Pendergast T., Pendergast S. St. James Encyclopedia of Popular Culture. Volume 1: A-D
Подождите немного. Документ загружается.


BIRTH OF A NATIONENCYCLOPEDIA OF POPULAR CULTURE
259
Scene from the film The Birth of a Nation.
between the States. It hasn’t been told accurately in history books.’’
When the film was being shot at a lot on Sunset Boulevard in Los
Angeles, the first-time-ever use of artificial lighting to illuminate
battle scenes shot at night led to public fears that southern California
was under enemy attack from the sea.
Although some scenes depicted the early arrival of slaves in
America, the decades of the 1860s and 1870s—Civil War and
Reconstruction—constitute the historical timeframe of The Birth of a
Nation. The film includes enactments of several historical scenes,
such as Sherman’s march to the sea, the surrender at Appomattox, and
the assassination of Lincoln, but the narrative focuses almost exclu-
sively on the saga of two white dynasties, the Stonemans from the
North and the Camerons from the South, interlinked by romantic
attachments between the younger generations of the two families. An
early scene depicts the Cameron plantation in South Carolina as an
idyllic estate with benevolent white masters and happy slaves coexisting
in mutual harmony until undermined by abolitionists, Union troops,
and Yankee carpetbaggers. After the war, Austin Stoneman, the
family patriarch, dispatches a friend of mixed-race, Silas Lynch, to
abet the empowerment of ex-slaves by encouraging them to vote and
run for public office in the former Confederacy. A horrified Ben
Cameron organizes the Ku Klux Klan as an engine of white resist-
ance. The film’s unflattering depiction of uncouth African American
legislators and of Lynch’s attempt to coax Elsie Stoneman into a
mixed-race marriage fueled much controversy over the years for
reinforcing stereotypes about Negro men vis-à-vis the ‘‘flower of
Southern womanhood.’’ To create dramatic tension, Griffith juxta-
posed images of domestic bliss with unruly black mobs and used
alternating close-up and panoramic scenes to give a sense of move-
ment and to facilitate the emotional unfolding of the narrative. During
a climactic scene in which the Ku Klux Klan rides to the rescue of the
Cameron patriarch from his militant black captors, a title reads: ‘‘The
former enemies of North and South are united again in common
defense of their Aryan birthright.’’ Bowing to protests, Griffith
excised some of the more graphic scenes of anti-white violence before
the film’s premiere, and also added an epilogue, now lost, favorably
portraying the Hampton Institute, a prominent black school in Virgin-
ia. Interviewed by his biographer, Barnet Bravermann in 1941, D. W.
Griffith thought that The Birth of a Nation should, ‘‘in its present form
be withheld from public exhibition’’ and shown only to film profes-
sionals and students. Griffith said ‘‘If The Birth of a Nation were done
again, it would have to be made much clearer.’’
BIRTHING PRACTICES ENCYCLOPEDIA OF POPULAR CULTURE
260
The title of the film remained The Clansman until a month
before its premiere, and was altered to its familiar title upon Dixon’s
own enthusiastic recommendation. Both Griffith and Dixon defended
their work against an avalanche of censorship threats, as in a letter by
Dixon to the Boston Journal (April 26, 1915), in which he wrote
‘‘This play was not written to stir race hatred. It is the faithful record
of the life of fifty years ago. It is no reflection on the cultured, decent
negro of today. In it are sketched good negroes and bad negroes, good
whites and bad whites.’’ Griffith also ardently defended his view-
point, as in a letter to the New York Globe (April 10, 1915) in which he
criticized ‘‘pro-intermarriage’’ groups like the NAACP for trying ‘‘to
suppress a production which was brought forth to reveal the beautiful
possibilities of the art of motion pictures and to tell a story which is
based upon truth in every vital detail.’’
The Birth of a Nation had its premiere at New York City’s
Liberty Theater on March 3, 1915, to critical and popular acclaim,
though the NAACP and other groups organized major protests and
violence broke out in Boston and other cities. Booker T. Washington
refused to let Griffith make a film about his Tuskegee Institute
because he did not want to be associated with the makers of a
‘‘hurtful, vicious play.’’ W. E. B. Du Bois adopted a more proactive
stance, urging members of his race to create films and works of art
that would depict its own history in a positive light. But response in
the mainstream press was generally favorable. Critic Mark Vance
boasted in the March 12 issue of Variety how a film ‘‘laid, played, and
made in America’’ marked ‘‘a great epoch in picturemaking’’ that
would have universal appeal. Reviews in the southern papers were
predictably partisan. A critic for the Atlanta Journal, Ward Greene,
obviously inspired by scenes of triumphant Klan riders, crowed that
Griffith’s film ‘‘is the awakener of every feeling . . . Loathing,
disgust, hate envelope you, hot blood cries for vengeance . . . [you
are] mellowed into a deeper and purer understanding of the fires
through which your forefathers battled to make this South of yours a
nation reborn!’’ Over the years, The Birth of a Nation was used as a
propaganda film both by the film’s supporters and detractors. Film
historian John Hope Franklin remarked to a 1994 Library of Congress
panel discussion that the film was used by a resurgent Ku Klux Klan
as a recruiting device from the 1920s onward, a point supported by
other historians, though disputed by Thomas Cripps, author of several
scholarly works on black cinema.
