Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.


CHAPTER 87 • Fasciotomy—Forearm and Leg 941
2. DISSECTION
◆ The subcutaneous tissues are divided to expose the deep fascia, and individual muscles are
mobilized for examination (Figure 87-1, C).
◆ If the muscles of the dorsal compartment require release after the volar fasciotomy, a
straight longitudinal incision is made below the lateral epicondyle toward the midline of the
wrist.
◆ Other incisions described for the treatment of compartment syndrome criss-cross the fore-
arm or gently sweep across it in various directions.
◆ Incisions that cross the forearm will transect more of the venous and lymphatic return than
will a straight incision, and the resolution of forearm edema could be impaired. Such
incisions may also prevent the future design of a radial forearm fl ap, because the vascular
supply and outfl ow of the skin pedicle would be compromised.

942 Section XII • Vascular
3. CLOSING
◆ Dressings
◆ Cover the wound with saline-soaked gauze and a nonconstricting bandage.
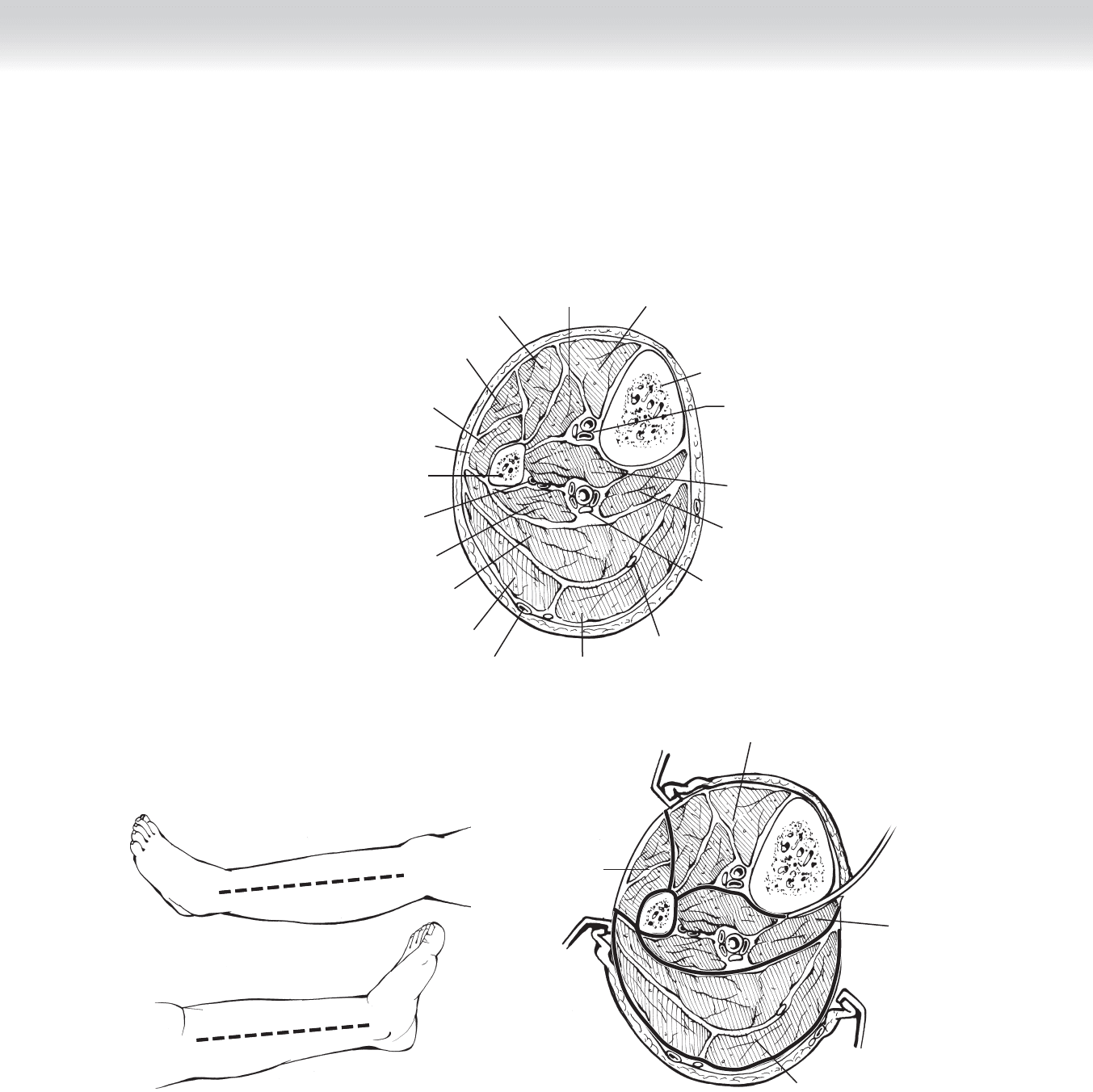
STEP 1: SURGICAL ANATOMY FOR LEG
◆ The lower leg has four muscular compartments with dense investing fascia that contribute
to the predisposition of this region to develop neurovascular compromise following injury
generally referred to as compartment syndrome.
