Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 91 MUSCULOSKELETAL TRAUMA AND CONDITIONS OF THE EXTREMITY628
40. What is a locked knee? What are the most common causes?
The patient is unable to extend the knee actively or passively beyond 10- to 45-degree flexion.
True locking and unlocking occur suddenly. The most common causes are a tear of the medial
meniscus, a loose body or joint mouse (osteochondral fragment) in the knee, or a dislocated
patella.
41. What injuries are associated with a calcaneal fracture?
Depending on the exact mechanism of injury and the type of calcaneal fracture, 10% to 50%
of patients have an associated compression fracture of the lumbar or lower thoracic spine. Of
calcaneal injuries, 10% are bilateral, and about 25% are associated with other lower extremity
injuries; 10% can result in a compartment syndrome of the foot, requiring fasciotomy.
42. What is the most common direction of a tibiofemoral knee dislocation?
Anterior (the tibia’s relationship to the femur). The mechanism of an anterior knee dislocation
is hyperextension of the knee. There is a 30% to 50% chance of a popliteal artery injury
following this type of dislocation.
43. What direction is considered the irreducible knee dislocation?
Posterolateral (the tibia is posterolateral to the femur). The medial femoral condyle produces a
dimple sign as it buttonholes through the anteromedial joint capsule becoming entrapped. An
open reduction in the operating room is required.
44. What vascular injury must be considered with a tibiofemoral knee
dislocation?
Injury or compression of the popliteal artery. Cadaver studies showed that anterior
dislocations tend to cause intimal flaps and occlusion, whereas posterior dislocations are
more likely to cause a rupture of the popliteal artery. Injuries also occur at the trifurcation just
distal to the popliteal fossa. Postreduction angiography should be considered for all patients
with abnormal distal pulses or ankle-brachial index.
45. How is the ankle-brachial index (ABI) calculated?
ABI 5 Doppler systolic arterial pressure in the injured limb (ankle)
Doppler systolic arterial pressure in uninjured limb (brachial)
An ABI value of 0.9 is considered normal. The ABI measurement may be inaccurate in
patients with risk factors for peripheral arterial disease, such as diabetes and hypertension.
Vessel calcification in the elderly can also increase the risk of a false-positive result.
PEDIATRIC ORTHOPEDICS
46. What is a torus or buckle fracture?
This fracture is typically seen in the metaphysis of the radius but is not limited to this
bone. Torus means a round swelling or protuberance. In children, the cortical bone and
metaphyseal bone fail in compression (buckling), while the opposite cortex remains
intact. The area of bone that fails in compression forms a torus. Because the opposite
cortex remains intact, these fractures are stable and require splint or cast immobilization
for 4 weeks.
47. What is a greenstick fracture?
Children’s bones have increased elasticity. An angular force applied to a long bone of a child
causes a greenstick fracture. One cortex fails in tension, while the opposite cortex bows but
does not fail or fracture in compression. The fracture is similar to what occurs when one
attempts to break a green branch of a tree. This fracture pattern is common in the radius and
ulna. These fractures require reduction, and often the fracture must be completed to achieve
an adequate reduction. Immobilization in a cast is required for 6 weeks.