Despite the continuing controversy over the depiction of interra-
cial conflict, The Birth of a Nation remains a landmark film in the
history of world cinema and its director an important pioneer in the
film medium. Writer James Agee, in a rhapsodic defense of Griffith,
wrote of him in a 1971 essay: ‘‘He achieved what no other known man
has ever achieved. To watch his work is like being witness to the
beginning of melody, or the first conscious use of the lever or the
wheel. . . .’’ The Birth of a Nation, continued Agee, was a collection
of ‘‘tremendous magical images’’ that equaled ‘‘Brady’s photo-
graphs, Lincoln’s speeches, and Whitman’s war poems’’ in evoking a
true and dramatic representation of the Civil War era.
—Edward Moran
F
URTHER READING:
Barry, Iris. D.W. Griffith: American Film Master. New York, Muse-
um of Modern Art, 1965.
Gish, Lillian, with Ann Pinchot. The Movies, Mr. Griffith, and Me.
Englewood Cliffs, New Jersey, Prentice Hall, 1969.
Grimes, William. ‘‘An Effort to Classify a Racist Classic.’’ New York
Times. April 27, 1994.
Phillips, Mike. ‘‘White Lies.’’ Sight & Sound. June 1994.
Silva, Fred, editor. Focus on ‘‘The Birth of a Nation.’’ Englewood
Cliffs, Prentice Hall, 1971.
Sarris, Andrew. ‘‘Birth of a Nation or White Power Back When.’’
Village Voice. July 17 and July 24, 1969.
Stanhope, Selwyn. ‘‘The World’s Master Picture Producer.’’ The
Photoplay Magazine. January 1915, 57-62.
Birthing Practices
Historically speaking, an overview of changing practices of
childbirth offers an overview of the changing dynamics of gender and
the increasing authority of professional medicine, particularly in the
United States and Western Europe. As midwives began to be ‘‘phased
out’’ in the late eighteenth century, they were replaced by male
doctors, and birthing practices changed as a result. Increasing medi-
cal knowledge and experience reinforced this shift, eventually
pathologizing pregnancy and childbirth and tying childbirth to a
hospital environment. In the late twentieth century, however, many
women began calling for a return to the earlier, less medicalized,
models of childbirth, and the debate about the costs and benefits of
various birthing practices continues to develop today.
In colonial America, deliveries were attended by midwives as a
matter of course. These women drew upon years of experience, often
passing their knowledge from one generation to the next, and general-
ly attending hundreds of childbirths during their careers. In some
cases, a midwife might call a ‘‘barber-surgeon’’ to assist with a
particularly difficult case (though often the surgeon’s skills were no
better than the midwife’s, and the patient and child were lost), but for
the most part women (mothers and midwives) controlled the birthing
process. With the rise in medical schools, however, and the teaching
of obstetrics as the first specialty in eighteenth-century Ameri-
can medical schools, medical doctors began to assume control
over childbirth.
Beginning in the 1830s, having a medical doctor in attendance at
a birth became a sign of social prestige—middle- and upper-class
women could afford to call in a doctor and did so more out of a desire
to display their economic and political clout than out of medical
necessity. Class pressures ensured that women would choose child-
birth assistance from someone of their own class (that is, a medical
doctor for the middle and upper classes, a midwife for working
classes). These pressures also meant that crusades to persuade mid-
dle- and upper-class women that they ‘‘deserved’’ physicians, that no
precaution was too great, and so on, were enormously effective in
shifting public opinion toward the presumed superiority of medical
doctors. As this kind of social pressure continued to spread through-
out the Victorian era, lay practitioners lost more and more status, and
medical doctors gained more and more control. Furthermore, the
systematic exclusion of women from the medical profession, particu-
larly during the nineteenth century, ensured that women themselves
began losing control of childbirth, giving it up to the increasing
authority of the male medical community.
Throughout the 1800s, doctors employed medical privilege to
protect their professional status from the economic and social threat

BIRTHING PRACTICESENCYCLOPEDIA OF POPULAR CULTURE
261
of midwives who lacked formal training. The Boston Women’s
Health Collective asserts that nineteenth-century physicians ‘‘waged
a virulent campaign against midwives, stereotyping them as ignorant,
dirty, and irresponsible. Physicians deliberately lied about midwifery
outcomes to convince legislators that states should outlaw it.’’ These
strategies, coupled with the significant risks of childbirth (infant and
maternal mortality rates remained high throughout the nineteenth
century), helped to create a climate of fear surrounding pregnancy and
birth. Rather than seeing childbirth as a natural practice, people began
to see it as a medical emergency, one that should be relinquished to a
physician’s control.
Once childbirth had been pathologized, the door was opened to
begin moving women in labor out of their homes and into hospitals
where, according to the medical community, the ‘‘disease of child-
birth’’ could best be battled. Until the beginning of the twentieth
century, it was actually a stigma to have to give birth in a maternity
ward, which had generally been reserved for the poor, immigrants,
and unmarried girls. As better strategies were developed to prevent
disease (especially deadly outbreaks of puerperal fever that had
flourished in hospitals throughout the nineteenth century), the hospi-
tal birth, with its concomitant costs, was recast as a status symbol.
Eventually, however, having babies in hospitals became a matter of
course. According to Jessica Mitford, while only 5 percent of babies
were born in hospitals in 1900, 75 percent were born in hospitals in
1935, and by the late 1960s, 95 percent of babies were born in
hospitals. Eakins’ American Way of Birth notes, ‘‘the relocation of
obstetric care to the hospital provided the degree of control over both
reproduction and women that would-be obstetricians needed in their
ascent to professionalized power.’’ This power was consolidated
through non-medical channels, with advice columns, media attention,
popular books, and community pressure working to reinforce the
primacy of the professional medical community in managing wom-
en’s childbirth experiences.
