Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

CHAPTER 57 • Stoma Takedown: Takedown of Loop Colostomy or Ileostomy 647
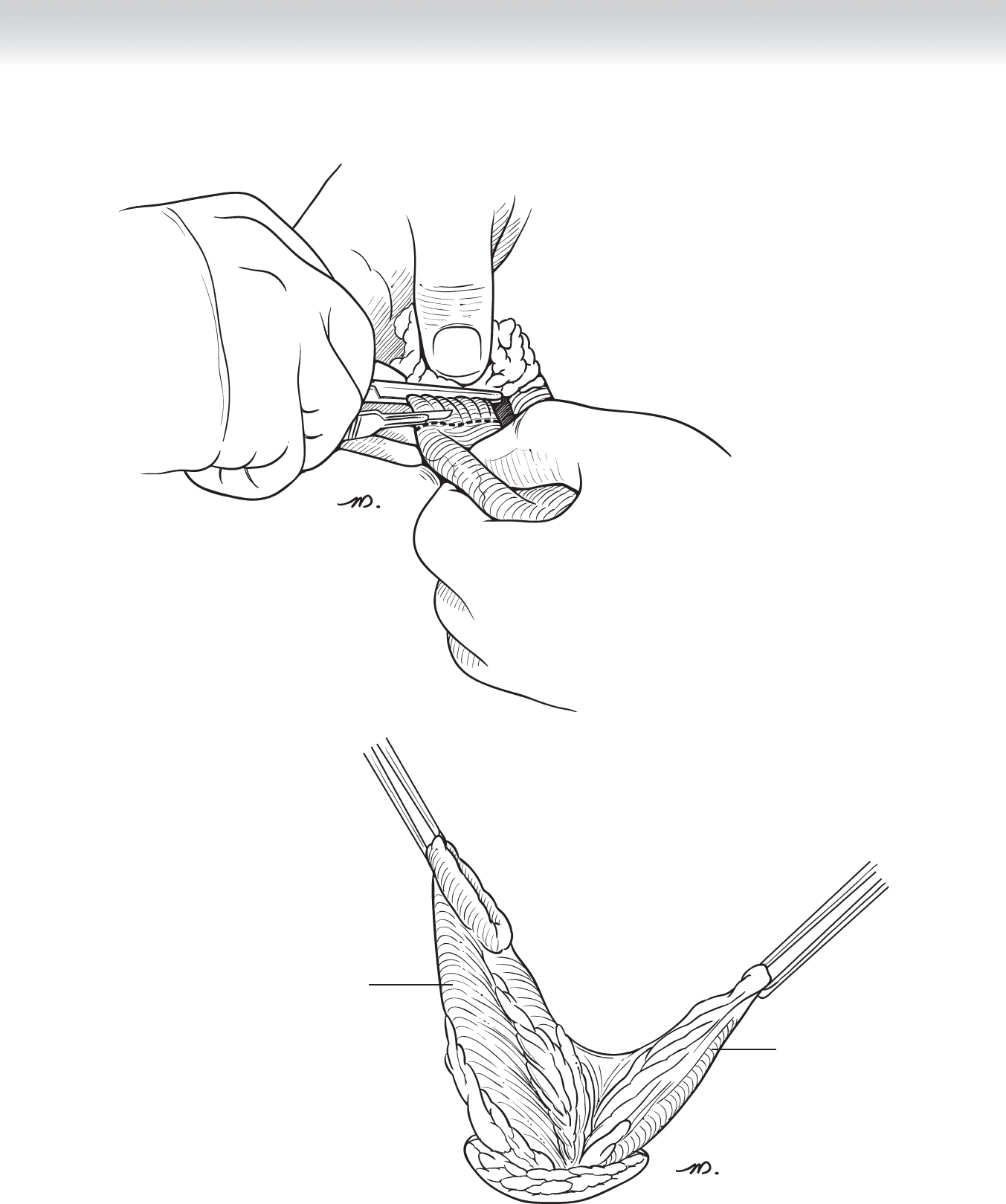
FIGURE 57 –8
Distal bowel
Proximal
bowel
FIGURE 57 –9
648 Section IX • Colon
◆ The antimesenteric and mesenteric borders of each lumen are lined up.
◆ A double-armed 4-0 Maxon monofi lament suture is used to create a single-layered running
anastomosis (Figure 57-10). The serosal edge is grasped and the mucosa and submucosal
edges are reapproximated. This is done by placing the knot on the outer portion of the
bowel at the antimesenteric border. One arm of suture is passed under the knot and used to
complete half of the anastomosis, as is the other arm on the other side. The suture line is
inspected for integrity.
