iliac arterial system (in particular, the superior gluteal artery bridging
the SI joint) may be affected by SI disruption. Significant blood loss can occur from vesicular
branches of the pudendal artery in association with pubic diastasis and anterior fractures.
Injury to the veins in the superior gluteal and pudendal distributions and the lumbosacral
venous plexus also contributes significantly to retroperitoneal and pelvic hemorrhage. LC
fractures are not usually associated with major blood loss because they result in compression
of local vasculature.
1. Multispecialty involvement is critical.
2. Bleeding is the leading cause of death.
3. Associated injuries are common.
4. Prompt, definitive decision making is the key to survival.
KEY POINTS: APPROACH TO PATIENTS WITH
A PELVIC FRACTURE
6. Name three goals of mechanical pelvic stabilization.
n
Reduce pelvic volume.
n
Promote tamponade of bleeding bone and vessels.
n
Prevent further fracture motion.
7. Discuss four methods of pelvic stabilization.
n
Wrapping the pelvis with a sheet and binding the knees and ankles with tape. This
intervention should be performed immediately on discovery of an unstable pelvic fracture,
particularly before patient transport. Prolonged use may result in extremity or abdominal
compartment syndrome.
n
Anterior external fixation. This is becoming the standard intervention for acute pelvic
stabilization. It is most effective with the anteroposterior open-book fracture. More complex
fractures such as vertical shear injury may also benefit from early stabilization, but fixation
is not as complete because of the instability of the posterior column.
n
Pelvic C-clamp. This intervention is more effective than a standard anterior frame in
stabilizing the posterior pelvis.
n
Pneumatic antishock garment (PASG). Use is controversial, particularly in prehospital care
in urban areas with short transport times. Given the efficacy of pelvic wrapping, there is
little role for the PASG today.
8. When should patients with pelvic trauma undergo laparotomy?
The incidence of active intraperitoneal visceral bleeding is 20% to 30% in association with pelvic
fracture. Ultrasound should be utilized during initial evaluation of unstable patients to exclude
hemoperitoneum. If ultrasound is not available, diagnostic peritoneal aspirate (DPA) should be
done at the supraumbilical ring to avoid dissecting pelvic hematoma. Ultrasound showing overt
intraperitoneal fluid, or a grossly positive DPA, should prompt immediate laparotomy. In the
patient with a normal ultrasound or DPL positive by red blood cell count only, the pelvic bleeding
should be managed first. In this case, the key decision is whether to employ skeletal fixation

Chapter 88 PELVIC FRACTURES AND GENITOURINARY TRAUMA610
alone, pelvic packing, or selective arterial embolization; prompt consultation of orthopedic and
interventional radiology specialists is imperative. (See Fig. 88-1.)
9. How frequently are rectal injuries associated with pelvic injuries? How are
they managed?
Approximately 5% of major pelvic fractures are associated with rectal injuries. These complex
injuries result in a high mortality rate secondary to septic complications. Current management
principles consist of fecal diversion, presacral drainage, and perineal debridement as needed.
Although some studies have shown that presacral drainage may be unnecessary, these were
based on small patient samples.
10. What is the role of pelvic packing for pelvic trauma?
Packing was employed commonly in Europe before being adopted in the United States.
Packing is beneficial in patients who do not appear to have an indication for laparotomy but
who remain hemodynamically unstable despite blood transfusion (see Fig. 88-1). The
interventional radiology suite is not an ideal place for these patients, so packing in the
operating room, followed by pelvic stabilization, can help with hemorrhage control. More
prospective studies are needed for this to gain wide acceptance in the United States.
11. What types of injuries are associated with genitourinary trauma?
Pelvic fracture can cause posterior (above the urogenital diaphragm) urethral tears or bladder
trauma, whereas perineal straddle injury is more likely to cause anterior urethral tear.
Fractures of the lower ribs, lower thoracic, or lumbar vertebrae are often associated with
renal or ureteral injuries.
