Marshall L. Stoller, Maxwell V. Meng-Urinary Stone Disease
Подождите немного. Документ загружается.


464 Kane
14. Cooper JT, Stack GM, Cooper TP. Intensive medical management of ureteral calculi. Urology
2000; 56: 575.
15. Andersson KE, Forman A, Effects of calcium channel blockers on urinary tract smooth muscle.
Acta Pharmacol Toxicol 1986; 58: 193.
16. Salman S, Castilla C, Vela Navarette R, Action of calcium antagonists on ureteral dynamics. Acta
Urol Esp 1989; 13: 150.
17. Capecchi S, Pignatelli R, Alegiani F, Emergency treatment of ureteral colic with nifedipine.
Minerva Urol Nephrol 1991; 43: 287.
18. Bajor G. Beta-blocking agent facilitating the spontaneous passage of ureteral stones. Int Urol
Nephrol 1990; 22: 33.
19. Muller TF, Naesh O, Svare E, Jensen A, Glyngdal P. Metoclopromide (Primperan) in the treatment
of ureterolithiasis. A Prospective double-blind study of metoclopromide compared with
morphatropin in ureteral colic. Urol Int 1990; 45: 112.
20. Hofstetter AG, Kriegmair M. Treatment of ureteral colic with glycerol trinitrate. Fortschritte
Medizin 1993; 111: 286.
21. Hussain Z, Inman RD, Elves AWS, Shipstone DP, Ghiblawi S, Coppinger SWV. Use of glyceryl
trinitrate patches in patients with ureteral stones: a randomized, double-blind, placebo-controlled
study. Urology 2001; 58: 521.
22. Engelstein D, Kahan E, Servadio C. Rowatinex for the treatment of ureterolithiasis. J Urol (Paris)
1992; 98: 98.
23. Perlow DL. The use of progesterone for ureteral stones: a preliminary report. J Urol 1980; 124:
715.
24. Mikkelsen AL, Meyhoff HH, Lindahl F, Christensen J. The effect of hydroxyprogesterone on
ureteral stones. Int Urol Nephrol 1988; 20: 257.
25. Weiss RM. Physiology and pharmacology of the renal pelvis and ureter. In: Campbell’s Urology,
8th Ed., (Walsh PC, ed.). Saunders, Philadelphia, PA, 2002, pp. 377–409.
26. Lennon GM, Thornhill JA, Grainger R, McDermott TE, Butler MR. Double pigtail ureteric stent
versus percutaneous nephrostomy: effects on stone transit and ureteric motility. Eur Urol 1997;
31: 24.
27. Kaid-Omar Z, Belouatek A, Driouch A, et al. Effects of diuretic therapy on spontaneous expulsion
of urinary calculi, urinary pH, and crystalluria in lithiasic patients. Prog Urol 2001; 11: 450.
28. Holm-Nielsen A, Jorgensen T, Mogensen P, Fogh J. The prognostic value of probe renography in
ureteric stone obstruction. Br J Urol 1981; 53: 504.
29. Irving SO, Calleja R, Lee F, Bullock KN, Wraight P, Doble A. Is the conservative management
of ureteric calculi of >4 mm safe? B J Urol Int 2000; 85: 637–640.
30. Van Savage JG, Palanca LG, Andersen RD, Rao GS, Slaughenhoupt BL. Treatment of distal
ureteral stones in children: similarities to the american urologic association guidelines in adults.
J Urol 2000; 164: 1089.
31. Lotan Y, Gettman MT, Roehrborn CG, Cadeddu JA, Pearle MS. Management of ureteral calculi:
a cost comparison and decision making analysis. J Urol 2002; 167: 1621.
Chapter 25 / Ureteral Stents 465
465
From: Current Clinical Urology, Urinary Stone Disease:
A Practical Guide to Medical and Surgical Management
Edited by: M. L. Stoller and M. V. Meng © Humana Press Inc., Totowa, NJ
25
Ureteral Stents
John S. Lam, MD and Mantu Gupta, MD
CONTENTS
INTRODUCTION
HISTORY OF STENTS
PHYSIOLOGY OF THE STENTED URETER
PROPERTIES OF STENT MATERIALS
BIOMATERIALS
STENT DESIGNS
CLINICAL APPLICATIONS AND OUTCOMES
STENT REMOVAL
COMPLICATIONS
PEARLS/TRICKS
FUTURE DIRECTIONS
SUMMARY
REFERENCES
Key Words: Ureter; stent; obstruction; biomaterial.