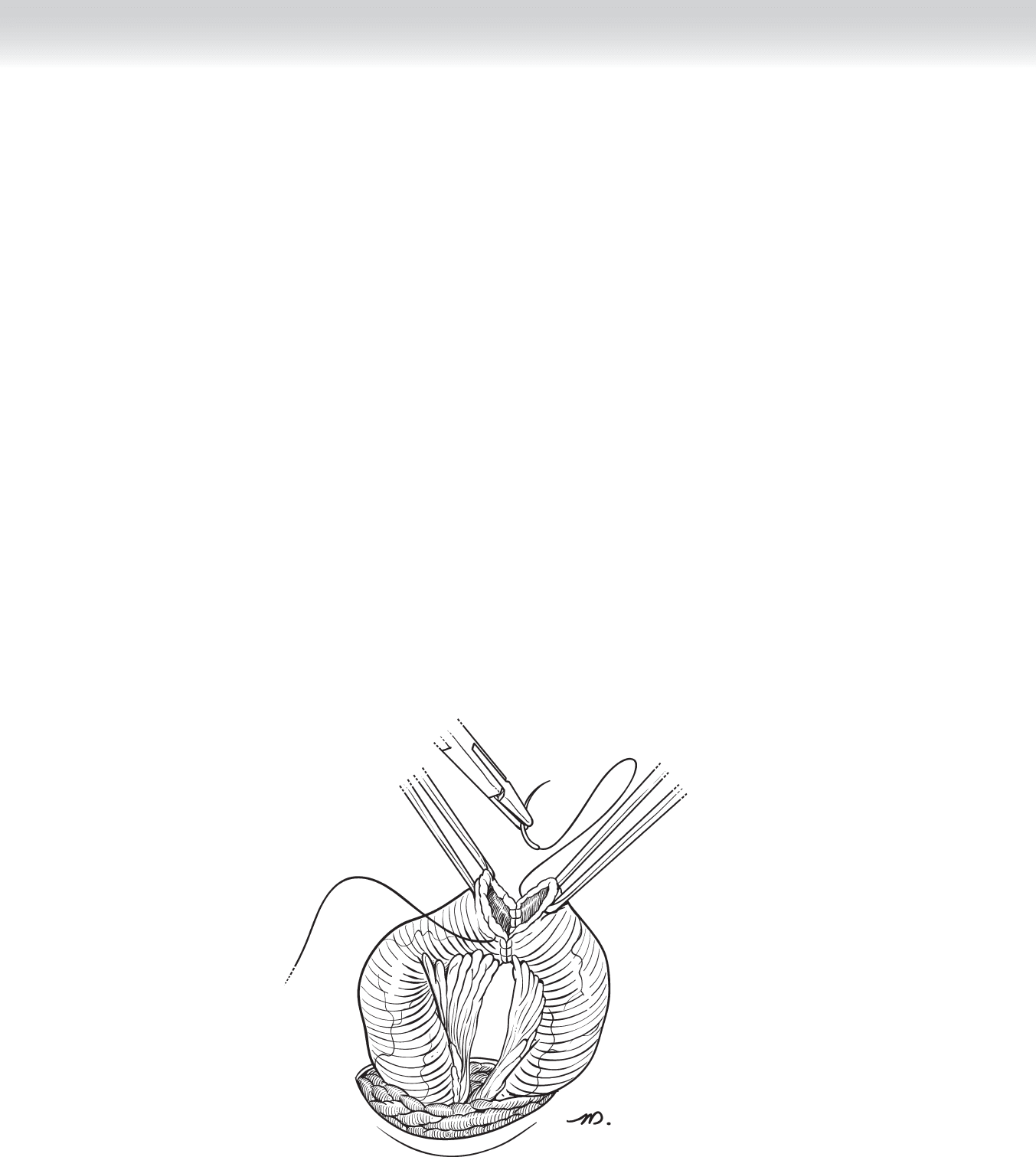
◆ The completed anastomosis is dropped back into the abdominal cavity (Figure 57-11).