Chapter 91 MUSCULOSKELETAL TRAUMA AND CONDITIONS OF THE EXTREMITY 629
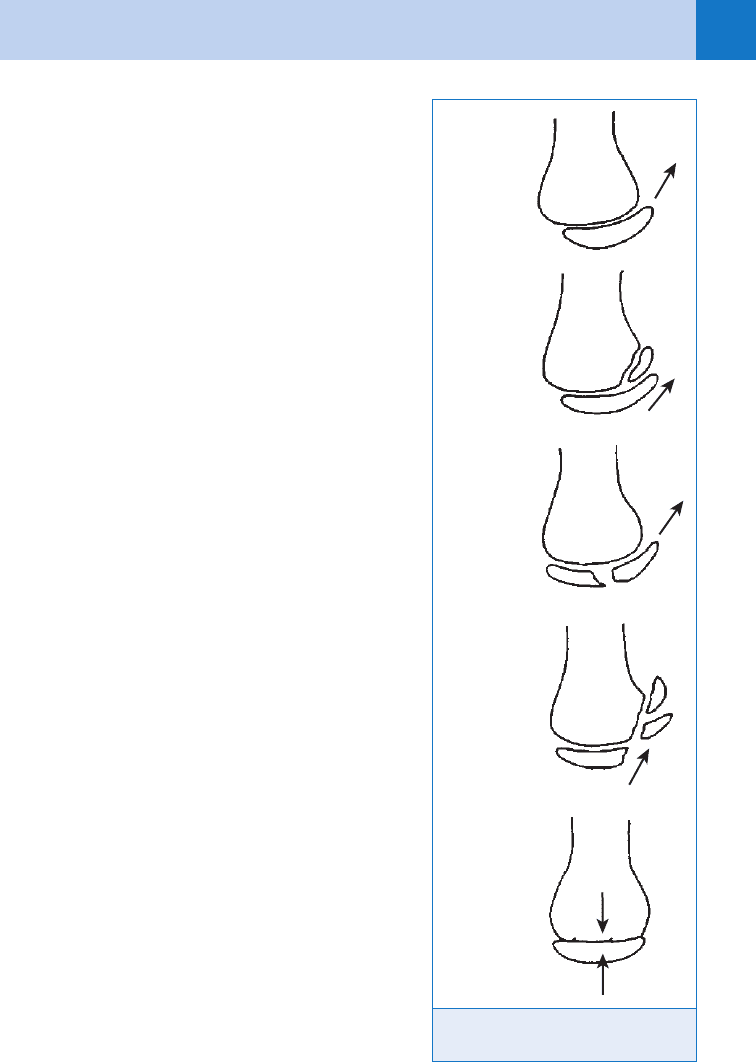
48. What is the Salter-Harris classification?
What is its clinical significance?
A method of classifying epiphyseal injuries
(Fig. 91-1). Fractures involving the epiphysis
may result in growth disturbance, and parents
must be informed of this potential. About 80%
of these injuries are Salter-Harris types I and
II, both of which have a low complication rate.
Salter-Harris types III, IV, and V injuries have a
more variable prognosis. Displaced Salter-
Harris types III and IV fractures may require
open reduction to restore the normal
relationship of the epiphysis and articular
surface. The five types are summarized as
follows:
n
Type I: Fracture extends through the
epiphyseal plate, resulting in displacement of
the epiphysis (this may appear merely as
widening of the radiolucent area representing
the growth plate).
n
Type II: Fracture is as above, with an
additional fracture of a triangular segment of
metaphysis.
n
Type III: Fracture line runs from the joint
surface through the epiphyseal plate and
epiphysis.
n
Type IV: Fracture line also occurs in type III
but also passes through adjacent metaphysis.
n
Type V: A crush injury of the epiphysis
occurs, which may be difficult to determine
by x-ray examination.
49. Describe the vascular complications
associated with pediatric supracondylar
humerus fractures.
Displaced supracondylar humerus fractures in
children have a 5% incidence of vascular
compromise. The brachial artery typically is
compressed or lacerated by the anteriorly
displaced humeral shaft. Posterior lateral
displacement of the supracondylar fracture is
the fracture pattern most likely to result in
vascular injury. The child with a viable hand
and absent pulse should undergo prompt
reduction and fracture fixation in the operating
room, with re-evaluation of the vascular status
after the procedure. In the patient with an
absent pulse and a devascularized hand,
longitudinal traction and splinting should be
done in the ED in an attempt to reconstitute
flow to the distal extremity. Prompt
consultation with orthopedic and vascular
surgeons is required.
Type I
Type II
Type III
Type IV
Type V
Figure 91-1. Salter-Harris classification
of epiphyseal injuries.
Chapter 91 MUSCULOSKELETAL TRAUMA AND CONDITIONS OF THE EXTREMITY630
50. Describe the neurologic complications associated with pediatric
supracondylar humerus fractures.