INTRODUCTION
Ureteral stents have become an integral part of contemporary urologic practice over
the past 20 yr. They are typically placed to prevent or relieve ureteral obstruction sec-
ondary to a variety of intrinsic or extrinsic etiologies that include obstructing ureteral
calculi, ureteral strictures, congenital anomalies, retroperitoneal tumor or fibrosis,
trauma, or iatrogenic injury. Ureteral stents are also commonly placed to provide urinary
diversion or postoperative drainage, or to help identify and prevent inadvertent injury to
the ureters before surgical procedures.
HISTORY OF STENTS
The concept of stenting the urinary system began as an adjunct to open surgery in
order to facilitate upper tract drainage or align the ureter. Gustav Simon, in the 19th

466 Lam and Gupta
century, performed the first reported case by placing a tube in the ureter while perform-
ing an open cystostomy (1). In the early 1900s, Joaquin Albarrano created the first
catheter intended for use in the ureter (1). Although vulcanization of rubber was first
reported in 1839, early catheters were constructed from fabric coated with varnish (2).
The development of plastics, such as polyethylene and polyvinyl, allowed for stents to
become more rigid and easier to place; however, bladder irritation, infection, and prob-
lems with encrustation and migration still occurred (3,4). In 1952, Tulluch described the
use of polyethylene tubes to help repair ureters and fistulas in patients (5).
In 1967, the era of modern long-term indwelling ureteral stents began when Zimskind
and colleagues reported the use of open-ended silicone tubing as an indwelling stent
that was inserted endoscopically to bypass malignant ureteral obstruction or ure-
terovaginal fistulas (6). Straight silicone stents provided good internal drainage and
developed less encrustation than other compounds; however, they had no distal or
proximal features to prevent migration. Minor improvements followed with Marmar
closing the proximal end of the silicone stent to facilitate passage through severely
obstructed ureters (7) and Orikasa and associates utilizing a “pusher” to hold the stent
in place during wire removal (8).
Gibbons and colleagues made several modifications to prevent stent migration, includ-
ing a distal flange to prevent proximal migration and sharply pointed barbs to prevent
downward migration and expulsion (9). This stent, however, was difficult to pass be-
cause the barbs increased the nominal 7 Fr stent to an actual 11 Fr. Proximal migration
remained a problem, and placement and removal of the stent was difficult. In 1974, the
Gibbons stent became the first commercially available “modern” internal ureteral stent.
Following the Gibbons stent, McCollough (10) and Hepperlen and associates (11)
designed single-pigtail stents that could be straightened and placed over a wire cysto-
scopically to prevent distal, but not proximal, migration. The migration issue was
resolved in 1978 when Finney reported the use of a “double-J” stent containing both
proximal and distal “J” hooks (12), and Hepperlen and Mardis described the use of a
pigtail arterial catheter (13).
Introduction of extracorporeal shockwave lithotripsy (SWL) and developments in
endourologic stone procedures dramatically increased the use of double-pigtail stents.
In the early 1980s, industry and research efforts started to focus on minimizing com-
plications and identifying the “ideal” stent. Development of “firm” stents reduced
migration, but at the expense of a higher incidence of dysuria and loin or flank pain (14).
Surgical errors were also identified as a cause of stent migration (15). Among errors
reported were inadequate stent length, inadequate bladder or renal pelvis curl, proximal
curl remaining in the upper calyx, and inadequate fluoroscopic monitoring. Stents were
also reported to fail in specific types of cases. One series reported a 46% failure rate
at 30 d in patients with extrinsic ureteral obstruction (16). Other studies reported high
failure rates even in routine stent cases (17,18). The importance of properly testing new
materials became evident when polyethylene, a material with attractive biocompati-
bility, was discovered to become brittle and fractured easily with long-term exposure
to urine (19).