◆ The treatment of compartment syndrome requires incision of the investing fascia of all four
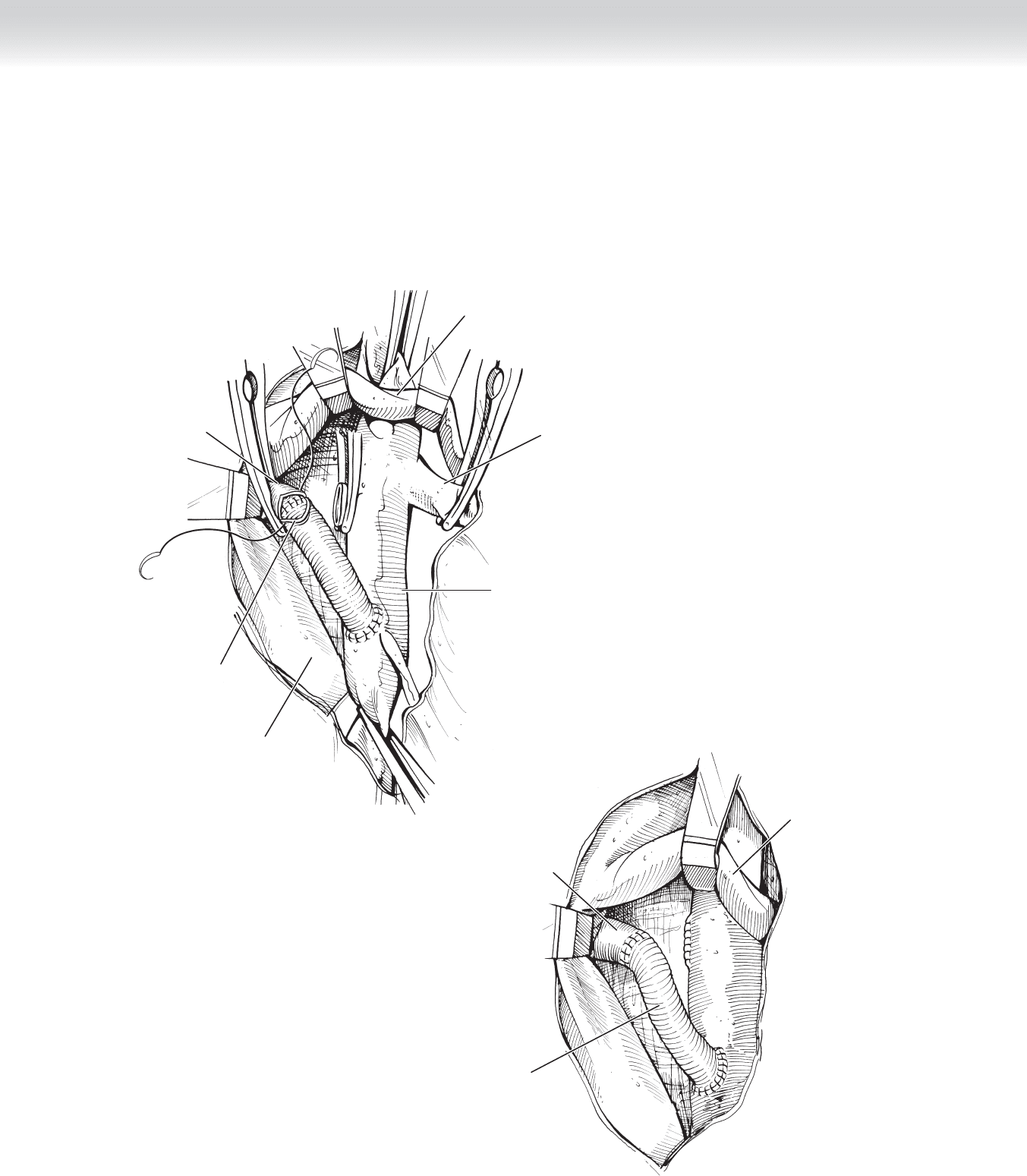
compartments: anterior, lateral, superfi cial posterior, and deep posterior (Figure 87-2, A).