The anterior interosseous nerve (branch of the median nerve) is potentially the most
commonly injured nerve. This nerve innervates the deep compartment of the forearm, which
consists of the flexor digitorum profundus to the index, the pronator quadratus, and the flexor
pollicis longus. The nerve can be checked by evaluating flexor pollicis longus function at the
interphalangeal joint of the thumb. The radial nerve is the next most commonly injured nerve,
followed by the ulnar nerve. A thorough physical examination must be done to identify these
injuries, a difficult task in the small child.
KEY POINTS: MUSCULOSKELETAL TRAUMA AND CONDITIONS
OF THE EXTREMITY
1. Never place an amputated part directly on ice or immerse in water.
2. Bleeding from a wound is best controlled with direct pressure
3. Multidisciplinary approach is paramount in the treatment of pelvic hemorrhage.
4. Knee dislocations require a thorough vascular examination.
5. Always rule out infection in a child presenting with atraumatic hip pain.
6. In nonambulating children with humeral or femoral fractures, be suspicious of child abuse.
51. What is a nursemaid’s or pulled elbow? What is its management?
A longitudinal pull on the outstretched arm of a 1- to 5-year-old child may result in a
subluxation of the annular ligament over cartilaginous radial head. The child typically presents
with pseudoparalysis of the injured extremity. Radiographs are negative for fracture or radial
head dislocation. Reduction involves simultaneous supination of the forearm and flexion of the
elbow. A distinct click over the radial head signifies reduction. The child often begins to use
the extremity within minutes of reduction. The parent or caregiver should be educated to avoid
longitudinal traction on the arm to prevent this from occurring in the future.
52. Describe the potential implications of a humeral or femoral fracture in a small
child.
In the nonambulating child with these fractures, the suspicion of child abuse should be high.
An unwitnessed event or a history that does not correspond to the injuries is another potential
sign of abuse. Careful examination of the child should be done, looking specifically for skin
bruises or burns, retinal hemorrhage, and evidence of previous fracture. A skeletal survey
should be considered because the presence of fractures at different stages of healing is a
sign of abuse. All cases of suspected abuse need to be reported to the local authorities.
(See Chapter 65.)
53. What is Waddell’s triad?
The constellation of injuries in a child struck by a car:
n
Femoral fracture
n
Intrathoracic or intra-abdominal injury
n
Head injury
54. Which nontraumatic hip disorders cause a limp in a child?
n
Septic arthritis
n
Transient synovitis (ages 2–12 years)
n
Idiopathic avascular necrosis (boys, ages 5–9 years)
n
Slipped capital femoral epiphysis (SCFE) (boys, ages 10–16 years)
Chapter 91 MUSCULOSKELETAL TRAUMA AND CONDITIONS OF THE EXTREMITY 631
n
Perthes’ disease
n
Juvenile rheumatoid arthritis
All are uncommon. Transient synovitis is probably the most common cause of nontraumatic
limp in a child but is a diagnosis of exclusion.
Symptomatic treatment is prescribed for transient synovitis, including nonsteroidal anti-
inflammatory drugs and non-weight bearing or bed rest. Untreated or delayed treatment of
septic arthritis can lead to irreversible and catastrophic sequelae from permanent damage and
deformation of the articular cartilage. Infection in a child presenting with atraumatic hip pain
must be convincingly ruled out. The white blood cell count, erythrocyte sedimentation rate,
and body temperature frequently are elevated in cases of infection. If doubt persists, the gold
standard is hip aspiration, usually done in the operating room. Standard anteroposterior and
lateral radiographs of the hip differentiate between Perthes’ disease and a slipped capital
femoral epiphysis.
55. What are the early radiographic findings of an SCFE?
Any asymmetry of the relationship of the femoral head to the femoral neck should raise the
suspicion of SCFE, even if evident on only one X-ray view. If anteroposterior and lateral
radiographs are normal, frog-leg views should be obtained. Comparison of the two hips may
not be helpful in discerning subtle changes because SCFE is bilateral in 20% of cases.