The word “stent” is commonly used in genitourinary reconstructive surgery. Two
related definitions of stent are given in most medical dictionaries. First, a stent is a
device used to maintain a bodily orifice, cavity, or contour; second, a stent is a catheter,
rod, or tube within a tubular structure to maintain lumenal patency or protect an
anastomosis or graft (20). Etymologically, the word stent is an eponym related to three

Chapter 25 / Ureteral Stents 467
English dentists named Stent who contributed to improving a substance used for dental
impressions at the end of the 19th century (20). Transition of the dental impression
compound into a urologic tool is attributed to J.F. Esser of Holland during World War
I, as the name became associated with a support for oral skin grafts, which were later
adopted in plastic surgery (21). Urologic stenting first appeared in print beginning in
the 1970s. Willard Goodwin, the originator of many commonly accepted urological
procedures, wrote a brief commentary in 1972 titled, “Splint, Stent, Stint,” conclud-
ing: “Urologists are always talking about putting a tube in a ureter or urethra. When
they do this, it is not a splint. It may be a stent. It probably is never a stint. Perhaps the
process is most properly described as leaving a tube or stent in an organ” (22). The
word “stent” became forged into the urologic literature when Montie, Stewart, and
Levin explicitly defined the term: “When referring to an intraluminal device to main-
tain patency until healing has taken place, the stent is most appropriate” (23).
PHYSIOLOGY OF THE STENTED URETER
In an unstented kidney, vesical pressures are only transmitted to the kidney in the state
of diuresis; however, when the ureter is stented, bladder pressure can be transmitted
back to the kidney (24). Acute ureteral intubation causes an elevation of intrarenal
pressure with a direct correlation to stent diameter, but the intrarenal pressure declines
back to baseline after 3 wk (24,25). This phenomenon is dependent on open tube flow,
where a standing column of urine causes direct transmission of pressure from the blad-
der to the renal pelvis. Increased intrarenal reflux is noted in up to 90% of patients
following stent placement for acute ureteral obstruction (26,27) that declines back to
baseline after 3 wk (25).
Urine flow is both extraluminal and intraluminal in the stented ureter, except in
cases of ureteral obstruction, where flow may be entirely intraluminal (12,28). As stent
diameter increases, intraluminal flow increases (29). Urine flow is multifactorial and
depends on intrarenal pressure, internal stent diameter, stent length, intravesical pres-
sure, and urine density (25,26). Side holes have also been shown to play an important
role. Stents without side holes drained 40–50% less efficiently than the identical stents
with side holes (30). Ureteral stents cause dilation of the ureter and urine flow becomes
more extraluminal despite patency of the stent (29,31). The dilation of the ureter may
be caused by the cytotoxic effect of the foreign body; and/or infection may play a role
(32). Peristalsis is also diminished but usually returns in about 2 mo (33). Stented
ureters demonstrate thickened walls, increased mucus production, and histologic
changes (12).
PROPERTIES OF STENT MATERIALS
The modern day self-retained internal ureteral stent is a synthetic polymeric bioma-
terial device that can be placed by a variety of endourologic techniques, and is designed
to retain its position within the ureter and drain urine between the renal pelvis and
bladder. The urinary system is an unstable chemical environment and supersaturation of
uromucoids and crystalloids at the interface between the material and urine creates a
significant problem for long-term biocompatibility and biodurability of devices within
this system. Mardis reviewed the basic properties of a ureteral stent, and optimization of
these key features is needed to create the ideal stent (34).

468 Lam and Gupta
Elasticity and Memory
Elasticity and memory produces a stent’s ability to maintain position within the
ureter. The memory of polymeric elastomers produces an elastic stent that has coils on
either end that can be straightened for passage over a guidewire. When the guidewire is
removed, the coils reform to its preset configuration to maintain the device in position,
thereby resisting stent migration. This property is a consequence of polymeric cross-
linking, which results from physical or chemical bonding among macromolecular chains.
The strength of this memory is the durometer, which can be varied within the same
material and depends on the type of crosslinking used. As crosslinking increases, the
durometer of the polymer changes from soft to hard.
