Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.


CHAPTER 89 • Mesenteric Ischemia 971
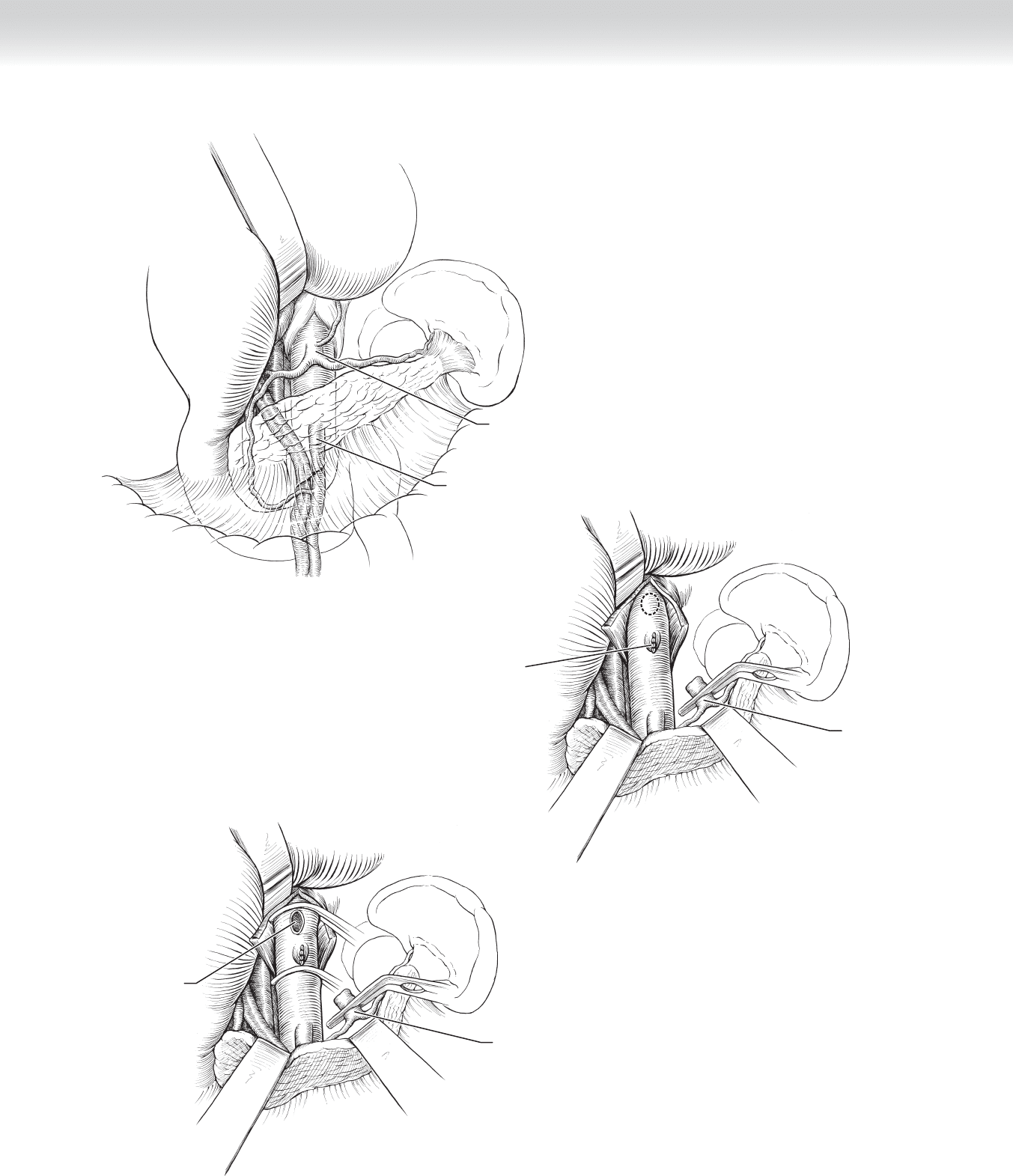
Mesenteric Thrombosis
◆ The proximal jejunum is usually ischemic because the stenosis involves the origin of the
SMA, and thrombectomy alone will not suffi ce.
◆ The SMA is isolated as for SMA embolectomy.