56. What is the ED management of a child with injury and tenderness over an
open epiphysis but a normal radiograph?
It is best to assume the child has sustained an undeterminable fracture of the physis
(Salter-Harris type I or V). Immobilize the joint in a posterior splint, and keep the child
non-weight bearing if the lower extremity is involved. Parents should be notified of the
possibility of this type of injury and the potential for growth disturbance. The need for
prompt follow-up must be emphasized and is best arranged before discharging the child
from the ED. A nondisplaced physeal fracture that becomes displaced because of lack of
immobilization can have significant long-term consequences. Short-term extremity
immobilization in an appropriately applied splint or cast is well tolerated. When in
doubt, immobilize.
BIBLIOGRAPHY
1. Browner BD, Trafton PG, Green NE, et al, editors: Skeletal trauma: basic science, management, and
reconstruction, ed 3, Philadelphia, 2002, W.B. Saunders.
2. Burkhead WZ Jr, Rockwood CA Jr: Treatment of instability of the shoulder with an exercise program. J Bone
Joint Surg Am 68:724–731, 1986.
3. Green OP, Hotchkiss RN, Pederson WC: Green’s operative hand surgery, ed 4, New York, 1999, Churchill
Livingstone.
4. Grotz MRW, Allami MK, Harwood P, et al: Open pelvic fractures: epidemiology, current concepts of
management outcome. Injury 1:1–13, 2005.
5. Lovell WW, Winter RB, Morrissy RT, et al: Lovell and Winter’s pediatric orthopaedics, ed 5, Philadelphia, 2001,
Lippincott Williams & Wilkins.
6. Mills WJ, Barei DP, McNair P: The value of the ankle-brachial index for diagnosing arterial injury after knee
dislocation: a prospective study. J Trauma 56:1261–1265, 2004.
7. Pagnani MJ, Galinat BJ, Warren RF: Glenohumeral instability. In DeLee JC, Drez D Jr, editors: Orthopaedics
sports medicine: principles and practice. Philadelphia, 1994, WB Saunders, vol 1, pp 580–622.
8. Pollock RG, Bigliani LU: Recurrent posterior shoulder instability: diagnosis and treatment. Clin Orthop
291:85–96, 1993.
9. Rockwood CA, Green DP, Bucholz RW, et al: Rockwood and Green’s fractures in adults, ed 5, Philadelphia,
2001, Lippincott Williams & Wilkins.
10. Rockwood CA, Green DP, Bucholz RW, et al: Rockwood and Green’s fractures in children, ed 5, Philadelphia,
2001, Lippincott Williams & Wilkins.
632
HAND INJURIES AND INFECTIONS
CHAPTER 92
Michael A. Kohn, MD, MPP
1. Are hand problems important in emergency medicine?
Yes. Our hands are our interface to the mechanical world, so they are frequently injured or
exposed to infection. There are 4.8 million ED visits per year for hand/wrist injuries. At least
one of every eight injury-related ED visits is for a hand/wrist injury.
2. List the essential elements of the history.
n
Age
n
Dominant hand
n
Occupation
n
How, where, and when injury occurred
n
Posture of hand when injured
n
Tetanus status
n
Prior injury or disability of the hand
3. List the elements of a complete hand examination.
n
Initial inspection of skin and soft tissue
n
Vascular examination
n
Evaluation of tendon function
n
Nerve examination (motor and sensory)
n
Determination of joint capsule integrity
n
Skeletal examination
4. What is topographical anticipation?
Looking at the skin wound and thinking about which underlying structure (vessel, tendon,
nerve, bone, ligament, or joint) could be injured. Know the anatomy. Do not hesitate to consult
an atlas.
5. What is the normal posture of the hand at rest?
With the wrist in slight extension, the resting fingers normally assume a cascade, progressively
more flexed from index to small. (See this by relaxing your own hand with the wrist in slight
extension.) An alteration in the normal posture can lead to immediate diagnosis of major
tendon and joint injuries.
