Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.

studies have shown that the risk of coronary artery
disease rises with the cholesterol level. Several large-
scale intervention studies have demonstrated that
lowering cholesterol reduces CHD risk in both pri-
mary and secondary (after the event) prevention.
0023 In addition to common or polygenic hyperchol-
esterolemia, a number of well-defined inherited
syndromes are well recognized resulting in hyper-
cholesterolemia and an increased CHD risk.
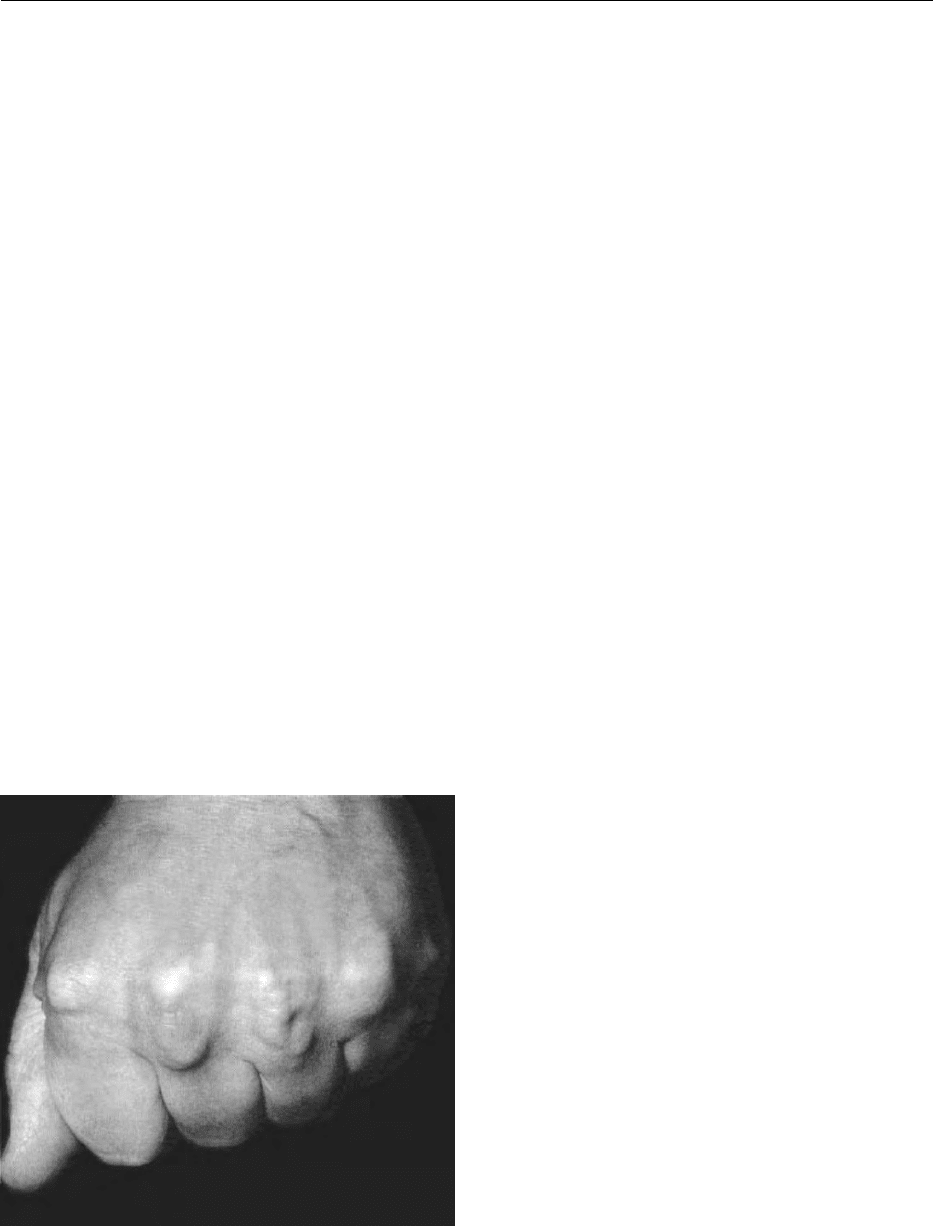
Familial Hypercholesterolemia (FH)
0024 Familial hypercholesterolemia is the commonest dis-
ease in Western populations to be caused by a single
dominant gene defect. It is characterized by a raised
cholesterol from birth, subsequent development of
cutaneous and tendon xanthomata, and premature
vascular disease (Figure 6). The gene coding the
LDL receptor is found on chromosome 19. Over
150 different LDL receptor mutations have been
characterized, affecting receptor synthesis and func-
tion. Heterozygous FH (1 mutant and 1 normal gene)
affects 0.2% of the population, the homozygous con-
dition occurring at a rate of 1:1 000 000. A true
homozygote will have two copies of the same defect,
but compound heterozygosity (with two different
defects) is more common.
0025 Homozygous FH is characterized by extreme
hypercholesterolemia (cholesterol is approximately
four times normal) with cutaneous and tendon xan-
thomata and corneal arcus beginning in childhood.
Significant atheromatous involvement of the aortic
root with coronary ostial stenosis is present by pu-
berty, and death from coronary heart disease usually
occurs prior to the age of 20 in untreated individuals.
0026Tendon xanthomata are also pathognomonic of
heterozygous FH occurring in some adults. LDL chol-
esterol is typically twice normal. Untreated, it leads to
CHD in 50% of males by the age of 50 years, and
50% will have died by the age of 60. Fifty per cent of
females will have clinical CHD by age 60 when 15%
will have died.
0027The diagnosis of homozygous FH is usually
straightforward. Heterozygous FH should be con-
sidered in any patient with hypercholesterolemia
and personal or family premature CHD. Tendon
xanthomata in any family member almost certainly
establish the diagnosis, as does high LDL in children.
0028FH is also caused by abnormalities in apoB such as
in familial defective apolipoprotein B-100 where a
glutamine-for-arginine substitution in the amino acid
3500 codon in apoB produces an abnormal truncated
apoB with impaired binding to the LDL receptor.
Like classical FH, it is also an autosomal dominant,
affecting about one in 600 of the population.
Familial Combined Hyperlipidemia (FCH)
0029FCH was first described in 1973 in families of hyper-
lipidemic patients surviving a myocardial infarction.
Less clearly defined than FH, it affects perhaps 1–2%
of the population. It is heterogeneous, the etiology
remaining uncertain without a single gene defect
having been found. Diagnosis requires multiple
affected family members and is complicated by
variation in time of lipid levels that on occasion may
be normal. Cholesterol, triglycerides, or both may be
raised with type IIa, IIb, or IV phenotypes.