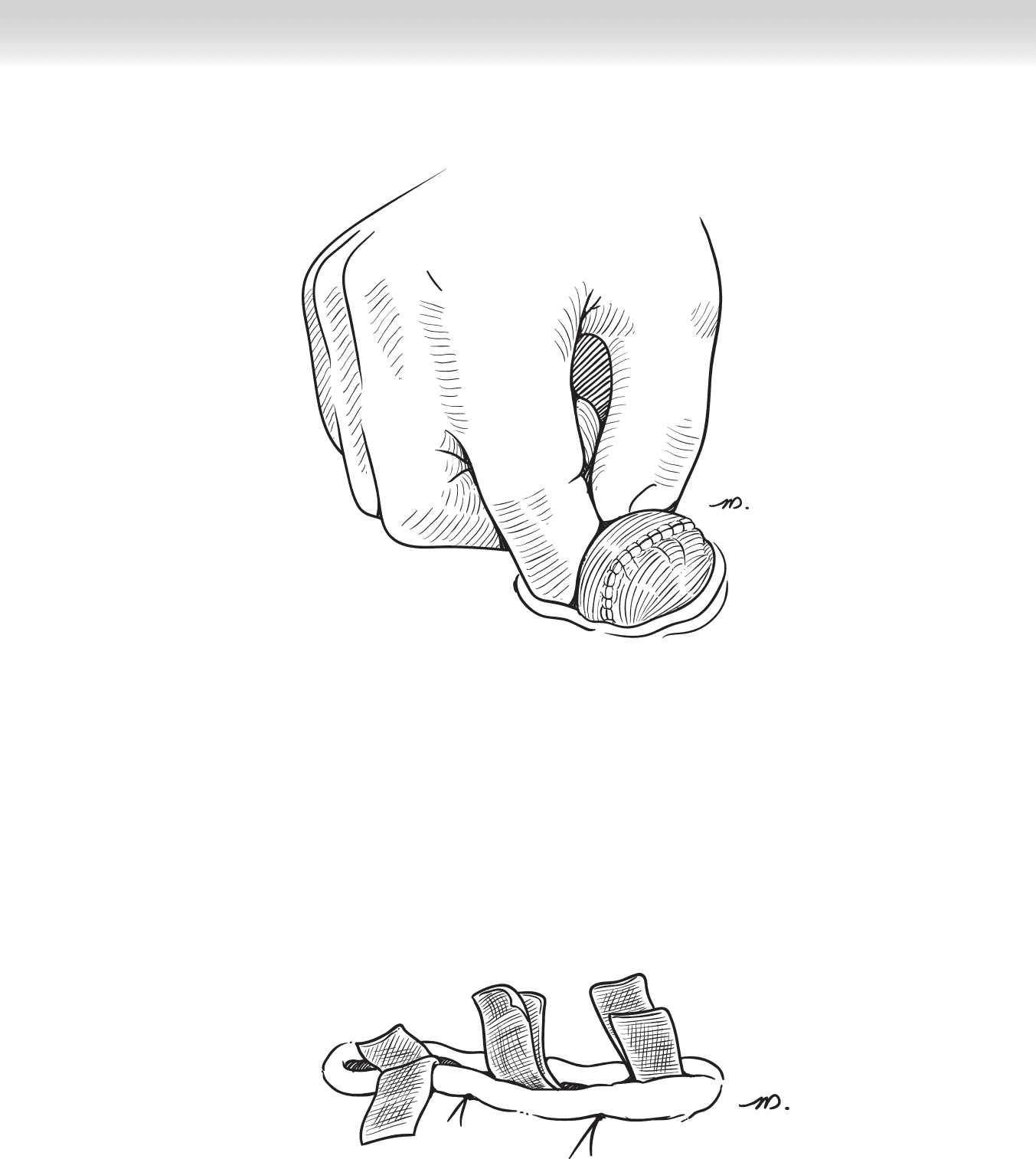
◆ Surgical gloves are changed and the anterior rectus fascia is reapproximated using 0
polydioxanone (PDS) in fi gure-of-eight interrupted sutures.
◆ The subcutaneous skin is irrigated with bacitracin antibiotic.
◆ A nylon vertical mattress suture is used to loosely close the skin, followed by placement of
Telfa wicks between each suture (Figure 57-12). A dry dressing is placed over the wicks
and changed as needed. The wicks, however, are not removed until the patient leaves the
hospital.
FIGURE 57 –10
CHAPTER 57 • Stoma Takedown: Takedown of Loop Colostomy or Ileostomy 649
FIGURE 57 –11
FIGURE 57 –12

650 Section IX • Colon
STEP 4: POSTOPERATIVE CARE
◆ Adherence to a postoperative colorectal clinical pathway ensures standardization of care.
◆ Nasogastric decompression is not necessary unless vomiting and postoperative ileus or
obstruction occurs.
◆ Adequate pain control is achieved using patient-controlled algesia.