STEP 2: PREOPERATIVE CONSIDERATIONS FOR LEG
◆ Same as previously mentioned for the forearm procedure.
STEP 3: OPERATIVE STEPS FOR LEG
1. INCISION
◆ Medial and lateral skin incisions are carried from just proximal to the medial and lateral
malleoli and carried cephalad to the level of the tibial plateau medially and the fi bula head
laterally, where care must be taken to avoid injury to the peroneal nerve (Figure 87-2, B).
2. DISSECTION
◆ Both the superfi cial and deep posterior compartments are released through the medial
incision, and the anterior and lateral compartments are released through the lateral incision
(Figure 87-2, C).
CHAPTER 87 • Fasciotomy—Forearm and Leg 943
Left Leg
Medial
Left Leg
Lateral
A
Tibialis
anterior muscle
Extensor hallucis
longus muscle
Extensor digitorum
longus muscle
Long
peroneal muscle
Short
peroneal muscle
Fibula
Interosseus membrane
Peroneal
artery, and vein
Flexor hallucis
longus muscle
Soleus muscle
Gastrocnemius muscle
lateral head
Gastrocnemius muscle
medial head
Plantaris
muscle tendon
Posterior
tibial artery,
vein, and nerve
Tibialis
posterior muscle
Flexor digitorum
longus muscle
Anterior tibial
artery, vein,
and nerve
Tibia
Lesser saphenous vein
C
Superficial
posterior compartment
Lateral
compartment
Deep
posterior
compartment
Anterior compartment
Lateral incision
Medial incision
B
FIGURE 87 –2

944 Section XII • Vascular
3. CLOSING
◆ Dressing of saline-soaked gauze and a nonconstricting bandage.
STEP 4: POSTOPERATIVE CARE
◆ Pain control is often a signifi cant issue following fasciotomy and is best managed with a
patient-controlled analgesia device. Wound care requires attention to aseptic technique and
ensures adequate material: sterile gowns, gloves, and dressing supplies are at hand before
dressing changes are begun to avoid contamination and serious morbidity associated with
wound infection. Elevation of the extremity will help reduce edema and hasten the recovery
and closure of the wound. The use of biologic dressings, either homograft or xenograft, may
also help in wound care.
STEP 5: PEARLS AND PITFALLS
◆ Most cases of compartment syndrome are adequately treated by release of the superfi cial
volar compartment, regardless of which surgical approach is chosen. Those clinical situa-
tions that mandate exploration of the deep volar or dorsal compartments, however, require
a signifi cant understanding of anatomy to follow a surgical approach that will minimize fur-
ther injury. Clinical examples include high-voltage electrical injury, severe crush injuries,
extended extrinsic forearm pressure (such as an unconscious patient lying on his or her
forearm), and ongoing evidence of myonecrosis or sepsis despite previous superfi cial fasci-
otomy. In some cases, even after compartment fasciotomy, the epimysium of individual
muscles must be incised to relieve persistently elevated tissue pressure. This can be
achieved only with adequate visualization of the deep space.