6. Does dorsal swelling always signify an injury or infection in the dorsum of the
hand?
No. Most of the palmar lymphatics drain to lymph channels and lacunae located in the loose
areolar layer on the dorsum of the hand. Always check for a palmar pathology when a patient
presents with dorsal swelling.
7. What is the Allen test? How is it performed?
The Allen test verifies patency of the radial and ulnar arteries as follows: Occlude radial
and ulnar arteries. Have patient open and close hand five or six times. Hand should blanch.
Release ulnar artery; blanching should resolve within 3 to 5 seconds. Repeat test, releasing
Chapter 92 HAND INJURIES AND INFECTIONS 633
radial artery instead of ulnar artery Blanching should resolve within 3 to 5 seconds. The most
accurate form of the Allen test uses digital blood pressures rather than return of color to monitor
reperfusion.
8. How is function of the flexor digitorum superficialis (FDS) tendon tested?
The FDS inserts on the middle phalanx and flexes the proximal interphalangeal (PIP)
joint. The flexor digitorum profundus (FDP) inserts on the distal phalanx and flexes the
PIP and the distal interphalangeal (DIP) joints. The FDS muscle-tendon units should be
independent of one another, whereas the FDP tendons arise from a common muscle belly.
Testing the FDS of a finger entails flexing it at the PIP joint, while stabilizing the other
three fingers in full extension, thereby taking the FDP out of action as a potential flexor of
the PIP joint.
9. In which finger is the test of FDS function unreliable?
Because the FDP to the index finger can be independent of the other profundi, the FDS test
is unreliable in the index finger. Flexion at the PIP joint may be due to the FDP, even with
the other fingers stabilized in extension. Suspected index finger FDS injuries must be
explored.
10. Why is the flexor or palmar aspect of the hand called the OR side, whereas
the extensor or dorsal aspect is the ED side?
In contrast to the extensors, the flexor tendons run through delicate sheaths. Because of these
sheaths, repairing flexor tendons requires more expertise and a more controlled environment
in the operating room than repairing extensor tendons does.
11. How is a partial tendon laceration diagnosed?
If the location of the skin laceration is suspicious, rule out an underlying partial tendon
laceration by exploration and direct visualization under tourniquet hemostasis. Because a
flexor tendon runs through its sheath like a piston through a cylinder, a sheath laceration
implies a partial tendon laceration, which is visible only when the hand is in the same posture
as when injured. A bloodless field and direct visualization of the tendon during full range of
motion must occur to rule out a partial tendon laceration. All wounds over tendons must be
explored for partial tendon lacerations since range of motion test can still be normal. Never
test for tendon integrity against resistance since a partial tendon laceration can be converted
to a complete (100%) laceration.
12. How do I test the extrinsic extensor tendons?
The extrinsic extensors alone extend the metacarpophalangeal (MCP) joints, whereas they
combine with tendons from the interossei and lumbricals to form the extensor mechanism
that extends the interphalangeal joints. To test the extrinsic extensor, ensure that the patient
can extend at the MCP joint (but see below).
13. Can extensor function to a finger be intact despite complete laceration of the
extensor digitorum communis (EDC) to that finger?
Yes. The juncturae tendinum interlink the EDC tendons at the midmetacarpal level. Even if the
EDC to a finger is completely lacerated in the dorsum of the hand, extension at the MCP still
may be possible because of the junctura.
14. How do I test sensory nerve function?
Assess nerve function before the use of anesthesia. Test digital nerves by checking two-point
discrimination on the volar pad. The two points should be 5 mm apart and aligned
longitudinally.