◆ Stress ulcer prophylaxis, such as famotidine (Pepcid) 20 mg IV every 12 hours, should be
used in patients with prior peptic ulcer disease (PUD), gastroesophageal refl ux disease
(GERD), or symptoms to suggest disease.
◆ All patients should receive prophylaxis for deep venous thrombosis (DVT), using sequential
compression devices while in bed and heparin 5000 U subcutaneously every 8 hours or
enoxaparin 40 mg subcutaneously every morning. Dosing schedules according to PQRI
quality measures may begin preoperatively, or, as we practice, within 24 hours from the
operation after morning laboratory test results are back, to ensure there is no signifi cant
drop in hemoglobin level to suggest postoperative bleeding.
◆ Adequate intravenous fl uid should be administered with monitoring of urine output via
urimeter on the Foley bag. The Foley catheter may be removed on postoperative day 1.
◆ The diet may be limited to ice chips and sips of water in the postanesthesia care unit and
on postoperative day 1. Return of bowel function is measured by the frequency and pitch of
bowel sounds, lack of abdominal distention, and the patient’s subjective will to eat. A clear
liquid diet may be offered as sips of clear liquids without carbonation and without a straw
to minimize buildup of air in the intestine. This may be advanced ad lib as bowel function
returns.
◆ Early ambulation is crucial for aid in return of bowel function. Patients should be instructed
to walk multiple times a day beginning on postoperative day 1.
◆ The incision site should be checked on postoperative day 1 and daily thereafter to ensure
absence of infection. Wicks should be removed before the patient leaves the hospital.

CHAPTER 57 • Stoma Takedown: Takedown of Loop Colostomy or Ileostomy 651
STEP 5: PEARLS AND PITFALLS
◆ Soft tissue infection can occur to varying degrees, with necrotizing fasciitis as the worst case
scenario. The ostomy site should be loosely closed and meticulous attention paid to the
appearance of the wound postoperatively. In addition, anastomotic leak may present in part
as a soft tissue infection.
◆ Wrapping a temporary ileostomy or colostomy with Seprafi lm allows for easier takedown
later. This consideration should be made during the initial surgery.
SELECTED REFERENCES
1. Zeng Q, Yu Z, You J, Zhang Q: Effi cacy and safety of Seprafi lm for preventing postoperative abdominal
adhesion: Systematic review and meta-analysis. World J Surg 2007;31:2125-2131;2132 [discussion].
2. QualityNet: Site index. Available at www.qualitynet.org.
3. Itani KM, Wilson SE, Awad SS, et al: Ertapenem versus cefotetan prophylaxis in elective colorectal surgery.
N Engl J Med 2006;355:2640-2651.
4. Beck DE, Opelka FG: Perioperative steroid use in colorectal patients: Results of a survey. Dis Colon
Rectum 1996;39:995-999.
5. Law WL, Bailey HR, Max E, et al: Single-layer continuous colon and rectal anastomosis using monofi la-
ment absorbable suture (Maxon): Study of 500 cases. Dis Colon Rectum 1999;42:736-740.
652
STEP 1: SURGICAL ANATOMY
◆ The right colon begins at the ileocecal valve, includes the right (ascending colon) hepatic
fl exure, and ends at the mid-transverse colon; the appendix is present at the inferior aspect
of the cecum. The blood supply to this area comes from the superior mesenteric artery
through its ileocolic, right colic, and right branches of the middle colic arteries. The lym-
phatics to the right colon follow its arterial blood supply. A minimum of 12 lymph nodes
within the mesentery is considered an adequate resection when performing a right hemico-
lectomy for cancer.
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ Indications: Colon resection is performed for benign diseases, such as diverticulitis, isch-
emic colitis, volvulus, polyposis, bleeding from arteriovenous malformation, trauma,
infl ammatory bowel disease, and curative treatment or palliation of malignant tumors of the
colon and rectum. The extent of resection is based on the vascular supply of the specifi c lo-
cation of the tumor. Tumors at the hepatic fl exure or on the proximal transverse colon can
be resected with an extended right hemicolectomy, which involves additionally taking the
blood supply and transverse colon to the left of the middle colic artery.
◆ Preoperative planning: In clinical practice throughout North America, an adequate mechan-
ical bowel preparation is generally considered desirable the day before surgical resection.
Preoperatively, intravenous antibiotics must be administered before the skin incision. A pre-
operative dose of subcutaneous heparin (5000 U) or a low-molecular-weight heparin is rec-
ommended to prevent deep venous thrombosis. Before induction of general anesthesia,
pneumatic compression boots are placed on both lower extremities and continued postop-
eratively until the patient ambulates on the fi rst postoperative day.