SELECTED REFERENCES
1. Lagerstrom CF, Reed RL Jr, Rowlands BJ, Fischer RP: Early fasciotomy for acute clinically evident post-
traumatic compartment syndrome. Am J Surg 1989;158:36-39.
2. Dente CJ, Feliciano DV, Rozycki GS, et al: A review of upper extremity fasciotomies in a level I trauma
center. Am Surg 2004;70:1088-1093.

945
Approximately 5% to 10% of patients with hypertension have renal artery stenosis (RAS) as the
underlying cause. Atherosclerotic occlusive disease in individuals older than 65 years and fi bro-
muscular dysplasia (FMD) in children and young adult females (20 to 40 years of age) are the
most common etiologies. Atherosclerosis of the renal arteries is usually confi ned to the orifi ce
and proximal third of the involved vessel (more commonly the left) and should be considered
as an extension of aortic atherosclerosis. In 20% of patients with RAS, there is severe associated
aortic aneurysmal or occlusive disease, which determines the extent and type of procedure to
be performed. RAS may occur in isolation (anatomic stenosis) or in association with hyperten-
sive ischemic nephropathy. FMD may be medial (85%), perimedial (10%), or intimal (5%) and
usually involves the mid-portion of the main renal arteries and their segmental branches.
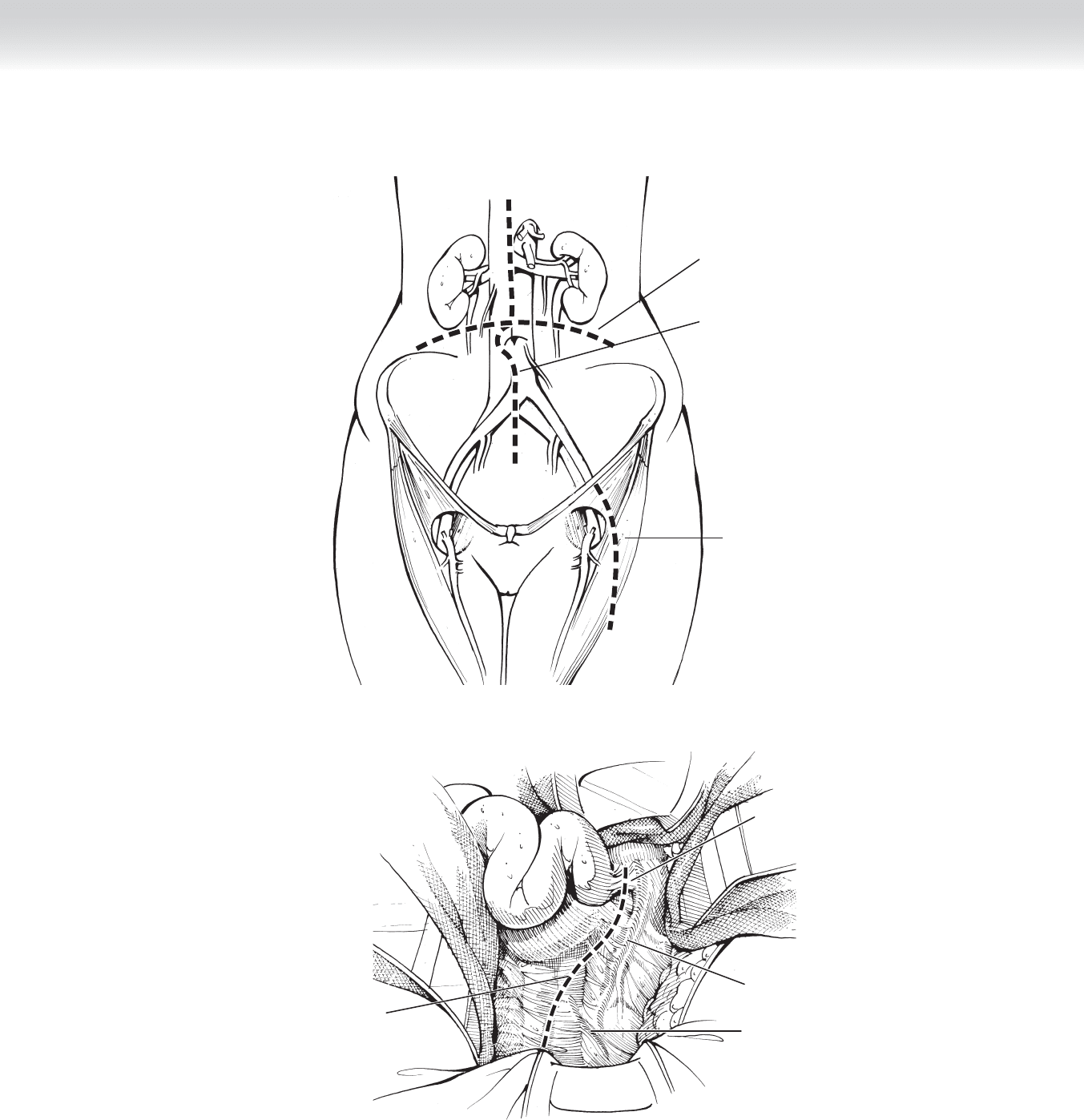
STEP 1: SURGICAL ANATOMY
◆ The renal arteries branch laterally from the aorta below the origin of the superior mesen-
teric artery. There is usually a single renal artery to each kidney. The right renal artery arises
higher and is longer than the left renal artery. The right renal artery runs posterior to the
inferior vena cava, right renal vein, head of the pancreas, and descending part of the duode-
num to the renal hilum. The left renal artery passes posterior to the left renal vein, body of
the pancreas, and splenic vein. Multiple renal arteries are present in up to 35% of patients
and should be identifi ed and evaluated before any surgical intervention.