In the twentieth century, giving birth in a hospital environment
has meant a loss of control for the mother as she becomes subject to
numerous, standardized medical protocols; throughout her pregnan-
cy, in fact, she will have been measured against statistics and fit into
frameworks (low-risk vs. high-risk pregnancy; normal vs. abnormal
pregnancy, and so on). As a result, the modern childbirth experience
seems to depersonalize the mother, fitting her instead into a set of
patient ‘‘guidelines.’’ Women in labor enter alongside the ill, the
injured, and the dying. Throughout most of the twentieth century,
women were anesthetized as well, essentially being absent from their
own birthing experience; fathers were forced to be absent as well,
waiting for the announcement of his child’s arrival in a hospital
waiting room. If a woman’s labor is judged to be progressing ‘‘too
slowly’’ (a decision the doctor, rather than the mother, usually
makes), she will find herself under the influence of artificial practices
designed to speed up the process. More often than not, her pubic area
will be shaved (a procedure that is essentially pointless) and some-
times cut (in an episiotomy) by medical personnel anxious to control
the labor process. Further advances in medical technology, including
usage of various technological devices and the rise in caesarian
sections (Mitford cites rates as high as 30 percent in some hospitals),
have also contributed to a climate of medicalization and fear for many
women giving birth. This is not to say, of course, that many of these
medical changes, including improved anesthetics (such as epidurals)
and improved strategies for difficult birthing situations (breech births,
fetal distress, etc.) have not been significant advances for women and
their babies. But others argue that many of these changes have been
for the doctors’ convenience: delivering a baby while lying on one’s
back with one’s feet in stirrups is surely designed for the obstetri-
cian’s convenience, and the rise in caesarian sections has often been
linked to doctors’ preferences rather than the mothers’.
In the 1960s and 1970s, as a result of their dissatisfaction with
the medical establishment and with the rising cost of medical care,
various groups began encouraging a return to older attitudes toward
childbirth, a renewal of approaches that treat birthing as a natural
process requiring minimal (if any) medical intervention. One of the
first steps toward shifting the birthing experience away from the
control of the medical establishment involved the introduction of
childbirth classes for expectant parents. These courses often stress
strategies for dealing with the medical community, for taking control
of the birthing process, and for maintaining a ‘‘natural childbirth’’
experience through education; the most famous methods of natural
childbirth are based on work by Grantly Dick-Read (Childbirth
Without Fear), Fernand Lamaze, and Robert Bradley.
Also significant were various feminist critiques of the standard
birth practices. The publication of the Boston Women’s Health
Collective’s Our Bodies, Ourselves in 1984 offered a resource to
women who wanted to investigate what had been essentially ‘‘under-
ground’’ alternatives to the medicalized childbirth experience. Through
this work (and others), women learned how to question their doctors
more assertively about the doctors’ practices, to file ‘‘birth plans’’
(which set out the mother’s wishes for the birth), and to find networks
of like-minded parents, midwives, and doctors who can assist in
homebirths, underwater births, and other childbirth techniques. In
some states, midwives not attached to hospitals are still outlaws, and
groups continue to campaign to change that fact.
Finally, many hospitals are recognizing women’s desire to move
away from the dehumanizing and pathological approaches to child-
birth associated with the professional medical community. In defer-
ence to these desires (or, more cynically, in deference to their
financial bottom lines), some hospitals have built ‘‘Birthing Cen-
ters,’’ semi-detached facilities dedicated specifically to treating child-
birth as a natural process. Women enter the Birthing Center, rather
than the hospital. There they are encouraged to remain mobile, to have
family and friends in attendance, and to maintain some measure of
control over their bodies. Often patient rooms are designed to look
‘‘homey,’’ and women (without complications) give birth in their
own room, rather than in an operating theater. Many of these facilities
employ Nurse Midwives, women and men who have been trained as
nurses in the traditional medical establishment but who are dedicated
to demedicalizing the childbirth practice while still offering the
security of a hospital environment.
As women and men continue to demand that childbirth be
recognized as a natural, rather than unnatural, process, the dominant
birthing practices will continue to shift. Additionally, rising pressures
from the insurance industry to decrease costs are also likely to
contribute to a decrease in the medical surveillance of childbirth—
already new mothers’ hospital stays have been drastically reduced in
length as a cost-cutting measure. Clearly the move in recent years has
meant a gradual return to earlier models of childbirth with a return of
control to the mother and child at the center of the process.
—Deborah M. Mix
F
URTHER READING:
Boston Women’s Health Collective. The New Our Bodies, Ourselves,
Updated for the 90s. New York, Simon and Schuster, 1992.
BLACK ENCYCLOPEDIA OF POPULAR CULTURE
262
Eakins, Pamela S., editor. The American Way of Birth. Philadelphia,
Temple University Press, 1986.
Mitford, Jessica. The American Way of Birth. New York, Dutton, 1992.