0030FCH predisposes to premature atherosclerosis and
may be present in 10% of patients with CHD before
age 60. Elevated apoB levels are frequently found that
may have a central role in atherogenesis in FCH, and
apoB concentrations can be a better predictor of
CHD than LDL cholesterol. LDL and VLDL each
contain one apoB100 molecule, so when apoB is
raised, there are increased plasma particle numbers.
As LDL numbers increase, the apoB:LDL cholesterol
ratio rises, as each particle is relatively cholesterol-
poor. LDL particles in FCH are smaller, denser, and
more atherogenic (see hyperlipidemia and the origins
of clinical atheroma). LDL
3
synthesis is enhanced by
the presence of hypertriglyceridemia.
0031In FCH, no mutations have been found in the apoB
structural locus on chromosome 2, but an apoB-
raising allele of uncertain location may occur in
fig0006 Figure 6 Xanthomata in the extensor tendons of the hands in
familial hypercholesterolemia. Reproduced from Hyperlipid-
aemia, Encyclopaedia of Food Science, Food Technology and Nutri-
tion, Macrae R, Robinson RK and Sadler MJ (eds), 1993,
Academic Press.
HYPERLIPIDEMIA (HYPERLIPIDAEMIA) 3189
some FCH patients. Families heterozygous for LPL or
apoC-II deficiency (see Severe hypertriglyceridemia
below) may exhibit a phenotype similar to FCH.
Further work is needed to characterize the FCH gen-
etic background. Hyperapobetalipoproteinemia is a
related condition characterized by raised apoB with
normal LDL associated with premature CHD.
Hypertriglyceridemia
0032 Hypertriglyceridemia results from overproduction
of triglyceride-rich lipoproteins and/or a catabolic
defect, due to either a primary lipoprotein disorder
or secondary to associated diseases.
Severe hypertriglyceridemia
0033 Severe hypertriglyceridemia (triglycerides > 11 mmol
l
1
) usually results from secondary factors (e.g., un-
controlled diabetes mellitus, obesity with insulin re-
sistance, and excess alcohol) acting upon a less severe
hyperlipidemia. Usually, treatment of the underlying
problem will partly correct the hypertriglyceridemia.
Inherited abnormalities of lipoprotein metabolism,
producing severe hypertriglyceridemia, cause accu-
mulation of chylomicrons with or without VLDL.
This gives a pancreatitic, and rarely a CHD, risk.
0034 Lipoprotein lipase deficiency A recessively inherited
condition affecting one per million population, this
deficiency is caused by mutations in the LPL gene on
chromosome 22 resulting in defective function and
chylomicron accumulation. Recurrent pancreatitis
usually occurs in early adulthood. Eruptive xantho-
mata are characteristic, and hepatosplenomegaly
and lipemia retinalis may occur, with triglycerides
100 mmol l
1
.
0035 Apolipoprotein C-II deficiency ApoC-II activates
LPL, and deficiency therefore presents similarly to
LPL deficiency, although it is rarer.
Moderate hypertriglyceridemia
0036 Moderate hypertriglyceridemia is often polygenic
exacerbated by secondary causes. It is seen frequently
with type 2 diabetes and obesity and is an independ-
ent CHD risk factor, particularly when associated
with a low HDL cholesterol. High triglycerides result
in reduced synthesis of HDL, more of which will be
HDL
3
, increased plasma levels of LDL
3
, and a
consequent increased risk of atheroma.
0037 The Insulin Resistance Syndrome (see Table 3) This
term was coined in 1988 to describe a cluster of
abnormalities that frequently occur together in type
2 diabetes. These people are often hypertensive and
obese with associated insulin resistance and hyper-
insulinemia. A consequence of insulin resistance is
increased catabolism of adipose tissue triglyceride
with release of nonesterified fatty acids. In the liver,
these are reformed into triglycerides and packaged as
VLDL, with larger VLDL numbers and size, a lower
HDL, and proportionately more LDL
3
. This partly
explains the threefold CHD increase seen in men with
type 2 diabetes and the three- to fivefold increase in
women.
Mixed Hyperlipidemia
0038Mixed hyperlipidemia with elevated triglycerides and
cholesterol is most commonly caused by polygenic
elevation of VLDL exacerbated by lifestyle or
environmental factors. It can manifest in FCH or FH.
Remnant Hyperlipidemia
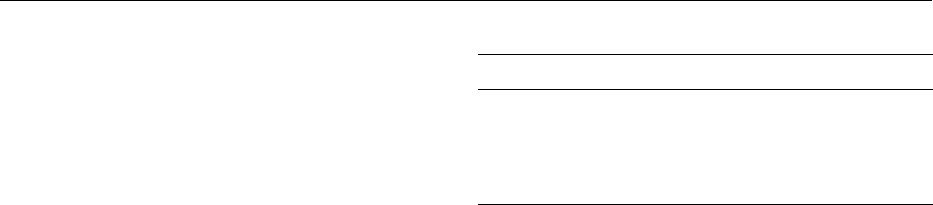
0039Remnant hyperlipidemia is also known as dysbeta-
lipoproteinemia, broad beta disease, or type III
hyperlipidemia, and has been recognized as a distinct
disease for 40 years. Remnant particles (IDL or b-
VLDL) of partial chylomicron or VLDL degradation
accumulate in about one in 5000 individuals, although
the gene defect affects about 1% of the population.
The diagnostic features are palmar crease and tuber-
ous xanthomata (Figure 7). Important complications
are premature CHD and peripheral vascular disease,
the predisposition to the latter being more than with
other dyslipidemias. It is more prevalent in men than
women, manifesting at age 25–40. The clinical dis-
order is brought out by factors such as obesity, dia-
betes, and untreated hypothyroidism.
0040Apolipoprotein E(apoE) is a 299-amino-acid glyco-
protein on all lipoproteins except LDL, serving as a
high-affinity ligand with the LDL, LRP, and apoE
receptors. A single gene controls ApoE expression,
with three common alleles, e2, e3, and e4, giving
rise to the major isoforms, E2, E3, and E4. Six differ-
ent phenotypes result: E2/E2, E2/E3, E2/E4, E3/E3,
E3/E4, and E4/E4. E3/E3 is the most common,
being found in 50–70% of populations. Isoforms
differ in amino acid composition, apoE2 having a
tbl0003Table 3 Features of the Insulin Resistance Syndrome
SyndromeX (The InsulinResistance Syndrome)
Hyperinsulinemia
Impaired glucose tolerance
Hypertension
Increased triglyceride
Decreased HDL cholesterol
3190 HYPERLIPIDEMIA (HYPERLIPIDAEMIA)
cysteine-for-arginine substitution at amino acid 158.