Tensile Strength and Elongation Capacity
Variations in tensile strength reflect the mechanism of crystallization and crosslinking
in biomaterials. Stents with a higher durometer, or more crosslinks, will have a greater
tensile strength than stents made of the same material, but with a soft durometer. Higher
tensile strength allows for creation of a higher internal to external diameter ratio and
greater number of side-holes for improved drainage. Elongation capacity is the percent
of elongation at stent breakage. Thermoplastic elastomeres, such as polyurethanes and
a variety of other proprietary copolymers, generally have more elongation capacity than
thermoset elastomeres, such as silicone (34).
Biodurability
Biodurability refers to a stent’s ability to exist within the body without the adjacent
system degrading stent structure and function. The urinary tract presents an unstable and
hostile environment to stent function, replete with free radicals, oxidizers, enzymes, and
a supersaturation of urinary mucoids and crystalloids. Stent degradation within the
urinary tract has been reported for polyethylene, polyurethane, and silicone internal
ureteral stents (34). Wide variations occur in the interface reactions between stent
materials and the urinary system. This unpredictability requires that all stents be moni-
tored at frequent intervals for maintenance of structure as well as function.
Biocompatibility
Biocompatibility is the utopian state where a material present within the ureter has no
significant effect on the interface between itself and the urothelium adjacent to it, such
as the ability to resist encrustation and infection. Currently available stents are well
tolerated by the body for short periods; however, no stent is completely biocompatible.
The biocompatibility of a stent may be enhanced with use of hydrophilic polymers that
have low protein absorption and low bacterial adherence (35). In a study of a variety of
stents, polyurethane has been shown to produce more epithelial effects than others
(36,37).
Coefficient of Friction
Coefficient of friction describes how easily a stent is passed or exchanged. All com-
mercial stent biomaterials present some surface friction generally dependent on the
durometer of the biomaterial. A material with a higher durometer lowers the coefficient
of friction, and consequently, soft durometer stents may be difficult to pass. Applying
a hydrophilic coating reduces the surface coefficient of friction.

Chapter 25 / Ureteral Stents 469
Radiopacity
Stents are best placed under fluoroscopic guidance, and radiopacity refers to the ease
of stent visualization during fluoroscopy. All stents are radiopaque; however, some
contain fillers that further enhance radiopacity, which is helpful when there is poor
fluoroscopic equipment or the patient is large.
BIOMATERIALS
The use of biomaterials within the urinary tract dates back to ancient Egypt where
lead and papyrus catheters were used for urinary drainage (38). Ureteral replacement
using glass, tantalum, or vitallium tubes were first described before World War II, but
migration and obstruction limited their success (39,40). In contemporary practice,
devices constructed from synthetic polymeric compounds are the most useful materials
implanted in the urinary tract. The advantages of these materials are that they are
readily available, easily configurable, and have generally acceptable biocompatibility.
Currently, self-retained internal ureteral stents are manufactured from “high poly-
mers.” Polymers are giant molecules of great variety and complexity. A typical poly-
meric chain has tens of thousands of chemical “monomers,” which are linked by
“polymerization.” These chains are organized in various configurations resulting in
complex and versatile macromolecules.
Polyethylene
Polyethylene consists of polyolefin polymers and was the first synthetic polymer em-
ployed
to fashion ureteral stents. It is flexible, odorless, translucent, and nonreactive in
the body. The stiffness of this material made it useful in the management of ureteral
strictures (30,36). On exposure to biological fluids, however, polyethylene was found to
promote protein deposits, leading to an increased likelihood of crystalloid adherence,
encrustation, and infection. Furthermore, long-term exposure of polyethylene to urine
caused it to become brittle, risking fragmentation (19,35).
Silicone
Silicone stents are composed of alternating silicone and oxygen atoms and remains
the gold standard for tissue compatibility owing to its nontoxic, inert nature (35). It is
nonirritating and resistant to encrustation and thus ideal for long-term use. However,
silicone stents migrate easily, have poor mechanical strength, and have a high coefficient
of friction, making these stents difficult to use when negotiating strictures or tortuous
ureters and difficult to pass or remove from the guidewire. Silicone stents have the lowest
internal to external diameter ratio and the smallest side holes of all materials in order to
prevent kinks or collapse.