◆ After systemic heparinization, the SMA is occluded and a longitudinal arteriotomy is made
in the SMA below any palpable plaque.
◆ The thrombectomy catheter is then passed proximally and distally to remove any thrombus
present. Antegrade blood fl ow is usually diminished or absent, but retrograde fl ow may be
quite brisk because of well-established collaterals.
◆ Arterial infl ow will be required from either the supraceliac, infrarenal aorta, or iliac arteries,
which will be described subsequently.
Mesenteric Venous Thrombosis
◆ Mesenteric venous thrombosis may be primary or secondary to a number of conditions
including cancer, hypercoagulable states, polycythemia, trauma, dehydration, and pancre-
atitis. Thrombus most often involves the superior mesenteric vein (70%) and inferior
mesenteric vein (30%).
◆ At laparotomy, segmental small bowel congestion with edema of the mesentery is the usual
fi nding. Segmental resection is usually the only treatment necessary. Long-term treatment
with the anticoagulant warfarin (Coumadin) to prevent further thrombotic episodes is
instituted postoperatively.
Chronic Mesenteric Ischemia
◆ Usually high-grade stenosis or occlusion of two of the three vessels (celiac artery and SMA)
supplying the viscera is necessary to cause chronic mesenteric ischemia. Evidence of large
collaterals on angiography suggests the diagnosis.
Retrograde Aortosuperior Mesenteric Bypass