◆ Anesthesia: General anesthesia is used.
CHAPTER
58
Right Hemicolectomy
Celia Chao
CHAPTER 58 • Right Hemicolectomy 653
STEP 3: OPERATIVE STEPS
1. INCISION
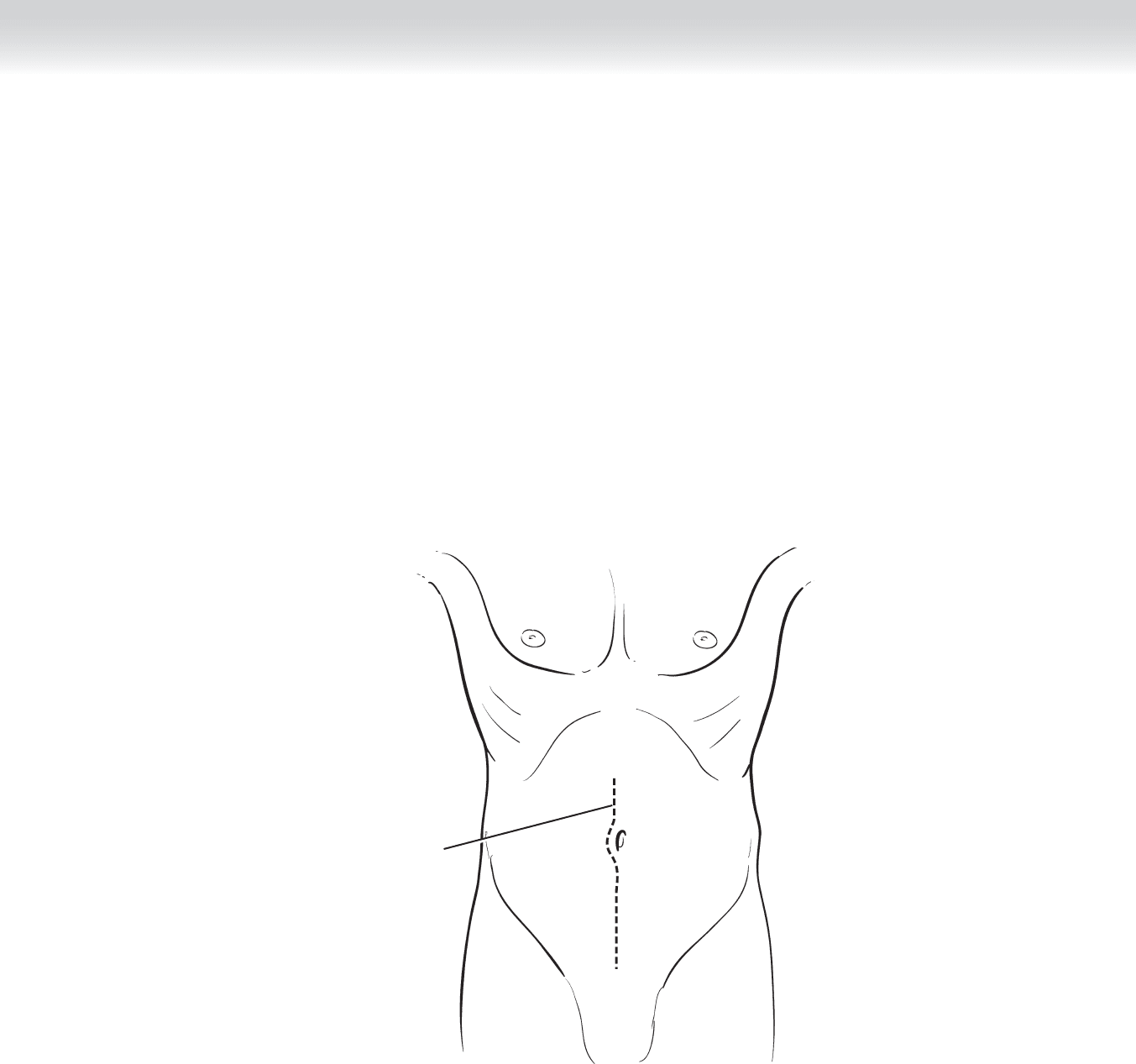
◆ A midline incision (Figure 58-1) is made, and a Thompson retractor is placed to retract the
anterior abdominal wall and increase exposure in the region of the right colon.