Polyurethane
Polyurethane, a common generic class of condensation polymers derived from poly-
isocynate and a polyol, has been used in stent construction in an effort to combine the
flexibility of silicone with the stiffness of polyethylene. Although polyurethane is
highly versatile and inexpensive, it has been shown to induce significantly more epi-
thelial ulceration and erosion than other materials (37). Polyurethane also has limited
durability and demonstrates slow in vivo biodegradation. These degradation products

470 Lam and Gupta
may be cytotoxic and as such, polyurethane stents are best employed as short-term
implants (37).
C-Flex
Proprietary modifications to silicone led to the development of C-Flex (Consolidated
Polymer Technologies, Inc., Clearwater, FL), a silicone-modified styrene/ethylene/
butylene block thermoplastic copolymer. The partial silicone composition of C-Flex
makes these stents softer than polyurethane and theoretically less likely to develop
encrustation.
Silitek
Silitek (ACMI Corp., Southborough, MA) is a second-generation, polyester copoly-
mer that followed silicone and polyurethane. Silitek is firm and resists extrinsic com-
pression. It combines strength for placement control with flexibility for patient comfort.
The UroPass, UroPass II, UroPass Obstruction, Single J Urinary Diversion, and pediat-
ric 4.8-Fr stent (all from ACMI) are made of Silitek.
Percuflex
Percuflex (Boston Scientific Corp., Natick, MA) is a proprietary olefinic block co-
polymer developed by Boston Scientific/Microvasive, which becomes soft and flexible
at body temperature. This material has excellent memory and strength, allowing these
stents to be designed with a thinner wall and greater lumen diameter, while allowing for
larger side holes without sacrificing tensile strength. The inert properties of Percuflex
also offer excellent biocompatibility.
Tecoflex
Tecoflex (Thermedics, Inc., Woburn, MA) is a thermosensitive proprietary copoly-
mer. Stents made with it have a smooth surface and a comparatively large inside diameter
(4.5 Fr stent still has a 0.042 internal diameter that accommodates a standard 0.038
guidewire). This material allows for ink labeling instead of laser labeling, which may
theoretically decrease the likelihood of encrustation from the rough surface created by
the laser. The Quadra-Coil Multi-length, Classic Double PigTail, Lubri-Flex, and
LithoStent, all from ACMI, are made of Tecoflex. Dual durometer Tecoflex stents,
which include the Multi-Flex, Sof-Curl, and Double-J II, have a stiffer proximal segment
to aid in accurate placement, while the softer distal segment improves patient comfort.
Other Proprietary Materials
Sof-Flex (Cook Urological Inc., Spencer, IN) is a proprietary compound from Cook
Urological that is used in several of their stents. Other stent materials from Cook include
Endo-Sof and Ultrathane. Pellethane (C.R. Bard, Inc., Covington, GA) is a proprietary
copolymer from Bard, which allows for a variable durometer and is used in their Inlay
stents. This material softens up to 50% when warmed to body temperature. Flexima is
a newer proprietary material from Boston Scientific/Microvasive, designed to resist
buckling during insertion. It is sold as a variable length stent called the Stretch VL from
Boston Scientific/Microvasive. Vertex (Applied Medical Inc., Rancho Santa Margarita,
CA) is a proprietary material from Applied Medical that is used in their ureteral stents.

Chapter 25 / Ureteral Stents 471
Bioabsorbable Materials
Bioabsorbable polymeric materials are designed to retain their tissue-supporting
properties for defined periods of time. After placement, they are gradually biode-
graded into tissue-compatible compounds that are absorbed and replaced by healing
tissue. Biodegradable devices were first developed for urological use in Finland in the
late 1980’s (41). The main benefit of their use is the elimination of a second surgical
intervention for removal. These stents will be most useful for clinical situations
where temporary upper urinary tract drainage is desired, such as following endo-
scopic or open ureteral surgery. Bioabsorbable materials used in urological stents are
high molecular weight polymers of polylactic and polyglycolic acid (41,42). Inves-
tigators have designed short biodegradable stents that expand at body temperature to
hold their position and degrade with time (42,43). These stents do not communicate
with the bladder or kidney and therefore would avoid vesicoureteral reflux and pos-
sibly have a lower infection rate. An alternative strategy is a standard double-pigtail
stent where degradation is controlled by modulating urinary pH to an alkaline level
when the stent is no longer needed (44). Currently, biodegradable stents require
clinical trials in the United States to evaluate concerns of biocompatibility and ade-
quate drainage of urine during stent degradation. Uniform stent degradation is diffi-
cult to achieve and consequently, these stents tend to break off in chunks that are
prone to obstruct the ureter.