12. What is considered a true genitourinary emergency?
Most genitourinary trauma is not life-threatening and can be addressed after stabilization of the
patient, including necessary operative control of significant hemorrhage and contamination.
However, renal pedicle injury can lead to uncontrolled hemorrhage or renal ischemia. The
kidneys are not fixed and move to a limited degree on the vascular pedicle. Complete severance
of this pedicle can lead to exsanguination, whereas lesser injury to the renal vessels can cause
thrombosis and subsequent ischemia. This is typically seen with deceleration injury. Early
diagnosis and surgical intervention are crucial for salvage of the affected kidney.
13. What four clinical signs may indicate injury to the kidney?
n
Flank ecchymosis
n
Lateral abdominal tenderness or mass
n
Hematuria
n
Fracture of lumbar posterior ribs or lumbar vertebrae
14. What is the general management strategy for renal injury?
Nonoperative management is appropriate in the large majority of patients because injuries will
heal spontaneously. Surgery is indicated for hemodynamic instability, ongoing bleeding, or
urinary extravasation. However, minimally invasive techniques, such as angio embolization for
hemorrhage and stenting for urinary extravasation, may allow renal salvage.
15. What diagnostic tools can be used to evaluate renal trauma?
CT is the preferred modality for the evaluation of blunt abdominal trauma. It allows for
comprehensive evaluation of all intra-abdominal structures. Helical CT has increased
sensitivity for ureteral injury. Intravenous pyelography (IVP) is less sensitive and does not
allow for evaluation of nonurologic injuries. However, it may still be used in cases of
suspected renal or ureteral injury when CT is unavailable, or if urologic imaging is required
in the operating room. Renal angiography may be indicated in the presence of a suspected
vascular injury, although it has also largely been replaced by CT. Magnetic resonance
Chapter 88 PELVIC FRACTURES AND GENITOURINARY TRAUMA 611
imaging (MRI) has imaging capabilities similar to CT but is far more expensive, time
consuming, and not as readily available. MRI may be useful in stable patients with contrast
allergies.
16. When should ureteral trauma be suspected?
In the presence of penetrating injuries in proximity to the ureter. These are the least common
of the genitourinary injuries. Hematuria may be absent when the ureter is completely
transected. Ureteral injuries can be detected by CT or IVP and should be managed operatively.
17. What are the associated clinical findings with bladder injury?
Traumatic bladder rupture is an uncommon injury secondary to the protected location of the
bladder within the pelvis. This injury most often occurs in conjunction with pelvic fracture but
can also be seen with lower abdominal compression due to lap belt or steering wheel injuries.
Gross hematuria is present in greater than 95% of patients.
18. How should bladder injury be evaluated?
The two main diagnostic modalities for evaluation of bladder injury are CT cystography and
conventional retrograde cystography. The accuracy of either method depends on adequate
distention of the bladder. Bladder imaging is mandatory in the setting of gross hematuria with
pelvic fracture. Relative indications include gross hematuria without pelvic fracture and pelvic
fracture with microhematuria. Penetrating trauma in the vicinity of the bladder should be
evaluated with a cystogram regardless of the presence of hematuria.
19. When should urethral injury be suspected?
Blood is visualized at the urethral meatus in 80% to 90% of patients with urethral injury. Other
signs of urethral injury are penile, scrotal, or perineal hematomas or a high-riding prostate on
rectal examination. If urethral injury is suspected, insertion of Foley catheter should be
deferred until retrograde urethrogram can be performed. The ED management of complete
urethral disruption is transcutaneous suprapubic cystostomy.
20. How is a retrograde urethrogram performed?
The urethrogram is obtained using a 12-French urinary catheter secured in the meatal fossa
by inflating the balloon to approximately 3 mL. Alternatively, a catheter-tipped syringe may be
used. Standard water-soluble contrast material (25–30 mL) is injected under gentle pressure
as the anteroposterior and oblique views are taken.
1. Renal injury is the most frequent urologic trauma.
2. Renal pedicle injury can lead to uncontrolled hemorrhage or ischemia.
3. Clinical signs of kidney damage may include flank ecchymosis, lateral abdominal tenderness
or mass, hematuria, or fracture of lumbar posterior ribs or lumbar vertebrae.