This reduces binding to the apoE receptor to *1% of
normal. Homozygosity for apoE2 is the commonest
genotype in remnant hyperlipidemia. However, the
abnormality does not usually lead to hyperlipidemia,
but rather to marginally lower LDL cholesterol levels,
for it is only with secondary factors or an additional
primary lipemia that the syndrome is clinically ex-
pressed.
Dietary Effects
Body weight
0041 Obesity is an often ignored factor in hyperlipidemia,
but it is important, not least because it is linked
to other CHD risk factors such as blood, diabetes,
and glucose intolerance. Weight control is important
in treating hyperlipidemia, coupled with increased
exercise.
Fatty Acids and Cholesterol
0042 In Western societies, reducing saturated fat intake as
a percentage of total food energy is associated with a
reduction in total cholesterol and, to a lesser extent,
triglycerides. Levels of LDL fall, possibly as a result of
a direct reduction of cholesterol synthesis in the liver,
or increased excretion as bile acids. If saturated fatty
acids, such as palmitic acid, are replaced by mono- or
polyunsaturated fatty acids, such as oleic or linoleic
acids, similar falls in serum cholesterol occur.
0043 Polyunsaturated fats of the n-6 series are primarily
of plant origin. In addition to the above, they help
reduce cholesterol by taking the place in the diet of
saturated fats, which tend to be of animal origin and
high in cholesterol. The n-3 series of fatty acids come
mainly from oily fish. These fatty acids may also have
beneficial effects on hemostatic variables of benefit in
thrombosis prevention. They can lower triglyceride
levels in some moderately hypertriglyceridemic indi-
viduals, but may have the disadvantage of increasing
LDL cholesterol. Plant sterols and stanols may also
reduce LDL by 10%.
0044The assumption that the amount of cholesterol in
the diet is the major factor causing hyperlipidemia is
false. It is the total fat intake as a percentage of the
total energy intake, and also whether or not the fat is
saturated, that matters most. Only a proportion of
cholesterol in the diet is absorbed, and for each
100 mg eaten, the serum cholesterol will rise by only
approximately 0.1 mmol l
1
. This response to dietary
cholesterol shows a considerable variation between
individuals.
Carbohydrate and Fiber
0045A high carbohydrate intake (particularly refined
carbohydrate and simple sugars) may induce hyper-
triglyceridemia. Substantial amounts of soluble or
mucilaginous fiber in the diet can lower LDL choles-
terol, possibly by increasing the fecal loss of sterols.
Individuals who eat a high-fiber diet also tend to eat
less saturated fat, and less total fat.
Alcohol
0046Alcohol, a rich source of energy, can contribute to
obesity and hypertriglyceridemia, and increase hep-
atic triglyceride synthesis and VLDL secretion. Sub-
strates that undergo oxidation in the liver have to
compete with alcohol, and therefore tend to be avail-
able for increased triglyceride synthesis. The tendency
to develop severe hypertriglyceridemia secondary to
alcohol is variable, but the risk of acute pancreatitis is
also increased.
See also: Bile; Cholecalciferol: Physiology; Cholesterol:
Role of Cholesterol in Heart Disease; Choline: Properties
and Determination; Essential Fatty Acids; Fats:
Classification; Occurrence; Fatty Acids: Properties;
Metabolism; Gamma-linolenic Acid; Fish Oils: Dietary
Importance; Hormones: Steroid Hormones;
Lipoproteins; Phospholipids: Properties and
Occurrence; Triglycerides: Structures and Properties
Further Reading
Barter PJ and Rye K (ed.) (1999) Plasma lipids and their role
in disease. In: Advances in Vascular Biology, vol. 5.
Chur, Switzerland: Harwood Academic Publishers.
fig0007 Figure 7 Palmar crease xanthomata of dysbetalipoprotein-
emia (remnant hyperlipidemia). Reproduced from Hyperlipid-
aemia, Encyclopaedia of Food Science, Food Technology and
Nutrition, Macrae R, Robinson RK and Sadler MJ (eds), 1993,
Academic Press.
HYPERLIPIDEMIA (HYPERLIPIDAEMIA) 3191

Betteridge DJ (ed.) (1990) Lipid and lipoprotein disorders.
In: Ballie
`
re’s Clinical Endocrinology and Metabolism,
vol. 4, no. 4. London: Ballie
`
re Tindall.
Betteridge DJ, Illingworth DR and Shepherd J (ed.) (1999)
Lipoproteins in Health and Disease. London: Arnold.
Durrington PN (1989) Hyperlipidaemia: Diagnosis and
Management. Oxford: Wright Butterworth.
Packard C and Caslake M (1996) Mixed hyperlipidaemia
and the lipid shuttle. Issues in Hyperlipidaemia 13: 1–6.
Reaven GM (1988) Banting Lecture 1988. Role of insulin
resistance in human disease. Diabetes 37(12):
1595–1607.
Syvanne M and Taskinen M (1997) Lipids and lipoproteins
as coronary risk factors in non-insulin dependent dia-
betes mellitus. The Lancet 350(supplement 1): 20–23.
Thompson GR (1999) The proving of the lipid hypothesis.
Current Opinion in Lipidology 10: 201–205.
HYPERTENSION
Contents
Physiology
Hypertension and Diet
Nutrition in the Diabetic Hypertensive
Physiology
J J Klawe and M Tafil-Klawe, The Ludwik-Rydygier
Medical University, Bydgoszcz, Poland
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Introduction
0001 An elevated blood arterial blood pressure is one of
the more important public health problems, being
asymptomatic, easily detectable, and often leading
to lethal complications.
Definition
0002 In adults a diastolic pressure below 85 mmHg is nor-
mal, between 85 and 89 mmHg is high normal, 90–
104 mmHg is mild hypertension, 105–114 mmHg
moderate hypertension, and 115 mmHg or greater is
severe hypertension. When the diastolic pressure is
below 90 mmHg, a systolic pressure below 140 mmHg
indicates normal blood pressure, between 140 and
159 mmHg is borderline isolated systolic hyperten-
sion, 160 mmHg or higher is isolated systolic hyper-
tension. Patients with arterial hypertension and no
definable cause are said to have primary, essential,
or idiopathic hypertension. More than 90% of all
patients with arterial hypertension are considered to
have essential or primary hypertension.
0003 The various forms of arterial hypertension are
listed below as a simplified classification of arterial
hypertension:
1.
0004Systolic hypertension with wide pulse pressure
a.
0005Decreased compliance of aorta
b.
0006Increased stroke volume
2.
0007Systolic and diastolic hypertension (increased
peripheral vascular resistance)
a.