Metals
Metallic superalloy titanium and nickel/titanium are materials currently used for
permanently implanted stents, such as the Wallstent (Medinrent, Lausanne, Switzer-
land) or the Memokath 051 (Engineers and Doctors of Copenhagen, Copenhagen, Den-
mark), to relieve conditions such as malignant obstruction and ureteral strictures
(45–47). These stents gradually become covered with urothelium following implan-
tation, thus preventing encrustation and infection. Problems associated with metal
stents include collagenous ingrowth, hyperplastic epithelium, distal ureteral narrowing,
intense fibrosis, and subsequent obstruction (48,49). In an attempt to minimize the
inflammatory process following stent placement and ensure ureteral patency, the use of
stent-associated liposomal formulations of dexamethasone are currently under investi-
gation (50).
Hydrophilic Coatings
Hydophilic coatings consist of nondissolvable polymers that swell on contact with
water and retain a large fraction of water within their polyanionic structure and that
layers on its surface. The surface water of hydrophilic materials not only reduce their
coefficient of friction, improving ease of stent insertion, but also contributes to bio-
compatibility by reducing frictional irritation and cell adhesion at the biomaterial-
urothelial interface (51). This low interfacial tension may explain the ability of hydrogels
to resist protein and crystalloid deposition on their surface (52).
LSe is Cook Urological’s ion implantation process, which attracts specific ions to the
stent surface where they are implanted into the chemical structure. LSe is designed to
reduce the coefficient of friction without presoaking in water and lower the surface
energy of the stent; this is thought to help resist bacterial adhesion and development of
encrustation (53).

472 Lam and Gupta
AQ is a hydrophillic coating made by Cook Urological that can be applied to any
standard or specialty stent to lower the coefficient of friction. Other hydrophilic coatings
include SL-6 by Applied Medical, and Hydro Plus by Boston Scientific/Microvasive.
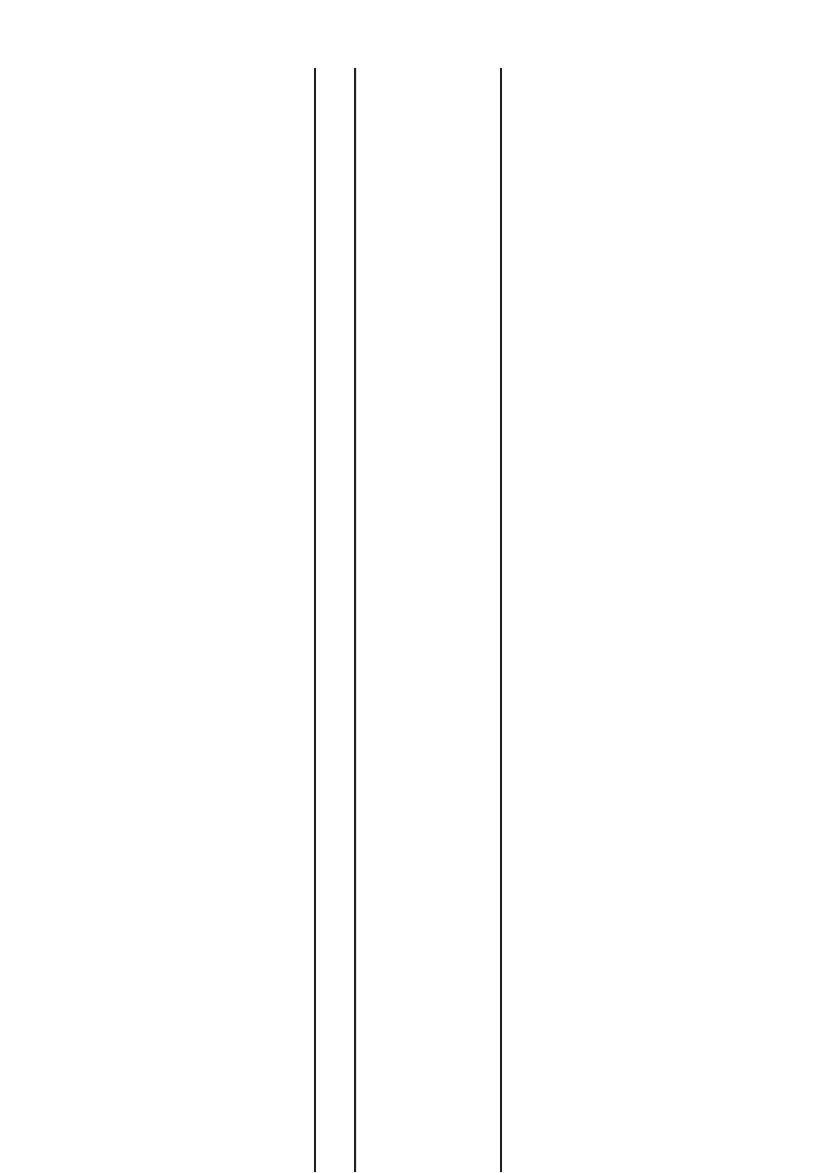
Comparison of Biomaterials
Features of an ideal ureteral stent include: easy maneuverability, radiopacity, ability
to relieve intraluminal and extraluminal obstruction, stability following placement,
biological inertia, chemical stability in urine, resistance to encrustation and infection,
excellent long-term flow, no causation of irritative voiding symptoms, and availability
at an affordable price (53). A comparison of properties among different stent materials
is shown in Table 1. However, no contemporary stent incorporates all of these charac-
teristics and there are too many different designs and biomaterials to attempt direct