Black, Clint (1962—)
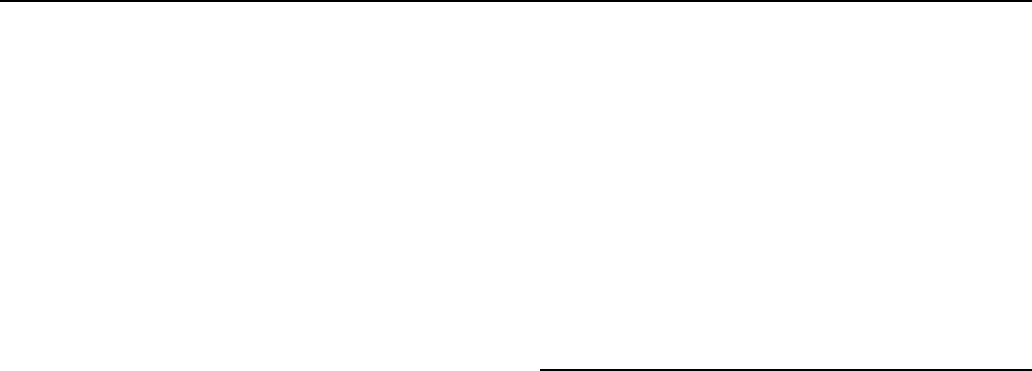
Since the release of his first album in 1989, Clint Black has
become one of country music’s biggest stars. He is also one of the
most prominent symbols of country’s revival in the 1980s and 1990s.
It was in the mid-1980s that country music had been written off as
dead. In 1985, The New York Times reported that this once mighty
genre had fallen off the edge of the American entertainment table and
it would never regain such stature with its audience. A year later, the
same newspaper reversed itself in an article hailing the new creative
and commercial vitality of country music, as traditionalists like
Randy Travis and young iconoclasts like Steve Earle brought new life
into old forms. That, however, was nothing compared to what was just
around the corner. Country was about to be taken over by a new
Clint Black
generation of heartthrobs in cowboy hats who were going to capture
the imagination of the American public to a degree hitherto unimagined.
Part of country music’s revival was due to the creative ground-
work that was laid for newcomers in the adventurous creativity of the
mid-1980s. Angry song-writing geniuses like Earle, quirky originals
like Lyle Lovett, and musical innovators like the O’Kanes all played a
part in paving the way for young new artists. Interestingly, the
aggressive urban anger of black music in the 1980s also influenced
the country scene. Rap drove a lot of middle class whites to a music
they could understand, and country radio was playing it. The audience
for pop music was also growing older and, in the 1980s, for the first
time, a generation over thirty-five continued to buy pop music.
Although the children of these suburban middle-class consumers
were buying rap, their parents were looking for the singer-songwriters
of their youth—the new Dan Fogelbergs and James Taylors—and
they found them wearing cowboy hats.
The country superheroes of the 1980s and 1990s were a new
breed indeed. They did not have the down-home background of Lefty
Frizzell, Porter Wagoner, or Johnny Cash, but they did have their own
skills that would help them succeed in the music industry. Garth
Brooks was a marketing major in college, and he knew how to market
himself; Dwight Yoakam was a theater major, and he knew how to
invent himself onstage; and Lyle Lovett’s day job at the time he
signed his first recording contract was helping his mother run high-
level business management training seminars.
Clint Black, who arrived on the scene in 1989, was a ‘‘folkie’’
from the suburbs of Houston. His father advised him against going
into country music precisely because he did not think he was country
enough. ‘‘Stick to doing other folks’ songs,’’ he advised. ‘‘Real
country songwriters, like Harlan Howard. Don’t try to write your
own. You haven’t done enough living—shooting pool, drinking beer,
getting into fights—to write a real country song.’’ Black’s ‘‘Noth-
ing’s News,’’ which graced his first album, was an answer to his
father and to all those other good old boys who ‘‘Spent a lifetime . . .
Down at Ernie’s icehouse liftin’ longnecks to that good old country
sound,’’ only to discover ultimately that they had ‘‘worn out the same
old lines, and now it seems that nothin’s news ....’’
The 1980s were a time when the rock influence hit country with a
vengeance. Rock acts like Exile and Sawyer Brown became country
acts. Country radio adopted the tight playlists of pop radio. Record
company executives from Los Angeles and New York started moving
into the little frame houses that served as office buildings on Nash-
ville’s Music Row. And even among the neo-traditional acts, rock
music management techniques became the norm. Clint Black’s career
blossomed under the managerial guidance of Bill Ham, who had
made his reputation guiding ZZ Top’s fortunes. Black’s first album,
Killin’ Time, became the first debut album ever, in any genre, to place
five singles at number one on the charts.
For many country artists, country superstardom seems to almost
automatically raise the question, ‘‘Now what?’’ For Black, marriage
was the answer to that question. He married Hollywood television star
Lisa Hartman (Knots Landing) in 1991 and their marriage has lasted.
It has also garnered him a certain amount of gossip column celebrity
beyond the country circuit. Although Black also has a movie role in
Maverick to his credit, his reputation rests solidly on what he does
best: writing and singing country songs. Black seems to have settled
in for the long haul.
—Tad Richards
BLACK MASKENCYCLOPEDIA OF POPULAR CULTURE
263
FURTHER READING:
Brown, C. D. Clint Black: A Better Man. New York, Simon &
Schuster, 1993.