4. Gross hematuria or persistent microhematuria warrant evaluation.
5. Urologic injury may be present in the absence of hematuria.
KEY POINTS: UROLOGIC TRAUMA
21. What is the diagnostic approach to asymptomatic microhematuria in the
patient with blunt trauma?
Asymptomatic microscopic hematuria is not a good predictor of genitourinary tract injury.
The amount of blood in the urine does not correlate with severity of injury. The relatively low
incidence of positive studies requiring surgery does not justify an extensive radiographic
Chapter 88 PELVIC FRACTURES AND GENITOURINARY TRAUMA612
evaluation. Close follow-up of these patients and repeat urinalyses are recommended, with
additional studies only if the hematuria persists. Controversy still exists regarding the evaluation
of pediatric patients with asymptomatic microhematuria. Pediatric patients are more susceptible
to significant renal injury with relatively benign mechanisms, and consequently many advocate
imaging studies with any degree of hematuria regardless of symptoms.
22. What is a penile fracture?
A sudden tear in the tunica albuginea with subsequent rupture of the corpora cavernosum.
It occurs only in the erect penis and usually is associated with falls or sudden unexpected
moves during sexual intercourse. It has also been reported with direct blunt trauma. A sudden
intense pain associated with a snapping noise and immediate detumescence usually occurs.
Most authors support surgical intervention in an attempt to restore normal function and
prevent angulation. Inability to urinate, bleeding from the urethral meatus, or extravasation
of urine may indicate injury to the corpora spongiosum and urethra, which occurs in
approximately 20% of cases.
23. What is the role of ultrasound in the evaluation of testicular trauma?
Testicular injuries are most often caused by a fall or a kick to the scrotal area. Ultrasound is a
valuable tool in assessing the integrity of the testicles. Adequate palpation may be prevented
by hematoma formation. Ultrasound can distinguish between simple hematoma and disruption
of the parenchyma. Failure to suspect and diagnose testicular rupture may result in
subsequent loss of the testicle.
BIBLIOGRAPHY
1. Biffl WL, Smith WR, Moore EE, et al: Evolution of a multidisciplinary clinical pathway for the management of
unstable patients with pelvic fractures. Ann Surg 233:843–850, 2001.
2. Burch JM, Feliciano DV, Mattox KL: Colostomy and drainage for civilian rectal injuries: is that all? Ann Surg
209:600–611, 1989.
3. Coburn M: Genitourinary trauma. In Feliciano DV, Mattox KL, Moore EE, editors: Trauma, ed 6, New York,
2008, McGraw-Hill, pp 789–825.
4. Cothren CC, Osborn PM, Moore EE, et al: Preperitonal pelvic packing for hemodynamically unstable pelvic
fractures: a paradigm shift. J Trauma 62:834, 2007.
5. Gonzalez RP, Falimirski ME, Holevar MR: The role of presacral drainage in the management of penetrating
rectal injuries. J Trauma 45:656–661, 1998.
6. Iverson AJ, Morey AF: Radiographic evaluation of suspected bladder rupture following blunt trauma: critical
review. World J Surg 25:1588–1591, 2001.
7. Mohany K, Musso D, Powell JN, et al: Emergent management of pelvic ring injuries: an update. Can J Surg
48:49–56, 2005.
8. Scalea TM, Stein DM, O’Toole RV: Pelvic fractures. In Feliciano DV, Mattox KL, Moore EE, editors: Trauma,
ed 6, New York, 2008, McGraw-Hill, pp 759–788.
9. Smith JK, Kenney PJ: Imaging of renal trauma. Radiol Clin North Am 41:1019–1035, 2003.
10. Tile M: Acute pelvic fractures. I: Causation and classification. J Am Acad Orthop Surg 4:143–160, 1996.
11. Young JWR, Burgess AR, Brumback RJ, et al: Pelvic fractures: value of plain radiography in early assessment
and management. Radiology 160:445–451, 1986.