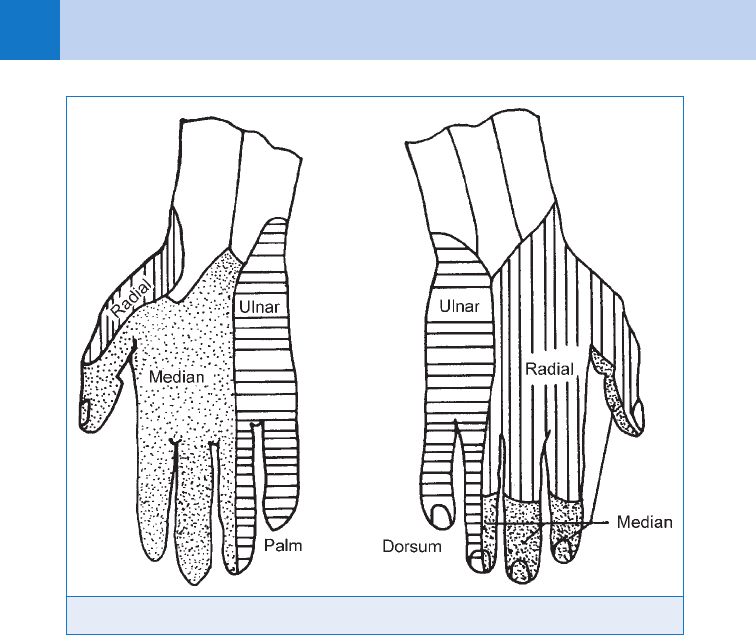
15. What are the sensory distributions of the median, ulnar, and radial nerves?
See Fig. 92-1.
Chapter 92 HAND INJURIES AND INFECTIONS634
Figure. 92-1. Sensory distributions of the median, ulnar, and radial nerves.
16. How is motor function of the median, ulnar, and radial nerves tested?
n
Median: Abductor pollicis brevis (APB)—abducts the thumb against resistance while
palpating the APB muscle belly.
n
Ulnar: First dorsal interosseous—abducts the index finger against resistance.
n
Radial (no intrinsics): Extensor pollicis longus (EPL)—extends the thumb interphalangeal
joint against resistance.
17. Which is the most frequently dislocated carpal bone?
The carpal bones from radial to ulnar side are as follows:
n
Proximal row—scaphoid, lunate, triquetrum, pisiform
n
Distal row—trapezium, trapezoid, capitate, hamate
The lunate is most frequently dislocated. Its blood supply comes through the volar and dorsal
ligaments from the radius. If both ligaments are ruptured, avascular necrosis results.
18. Which is the most frequently fractured carpal bone?
The scaphoid. Its distal blood supply increases the likelihood of avascular necrosis in the
proximal segment after fracture.
19. What is the classic sign of a scaphoid fracture?
Snuffbox tenderness. Even without radiographic evidence of a fracture, the patient with
tenderness to palpation of the anatomic snuffbox gets a thumb spica splint and must have a
repeat radiograph in 2 weeks.
20. How do I control hemorrhage from a hand injury?
Direct pressure and elevation. This will work 99.9% of the time. Elevate and hold pressure for 10
minutes by the clock. Very rarely, an incomplete arterial laceration requires a proximal tourniquet
Chapter 92 HAND INJURIES AND INFECTIONS 635
for temporary control, followed by sensory examination, anesthesia, irrigation, and exploration
under good light and magnification to tie off the bleeding vessel. Never blindly clamp a bleeder.
21. Why the rule, no blind clamping of bleeders?
In the hand, the arteries run in close approximation to the nerves. Blindly clamping an artery
may irreparably damage the associated nerve. Also, the clamp may damage a section of vessel
vital to successful reanastomosis. All hand bleeding can be controlled by direct pressure or a
tourniquet.
22. What should be done with an amputated digit?
Gently clean the digit with sterile saline, wrap it in moist gauze, place it in a sterile container,
and float the container in ice water. (Avoid direct contact between ice and tissue to prevent
freezing.)
23. What should be done with a devascularized but still partially attached digit?
Leave part attached (preserves veins for reimplantation), gently wrap in moist gauze, and
apply a bulky dressing.