comparisons. In addition, the quality of study designs and conflicting results from
many studies prevent supporting or contesting the use of any single design or bioma-
terial. The American Society for Testing and Materials (ASTM) has developed stan-
dards and test protocols for the evaluation of various materials that include polymeric
biomaterials (34). Most current methods of biocompatibility testing include cell cul-
ture techniques and animal models, controlled in vitro encrustation testing, and ad-
vanced microscopic and surface analytical techniques, such as X-ray photoelectron
spectroscopy, atomic force microscopy, scanning electron microscopy, and energy-
dispersive X-ray analysis.
STENT DESIGNS
Indwelling ureteral stents should be able to provide constant, unobstructed drainage
and ensure stability of stent position. Stents with varying sizes, from 4.7 to 18 Fr in outer
diameter, with side draining ports along their entire length have been developed for
maximal urinary drainage. Maintenance of stent position is due to design of the distal
ends as well as proper choice of stent length.
Double-J or Double-Pigtail Stents
These are the most popular ureteral stents. Double-J refers to an open hook configu-
ration at either end of the ureteral stent, whereas a double-pigtail stent has a full retentive
coil at either end. The Double-J stent is the original, silicone, closed-tipped stent to
which ACMI/Surgitek holds the patent and has marketed since 1978 (12). An open-
tipped version is called the Uroguide. All stent manufacturers produce a basic double-
pigtail stent, which have a variety of names, designs, and compositions. Standard
double-pigtail stents must be sized correctly because those that are too long can cause
bladder irritation, whereas those too short can migrate up the ureter. A 24-cm ureteral
stent is well suited for most adults, but should be individualized based on the ureteral
length of the patient.
Multiple-Coil Stents
Multiple-coil stents were designed to meet the “one size fits all” concept, which is
advantageous for the urologist who does not have to worry about choosing the correct
size, and the hospital which does not need to maintain an excessive inventory. Multiple-
coil stents leave redundant length coiled in the bladder coiled so that the trigone is not
irritated.
Chapter 25 / Ureteral Stents 473
Table 1
Comparison of Properties Among Different Stent Materials
Polyethylene Polyurethane C-Flex
®
Silitek
®
Percuflex
®
Silicone
Biocompatibility Low Low Intermediate–High
Intermediate Intermediate–High High
Biodurability Low Intermediate Intermediate Intermediate Intermediate Intermediate
Memory
a
High High High High High Low
Tensile strength
a
High High Intermediate High Intermediate–High Low
Elongation capacity High Intermediate High High High Low
a
Dependent on durometer.
473
