Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

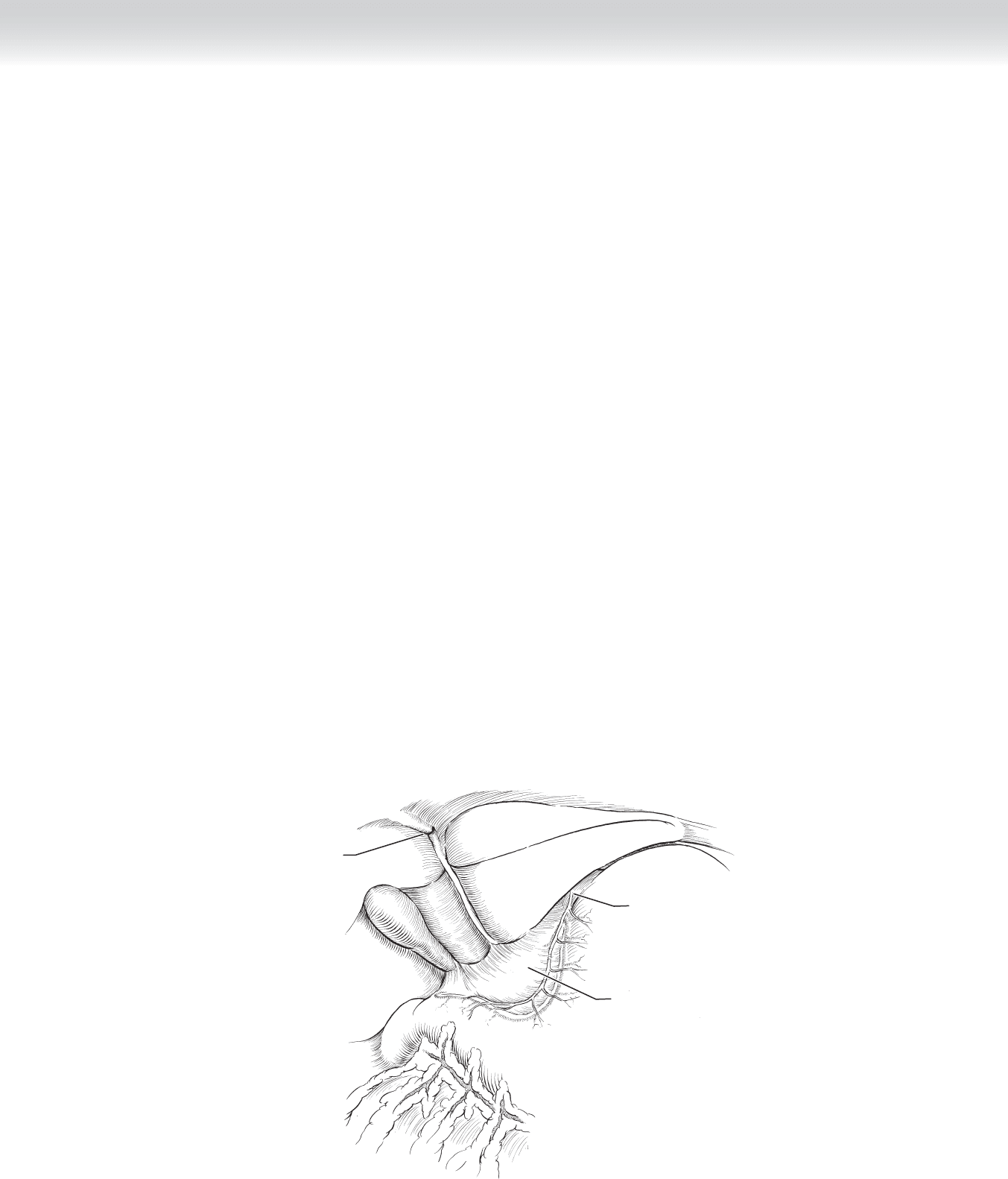
Duodenopyloric junction
Serosal incision
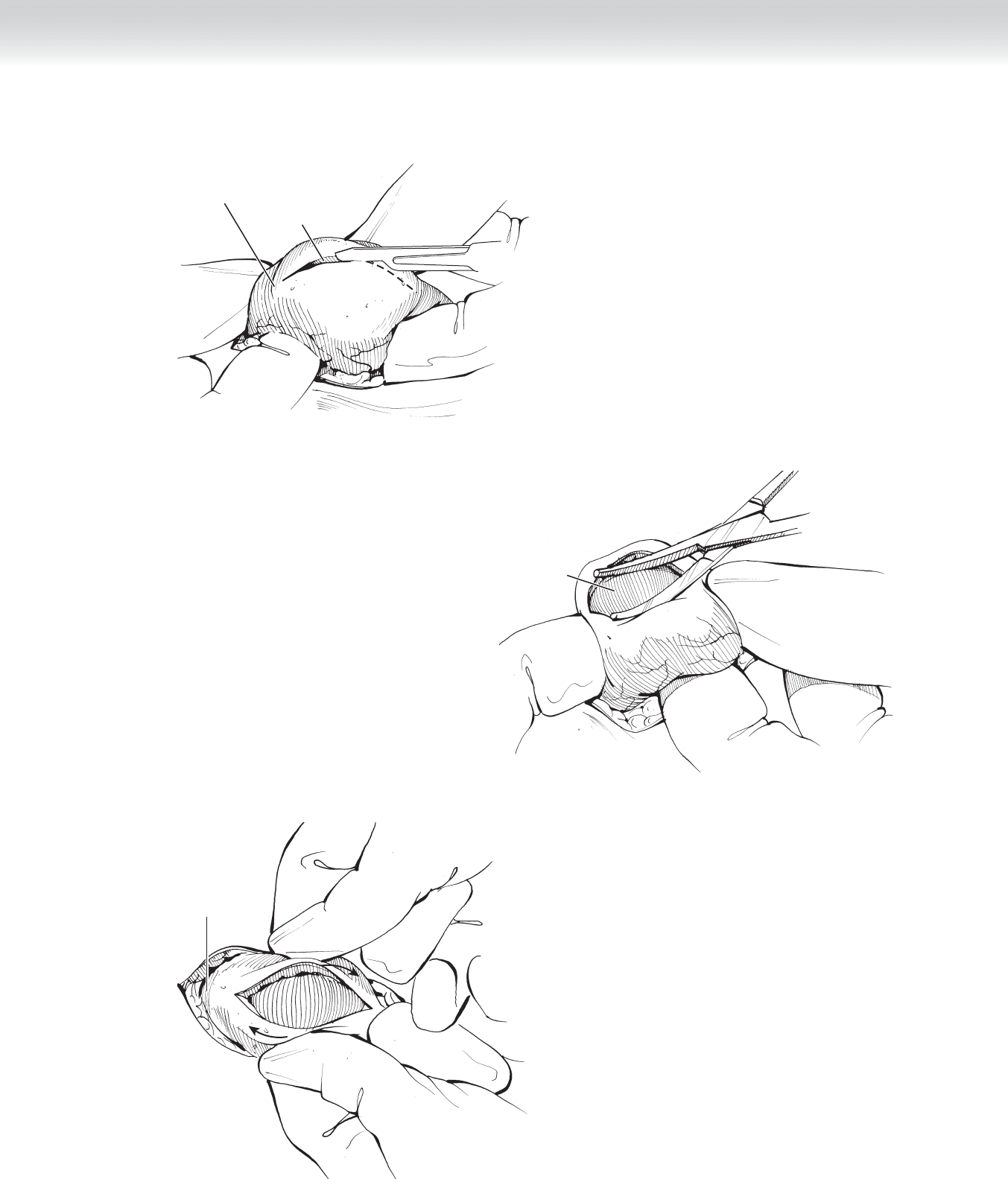
FIGURE 33–3
Mucosal layer of
pyloric channel
FIGURE 33–4
Duodenum
FIGURE 33–5
CHAPTER 33 • Pyloromyotomy 349
350 Section IV • The Abdomen
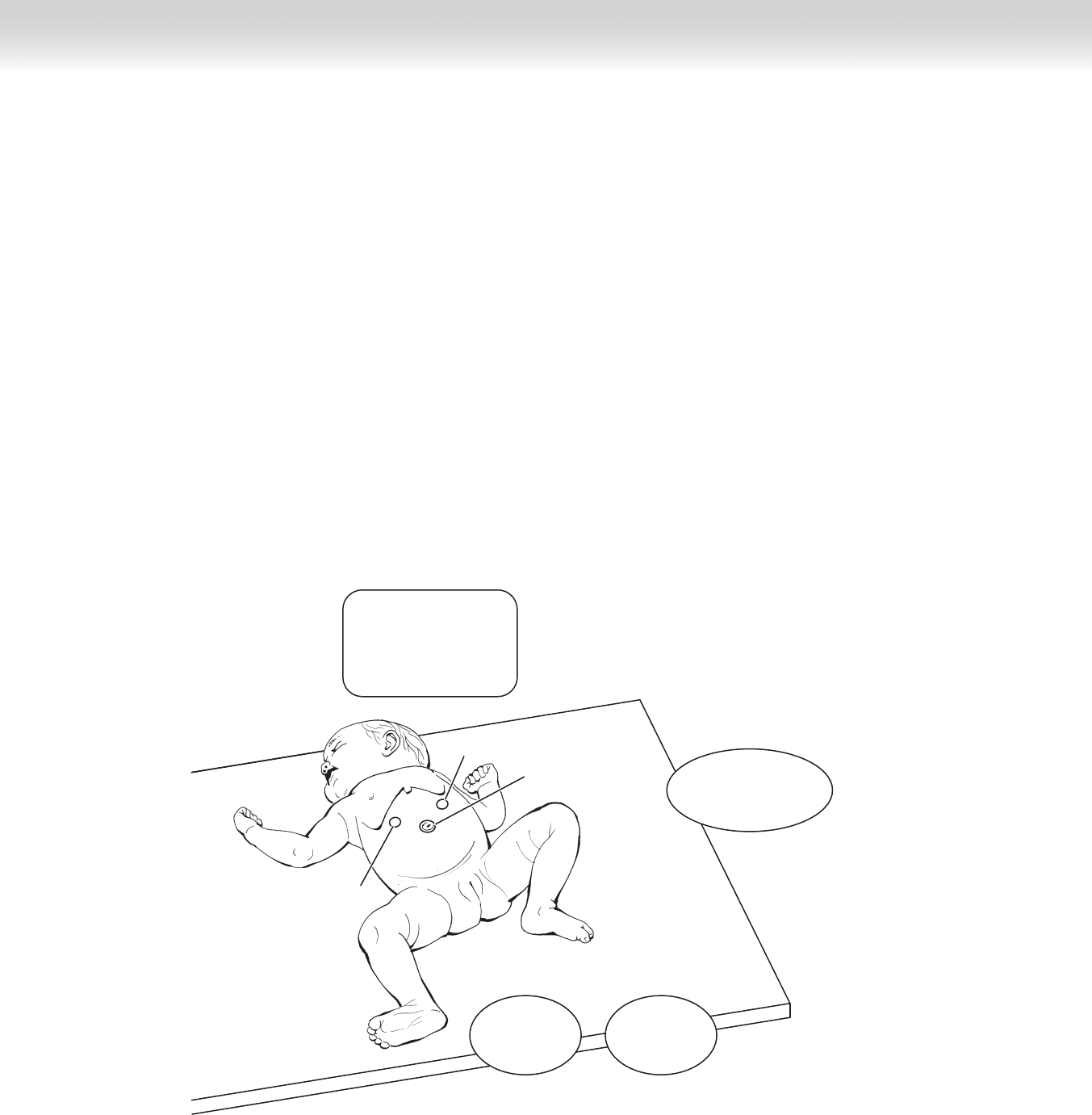
◆ Laparoscopic pyloromyotomy: The patient is placed across the operating table so that sur-
geon and patient are properly aligned. A 3-mm camera port is placed through the umbilicus
with an open technique, and pneumoperitoneum is created to a maximum pressure of
8 mm Hg. A short (22 cm) 3-mm 30-degree telescope is introduced. Two additional 3-mm
ports are placed in the upper quadrants lateral to the rectus muscles (alternatively, the 3-mm
knife and grasper can be placed directly into the abdomen (Figure 33-6). Atraumatic grasp-
ers are used to grasp the duodenum and rotate the pylorus to expose the avascular plane. An
endoscopic pyloromyotomy knife (some surgeons prefer arthroscopy knives) is used to incise
the pyloric serosa over the avascular plane (Figure 33-7). One of the arms of the pyloric
spreader is used to deepen this incision by pushing on the brittle muscle until it gives. This
maneuver is performed in the middle of the incision and never close to the duodenum. The
operation is complete by spreading the muscle until the mucosa prolapses and independent
movement of both pyloric halves can be verifi ed (Figure 33-8). At this time a small amount
of saline is instilled over the pylorus, and the anesthesiologist is asked to insuffl ate the
stomach with air to check for leaks. All incisions are infi ltrated with 0.25% bupivacaine and
closed with 6-0 subcuticular, absorbable sutures or Steri-Strips.