Incision
FIGURE 58 –1
654 Section IX • Colon
2. DISSECTION
◆ A standard exploration of the intra-abdominal cavity is performed to determine the extent
of disease and resectability. The peritoneal surface, liver, porta hepatis, mesenteric nodes,
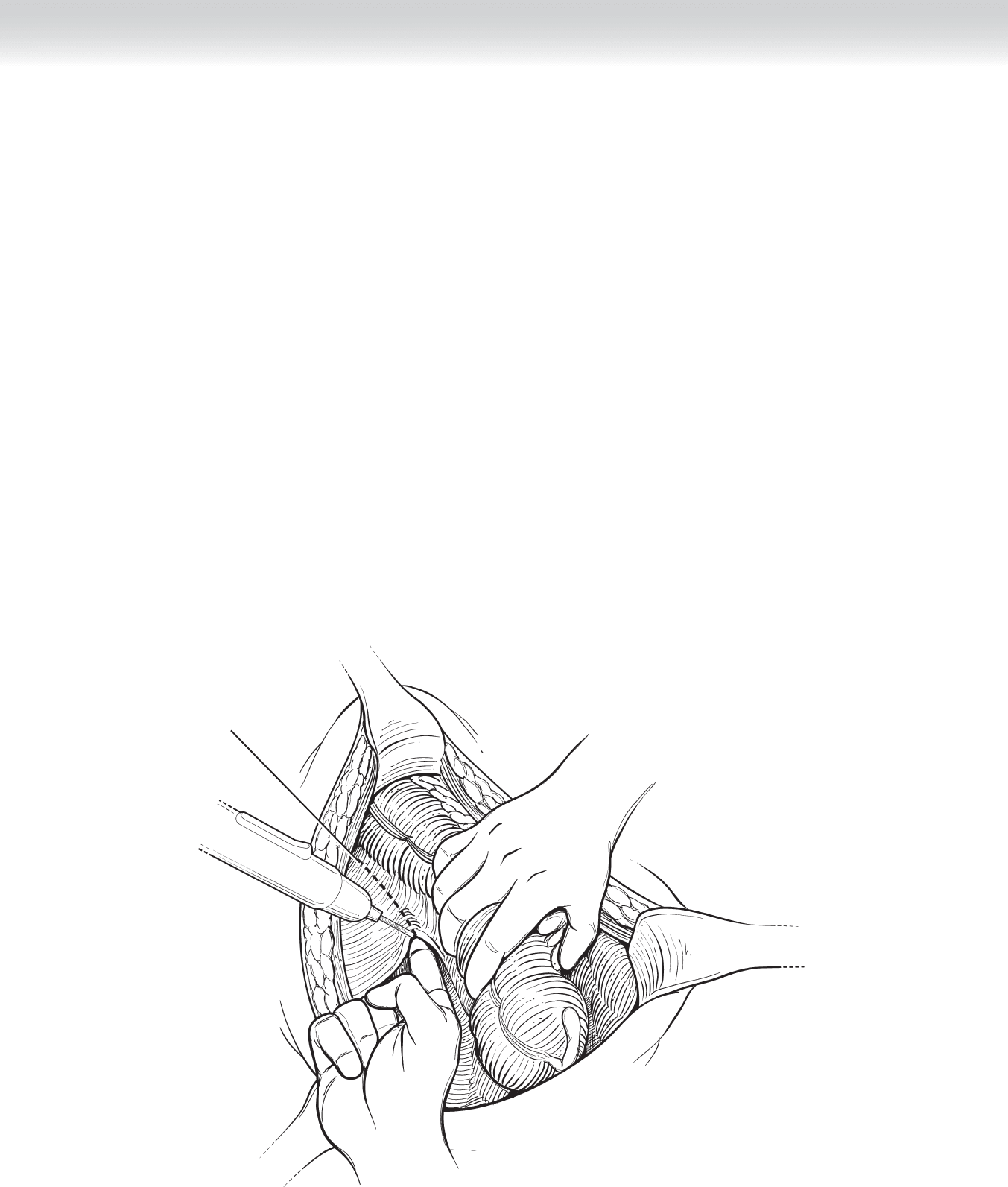
and ovaries are examined. The right colon is mobilized from its retroperitoneal attachments
by incising the white line of Toldt (Figure 58-2).