◆ The SMA is exposed as described for mesenteric embolectomy, and a self-retaining
retractor is placed.
◆ A segment of the abdominal aorta that is free of signifi cant atherosclerosis (as determined
on the CT scan) between the renal artery and IMA is isolated and mobilized.
◆ After systemic heparinization, the aorta is occluded between clamps, and an arteriotomy is
made on its anterior lateral aspect.

972 Section XII • Vascular
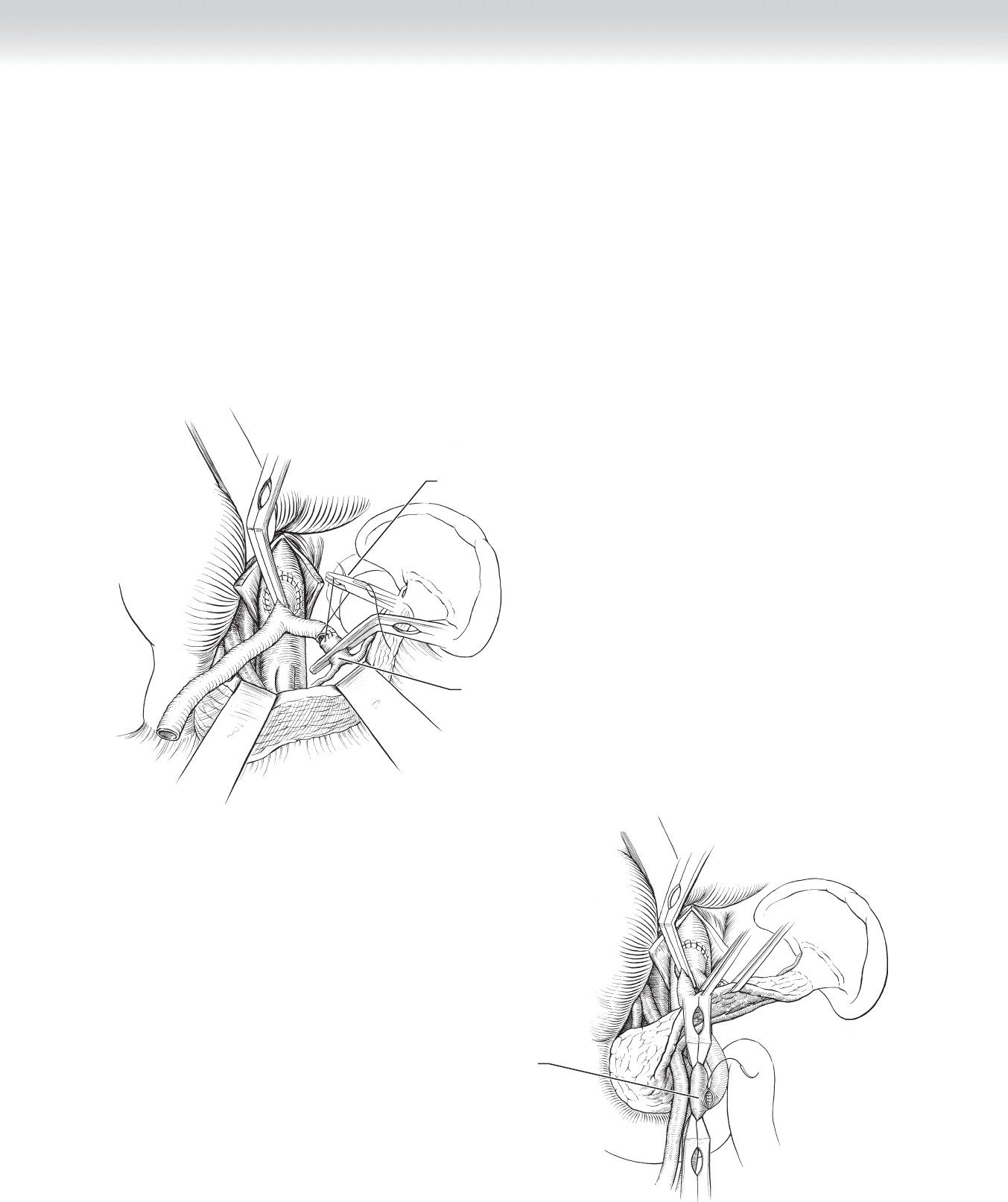
◆ A harvested segment of saphenous or superfi cial femoral vein or 6- or 7-mm ringed polytet-
rafl uoroethylene (PTFE) or Dacron graft is fashioned and anastomosed end-to-side to the
aorta with running 4-0 polypropylene suture (Figure 89-4, A). The graft is then routed in a
gentle curve to the SMA. The SMA and its branches distal to the stenosis or occlusion are
occluded with clamps and vessel loops, and a longitudinal arteriotomy is made beyond any
palpable plaque.
◆ The graft is anastomosed end-to-side to the SMA with running 5-0 or 6-0 polypropylene
suture, with care given to fl ush the artery and the graft before the anastomosis is completed
(Figure 89-4, B).
◆ The entire bowel is then inspected, the mesenteric vessels are auscultated, and the anasto-
moses are assessed with color fl ow Doppler ultrasound.

CHAPTER 89 • Mesenteric Ischemia 973
A
Superior
mesenteric artery
Aorta
Ringed
prosthetic graft
Inferior vena cava
Left renal vein
Completing
anastomosis