0008Renal
b.
0009Endocrine
c.
0010Neurogenic
d.
0011Miscellaneous
e.
0012Unknown etiology
Individuals with a specific organ defect which is
responsible for hypertension are defined as having a
secondary form of hypertension.
0013The following information relates to the primary
form of arterial hypertension. Cardiac output and
peripheral vascular resistance are two basic hemody-
namic parameters regulating mean arterial pressure.
Cardiac output is usually normal in patients with
essential hypertension. Elevated blood pressure
appears to be associated with increased peripheral
vascular resistance. Some investigators have specu-
lated that the increased resistance may be due to
lack of nitric oxide, the locally produced vasodilator
that is produced by endothelial cells.
Genetic Factors in Hypertension
0014Animal studies and human investigations have indi-
cated an important role of genetic factors in essential
hypertension. Most studies support the concept that
inheritance is probably multifactorial or that a
number of different genetic defects each have elevated
blood pressure as one of their phenotypic expressions.
3192 HYPERTENSION/Physiology

Three monogene defects – glucocorticoid-remediable
aldosteronism (GRA), syndrome of apparent mineral-
ocorticoid excess (AME), and Liddle’s syndrome –
and susceptibility genes such as angiotensinogen gene
(AGT), renin gene (RN), pseudohipoaldosteronism
type II, and a-adducin gene (ADDI) have been
reported which have as one of their consequences
increased arterial pressure.
Environmental Factors
0015 A number of environmental factors are involved in the
development of hypertension. These include: obesity,
salt intake, alcohol intake, family size, and occupa-
tion. The influence of these factors increases with the
age of patients.
Salt Sensitivity
0016 In hypertensive population the blood pressure in
about 60% is responsive to level of sodium intake.
The cause of this special sensitivity to salt varies, and
includes primary aldosteronism, bilateral renal artery
stenosis, and other factors.
Renin and its Importance in Hypertension
0017 Renin is an enzyme secreted by the juxtaglomerular
cells of the kidney. It interacts with aldosterone in a
negative-feedback loop. Some hypertensive patients
are defined as having low-renin and high-renin
essential hypertension. About 20% of hypertensive
patients have suppressed plasma renin activity.
Approximately 15% of patients with essential hyper-
tension have plasma renin activity levels above the
normal range, which suggests that in these patients
plasma renin plays a significant role in the pathogen-
esis of arterial hypertension, activating the renin–
angiotensin–aldosterone axis. However other findings
have led some investigators to postulate that the
elevation of blood pressure and elevated renin levels
may be secondary to an increase in adrenergic system
activity.
Cell Membrane Defect
0018 The hypothesis about the role of a generalized cell
membrane defect in the pathogenesis of salt-sensitive
hypertension is derived from data from studies on red
blood cells, in which abnormalities in the transport
of sodium across the cell membrane have been
documented. This abnormality in sodium transport
reflects an alteration in cell membrane, and this defect
may occur in all cells of the body. An abnormal
accumulation of calcium in vascular smooth muscle
results in an increase in vascular responsiveness to
vasoconstrictor agents.
Reflex Mechanisms in Regulation of Blood
Pressure in Arterial Hypertension
0019The reflex mechanisms regulating blood pressure
include: arterial baroreceptors, cardiopulmonary
mechanoreceptors, arterial chemoreceptors, and
visceral receptors localized in the kidney, liver, and
intestine.
0020The baroreceptor reflex and from cardiopul-
monary mechanoreceptors are primary homeostatic
controls for blood pressure. Stretch-sensitive
mechanoreceptors are tonically active and thereby
tonically decrease a sympathetic activity. Addition-
ally, local release of NO from vascular epithelium
after each increase in blood pressure counteracts
blood pressure elevation. The cardiac response to
baroreceptor activation is vagal activation and a
decrease in heart rate. Several studies have shown
the impairment of baroreceptor function in arterial
hypertension.
0021The carotid chemoreceptors, activated by partial
pressure of oxygen in arterial blood and its
decrease, showed an augmented resting drive in
arterial hypertension. The pressor response to hyp-
oxic stimulation is also augmented in young
patients with essential hypertension. Reflex from
arterial chemoreceptors is probably involved in
the pathogenesis of arterial hypertension in ob-
structive sleep apnea syndrome. The episodes of
nocturnal hypoxia during sleep seem to be respon-
sible for an increase in sympathetic activity and
blood pressure.
0022The kidney–kidney reflex inhibits sympathetic
activity, increasing natriuresis and diuresis.
0023The osmoreceptors in the liver and in the digestive
system increase natriuresis and diuresis, decreasing
blood pressure.
0024The disturbance of interaction between the reflex
regulatory mechanisms is discussed as a factor which
may be involved in the pathogenesis of essential
arterial hypertension.
0025Hypertension is a risk factor for atherosclerosis
because high pressure in arteries damages the endo-
thelial lining of the vessels and promotes the forma-
tion of atherosclerotic plaques. Additionally, elevated
arterial pressure increases cardiac afterload.
See also: Atherosclerosis; Enzymes: Functions and
Characteristics; Hypertension: Hypertension and Diet;
Nutrition in the Diabetic Hypertensive; Renal Function
and Disorders: Kidney: Structure and Function
HYPERTENSION/Physiology 3193

Further Reading
Klawe JJ, Tafil-Klawe M, Peter JH and Smietanowski M
(1999) Cardiac response study towards activation and
inactivation of the carotid baroreceptor in obstructive
sleep apnea patients. Medical Science Monitoring 5(3):
449–451.
Narkiewicz K and Somers VK (1997) The sympathetic
nervous system and obstructive sleep apnea: implica-
tions for hypertension. Journal of Hypertension 15:
163–1619.
Person PB (1996) Modulation of cardiovascular control
mechanisms and their interaction. Physiological Review
76: 193–244.
Przybylski J (1981) Do arterial chemoreceptors play a
role in the pathogenesis of hypertension? Medical
Hypotheses 20: 173–177.
Tafil-Klawe M, Raschke F and Hildebrandt G (1990)
Functional asymetry in carotid sinus cardiac reflexes in
humans. European Journal of Applied Physiology and
Occupational Physiology 60: 402–405.
Tafil-Klawe M, Raschke F, Becker H et al. (1991) Investi-
gations of arterial baro- and chemoreflexes in patients
with arterial hypertension. In: Peter JH, Penzel T,
Podszus T and v Wichert P (eds) Sleep and Health
Risk, pp. 319–334. Springer Verlag.
Trzebski A (1992) Arterial chemoreceptor reflex and hyper-
tension. Hypertension 19: 562–566.