Monitor
Surgeon
Assistant
Anesthesiologist
Grasper
Knife
Camera
FIGURE 33–6
CHAPTER 33 • Pyloromyotomy 351
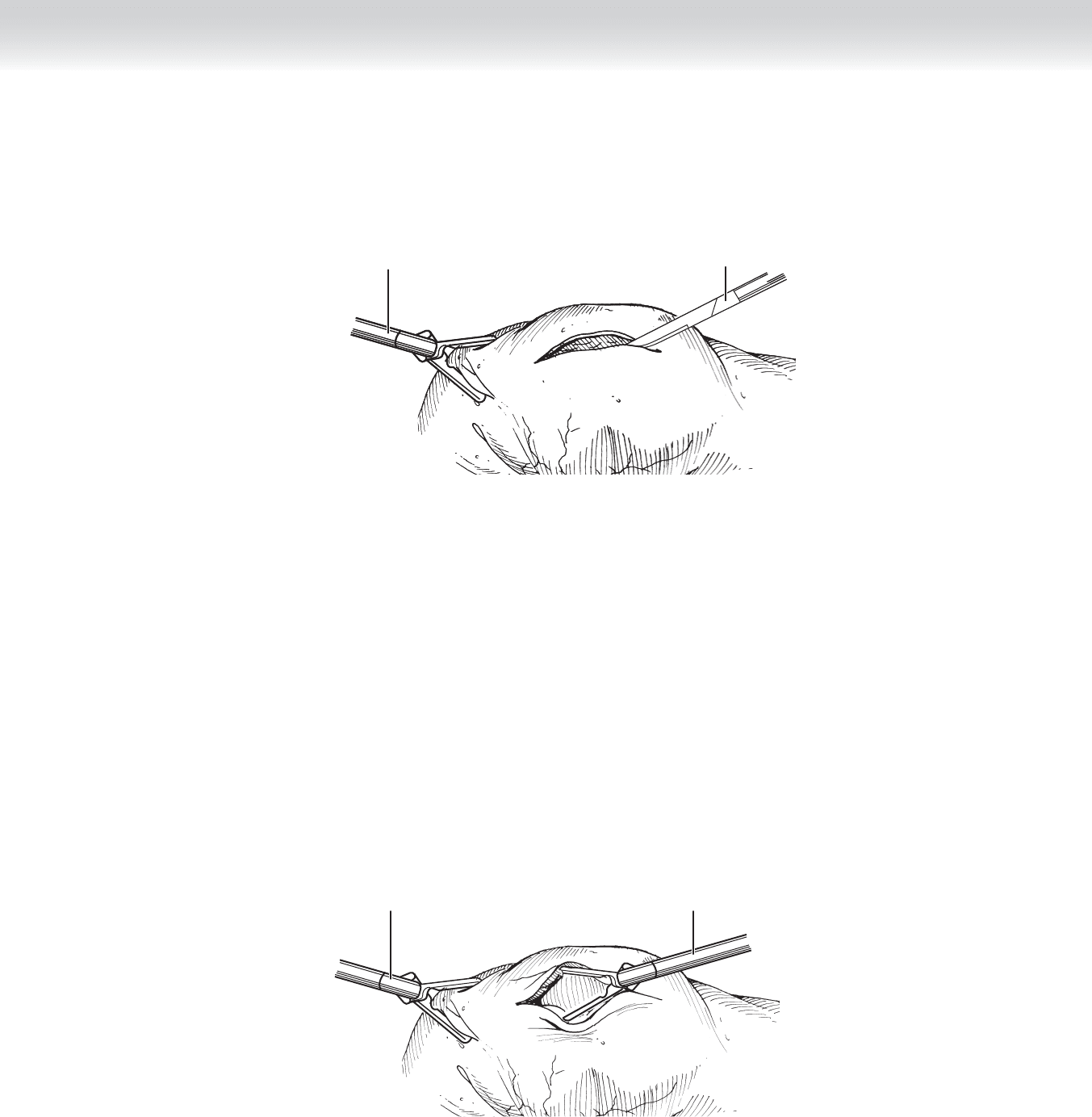
Atraumatic
grasper
Endoscopic pyloromyotomy
knife (or arthroscopy knife)
FIGURE 33–7
Atraumatic
grasper
Endoscopic
pyloric spreader
FIGURE 33–8

352 Section IV • The Abdomen
3. CLOSING
◆ The incision is closed in separate layers with running 5-0 or 6-0 polyglactin sutures. Poste-
rior rectus fascia and peritoneum are closed together; no attempt is made to close the peri-
toneum by itself. The rectus muscle does not need to be reapproximated. After closure of
the anterior rectus fascia, interrupted subcutaneous sutures of 6-0 polyglactin will obliterate
any dead space. The skin is closed with subcuticular 6-0 undyed absorbable monofi lament
sutures and adhesive strips. Before closing, the skin is infi ltrated with 0.25% bupivacaine
without epinephrine at the appropriate dose.
STEP 4: POSTOPERATIVE CARE
◆ Maintenance intravenous fl uids are continued until the patient is tolerating bottle feeds,
which are started 4 to 6 hours after the operation and gradually advanced. It is a good prac-
tice to examine the patient’s abdomen before proceeding with enteral feeds. Many surgeons
use an electrolyte solution such as Pedialyte for the fi rst feed. Some vomiting can be ex-
pected. Most patients are ready for discharge 24 to 48 hours after the procedure.