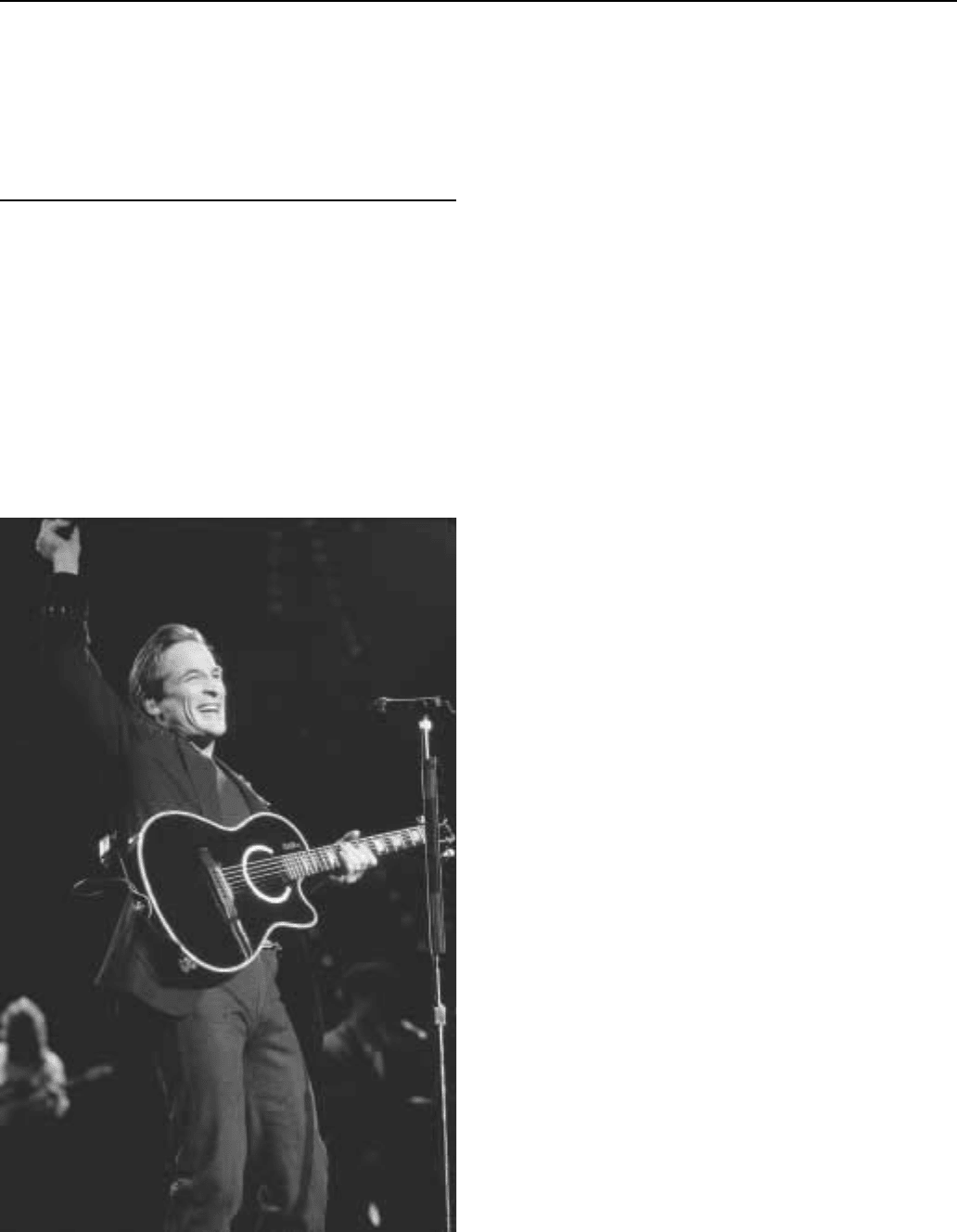
Black Mask
One of the most important detective fiction magazines of the
twentieth century, Black Mask began early in 1920 and introduced
and developed the concept of the tough private eye. It also promoted,
and in some cases introduced, the work of such writers as Dashiell
Hammett, Raymond Chandler, Erle Stanley Gardner, and John D.
MacDonald. Hammett’s The Dain Curse, Red Harvest, The Glass
Key, and The Maltese Falcon all appeared originally as serials in the
magazine and Chandler sold his first detective story to Black Mask. In
its over 300 issues the pulp showcased the work of dozens of other
writers. Though many are forgotten today, such contributors as
Frederick Nebel, Norbert Davis, W.T. Ballard, John K. Butler, Raoul
Whitfield, Carroll John Daly, Horace McCoy, Lester Dent, and
William Campbell Gault all helped shape and define the hardboiled
school of mystery writing.
Early in 1919, H. L. Mencken, literary man and dedicated
iconoclast, wrote a letter to a friend. ‘‘I am thinking of venturing into a
new cheap magazine,’’ he explained. ‘‘The opportunity is good and I
need the money.’’ Mencken and his partner, theater critic George Jean
Nathan, required funds to keep their magazine The Smart Set afloat.
He considered that a quality publication, but in his view the new one
that he and Nathan launched early in 1920 was ‘‘a lousy magazine’’
that would cause them nothing but ‘‘disagreeable work.’’ Their new
publication was christened The Black Mask and featured mystery
stories. Pretty much in the vein of Street & Smith’s pioneering
Detective Story pulp, the early issues offered very sedate, and often
British, detective yarns. Nathan and Mencken soon sold out, leaving
the magazine in other hands.