Trzebski A, Tafil M, Zoltowski M and Przybylski J (1982)
Increased sensitivity of the arterial chemoreceptor drive
in young men with mild hypertension. Cardiovascular
Research 16: 162–172.
Williams GH (2001) Hypertensive vascular disease. In: Har-
rison’s Principles of Internal Medicine, pp. 1380–1394.
New York: McGraw-Hill Book Company.
Hypertension and Diet
B M Y Cheung and T C Lam, University of Hong Kong,
Pokfulam, Hong Kong
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Nutrition as a Cause of Hypertension
0001 Hypertension is a common condition that affects
more than one-tenth of the adult population. The
complications of untreated hypertension include
stroke, myocardial infarction, cardiac and renal fail-
ure. Its etiology is complex and probably involves the
interaction of genetic predisposition and the environ-
ment in the widest sense. There is familial clustering
of hypertension, which can be a reflection of both
shared genes and shared environment or both. As a
person’s genes is probably not open to modification,
especially when the disease-causing gene(s) have not
been identified, prevention and treatment of hyper-
tension should be targeted at altering the environ-
mental factors. Results from many population and
migrant studies show that environmental factors
play an important role in the occurrence of hyperten-
sion. One such factor determining the development of
hypertension is undoubtedly nutrition. Poor nutri-
tional habits, alcohol consumption, excessive sodium
and insufficient potassium intake are some of the
nutritional factors leading to hypertension. These,
together with socioeconomic status, physical inactiv-
ity, psychological stress, and obesity, influence blood
pressure in an individual.
Fetal Origin of Hypertension
0002Barker and colleagues have put forward the ‘fetal
origins hypothesis’ that links cardiovascular disease
manifested in adulthood to poor nutrition in utero
and infancy. Fetal undernutrition in middle to late
gestation is thought to result in adaptive changes in
fetal growth that predispose to coronary heart dis-
ease. The evidence comes from a longitudinal study of
25 000 middle-aged Britons. Those who were small at
birth and not premature had relatively high rates of
coronary heart disease, hypertension, hypercholester-
olemia, and diabetes. Postnatal nutrition also appears
to influence blood pressure in later life. Premature
babies randomized in a study to breast milk had
lower blood pressure in adolescence than those ran-
domized to formula milk. If the fetal origins hypoth-
esis, which is difficult to prove prospectively, is
correct, optimizing prenatal care may prevent hyper-
tension and other cardiovascular diseases in adult-
hood.
Dietary Pattern and Hypertension
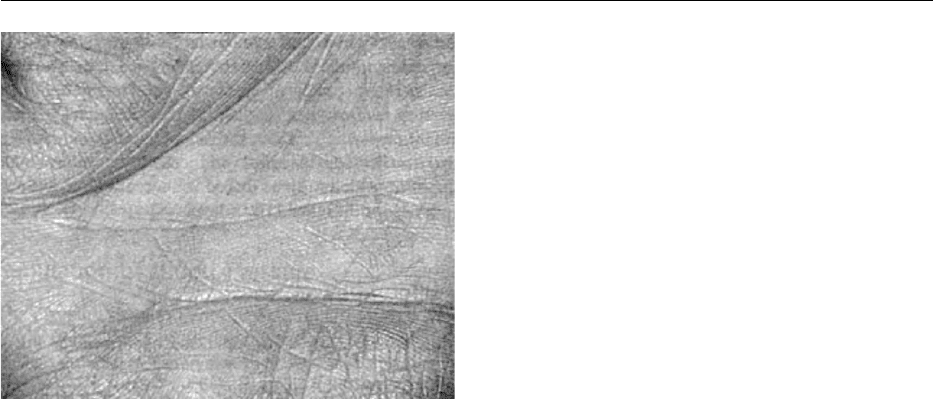
0003There are striking differences in the blood pressure of
populations worldwide. Blood pressure is higher and
rises more steeply with age in industrialized than
in nonindustrialized societies. A predominantly vege-
tarian dietary pattern is generally present in those
populations that have low average blood pressure.
In industrialized countries, vegetarians have lower
blood pressures than nonvegetarians (Figure 1).
0004Epidemiological and intervention studies including
the Multiple Risk Factor Intervention Trial (MRFIT)
suggest a multitude of dietary changes that may
reduce blood pressure. The Dietary Approaches to
Stop Hypertension (DASH) Trial tested three diet-
ary patterns: (1) a control diet that resembled the
average US diet; (2) a combination diet high in fruit,
3194 HYPERTENSION/Hypertension and Diet
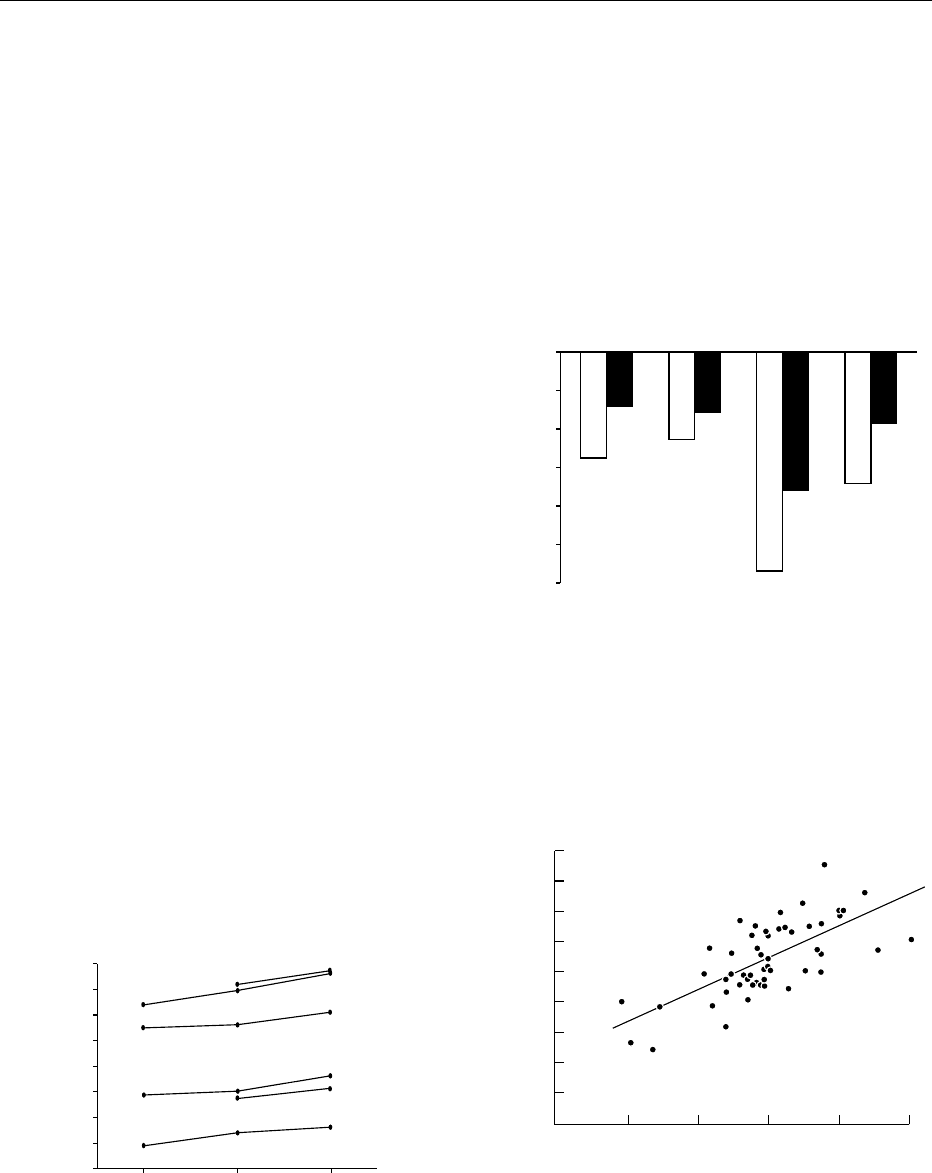
vegetables, whole-grain cereal products, low-fat dairy
products, fish, chicken, and lean meats but low in fat
and cholesterol; and (3) a fruit and vegetables diet
that tested the effects of fruit and vegetables alone
and was similar in other nutrients to the control diet.