Atherosclerotic
lesion
Clamp
B
Superior
mesenteric artery
Aorta
Inferior vena cava
Left renal vein
Atherosclerotic
lesion
Ringed
prosthetic graft
FIGURE 89 –4

974 Section XII • Vascular
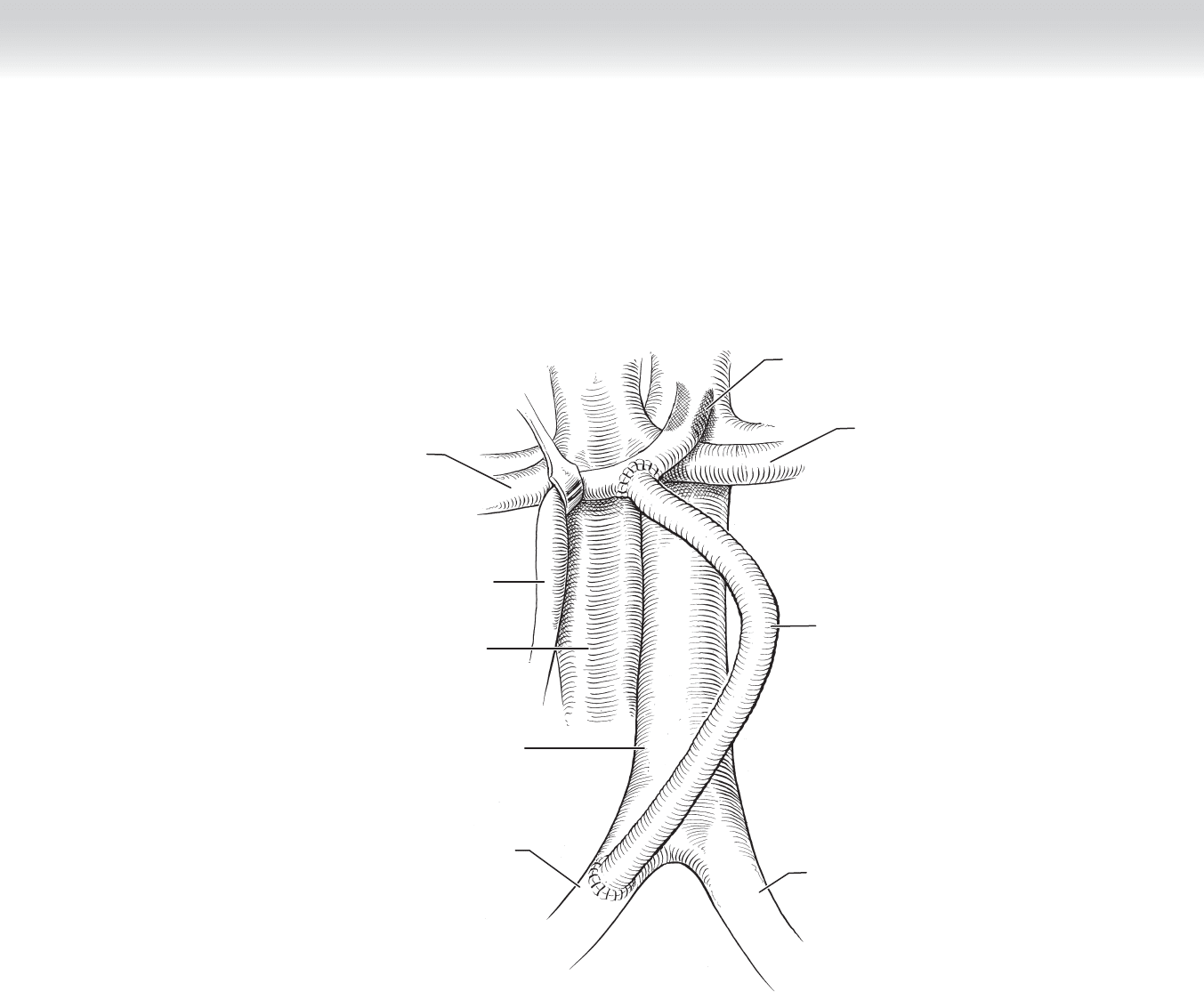
Antegrade Aortomesenteric Bypass
◆ When the infrarenal aorta is severely diseased, an antegrade mesenteric bypass originating
from the supraceliac aorta should be considered.
◆ After the abdomen is explored, the left lobe of the liver is mobilized by dividing the trian-
gular ligament, and the lesser sac is entered by dividing the gastrohepatic ligament.
◆ The stomach and esophagus are retracted to the left, with care given not to injure the vagus
nerves. The left lobe of the liver is retracted to the right with a self-retaining retractor
(Figure 89-5, A).
◆ The diaphragmatic crura and median arcuate ligament are then divided in the midline, and
the supraceliac aorta is mobilized for a distance of approximately 6 to 8 cm.
◆ The celiac artery and SMA are then identifi ed and mobilized by dividing the autonomic
neural fi bers so that a segment of each artery uninvolved with atherosclerosis is identifi ed.
Heparin (100 U/kg) and mannitol (25 g) are administered.
◆ The celiac artery is then divided between clamps, and the proximal end is oversewn with
5-0 polypropylene suture (Figure 89-5, B).
◆ The aorta is occluded between clamps, and an elliptical arteriotomy is made in the aorta
(Figure 89-5, C).