◆ Complications: The most dreaded complication of this procedure is duodenal perforation,
which is reported in approximately 1% of open pyloromyotomies and between 1% and 2%
of laparoscopic pyloromyotomies. Every effort must be made to identify this complication at
operation, so that the entire pyloromyotomy can be closed with interrupted 4-0 silk sutures
and a new pyloromyotomy performed. The patient is kept on intravenous fl uids, antibiot-
ics, and orogastric suction for 2 to 3 days. A contrast study to confi rm patency of the pylo-
rus and absence of leaks is performed before resuming enteral feeds. Failure to recognize a
perforation results in life-threatening peritonitis and sepsis that mandates immediate resus-
citation, and administration of broad-spectrum intravenous antibiotics, followed by laparot-
omy and washing of the abdominal cavity. The original pyloromyotomy is closed as de-
scribed previously, and a new pyloromyotomy is performed.
◆ Postoperative care is done in a critical care setting, and the need for hemodynamic support
is not unusual. These young patients have an increased incidence of wound infections and
wound dehiscence.
◆ Up to one third of infants after an uncomplicated pyloromyotomy will experience vomiting,
which is typically self-limited. Vomiting is usually managed by holding the next feed and
resuming feeds 6 hours later. If vomiting persists, one must begin to consider the possibility
of an incomplete pyloromyotomy. Although vomiting is not unusual after pyloromyotomy,
abdominal distention is. Abdominal distention should prompt the surgeon to stop feeds and
investigate for duodenal leaks. Wound infections after uncomplicated pyloromyotomy occur
in approximately 2% of cases, and wound dehiscences are quite rare.

STEP 5: PEARLS AND PITFALLS
◆ Avoid incisions that extend into the duodenum. This will surely result in perforation,
because the area of the distal pylorus and proximal duodenum is extremely thin. In fact,
the scoring incision made over the pylorus should stop 2 to 3 mm short of the ring that is
palpated at the distal pylorus. Spreading wide proximal to this area will result in disruption
of the hypertrophic muscle fi bers and release of the constrictive ring.
SELECTED REFERENCES
1. Lobe T, Kumar T: Pyloromyotomy. In Spitz L, Coran AG (eds): Operative Pediatric Surgery, 6th ed.
London, Hodder Arnold, 2006, pp 367-375.
2. Ashcraft K: Atlas of Pediatric Surgery. Philadelphia, Saunders, 1994, pp 85-89.
3. Fujimoto T: Pyloromyotomy. In Najmaldin A, Rothenberg S, Crabbe D, Beasley S (eds): Operative
Endoscopy and Endoscopic Surgery in Infants and Children. New York, Oxford University Press, 2005,
pp 231-234.
CHAPTER 33 • Pyloromyotomy 353

354
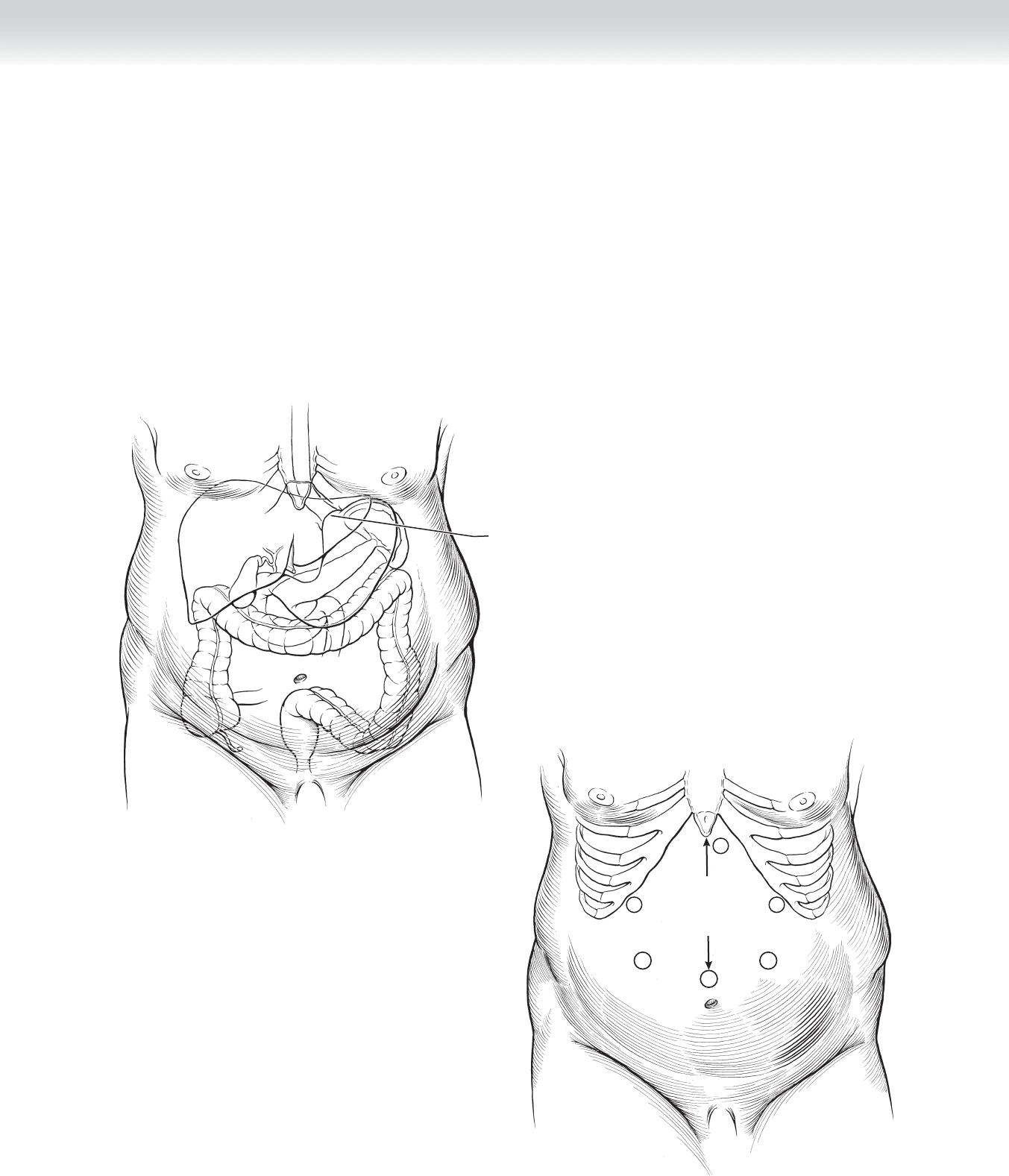