Sodium content was the same in all the diets and the
subjects maintained their prestudy body weight
throughout the trial. The combination diet was
found to reduce the systolic pressure by 11 mmHg
and the diastolic pressure by 6 mmHg (Figure 2).
The fruit and vegetables diet reduced blood
pressure by half this amount. Remarkably, the effect
of the combination diet in the hypertensives
approaches the effect of treatment with a single
antihypertensive drug.
Sodium
0005 Sodium is tightly regulated through a variety of
coordinated homeostatic mechanisms involving the
sympathetic nervous system, the renin–angiotensin
system, and natriuretic peptides. A minute rise in
blood pressure is sufficient to augment sodium excre-
tion to achieve sodium balance in normal kidneys. In
salt-sensitive hypertension, there is an exaggerated
blood pressure response to increased sodium intake.
Older patients, overweight type 2 diabetics, or those
of African descent tend to have hypertension of this
type. They have low renin levels and a lesser pressor
response to sodium deprivation. In such hyper-
tensive individuals, sodium restriction is effective
and beneficial. The controversy surrounding salt and
hypertension stems from the fact that not everyone is
salt-sensitive and it has been argued that reducing
the salt intake in the general population is neither
practical nor effective, and may even be harmful to
some people. However, the relationship between salt
and blood pressure is now well established (Figure 3),
and the higher the salt intake of the population, the
steeper the rise in blood pressure with age. Interest-
ingly, in primitive communities, blood pressure does
not rise with age.
0006In many western countries, daily sodium intake
is between 150 and 200 mmol. The Trial Of
16−29
50
60
70
80
90
Strict vegetarian
Systolic
BP
Diastolic
Strict vegetarian
Nonvegetarian
Nonvegetarian
Framingham
Framingham
East Boston
East Boston
100
110
120
130
30−39
Age (years)
40−65
fig0001 Figure 1 Blood pressure (BP) in a strict vegetarian population
in Boston and in nonvegetarian populations in East Boston and
Framingham, MA. Adapted from Sacks FM and Kass EH. Low
blood pressure in vegetarians: effects of specific food and nutri-
ents. American Journal of Clinical Nutrition 48: 795–800, with
permission.
−12
−5.5
−2.8
−4.5
−3.1
−11.4
−7.2
−6.8
−3.6
−10
−8
Change
in
systolic
BP
Clinic
Overall
Hypertensives
clinic
Minority-group
clinicABP
−6
−4
−2
0
fig0002Figure 2 Effect of dietary patterns on blood pressure (BP) in the
Dietary Approaches to Stop Hypertension (DASH) study. ABP,
ambulatory blood pressure. Open columns, combination diet;
filled columns, fruit and vegetable diet. Adapted from Appel LJ,
Moore TJ, Obarzanek E et al. (1997) A clinical trial of the effects
of dietary patterns on blood pressure. DASH Collaborative
Research Group. New England Journal of Medicine 336(16): 1117–
1124, with permission.
0
Adjusted diastolic blood pressure slope with age
(mmHg year
−1
)
Adjusted sodium excretion (mmol 24 h
−1
)
52 centers: b = 0.0021
(SE 0.0003) mmHg year
−1
mmol
−1
sodium*
−0.1
0.0
0.1
0.2
0.3
0.4
0.5
0.6
0.7
50 100 150 200 250
fig0003Figure 3 Cross-center plots of diastolic pressure slope with
age and median sodium excretion and fitted regression lines
for 52 centers, also adjusted for body mass index and alcohol
intake. *P < 0.001. Reproduced from Intersalt Cooperative Re-
search Group (1988). Intersalt: an international study of electro-
lyte excretion and blood pressure: results for 24-hour urinary
sodium and potassium excretion. British Medical Journal 297:
319–328, with permission.
HYPERTENSION/Hypertension and Diet 3195

Nonpharmacological Intervention in the Elderly
(TONE) showed that a 40 mmol day
1
reduction is
accompanied by significant reductions in blood
pressure (5.3/3.4 mmHg). This modest salt restric-
tion can be achieved by not adding salt at the table
and avoiding foods that are high in sodium content
(e.g., preserved food). Saltiness is a rather crude
taste and is used by the industry to enhance the
palatability of food cheaply and to boost the sale
of beverages. Historically, salt was needed to pre-
serve food for the winter months but nowadays,
refrigeration renders this unnecessary. Fresh food is
usually low in salt content and its flavors are better
appreciated when not too much salt has been added
in cooking.
0007 Carefully controlled clinical studies have demon-
strated a dose-dependent relationship between
dietary salt intake and blood pressure, although trials
of salt restriction do not always show a useful re-
duction in blood pressure due to their various trial
designs. Salt restriction is particularly important
when the patient is treated with an angiotensin-
converting enzyme inhibitor (ACEI) or an angiotensin
II antagonist (sartan). The efficacy of these drugs is
diminished in the presence of high salt intake that
suppress the renin–angiotensin system.