24. What are the indications and contraindications for reimplantation?
n
Indications: Multiple finger injury; thumb amputations (especially proximal to
interphalangeal joint); single finger injury in children; clean amputation at hand, wrist,
or distal forearm.
n
Contraindications: Severe crush or avulsion, heavy contamination, single-finger
amputations in adults, severe associated medical problems or injuries, severe multilevel
injury of amputated part, willful self-amputation. Bottom line: Give the hand surgeon the
opportunity to decide.
25. Which are the most deceptive of all serious hand injuries?
High-pressure injection injuries (from paint guns, grease guns, or hydraulic lines) initially
may seem innocuous, often involving just the fingertip. In one published case series, 6 out of
15 high-pressure injection injuries resulted in some form of amputation, and only one patient
regained normal sensation, despite aggressive early surgical treatment.
26. List Kanavel’s four cardinal signs of flexor tenosynovitis.
n
Slightly flexed posture of the digit
n
Fusiform swelling of the digit
n
Pain on passive extension
n
Tenderness along the flexor tendon sheath
Flexor tenosynovitis requires admission and surgery.
27. What is a paronychia? How is it treated?
A common bacterial infection involving the folds of skin that hold the fingernail in place. In the
absence of visible pus, treatment should consist of warm moist compresses, elevation, and
antistaphylococcal antibiotics. If pus is present, do the minimum necessary to drain and
maintain drainage. This usually consists of simply elevating the eponychial fold or making a
small incision. Sometimes removal of a longitudinal section of the nail plate is necessary.
28. How is whitlow different from a paronychia?
Whitlow is infection of the tissue around the nail plate with herpes simplex virus (rather than
bacteria). The discharge is serous and crusting rather than purulent. The patient also may
have perioral cold sores. Do not incise and drain herpetic whitlow.
29. What is a felon? How is it treated?
A painful and potentially disabling infection of the fingertip pulp. Treatment is controversial.
Some clinicians argue for immediate drainage of the tensely swollen and painful fingertip pad.
Others argue that early treatment with antibiotics, elevation, and immobilization may prevent
Chapter 92 HAND INJURIES AND INFECTIONS636
the need for surgical drainage. Even if drainage is necessary, the best method is also a matter
of controversy. The full fishmouth incision has fallen out of favor, but the three-quarter
fishmouth incision and the simple lateral incision are both acceptable.
30. What is a football jersey finger? How is it treated?
Rupture of the FDP occurs commonly when a football player catches his finger in an
opponent’s jersey. The tendon is avulsed from its insertion at the palmar base of the distal
phalanx, often taking a bone fragment along. Surgical repair within the next several days is
indicated.
31. What is a mallet finger? How is it treated?
A mallet finger is the opposite of a football jersey finger; the insertion of the extensor tendon,
rather than the flexor tendon, is avulsed from the dorsum of the distal phalanx, often pulling
off a bone fragment. Appropriate treatment is to splint the DIP joint in extension (not
hyperextension) for 6 weeks.
32. Describe a subungual hematoma. How is it treated?
A collection of blood under the nail plate can be painful. Classically, this occurs when a
weekend carpenter strikes his or her thumb with a hammer. Relieving the pressure by nail
trephination (poking a hole in the nail) will make you a hero to the patient. Use electrocautery,
a red-hot paperclip, or an 18-gauge needle (twisting it between your fingers like a drill bit).
Removal of an intact nail plate is almost never indicated.
33. What is a gamekeeper’s thumb? How is it diagnosed?
A torn ulnar collateral ligament of the thumb MCP joint resulting from forceful abduction of
the thumb. In 1955, the injury was reported in 24 Scottish game wardens, arising from
their technique for breaking the necks of wounded rabbits. The injury is more properly
called skier’s thumb because it most commonly occurs when a skier either catches the
thumb on a planted ski pole or falls while holding a pole in the outstretched hand. The
injury is potentially severely disabling. Complete rupture of the ligament always requires
surgery. ED treatment consists of a thumb spica splint and referral. One way to test for
injury to the ulnar collateral ligament of the thumb MCP is to hand the patient a heavy can
(e.g., of soda) or bottle (e.g., of hydrogen peroxide). If the injury is present, the patient
will be unable to hold the object in the usual way, either supinating to balance the object in
the palm or dropping it.