STEP 1: SURGICAL ANATOMY
◆ Experience with the anatomy and surgical procedures of the esophagogastric junction are a
prerequisite to a successful gastric bypass operation (Figure 34-1).
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ The standard indications for a bariatric operation include either a body mass index of at
least 40 kg/m
2
or a body mass index of at least 35 kg/m
2
with signifi cant associated medical
illness. Potential patients must also have tried multiple dietary, activity, and lifestyle modifi -
cation programs. They should be free of substance abuse and psychologically stable so that
they can make an intelligent decision regarding the risks of the operation and the need to
dramatically alter their lifestyles.
◆ Bariatric operations should not be offered unless a dedicated team is in place for the thorough
preoperative evaluation and close long-term follow-up that are required for every patient.
◆ Patients should receive prophylaxis against wound infection with an intravenous cephalo-
sporin and against venous thrombosis with sequential compression devices and low-
molecular-weight heparin before induction of anesthesia.
◆ General anesthesia is required for this operation. An anesthesia team specially trained and
equipped for the morbidly obese patient is necessary.
◆ Obtaining a controlled airway can sometimes be quite challenging in the morbidly obese patient.
A fi ber-optic scope can be very helpful for an awake intubation. Elective tracheostomy is some-
times a good idea for the massively obese patient, especially one who already has some baseline
respiratory dysfunction where airway control may continue to be a problem postoperatively.
◆ Each incision site is preemptively anesthetized with local anesthetic injection.
CHAPTER
34
Roux-en-Y Gastric Bypass
(Open and Laparoscopic)
Michael D. Trahan
CHAPTER 34 • Roux-en-Y Gastric Bypass (Open and Laparoscopic)
355
STEP 3: OPERATIVE STEPS
LAPAROSCOPIC
1. INCISIONS
◆ Six small incisions are used for the laparoscopic approach. The incision for the left-sided 12-mm
trocar needs to be approximately 3 cm to later accommodate the circular stapler (Figure 34-2).
Esophagogastric junction
/
esophageal hiatus
MC
FIGURE 34–1
15 - 20 cm
12
12
12
5
5
5
FIGURE 34–2
356 Section IV • The Abdomen
2. DISSECTION
◆ The 12-mm camera port is placed 15 to 17 cm from the xiphoid process in the midline. A
port with internal visual capability is preferred. The umbilicus is not a useful landmark in
the morbidly obese patient. The peritoneal cavity is infl ated with carbon dioxide to 13 to
15 mm Hg.
◆ The remaining four ports (one 5 mm and one 12 mm in each of the upper abdominal
quadrants as diagrammed) are then placed with internal visualization.