Potassium
0008 In contrast to sodium, potassium is less tightly regu-
lated physiologically. In diuretic therapy, the renal
tubules will conserve sodium at the expense of
potassium. Plasma potassium concentration is also
linked to acid–base balance. Nevertheless, potassium
is also closely associated with blood pressure. Cross-
sectional studies in many countries worldwide had
identified an inverse relationship between blood pres-
sure and various measures of serum, urine, total body
and dietary potassium. Low potassium intake may
also underlie the high incidence and prevalence of
hypertension in blacks and the elderly. Potassium
supplementation alone will decrease blood pressure
slightly. The effect is more pronounced in hyperten-
sives than normotensives, in blacks than in whites,
and in those with high sodium intake. In reality,
higher potassium intake is usually associated with a
diet rich in fruit and vegetables. Such a diet will in
itself be conducive to a lower blood pressure, so one
cannot always disentangle the components of a
‘healthy diet’ which are actively antihypertensive.
High sodium intake and low potassium intake is a
common scenario amongst hypertensive patients.
Therefore, sodium and potassium should be con-
sidered jointly in our dietary recommendations.
For example, using a salt substitute that contains
potassium chloride increases potassium intake whilst
reducing sodium intake.
Calcium
0009The relationship between calcium and hypertension
is controversial. Dietary intake of calcium tends
to be lower in hypertensives and calcium supple-
mentation is associated with a modest reduction in
blood pressure. A metaanalysis of 23 observational
studies showed an inverse association between
blood pressure and dietary calcium intake. The effect
size was however small and heterogeneous across
studies. Metaanalysis of randomized trials of calcium
supplementation showed that systolic blood
pressure is reduced by around 1 mmHg. Although it
is possible that certain subgroups may be more sensi-
tive to the effects of calcium, it is certainly not the
major factor in the pathogenesis of hypertension,
despite the recent identification of a parathyroid
hypertensive factor. Therefore, calcium supplementa-
tion, though desirable for other reasons, is not
currently recommended as an efficacious means of
treating hypertension.
Fat
0010The relationship between lipids and coronary heart
disease is now proven beyond doubt by epidemi-
ological studies and large-scale trials of lipid-
lowering drugs (statins) that reduce coronary events.
Reduction in cholesterol by pharmacological means
may not lower blood pressure, but should be viewed
in the context of the overall reduction of cardiovas-
cular risk and the reduction of complications of
hypertension such as myocardial infarction. Hyper-
tension and dyslipidemia are independent cardio-
vascular risk factors and, when they are both present
in the same person, the cardiovascular risk is aug-
mented. Therefore, it makes sense to address both
risk factors. Nonpharmacological means of lipid
lowering through diet and exercise is likely to have
a beneficial effect on blood pressure in addition to
improving the cardiovascular risk profile. The
DASH study suggested that a healthy diet based on
less fat and more fruit and vegetables reduces blood
pressure, although precisely which component of the
DASH diet lowers blood pressure remains to be
elucidated.
0011The effects of saturated, monosaturated, and poly-
unsaturated fatty acids and carbohydrates have been
studied in many clinical trials. Omega-3 unsaturated
fatty acids (fish oils) reduce blood pressure but a large
intake is needed, so this is not a practical treatment
for hypertension.
3196 HYPERTENSION/Hypertension and Diet
Obesity
0012 It has become clear in recent years that obesity is one
of the major determinants of blood pressure. Our
own observations in relatives of hypertensive patients
suggest that the occurrence of hypertension is related
to whether the relative is obese or not. It therefore
appears that those who may be genetically predis-
posed to hypertension will develop the condition if
they become obese.
0013 Recently, two genes involved in the control of body
weight, the OB gene and the OB receptor gene, which
code for the hormone leptin and its receptor respect-
ively, have been described in the mouse. Deletions in
the OB gene or the OB receptor lead to profound
obesity of early onset with excessive food intake,
decreased energy expenditure, and insulin resistance.
In humans, mutations in the corresponding genes
have been reported. A high level of circulating leptin
is found in the majority of obese people, suggesting
that they have leptin resistance. Transgenic mice over-
expressing leptin develop hypertension. However, the
association of high leptin levels and hypertension
has not been firmly established in humans, so the
relevance of these genes to the pathogenesis of essen-
tial hypertension remains to be elucidated.
0014 Obesity, especially abdominal adiposity, is more
closely related to blood pressure than body weight.
Moreover, obesity can lead to insulin resistance
and ultimately overt type 2 diabetes mellitus. Lean,
normoglycemic untreated hypertensive subjects are
more insulin-resistant than comparable normo-
tensive subjects. The relationship between insulin
resistance and hypertension may involve a variety of
mechanisms, including increased sympathetic ner-
vous system activity, proliferation of vascular
smooth-muscle cells, altered cation transport, and
increased sodium retention. It is worth noting than
one-third of diabetics have hypertension and a signifi-
cant proportion of hypertensives have diabetes. The
two conditions overlap to a large extent as compon-
ents of the ‘metabolic syndrome’ or ‘syndrome X.’
0015 Measurement of blood pressure in those who are
obese and have large arms is prone to overestimation
if the cuff is not large enough. Nevertheless, the rela-
tionship between obesity and blood pressure is well
established and indeed, for the overweight hyperten-
sive, losing weight, if it can be achieved, is the most
efficacious means of reducing blood pressure amongst
the various nonpharmacological treatment options.
Our own data and those of other investigators suggest
that for each kilogram of body weight lost, there is
approximately a 1 mmHg reduction in diastolic blood
pressure and a 2 mmHg reduction in systolic blood
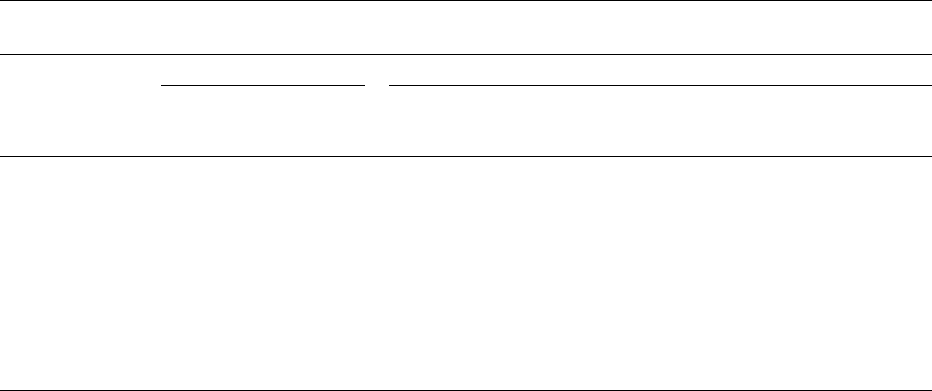
pressure (Figure 4). Unfortunately, outside clinical
trials, this is easier said than done. A coordinated
approach involving a physician, nurse, and dietitian
and attendance of classes is probably more effective
than advice from a single professional. As with
other nonpharmacological measures, weight control
through diet and exercise will lead to benefits in
addition to blood pressure control, such as a better
lipid profile, better cardiovascular fitness, less stress
on the joints, and so on.