Then in 1923 two beginning writers started submitting stories
about a new kind of detective. Carroll John Daly, a onetime motion
picture projectionist and theater manager from New Jersey, intro-
duced a series about a tough, gun-toting private investigator named
Race Williams. Written in a clumsy, slangy first person, they recount-
ed Williams’ adventures in a nightmare urban world full of gangsters,
crooked cops, and dames you could not trust. Williams explained
himself and his mission this way—‘‘The papers are either roasting me
for shooting down some minor criminals or praising me for gunning
out the big shots. But when you’re hunting the top guy, you have to
kick aside—or shoot aside—the gunmen he hires. You can’t make
hamburger without grinding up a little meat.’’ This tough, humorless
metropolitan cowboy became extremely popular with the magazine’s
readers, who were obviously tired of the cozy crime stories that the
early Black Mask had depended on. For all his flaws, Race Williams is
acknowledged by most critics and historians to be the first hardboiled
detective, and the prototype for others to follow.
Unlike Daly, Dashiell Hammett knew what he was talking
about. He had been a private investigator himself, having put in
several years with the Pinkerton Agency. Exactly four months after
the advent of Race Williams, Hammett sold his first story about the
‘‘Continental Op(erative)’’ to the magazine. Titled ‘‘Arson Plus,’’ it
introduced the plump middle-aged operative who worked out of the
San Francisco office of the Continental Detective Agency. Although
also in the first person, the Op stories were written in a terse and
Various covers of Black Mask.
believable vernacular style that made them sound real. Hammett’s
private detective never had to brag about being tough and good with a
gun; readers could see that he was. His nameless operative soon
became Race Williams’ chief rival and after he had written nearly two
dozen stories and novellas about him, Hammett put him into a novel.
The first installment of Red Harvest appeared in the November 1927
issue of Black Mask. In November of the next year came the second
Op serial, The Dain Curse. Then in 1929 Hammett introduced a new
San Francisco private eye, a pragmatic tough guy he described as
resembling a blond Satan. The Maltese Falcon, told in the third
person, introduced Sam Spade and the quest for the jewel-encrusted
bird. The story quickly moved into hardcovers, movies, and interna-
tional renown. Hammett’s The Glass Key ran in the magazine in 1930
and his final Op story in the November issue of that year. With the
exception of The Thin Man, written initially for Redbook in the early
1930s, everything that Hammett is remembered for was published in
Black Mask over a period of less than ten years.
Joseph Shaw was usually called Cap Shaw, because of his Army
rank during World War I. Not at all familiar with pulp fiction or Black
Mask when he took over as editor in 1926, he soon educated himself
on the field. Shaw never much liked Daly’s work, but kept him in the
magazine because of his appeal to readers. Hammett, however, was
an exceptional writer and Shaw used him to build the magazine into
an important and influential one. ‘‘Hammett was the leader in the
thought that finally brought the magazine its distinctive form,’’ Shaw
explained some years later. ‘‘Without that it was and would still have
been just another magazine. Hammett began to set character before
situation, and led some others along that path.’’ In addition to
BLACK PANTHERS ENCYCLOPEDIA OF POPULAR CULTURE
264
concentrating on character, one of the goals of the best Black Mask
authors was to develop prose that sounded the way people talked and
not the way writers wrote. In addition to Hammett, Cap Shaw
encouraged other writers who had already been contributors when he
joined as editor. Among them were Erle Stanley Gardner, Raoul
Whitfield, and Frederick Nebel. He asked Nebel to create a new
hardboiled private eye and the result was, as a blurb called him, ‘‘an
iron-nerved private dick’’ named Donahue. One of the things he got
from Whitfield was a serial titled ‘‘Death in a Bowl,’’ which
introduced Ben Jardinn, the very first Hollywood private eye. In
1933, Shaw bought ‘‘Blackmailers Don’t Shoot’’ from Raymond
Chandler, a failed middle-aged business man who was hoping he
could add to his income by writing pulpwood fiction. The tough and
articulate private eye Chandler wrote about for Black Mask, and later
for its rival Dime Detective, was called Mallory and then John
Dalmas. When he finally showed up in the novel The Big Sleep in
1939, he had changed his name to Philip Marlowe. Among the many
other writers Shaw introduced to Black Mask were Horace McCoy,
Paul Cain, Lester Dent, and George Harmon Coxe.
After Shaw quit the magazine in 1936 over a salary dispute, it
changed somewhat. Chandler moved over to Dime Detective, where
Nebel had already been lured, and the stories were not quite as
‘‘hardboiled’’ anymore. New writers were recruited by a succession
of editors. Max Brand, Steve Fisher, Cornell Woolrich, and Frank
Gruber became cover names in the later 1930s. Black Mask was
bought out by Popular Publications in 1940 and started looking
exactly like Popular’s Dime Detective. Kenneth S. White became the
editor of both and put even more emphasis on series characters.
Oldtime contributors such as H.H. Stinson and Norbert Davis provide
recurring detectives, as did newcomers like Merle Constiner, D.L.
Champion, and Robert Reeves. Later on John D. MacDonald, Richard
Demming, and William Campbell Gault made frequent appearances.
The decade of the 1950s saw the decline and fall of all the pulp
fiction magazines. Black Mask ceased to be after its July 1951 issue.
By then, it was a smaller-sized magazine that included reprints from
earlier years with few new detective tales. Attempts to revive it in the
1970s and the 1980s were unsuccessful.
—Ron Goulart
F
URTHER READING:
Cook, Michael L., editor. Mystery, Detective, and Espionage Maga-
zines. Westport, Greenwood Press, 1983.
Goulart, Ron. The Dime Detective. New York, Mysterious Press, 1988.
Sampson, Robert. Yesterday’s Faces. Bowling Green, Ohio, Bowling
Green State University Popular Press, 1987.