613
CHAPTER 89
TRAUMA IN PREGNANCY
Jedd Roe, MD, MBA, and Bophal Sarha Hang, MD
1. What is the most important concept I need to remember from this chapter?
Fetal outcome is largely related to maternal morbidity. The best fetal resuscitation is
aggressive maternal resuscitation.
2. How common is trauma in pregnancy?
An estimated 6% to 7% of pregnancies are complicated by trauma. In blunt abdominal
trauma, the usual causes are motor vehicle accidents (MVAs; 60%), falls (22%), and direct
blows (17%) to the abdomen. One study showed that serious MVAs accounted for a 7%
maternal mortality rate, whereas the fetal mortality rate was 15%. Of falls, 80% occur after
32 weeks of gestation.
3. Is physical or sexual abuse seen frequently in pregnant patients?
Yes. One large study reported a prevalence of abuse in pregnant women in urban settings of
32%. Of physically abused women, 60% reported two or more episodes of assault. Injury was
more common to the head, neck, and extremities; a fourfold increase in the incidence of
genital trauma was noted in this population. When pregnant patients are physically abused,
there is a higher incidence of low-birth-weight infants, low maternal weight gain, maternal
anemia, and drug and alcohol abuse. Homicides account for one third of maternal trauma
deaths. In low-income pregnant women, there have been reported high rates of violence-
related abdominal trauma. Another study showed that three screening questions asked of
pregnant patients in the ED can detect the majority of patients who are victims of partner
abuse, which suggests that screening for domestic violence should be pursued with pregnant
trauma patients. (See Chapter 98.)
4. How do physiologic changes in pregnancy affect the evaluation of the trauma
victim?
First, decreasing blood pressure and rising heart rate might indicate hypovolemic shock in
a nonpregnant woman, but in pregnancy this may merely reflect physiologic changes or
supine positioning. The maternal blood volume increases 50%. As a result, signs of shock
may not be clinically apparent until 2000 mL or 30% to 40% of maternal blood volume is lost.
Furthermore, uterine flow comprises 20% of cardiac output, approximately 600 mL/min. Given
the markedly increased blood flow, the uterus is a new potential source of blood loss that
requires aggressive investigation. Because physiologic changes result in increased oxygen
demand and decreased oxygen reserve, tissue hypoxia develops more rapidly in response to a
traumatic insult. Also, placental blood flow has no autoregulation and thus, small changes in
blood pressure can result in fetal distress.
5. How do physiologic changes of pregnancy affect laboratory values?
A physiologic anemia is seen as the plasma volume rises by more than twice the amount of
red blood cells. It is not unusual for one to see hematocrits of 32% to 34% by the third
trimester. Fibrinogen levels are double those seen in other trauma patients. Disseminated
intravascular coagulation (DIC) may be seen with normal fibrinogen levels. Because of
hormonal stimulation of the central respiratory drive, PCO
2
falls between 27 and 32 mm Hg,
Chapter 89 TRAUMA IN PREGNANCY614
and injury sufficient to cause a respiratory acidosis might be manifested by what ordinarily
would be considered a normal PCO
2
of 40 mm Hg.
6. Are serious maternal injuries required for fetal injury to be present?
Not always. Although in utero damage is often associated with maternal pelvic fractures, 7%
of maternal cases of minor trauma have been associated with poor fetal outcome. Direct
injuries to the fetus in utero are unusual, but given the size of the fetal head, when direct
trauma occurs, fetal head injury is the most common injury.
7. Name the most common causes of fetal death.
Maternal death, maternal shock, and placental abruption.
8. How does placental abruption occur?
Abruption results from the separation of a relatively inelastic placenta from an elastic uterus
secondary due to a shearing, deceleration force. There may be little or no external evidence
of such a mechanism. Although abruption may be present in 50% of patients with life-
threatening injuries, it also exists in 2% to 4% of minor mechanisms. Classically, the clinical
findings of abruption have included vaginal bleeding and abdominal and uterine tenderness.