Alcohol
0016The effect of alcohol on health in general and cardio-
vascular diseases in particular is dose-dependent. A
modest regular intake is probably beneficial because
of the increase in high-density lipoprotein cholesterol
(HDL-C) and the relief of stress whilst a high intake is
definitely harmful. With increasing levels of alcohol
intake, more than 50 epidemiological studies from a
variety of cultures have reported an increase in blood
pressure or a higher prevalence of hypertension. An
excessive alcohol intake raises blood pressure and
moderation of alcohol intake leads to reduction in
blood pressure (Table 1). In practice, hypertensive
patients who do not drink alcohol should not be
encouraged to start doing so whilst those who do
drink large quantities must be encouraged to reduce
Wei
g
ht (k
g
)
DBP (mmHg)
50
70
60 70 80 90 100
75
80
85
90
95
100
105
110
fig0004Figure 4 The effect of weight reduction on diastolic blood pres-
sure (DBP). (^) MacMahon et al. (1985) Lancet 1: 1233–1236; (&)
Gordon et al. (1997) American Journal of Cardiology 79: 763–767;
(m) Singh et al. (1995) Journal of Human Hypertension 9: 355–362;
() Jalkanen et al. Scandinavian Journal of Social Medicine 19: 66–
71; (
*
) Singh et al. (1990) Nutrition 6: 297–302; () Wassertheil-
Smoller S et al. (1992) The Trial of Antihypertensive Interventions
and Management (TAIM) study. Archives of Internal Medicine
152(1): 131–136; (|) Darne et al. (1993) Blood Pressure 2: 130–135;
(s) Haynes et al. (1984) Journal of Hypertension 2: 535–539; (n)
Fagerberg et al. (1989) British Medical Journal 299: 480–485; (^)
Andersson et al. (1991) Hypertension 18: 783–789.
HYPERTENSION/Hypertension and Diet 3197
their intake to the recommended levels. Currently, it
is believed that men should not drink more than 21
units per week and women should not drink more
than 14 units per week. Approximately one unit of
alcohol, or 14 g ethanol, is contained in one glass
of table wine.
Dietary Approach to Prevent or Treat
Hypertension
0017 Alteration of the diet to bring about a lower
blood pressure is not only beneficial in those who
are hypertensive, but is prudent in those who are not
yet hypertensive and even in those who are normo-
tensive. A shift in the distribution of the blood pres-
sures to a lower mean for the population is expected
to lead to a massive reduction in the incidence of
coronary heart disease and stroke. Achieving a
healthier diet will delay or even prevent the onset of
hypertension. This may be especially relevant in
young people who have a strong family history of
hypertension or cardiovascular diseases. In those
who have newly diagnosed hypertension, dietary
intervention may obviate the need for drug therapy.
In patients with mild hypertension who respond to
diet and the nonpharmacological approach, cessation
of therapy may be possible. In those hypertensive
patients who still require drug therapy, an appropri-
ate diet will reduce the intensity of treatment and
facilitate blood pressure control.
0018 There is no single diet that will fit everyone’s
needs. The elderly might be more responsive to salt
restriction whilst the young obese hypertensive
should have a diet low in fat and calories. Clinicians
rarely have the time or the training to go through a
diet with the patient so the help of dietitians and other
health care professionals is crucial for successful
implementation of dietary intervention.
0019Although most of the dietary recommendations are
well accepted by health care professionals and the
community, their implementation is a major problem
since a change in behavior is needed. Eating and alco-
hol drinking are normally pleasurable experiences
and many do not find regular exercise enjoyable, so
diet, abstinence, and exercise require determination
and commitment. There is a limit as to how much
health care professionals can do in this regard. It is
therefore important that the doctor, nurse, and
dietitian complement each other and reinforce the
message in a team approach.
0020There is another obstacle to a healthy diet: food
sold in fast-food outlets is convenient, inexpensive,
and therefore popular. Such food is high in salt and fat
content and is generally not fresh. Tinned and other
preserved food has a high salt content; McGregor has
argued that reducing the salt intake in the general
population requires the cooperation of the food
industry to reduce the salt content in its products.
Health care professionals need to be aware of the
economical and social aspects in order to give advice
that can feasibly be followed. In developing countries,
the highest incidence of hypertension is found in
people with high socioeconomic status. As countries
become more affluent, hypertension becomes more
prevalent in the lower socioeconomic classes. In
developed countries, there is an inverse relationship
between socioeconomic status and blood pressure.
Proposed mechanisms include differences in diet
(sodium, potassium, calories), physical activity, body
mass, alcohol intake, psychosocial stress, and access
tbl0001 Table 1 Randomized controlled trials of the effects of alcohol reduction on blood pressure (BP)
Study, year Studypopulation Studyresults
n Age (years)
(mean + SD or range)
Duration
(weeks)
Baseline
BP
(mm Hg)
Alcoholintake
difference
(drinks
a
perday)
BP difference
(mm Hg)
P
Puddey, 1985 46 35+8 6 133/76 3.7 3.8/1.4 <0.001/<0.05
Howes, 1985 10 25–41 0.6 120/66 5.7 8/6 <0.025/<0.001
Puddey, 1987 44 53+16 6 142/84 4.0 5/3 <0.001/<0.001
Ueshima, 1987 50 46+7 2 148/93 2.6 5.2/2.2 <0.005/NS
Wallace, 1988 641 42+20 52 136/82 1.0 2.1/? <0.05/NS
Parker, 1990 59 52+11 4 138/85 3.8 5.4/3.2 <0.01/0.01
Cox, 1990 72 20–45 4 132/73 3.4 4.1/1.6 <0.05/<0.05
Maheswaran, 1992 41 40s 8 144/90 3.1 Not reported NS
Puddey, 1992 86 44 18 137/85 3.0 4.8/3.3 <0.01/<0.01
Ueshima, 1993 54 44+8 3 144/96 1.7 3.6/1.9 <0.05/NS
PATHS, 1998 641 57+11 104 140/86 1.3 0.9/0.6 0.16/0.10
a
A standard drink is defined as 14 g ethanol and is contained in a 12-oz/350 ml glass of beer, a 5-oz/146 ml glass of table wine, or 1.5/44 ml oz of distilled
spirits.
3198 HYPERTENSION/Hypertension and Diet