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ Medical history, physical examination, and assessment of renal and cardiac function should
be performed in all patients. Features suggestive of RAS as the cause of hypertension
include hypertension of abrupt onset, hypertension refractory to medical therapy (more
than three drugs), unexplained azotemia or azotemia induced by angiotensin-converting
enzyme (ACE) inhibitors, and hypertension in children and young adults.
◆ Screening and diagnostic studies: Duplex ultrasound is useful as a screening test for RAS
and evaluation of kidney size. Interrogation of the renal arteries from their origin to the
hilum can be achieved in 95% of cases. A peak systolic velocity of greater than 180 cm/sec
and renal-to-aortic ratio ⱖ3.5 with distal turbulence is usually indicative of a hemodynami-
cally signifi cant stenosis (⬎60%). Occlusion of the renal artery is usually identifi ed by the
absence of a Doppler signal.
CHAPTER
88
Renal Revascularization
Glenn C. Hunter

946 Section XII • Vascular
◆ Computed tomography (CT) or digital angiography is used to delineate the stenosis before in-
tervening. There is a high risk of contrast-induced nephrotoxicity, and care should be taken in
performing these studies in patients with renal impairment. The administration of intravenous
(IV) fl uids (1.5 mL/kg/hr), limiting the dose of or diluting the contrast agent, and the adminis-
tration of acetylcysteine 600 mg orally before and after the contrast procedure are among the
measures used to reduce the risk of nephrotoxicity. Magnetic resonance angiography is an alter-
native method of assessing RAS in patients with a glomerular fi ltration rate ⱖ30 ml/min/1.73 m
2
.
◆ Functional studies: A captopril renal scan may be helpful if there is unilateral stenosis and
minimal parenchymal disease. The signifi cance of unilateral RAS should be confi rmed by
plasma renin determinations. This may require admission to the hospital, withholding med-
ications that interfere with renin release, and sodium restriction (ⱕ2 g Na
⫹
/day) for approx-
imately 2 weeks.