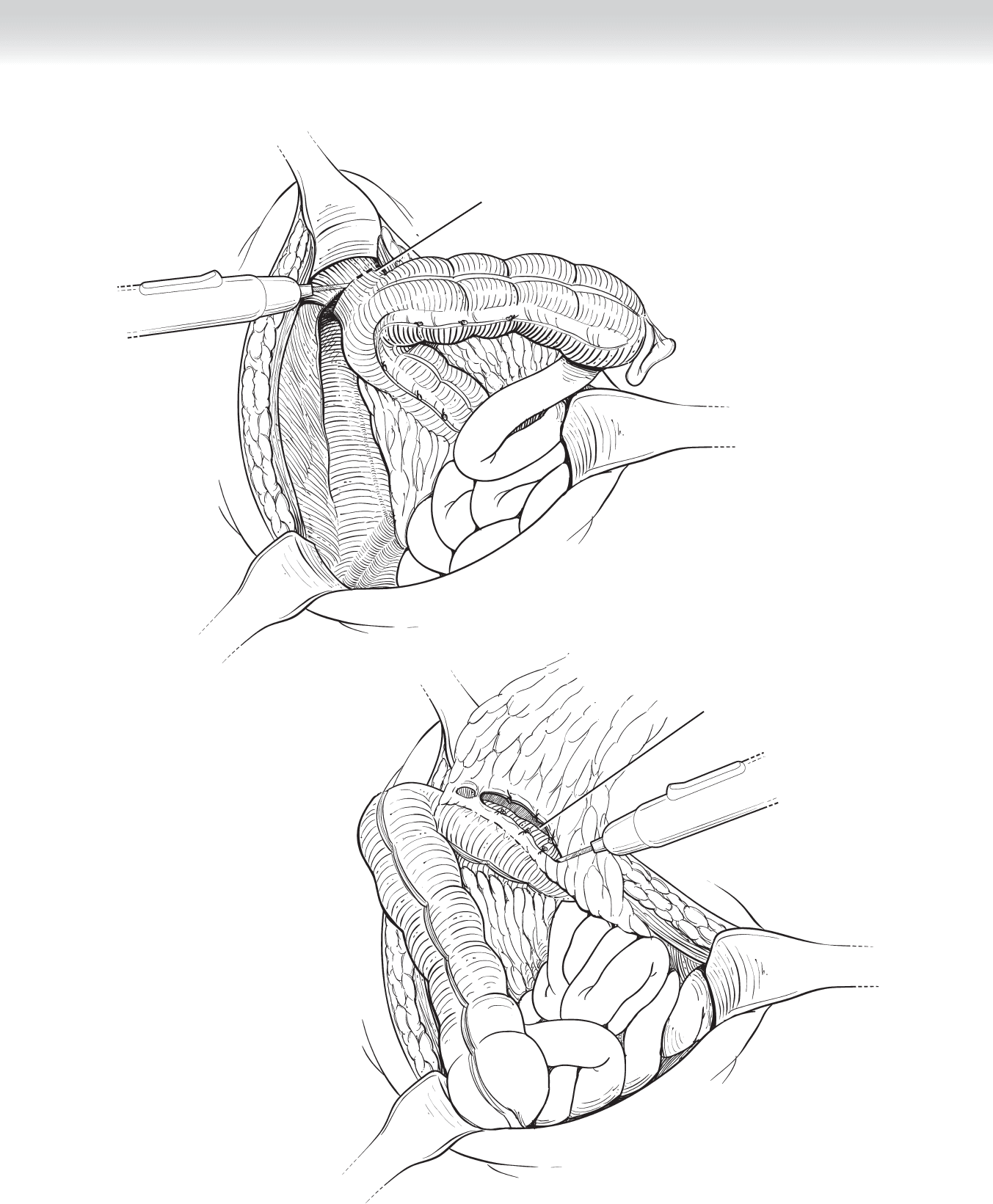
◆ The cecum and ascending colon are retracted medially, exposing the right ureter and gonadal
vessels. Continuing superiorly along this retroperitoneal plane, the hepatocolic ligament is
divided to release the hepatic fl exure (Figure 58-3).
◆ Posteriorly, the duodenum is identifi ed and separated from the colon. The omentum is mo-
bilized off the transverse colon by dissecting along an avascular plane (Figure 58-4).