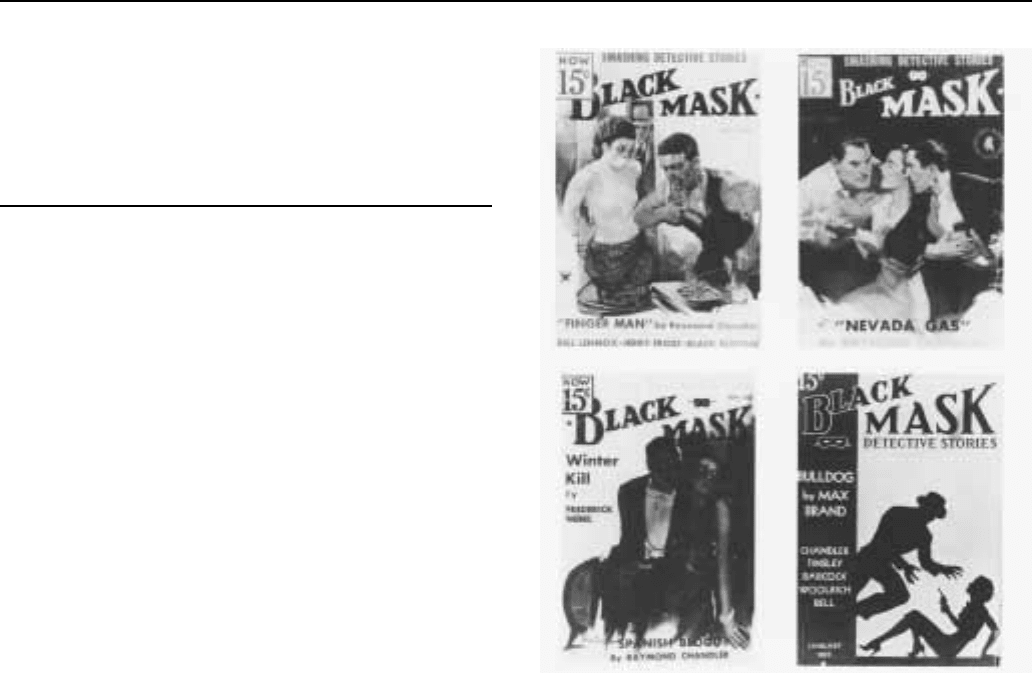
Black Panthers
The Black Panther Party (BPP) came to represent the West Coast
manifestation of Black Power as well as the angry mood within urban
African American communities in the 1960s. The groups main
influences were Malcolm X, especially after his 1964 break from the
Nation of Islam, and Robert F. Williams, the then Cuban-based civil
rights leader and advocate of armed self-defense. Philosophically, the
Black Panthers (from left): 2nd Lt. James Pelser, Capt. Jerry James, 1st
Lt. Greg Criner and 1st Lt. Robert Reynolds.
organization was rooted in an eclectic blend of Marxist-Leninism,
black nationalism, and in the revolutionary movements of Africa
and Asia.
The BPP was founded in October 1966 by Huey Newton and
Bobby Seale, two young black college students in Oakland, Califor-
nia. The name of the organization was taken from the Lowndes
County Freedom Organization, which had used the symbol and name
for organizing in the rural black belt of Alabama in 1965. The BPP
was initially created to expand Newton and Seale’s political activity,
particularly ‘‘patrolling the pigs’’—that is, monitoring police activi-
ties in black communities to ensure that civil rights were respected.
Tactically, the BPP advocated ‘‘picking up the gun’’ as a means
to achieve liberation for African Americans. Early on, Newton and
Seale earned money to purchase guns by selling copies of Mao Tse-
tung’s ‘‘Little Red Book’’ to white radicals on the University of
California-Berkeley campus. The group’s ‘‘Ten Point Program’’
demanded self-determination for black communities, full employ-
ment, decent housing, better education, and an end to police brutality.
In addition, the program included more radical goals: exemption from
military service for black men, all-black juries for African Americans
on trial and ‘‘an end to the robbery by the capitalists of our Black
Community.’’ Newton, the intellectual leader of the group, was
appointed its first Minister of Defense and Eldridge Cleaver, a prison
activist and writer for the New Left journal Ramparts, became
Minister of Information. Sporting paramilitary uniforms of black
leather jackets, black berets, dark sunglasses, and conspicuously
displayed firearms, the Panthers quickly won local celebrity.

BLACK SABBATHENCYCLOPEDIA OF POPULAR CULTURE
265
A series of dramatic events earned the Black Panthers national
notoriety in 1967. That spring, as a result of the Panthers’ initial police
surveillance efforts, members of the California state legislature
introduced a bill banning the carrying of loaded guns in public. In
response, a group of Black Panthers marched into the capitol building
in Sacramento toting loaded weapons. Then, on October 28 of the
same year, Newton was arrested on murder charges following an
altercation with Oakland police which left one officer dead and
Newton and another patrolman wounded. The arrest prompted the
BPP to start a ‘‘Free Huey!’’ campaign which attracted national
attention through the support of Hollywood celebrities and noted
writers and spurred the formation of Black Panther chapters in major
cities across the nation. In addition, Newton’s arrest forced Seale and
Cleaver into greater leadership roles in the organization. Cleaver, in
particular, with his inflammatory rhetoric and powerful speaking
skills, increasingly shaped public perceptions of the Panthers with
incendiary calls for black retribution and scathing verbal attacks
against African American ‘‘counter-revolutionaries.’’ He claimed the
choice before the United States was ‘‘total liberty for black people or
total destruction for America.’’