In many cases, fetal distress may be the only presenting sign because the reduction in
placental blood flow to the fetus causes hypoxia and acidosis. DIC may occur with placental
injury, and evaluation for DIC can be performed by screening with a serum fibrinogen level,
with low levels stimulating the sending of a more complete DIC panel.
9. How often does ultrasound detect cases of placental abruption?
Because a large separation must be present for ultrasound to be diagnostic, it detects only
about half of cases. In many instances, fetal distress is present before the clear visualization
of an abruption by ultrasound. Fetal mortality from abruption is reported to be 30% to 68%.
Usually an abruption large enough to place the fetus at risk becomes apparent within
48 hours. Detection of fetal distress mandates prompt delivery of the fetus.
10. Are radiologic investigations harmful to the fetus?
The fundamental effects of radiation on the developing fetus are intrauterine growth
retardation and defects in the central nervous system (microcephaly, mental retardation).
The most vulnerable period is between 2 and 15 weeks’ gestation. Cumulative exposure of
less than 5 rads (0.05 Gy) during pregnancy has not been shown to affect the outcome of
pregnancy compared to control populations. In general, all radiographic studies should be
undertaken with appropriate fetal shielding. All clinically indicated studies should be done
regardless of any radiation concerns. Furthermore, there has been no reported adverse effects
on neonatal thyroid function with the use of iodinated contrast, and it should be administered
if absolutely necessary. Consideration also should be given to nonradiographic alternative
evaluation with ultrasound. See Chapter 9 for radiation exposures from diagnostic imaging
studies.
11. How should these patients be managed in the field?
Given the reduced maternal oxygen reserve, oxygen therapy is crucial. Intravenous volume
resuscitation with crystalloid should proceed as with other trauma patients. Avoid
compression of the inferior vena cava by transporting the patient on her left side, or if the
patient is immobilized, elevate the right side of the backboard to 15 or 20 degrees. Aside from
early transport, the most important aspect of prehospital management is to notify the ED so
that the appropriate obstetric consultants may participate on the trauma team.
12. What are the priorities for ED management?
The prehospital therapies mentioned previously should be continued. Of particular interest is
the history of this pregnancy with attention directed at estimating gestational age and fetal
viability. After the usual primary and secondary survey, a sterile speculum examination should
be performed to evaluate for the presence of vaginal fluid, opening of the cervical os, and

Chapter 89 TRAUMA IN PREGNANCY 615
genital tract trauma. Continued aggressive resuscitation with warmed lactated Ringer’s
solution (less acidotic, more physiologic) and blood is especially important given the
physiologic changes mentioned previously.
13. How do I begin to evaluate the fetus?
First, determine the size of the uterus and the presence of abdominal and uterine tenderness.
Uterine size, measured in centimeters from the pubic symphysis to fundus, provides a rough
estimate of gestational age and potential viability. Carefully inspect the vaginal introitus for
evidence of vaginal bleeding. Next, assess for fetal distress, which may be the earliest
indication of maternal hypovolemia. Abnormal fetal heart rates are greater than 160 beats
per minute and less than 120 beats per minute. As soon as possible after patient arrival,
continuous cardiotocographic monitoring (CTM) should be initiated to ascertain early signs of
fetal distress (e.g., decreased variability of heart rate or fetal decelerations after contractions).
Ultrasound should be done promptly thereafter to confirm gestational age, fetal viability, and
the integrity of the placenta.
14. Is diagnostic peritoneal lavage (DPL) safe and accurate in pregnant women?
DPL has been reported to be safe and accurate when using an open, supraumbilical technique.
Although the cell count thresholds and clinical indications for DPL are the same, ED
ultrasound has become the more prevalent investigation. The physiologic changes that take
place with pregnancy and the elimination of radiation exposure from abdominal computed
tomography (CT) provide persuasive arguments for aggressive use of ED ultrasound as a
diagnostic tool. With the exception of concern for diaphragmatic injury secondary to
penetrating trauma, the need for DPL as an evaluation modality has largely been supplanted
by the use of ED ultrasound (focused abdominal sonogram of trauma [FAST]) to determine
rapidly the presence of intraperitoneal hemorrhage.