◆ A suture looped under the falciform ligament can often improve visualization and reduce
interference with instrument introduction (Figure 34-3).
◆ The omentum is divided in the midline all the way to and for a short distance along the
transverse colon using the ultrasonic shears. This will allow placement of the Roux limb
anterior to the colon and stomach with less tension. Adhesions to the abdominal wall may
need to be divided fi rst (Figure 34-4).
◆ The omentum is placed above the transverse colon, which is then retracted superiorly by
the assistant’s grasping of the transverse mesocolon (Figure 34-5).
Sutured loop
under falciform
ligament
Hepatogastric
ligament
Anterior
vagus nerve
FIGURE 34–3
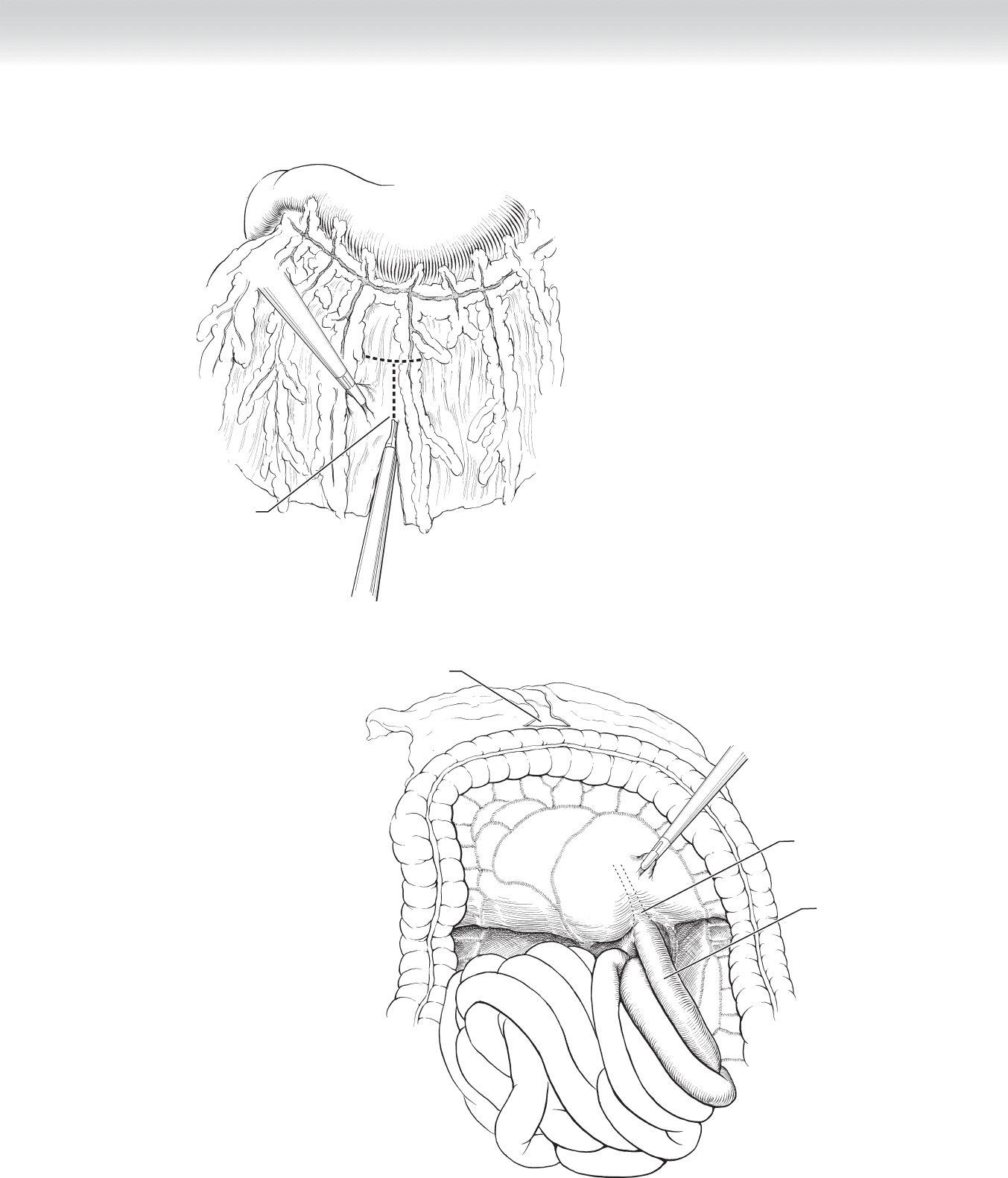
Creating omental window
FIGURE 34–4
Jejunum
Ligament of Treitz