CHAPTER 89 • Mesenteric Ischemia 975
Celiac trunk
Superior
mesenteric artery
A
FIGURE 89 –5
C
Aorta ready for
anastomosis
Celiac artery
Celiac artery
Oversewn
celiac origin
B
976 Section XII • Vascular
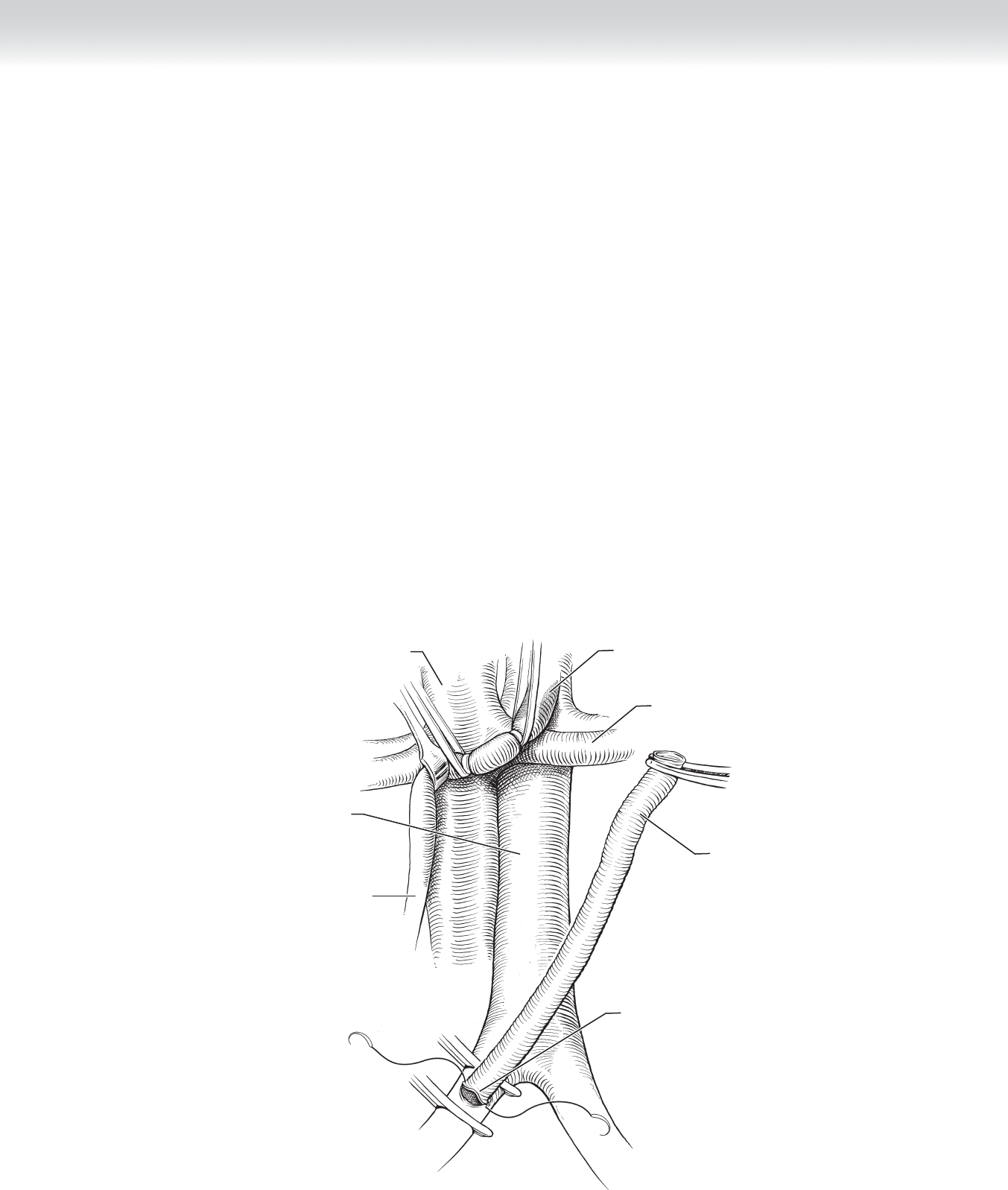
◆ A 14 ⫻ 7 bifurcated prosthetic graft is fashioned and anastomosed end-to-side to the aorta
with running 3-0 Prolene suture. One limb of the graft is cut to an appropriate length,
beveled, and anastomosed end-to-end to the distal celiac artery with 5-0 polypropylene
suture (Figure 89-5, D). The vessel and graft are fl ushed, the anastomosis is completed,
and fl ow is reestablished.
◆ The second limb of the graft is routed behind the pancreas to the SMA. The SMA is
occluded between clamps, and a longitudinal arteriotomy is made. The graft limb is dis-
tended with blood to its optimal length and is beveled, and the anastomosis is completed
with 5-0 or 6-0 polypropylene suture (Figure 89-5, E).