15. What is fetomaternal hemorrhage (FMH)?
Hemorrhage of fetal blood into the usually distinct maternal circulation. The incidence of
FMH in trauma patients has been reported to be 30% (four to five times the incidence of
noninjured controls). With FMH, the complications of maternal Rh sensitization, fetal
anemia, and fetal death can occur. Laboratory techniques are not sensitive enough to
diagnose FMH accurately. The prudent course is to give Rh immunoglobulin to all Rh-
negative patients who present with the suspicion of abdominal trauma because a 300-mg
dose of Rh immunoglobulin given within 72 hours of antigenic exposure prevents Rh
isoimmunization. Massive transfusion (.30 mL) into the maternal circulation sometimes is
seen with severe abdominal trauma. The Kleihauer-Betke (KB) test detects fetal erythrocytes
in the maternal circulation, and positive KB tests have not been shown to alter management
except in Rh-negative patients. However, one study showed that the incidence of positive KB
tests did not differ between low-risk pregnant patients and maternal trauma patients. Given
the inaccuracy of the KB test in the setting of trauma, administration of Rh immunoglobulin
should proceed as described previously.
16. When is cesarean section indicated?
The first factor to be considered is the stability of the mother. If the mother has sustained
serious injuries elsewhere and is critically ill, she may not be able to tolerate an additional
procedure and the blood loss it would entail. Next, fetuses whose gestational age is 24 weeks
or whose weight is estimated to be greater than 750 gm are predicted to have a 50% survival
rate in the neonatal intensive care unit (ICU) setting and are considered viable. The most
common indication for cesarean section is fetal distress. Other indications are uterine rupture
and malpresentation of the fetus. Perimortem cesarean section should be done when
ultrasound or uterine size suggests viability (i.e., above the umbilicus) and maternal
decompensation is acute. Resuscitation should be instituted within 4 minutes, but fetal
survival with normal neurologic outcome has been reported 40 minutes after maternal
decompensation.
Chapter 89 TRAUMA IN PREGNANCY616
17. Which pregnant patients with abdominal trauma require admission for fetal
monitoring?
Any viable (.23-24 weeks) fetus requires continuous fetal monitoring or CTM. CTM is
recommended even for patients without external evidence of trauma because it has been well
documented that these patients are at risk from placental abruption, and CTM is sensitive for
its detection. Current guidelines suggest that these patients be observed for a minimum of
4 hours with a cardiotocograph. If any abnormalities are discovered, including more than
four uterine contractions/hour, amniotic membrane rupture, vaginal bleeding, serious maternal
injury, significant abdominal pain, and signs of fetal distress, the patient should be
hospitalized and monitored for 24 hours.
1. Aggressive maternal resuscitation is the best therapy for the fetus.
2. The fetus may be in acute distress with little or no maternal manifestations.
3. Ultrasound is the investigation of choice to evaluate the maternal abdomen and the fetus.
4. All clinically necessary radiologic investigations should be performed regardless of radiation
concerns.
KEY POINTS: TRAUMA IN PREGNANCY
www.perinatology.com/exposures/Physical/Xray.htm
WEBSITE
BIBLIOGRAPHY
1. Capobianco G, Balata A, Mannazzu MC, et al: Perimortem cesarean delivery 30 minutes after a laboring
patient jumped from a fourth-floor window: baby survives and is normal at age 4 years. Am J Obstet Gynecol
198(1):e15–e16, 2008.
2. Chames MC, Pearlman MD: Trauma during pregnancy: Outcomes and clinical management. Clin Obstet Gyne
51(2):398–408, 2008.
3. Chen MM, Coakley FV, Kaimal A, et al: Guidelines for computer tomography and magnetic resonance imaging
use during pregnancy and lactation. Obstet Gynecol 112:333–340, 2008.
4. Dhanraj D, Lambers D: The incidences of positive Kleihauer-Betke test in low-risk pregnancies and maternal
trauma patients. Am J Obstet Gynecol 190:1461–1463, 2004.