34. What is a boxer’s fracture?
Fracture of the fifth (small finger) metacarpal is common in barefisted pugilists. Because
the small finger metacarpal is second only to the thumb metacarpal in mobility, large
angles of angulation are tolerated without functional deficit. Nevertheless, attempts to
correct significant angulation of an acute boxer’s fracture are warranted. Any rotational
deformity must be corrected. A laceration accompanying a boxer’s fracture is assumed to
be a fight bite.
35. What is a fight bite?
The most notorious of all nonvenomous bite wounds is the fight bite. As the name implies,
the injury occurs when the soon-to-be-patient punches his or her adversary in the teeth,
lacerating the dorsum of one or more MCP joints. Other names for this injury such as
morsus humanus or closed fist injury have been proposed. Fight bite is more compact,
descriptive, and poetic. All such wounds require formal exploration, including extension of
the skin laceration if necessary. They should be débrided, irrigated, dressed open (no
sutures), and splinted. If the wound penetrates the extensor hood, the MCP joint requires
thorough washout, and strong consideration should be given to hospitalization for
intravenous (IV) antibiotics and meticulous wound care. If the wound is already infected,
hospitalization is mandatory.
Chapter 92 HAND INJURIES AND INFECTIONS 637
KEY POINTS: HAND INJURIES AND INFECTIONS
1. Because scaphoid fractures are frequently radiographically occult, even without X-ray
evidence of a fracture, the patient with tenderness to palpation of the anatomic snuffbox
should be treated with a thumb spica splint and repeat evaluation in 1 to 2 weeks.
2. The most deceptive of serious hand injuries is the high-pressure injection injury sustained
while testing a hydraulic paint or oil gun because, despite seeming innocuous on initial
presentation, these injuries require aggressive, surgical management.
3. Any laceration over the dorsal MCP joint is suspicious for a fight bite. Fight bites require
meticulous exploration and wound care. If the wound penetrates the extensor hood,
thorough joint washout and IV antibiotics are required.
36. Are human bites more dangerous than other animal bites?
No. The fight bite gave human bites their reputation for being more prone to infection than
other animal bites. This probably has more to do with the location of the bite and the typical
delay in treatment than with the mix of organisms in the human mouth. True human bites
(occlusive bites rather than fight bites) have no higher infection rates than animal bites.
If humans punched animals in the teeth, these animal fight bites would have high infection
rates also.
37. Name six true hand emergencies.
n
Amputation or other devascularization injury
n
Compartment syndrome
n
Third-degree and circumferential burns
n
High-pressure injection injury
n
Flexor tenosynovitis
n
Septic joint
BIBLIOGRAPHY
1. American Society for Surgery of the Hand: The hand: examination and diagnosis. Blue book, ed 3, New York,
1990, Churchill Livingstone.
2. American Society for Surgery of the Hand: The hand: primary care of common problems. Red book, ed 2,
New York, 1985, Churchill Livingstone.
3. Cambell CS: Gamekeeper’s thumb. J Bone Joint Surg 37B:148–149, 1955.
4. Carter PR: Common hand injuries and infections: a practical approach to early treatment. Philadelphia, 1983,
W.B. Saunders.
5. Christodoulou L, Melikyan EY, Woodbridge S, et al: Functional outcome of high-pressure injection injuries of
the hand. J Trauma 50:717–720, 2001.
6. Daniels JM II, Zook EG, Lynch JM: Hand and wrist injuries. Part II: Emergent evaluation. Am Fam Physician
69:1949–1956, 2004.
7. Kanavel AB: Infection of the hand. Philadelphia, 1925, Lea & Febiger.
8. Lampe EW (with illustrations by F. Netter): Surgical anatomy of the hand. Clin Symp 403, 1988.
9. Perron AD, Miller MD, Brady WJ: Orthopedic pitfalls in the ED: fight bite. Am J Emerg Med 20:114–117, 2002.