Omental window
FIGURE 34–5
CHAPTER 34 • Roux-en-Y Gastric Bypass (Open and Laparoscopic)
357
358 Section IV • The Abdomen
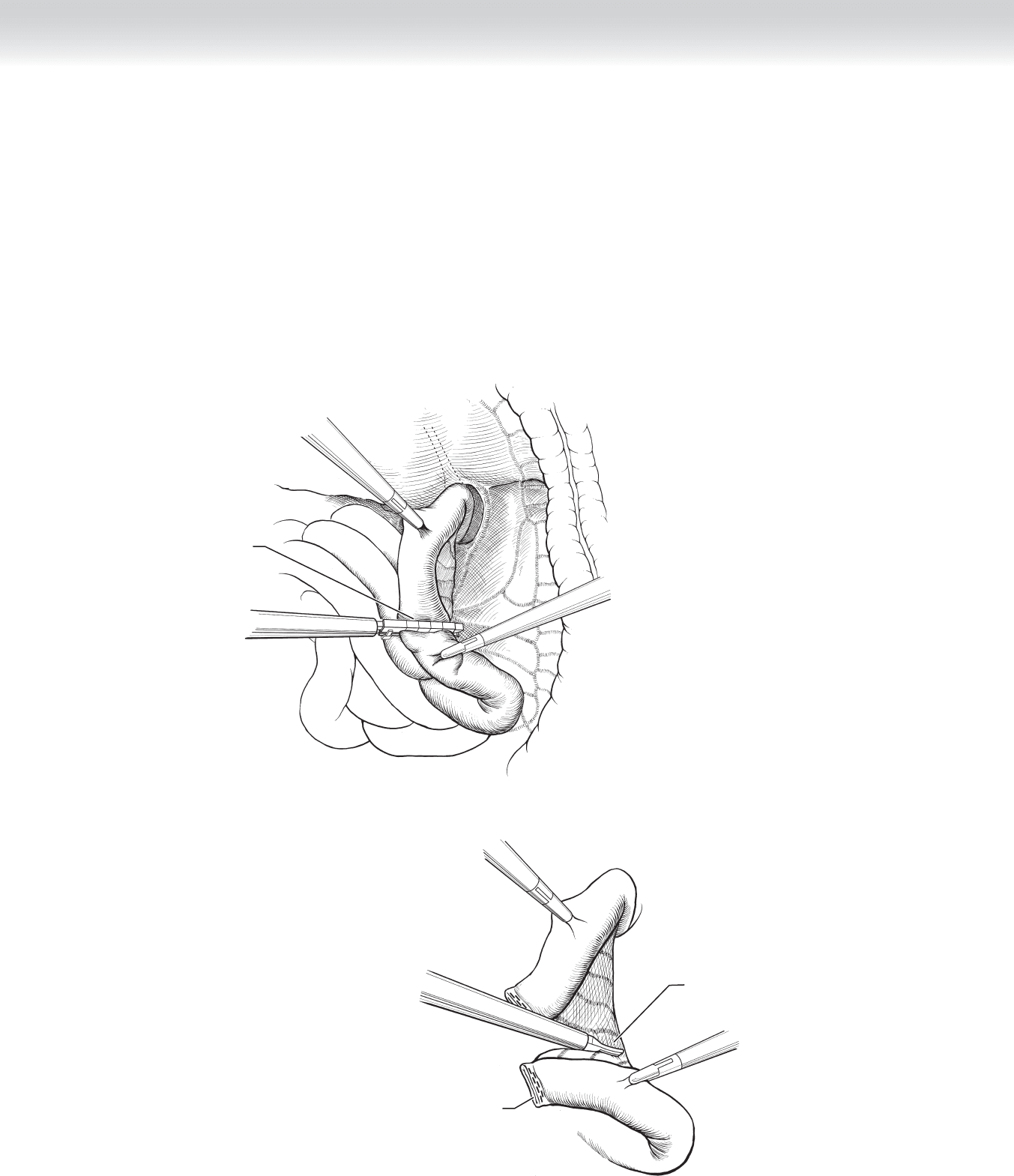
◆ The ligament of Treitz is identifi ed and followed until the mesentery lengthens (usually
30 to 40 cm). The jejunum is divided transversely with a linear cutting stapler loaded with
2.5-mm staples. A 45-mm stapler length is adequate (Figure 34-6).
◆ The mesentery of the distal aspect of the divided jejunum is incised next to the bowel wall
to provide additional mobility of the Roux limb. Any ischemic area created by this maneu-
ver will be trimmed during one of the fi nal steps (Figure 34-7).
Dividing jejunum
approximately 30 cm
distal to ligament of Treitz
FIGURE 34–6
Incising mesentery
several cm along Roux limb
Roux limb
of jejunum
FIGURE 34–7