◆ Indications for the operative treatment of RAS include stenosis greater than 70% with
poorly controlled hypertension, renal insuffi ciency, or recurrent bouts of congestive heart
failure (CHF) with no attributable myocardial ischemia. Patients with branch vessel disease
and FMD and selected patients with restenosis after angioplasty and stenting may be
candidates for surgery.
STEP 3: OPERATIVE STEPS—AORTORENAL BYPASS
◆ The patient is admitted the day before the procedure for IV hydration, control of blood
pressure, and a mechanical bowel preparation. Antihypertensive medications should be
reduced to the minimum necessary to control the blood pressure. If the diastolic blood
pressure is higher than 120 mm Hg, the patient should be admitted to the intensive care
unit (ICU) and the blood pressure controlled with IV sodium nitroprusside or nicardipine.
1. INCISION
◆ A midline or transverse incision allows both access to the renal arteries and reconstruction
of associated aortic disease if required. The abdomen is explored, the transverse colon
and small bowel are lifted out of the abdomen, and a self-retaining retractor such as the
Omni-Tract system is placed (Figure 88-1, A).
2. DISSECTION
◆ The peritoneum over the aorta is incised in the midline, and the dissection is carried down
to the left renal vein superiorly and the aortic bifurcation inferiorly (Figure 88-1, B). The
left renal vein is then mobilized and retracted cephalad or caudally depending on the loca-
tion of the origin of the renal vessels. Retraction of the left renal vein is facilitated by liga-
tion and division of the gonadal, adrenal, and lumbar veins.
◆ Both renal arteries are then dissected out 2 cm beyond the orifi cial stenotic lesion. An aor-