5. El Kady D, Gilbert WM, Anderson J, et al: Trauma during pregnancy: an analysis of maternal and fetal
outcomes in a large population. Am J Obstet Gynecol 190:1661–1668, 2004.
6. Feldhaus KM, Koziol-McLain J, Amsbury HL, et al: Accuracy of 3 brief screening questions for detecting
partner violence in the emergency department. JAMA 277:1400–1401, 1997.
7. Hill CC, Pickinpaugh J: Trauma and surgical emergencies in the obstetric patient. Surg Clin North Am 88:
421–440, 2008.
8. Ikossi DG, Lazar AA, Morabito D, et al: Profiles of mothers at risk: an analysis of injury and pregnancy loss in
1,195 trauma patients. J Am Coll Surg 200:49–56, 2005.
9. Nannini A, Lazar J, Berg C, et al : Physical injuries reported on hospital visits for assault during the
pregnancy-associated period. Nurs Res 57(3):144–149, 2008.
10. Shah AJ, Kilcline BA: Trauma in pregnancy. Emerg Med Clin North Am 21:615–629, 2003.
617
CHAPTER 90
PEDIATRIC TRAUMA
Katherine M. Bakes, MD, and Walter L. Biffl, MD, FACS
1. Which children get injured? How do they do it?
Every year, nearly one in three children is injured. Trauma is the leading cause of mortality for
children younger than 14 years, greater than all other causes combined in children older than
1 year of age. Motor vehicle crashes account for most deaths in all age groups, followed by
drownings, house fires, homicides, and falls in descending order. A very common site of lethal
pediatric trauma is the home. Boys are injured twice as often as girls. Falls are the most
common cause of severe injury in infants and toddlers; bicycle crashes are the most common
cause in children and adolescents.
2. Aren’t children just little adults?
No. Anatomically, unique characteristics in children require special consideration:
n
A smaller body mass results in more force applied per unit area, with a propensity toward
multiple injuries in a child. An example of this is Waddell’s triad: a femur fracture, truncal
trauma (i.e., intra-abdominal or intrathoracic injury), and head injury, typically occurring
after a child is struck by an automobile at high speed.
n
Due to a greater head-to-body ratio, thinner cranial bones and less myelinated brain tissue,
intracranial injury is the leading cause of mortality and morbidity in the pediatric trauma
population.
n
Relatively larger solid organs with relatively smaller thoracic and pelvic bony structures,
coupled with less subcutaneous fat and less mature abdominal musculature, makes
intra-abdominal solid organs more anatomically susceptible to injury.
n
A child’s incompletely calcified and thus compliant skeleton allows internal organ damage
without overlying fractures.
n
A high body surface area-to-volume ratio results in significant thermal energy loss and
early hypothermia in a child.
3. How does prioritization of ABCs differ between children and adults?
Airway, breathing, and circulation always take priority in that order, whether in an adult or a
child. Relative to adults, children have a higher baseline respiratory rate due to increased
metabolic demands. Blood loss and an increase in lactate production can quickly lead to
marked increased work of breathing and respiratory arrest from fatigue. Thus, tachypnea can
be the first clue to the child with acute blood loss. Tachycardia may be a manifestation of
emotional factors in the injured child but should not be easily dismissed as such. Tracking
the patient’s capillary refill time and urine output with repeated vital signs can help guide the
provider. Bradycardia in a child is often secondary to head injury, hypoxia, or inadequate
ventilation. In the setting of trauma without respiratory compromise, bradycardia is an
ominous sign.
4. Which factors affect the patency of a child’s airway?
Particularly in infants, craniofacial disproportion (the child’s occiput is relatively large
compared with the midface) results in cervical flexion when the child is lying supine. To align
the oral, pharyngeal, and tracheal axes, a roll may be placed under the shoulders in very
young children. Compared with an adult, a child has a large tongue, floppy epiglottis, and
increased lymphoid tissue; these factors may contribute to airway obstruction. The sniffing