D
Celiac anastomosis
Celiac artery
Completing superior
mesenteric artery
anastomosis
(end-to-side)
E
FIGURE 89 –5, cont’d
CHAPTER 89 • Mesenteric Ischemia 977
Iliomesenteric Bypass
◆ When the supraceliac and infrarenal aorta are both severely involved with atherosclerosis or
the patient is in poor general health, the common iliac artery can be used as the infl ow
vessel.
◆ The peritoneum over the common iliac artery is incised, and a segment of artery is mobi-
lized, with care given not to injure the left common iliac vein.
◆ After systemic heparinization, the common iliac artery is occluded between clamps, and a
longitudinal is arteriotomy made. A limb of a bifurcated prosthetic graft including cuff of
the body or saphenous vein is fashioned and anastomosed end-to-side to the common iliac
artery with 4-0 polypropylene suture (Figure 89-6, A).
A
Superior
mesenteric artery
Aorta
Inferior vena cava
Left renal vein
Completing
anastomosis
Atherosclerotic
lesion
Ringed
prosthetic graft
FIGURE 89 –6
978 Section XII • Vascular
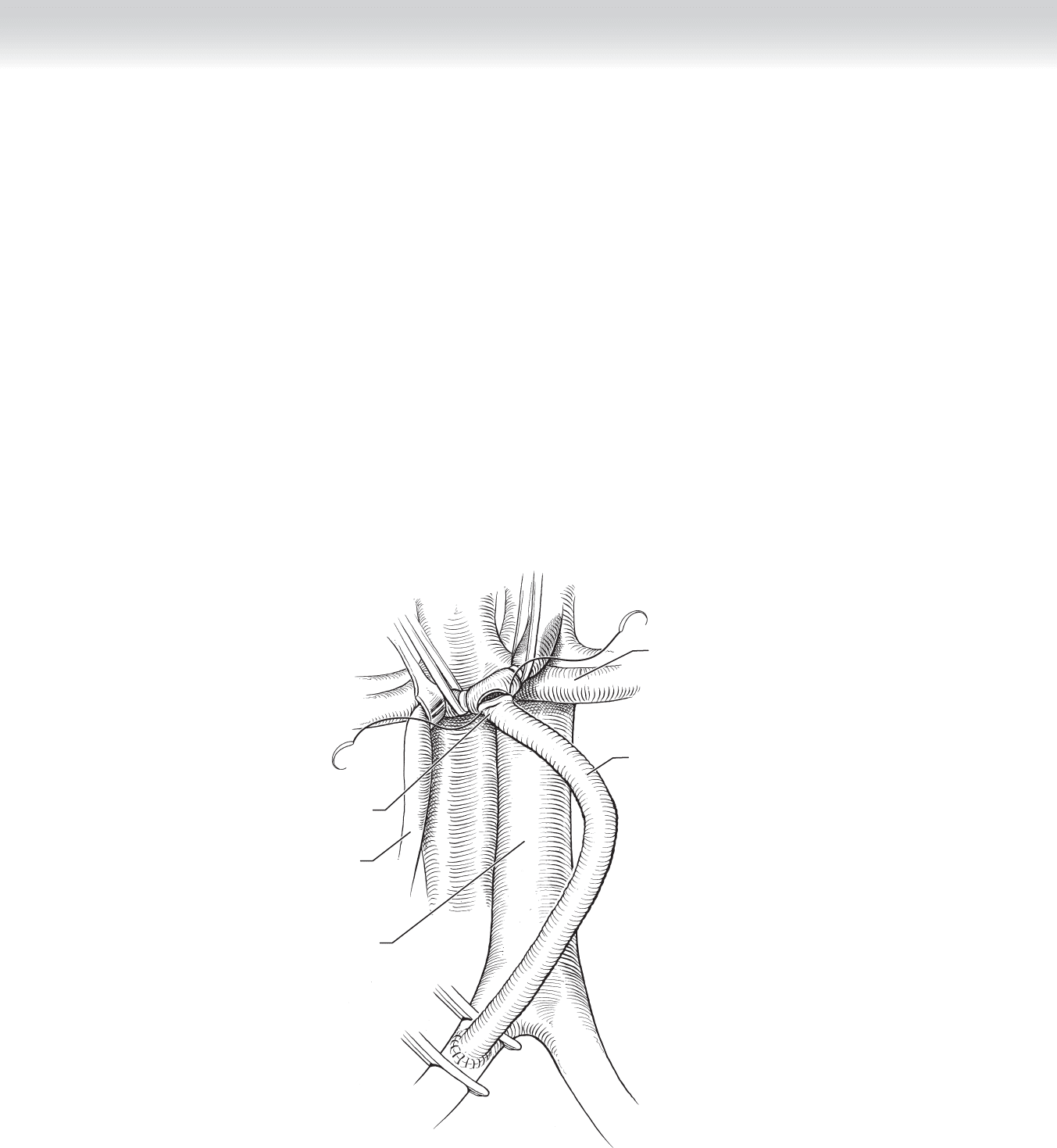
◆ The limb of the graft is routed in a gentle curve to the SMA, and the anastomosis is con-
structed end-to-side to the SMA with running 5-0 polypropylene suture (Figure 89-6, B-C).