torenal bypass is the most common revascularization procedure performed but requires
clamping of the aorta. This technique is applicable only to patients with large paired renal
arteries with minimal aortic atherosclerosis or aneurysmal dilation.
CHAPTER 88 • Renal Revascularization 947
Midline incision
Transverse incision
Incision over
femoral vessels
and saphenous vein
A
B
Ligament
of Treitz
Inferior
mesenteric
artery
Marginal
artery
Peritoneal
incision
FIGURE 88 –1
948 Section XII • Vascular
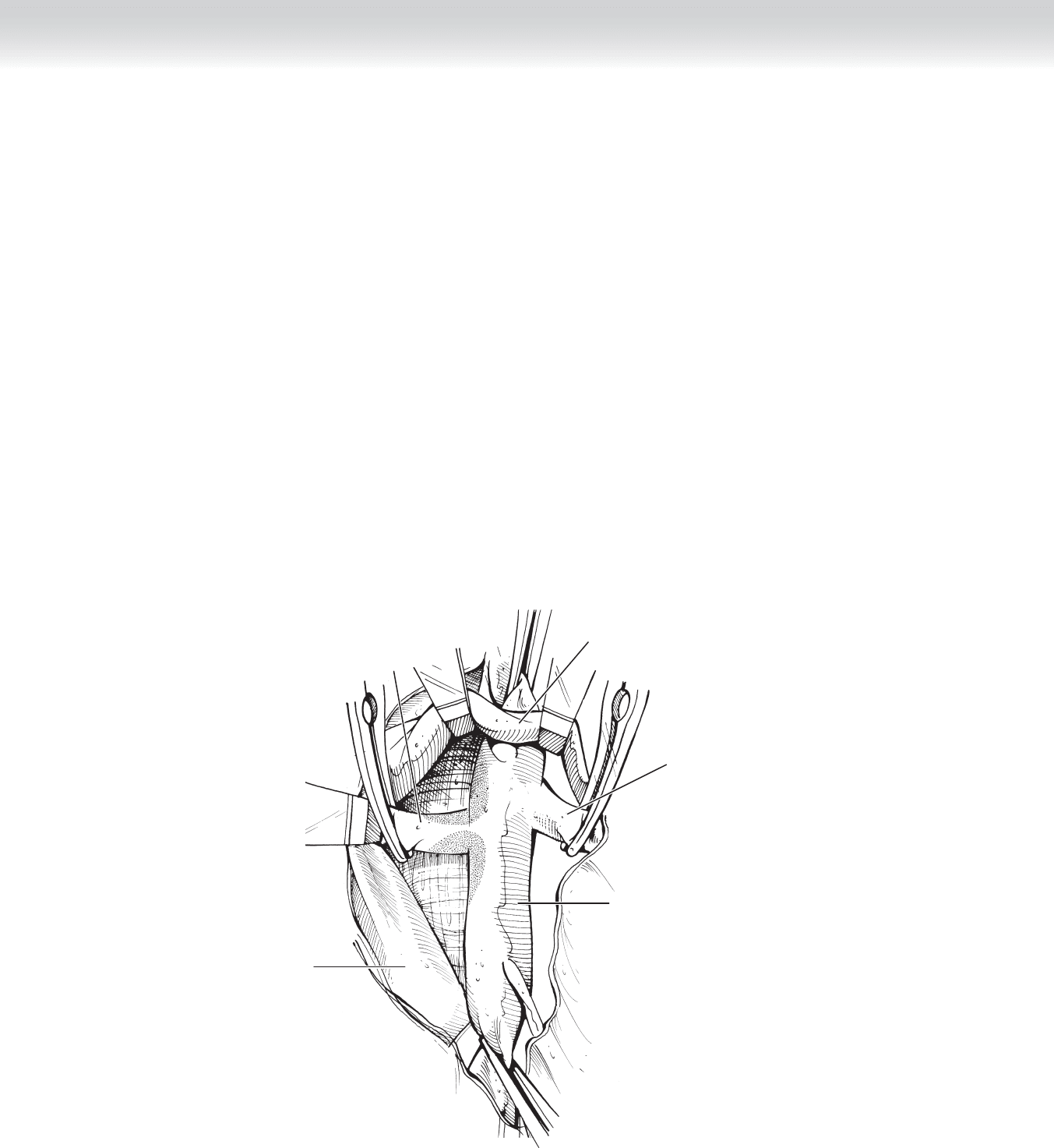
◆ The proximal right renal artery is exposed by retracting the left renal vein superiorly
and the vena cava to the right. The distal portion of the renal artery is exposed by mobiliz-
ing the duodenum and hepatic fl exure medially. If both renal arteries need to be exposed,
the entire small bowel is mobilized from the ligament of Treitz to the mesentery of the
cecum and along the right paracolic gutter to the foramen of Winslow. The peritoneal
incision is extended along the inferior border of the pancreas, exposing the aorta above the
origin of the superior mesenteric artery.
◆ Once the renal arteries have been isolated, a segment of the infrarenal aorta below the renal
arteries is mobilized. After systemic heparinization (100 U/kg) and the administration of
mannitol (12.5 to 25 g), the aorta is occluded below the renal arteries and above the bifur-
cation, and an ellipse approximately three times the diameter of the renal artery is excised
from the anterior lateral aortic wall. Saphenous vein or a prosthetic Dacron or polytetra-
fl uoroethylene (PTFE) graft 6 or 7 mm in diameter is beveled, and the aortic anastomosis is
completed with 4-0 polypropylene suture (Figure 88-2, A-C).