Incision of white
line of Toldt
FIGURE 58 –2
CHAPTER 58 • Right Hemicolectomy 655
Division of hepatocolic
ligament
FIGURE 58 –3
Dissection of omentum
from transverse colon
FIGURE 58 –4
656 Section IX • Colon
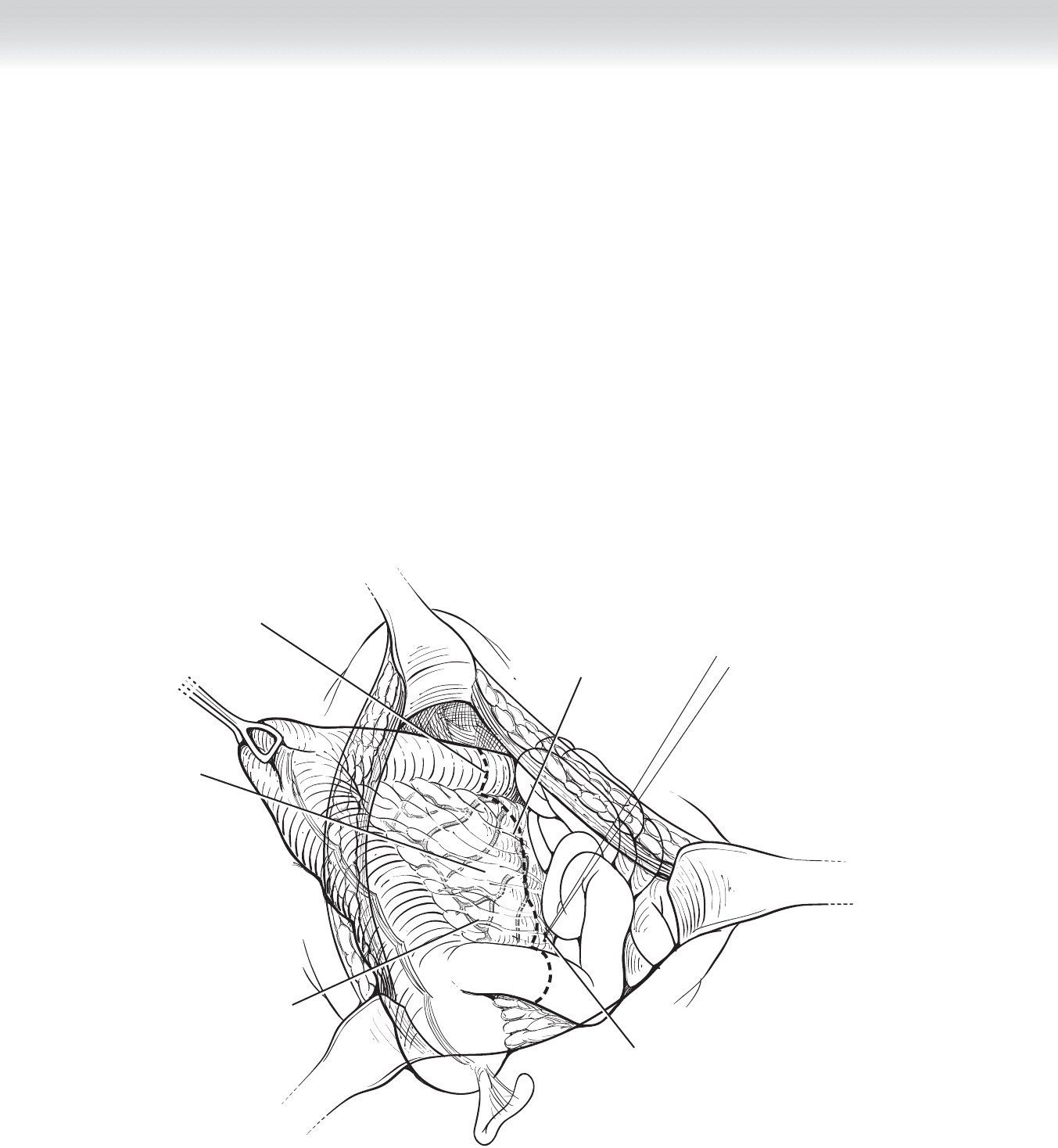
◆ If the omentum is adherent or close to the tumor, that portion of the omentum can be re-
moved en bloc with the resected colon. The points of transection of the terminal ileum and
transverse colon are decided based on the mesenteric blood supply (Figure 58-5).
◆ Using a gastrointestinal anastomosis (GIA) stapler, transect the terminal ileum 10 to 15 cm
from the ileocecal valve for lesions involving the cecum and approximately 5 cm for lesions
distal to the cecum (Figure 58-6).
◆ The transverse colon is divided in similar fashion with the GIA stapler just to the right of
the middle colic artery. The peritoneum to the mesentery is scored with electrocautery; the
vessels, and not the surrounding fatty tissue, can be more easily clamped and tied. The
mesentery corresponding to the points of resection are divided to the origins of the ileocolic
and right colic arteries to ensure adequate removal of the node-bearing tissue in the mesen-
tery.
Middle colic
vessels
Ileocolic
vessels
Right colic
vessels
Line of transection
Ligation of distal
ileomesenteric vascular
arcade
FIGURE 58 –5