3. CLOSING
◆ Hemostasis is secured, and the blood supply to the viscera is carefully assessed by palpation
and auscultation of the mesenteric vessels and interrogation of the anastomoses with color
fl ow Doppler ultrasound.
◆ The abdomen is then closed with a looped 1-0 polydioxanone (PDS) suture.
B
Aorta
Superior
mesenteric artery
Completing
anastomosis
Left renal vein
Ringed
prosthetic graft
FIGURE 89 –6, cont’d
CHAPTER 89 • Mesenteric Ischemia 979
Right common
iliac artery
Inferior
vena cava
Superior
mesenteric artery
Left renal vein
Right renal vein
Ringed
prosthetic graft
Left common
iliac artery
Atherosclerotic
lesion
C
Aorta
FIGURE 89 –6, cont’d

980 Section XII • Vascular
STEP 4: POSTOPERATIVE CARE
◆ The patient is returned to the intensive care unit. Fluid volume, hematocrit, acid-base sta-
tus, liver function tests, and clotting factors are carefully monitored and replaced. Persistent
acidosis is usually indicative of ongoing bleeding or bowel or hepatic ischemia.
◆ Colonoscopy should be performed with care if colonic ischemia is suspected, because an
intraluminal pressure greater than 30 mm Hg may further impair colonic blood fl ow.
Prompt surgery is indicated if there is persistent acidosis, ongoing bleeding, or evidence of
sepsis.
STEP 5: PEARLS AND PITFALLS
◆ Early diagnosis and treatment of mesenteric ischemia is essential if the survival rate is to be
improved.
◆ A planned second-look operation to resect marginally viable segments of bowel is an inte-
gral part of the postoperative care of patients with mesenteric ischemia.
◆ Ongoing bleeding may be due to increased fi brinolysis, especially in patients undergoing
antegrade mesenteric bypass with prolonged hepatic ischemia. After other causes of bleed-
ing have been excluded, blood should be drawn for plasminogen levels, and an infusion of
small amounts of epsilon aminocaproic acid should be considered.
◆ The choice of graft material is determined by the presence or absence of fecal contamina-
tion. Prosthetic grafts are preferred because they are less likely to kink. If there is gross con-
tamination, an autogenous saphenous vein or superfi cial femoral vein graft should be used.
These grafts should be carefully placed to avoid kinking and recurrent ischemia.
◆ Patients undergoing surgery for mesenteric ischemia may require large volumes of fl uid
intraoperatively and postoperatively and are prone to developing abdominal compartment
syndrome. If there is signifi cant bowel edema, the abdomen should not be closed primarily.
Temporary abdominal content containment with plastic bags (Bogota bag) or polyglactin
mesh or application of a wound vacuum-assisted closure (VAC) device and delayed
primary closure should be done once the visceral edema has resolved.
◆ There is ongoing debate about the number of vessels to be revascularized. Patients with
acute mesenteric ischemia are usually too critically ill to withstand total revascularization,
and only the SMA should be revascularized. Revascularization of both the celiac artery and
SMA should be considered in patients with chronic mesenteric ischemia.