Abdominal
aorta
A
Right
renal artery
Left
renal vein
Inferior
vena cava
Left
renal artery
FIGURE 88 –2
CHAPTER 88 • Renal Revascularization 949
B
Harvested
saphenous vein
Abdominal
aorta
C
Right
renal artery
Left
renal vein
Left
renal artery
Prosthetic
graft
Inferior
vena cava
FIGURE 88 –2, cont’d
950 Section XII • Vascular
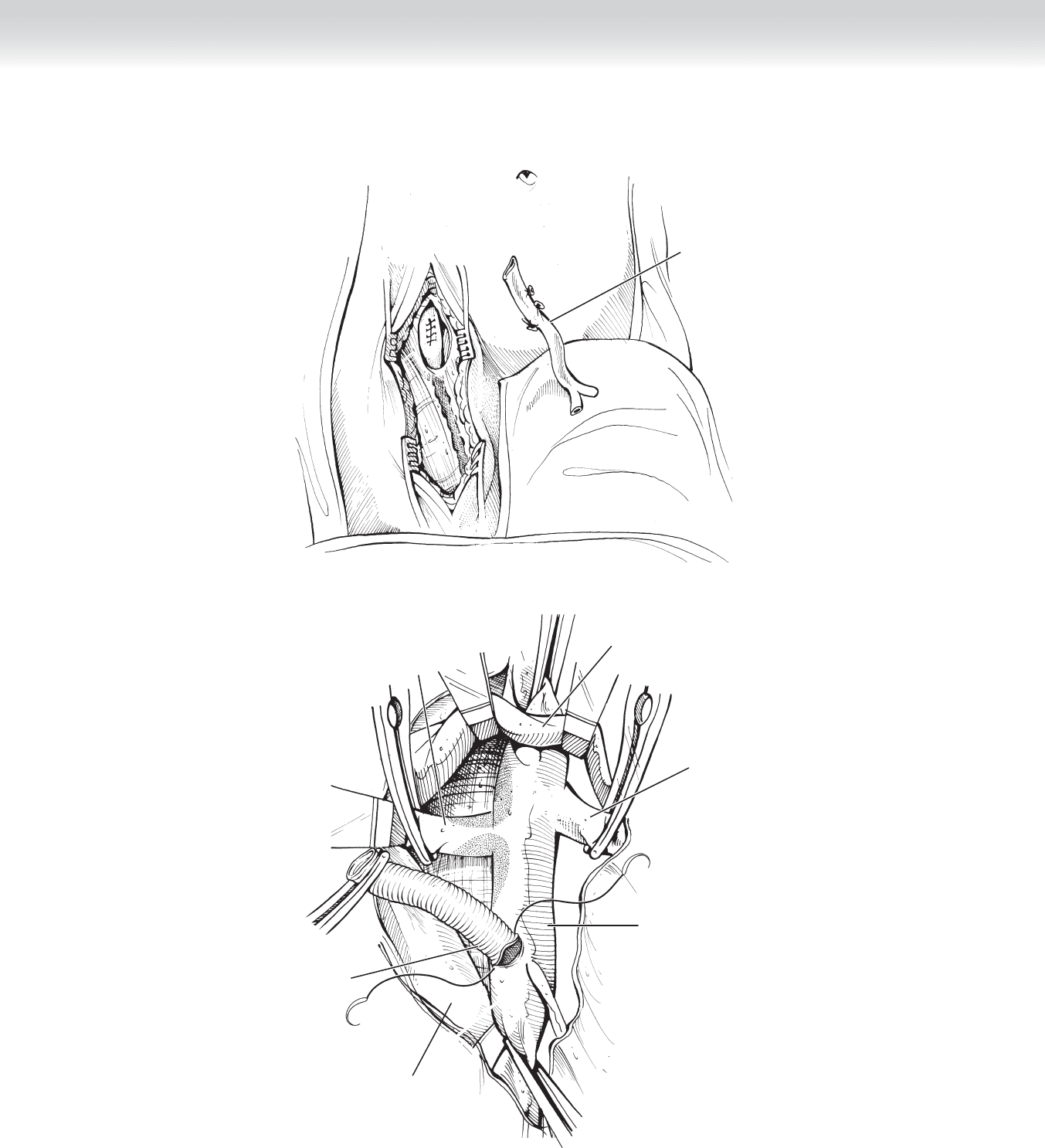
◆ The renal artery is divided between clamps, and the proximal end of the artery is oversewn
with 5-0 polypropylene suture. The saphenous vein or prosthetic graft is spatulated, and
the distal anastomosis is constructed end-to-end with running (posterior wall) and inter-
rupted 6-0 polypropylene suture (Figure 88-2, D-E).
D
Inferior
vena cava
Abdominal
aorta
Right
renal artery
Left
renal vein
Left
renal artery
Completing
distal anastomosis
Left
renal vein
Right
renal artery
Prosthetic
graft
E
FIGURE 88 –2, cont’d