In February 1968, former Student Non-Violent Coordinating
Committee (SNCC) leader, Stokely Carmichael, who had been invit-
ed by Cleaver and Seale to speak at ‘‘Free Huey!’’ rallies, challenged
Cleaver as the primary spokesman for the party. Carmichael’s Pan-
Africanism, emphasizing racial unity, contrasted sharply with other
Panther leaders’ emphasis on class struggle and their desire to attract
white leftist support in the campaign to free Newton. The ideological
tension underlying this conflict resulted in Carmichael’s resignation
as Prime Minister of the BPP in the summer of 1969 and signaled the
beginning of a period of vicious infighting within the black militant
community. In one incident, after the Panthers branded head of the
Los Angeles-based black nationalist group US, Ron Karenga, a ‘‘pork
chop nationalist,’’ an escalating series of disputes between the groups
culminated in the death of two Panthers during a shoot-out on the
UCLA campus in January 1969.
At the same time, the federal government stepped up its efforts to
infiltrate and undermine the BPP. In August 1967, the FBI targeted
the Panthers and other radical groups in a covert counter-intelligence
program, COINTELPRO, designed to prevent ‘‘a coalition of militant
black nationalist groups’’ and the emergence of a ‘‘black messiah’’
who might ‘‘unify and electrify these violence-prone elements.’’ FBI
misinformation, infiltration by informers, wiretapping, harassment,
and numerous police assaults contributed to the growing tendency
among BPP leaders to suspect the motives of black militants who
disagreed with the party’s program. On April 6, 1968, police descend-
ed on a house containing several Panthers, killing the party’s 17-year-
old treasurer, Bobby Hutton, and wounding Cleaver, who was then
returned to prison for a parole violation. In September, authorities
convicted Newton of voluntary manslaughter. In December, two
Chicago party leaders, Fred Hampton and Mark Clark, were killed in
a police raid. By the end of the decade, 27 members of the BPP had
been killed, Newton was in jail (although he was released after a
successful appeal in 1970), Cleaver had fled to Algeria to avoid
prison, and many other Panthers faced lengthy prison terms or
continued repression. In 1970, the state of Connecticut unsuccessfully
tried to convict Seale of murder in the death of another Panther in
that state.
By the early 1970s, the BPP was severely weakened by external
attack, internal division, and legal problems and declined rapidly.
After his release from prison in 1970, Newton attempted to wrest
control of the party away from Cleaver and to revive the organiza-
tion’s popular base. In place of Cleaver’s fiery rhetoric and support
for immediate armed struggle, Newton stressed community organiz-
ing, set up free-breakfast programs for children and, ultimately,
supported participation in electoral politics. These efforts, though,
were undermined by widely published reports that the Panthers
engaged in extortion and assault against other African Americans. By
the mid-1970s, most veteran leaders, including Seale and Cleaver,
had deserted the party and Newton, faced with a variety of criminal
charges, fled to Cuba. After his return from exile, Newton earned a
doctorate, but was also involved with the drug trade. In 1989, he was
shot to death in a drug-related incident in Oakland. Eldridge Cleaver
drifted rightward in the 1980s, supporting conservative political
candidates in several races. He died on May 1, 1998, as a result of
injuries he received in a mysterious mugging. Bobby Seale continued
to do local organizing in California. In 1995, Mario Van Pebbles
directed the feature film, Panther, which attempted to bring the story
of the BPP to another generation. The Panthers are remembered today
as much for their cultural style and racial posturing as for their
political program or ideology.
—Patrick D. Jones
F
URTHER READING:
Brown, Elaine. A Taste of Power: A Black Woman’s Story. New York,
Pantheon, 1992.
Chruchill, Ward. Agents of Repression: The FBI’s Secret Wars
Against the Black Panther Party and the American Indian Move-
ment. Boston, South End, 1988.
Cleaver, Eldridge. Soul On Ice. New York, Laurel/Dell, 1992.
Hilliard, David. This Side of Glory: The Autobiography of David
Hilliard and the Story of the Black Panther Party. Boston, Little
Brown, 1993.
Keating, Edward. Free Huey! Berkeley, California, Ramparts, 1970.
Moore, Gilbert. Rage. New York, Carroll & Graf, 1971.
Newton, Huey. To Die for the People: The Writings of Huey P.
Newton. New York, Random House, 1972.
Pearson, Hugh. The Shadow of the Panther: Huey Newton and the
Price of Black Power In America. Reading, Massachusetts, Addi-
son-Wesley, 1994.
Seale, Bobby. Seize the Time: The Story of the Black Panther Party
and Huey P. Newton. New York, Random House, 1970.
Black Sabbath
Formed in Birmingham, England in 1968, Black Sabbath was
one of the most important influences on hard rock and grunge music.
While the term ‘‘heavy metal’’ was taken from a Steppenwolf lyric
and had already been applied to bands such as Cream and Led
Zeppelin, in many ways Black Sabbath invented the genre. They were
perhaps the first band to include occult references in their music, and
they began to distance themselves from the blues-based music which
was the norm, although they had started their career as a blues band.
Originally calling themselves Earth, they discovered another
band with the same name. After renaming themselves Black Sabbath
BLACK SOX SCANDAL ENCYCLOPEDIA OF POPULAR CULTURE
266
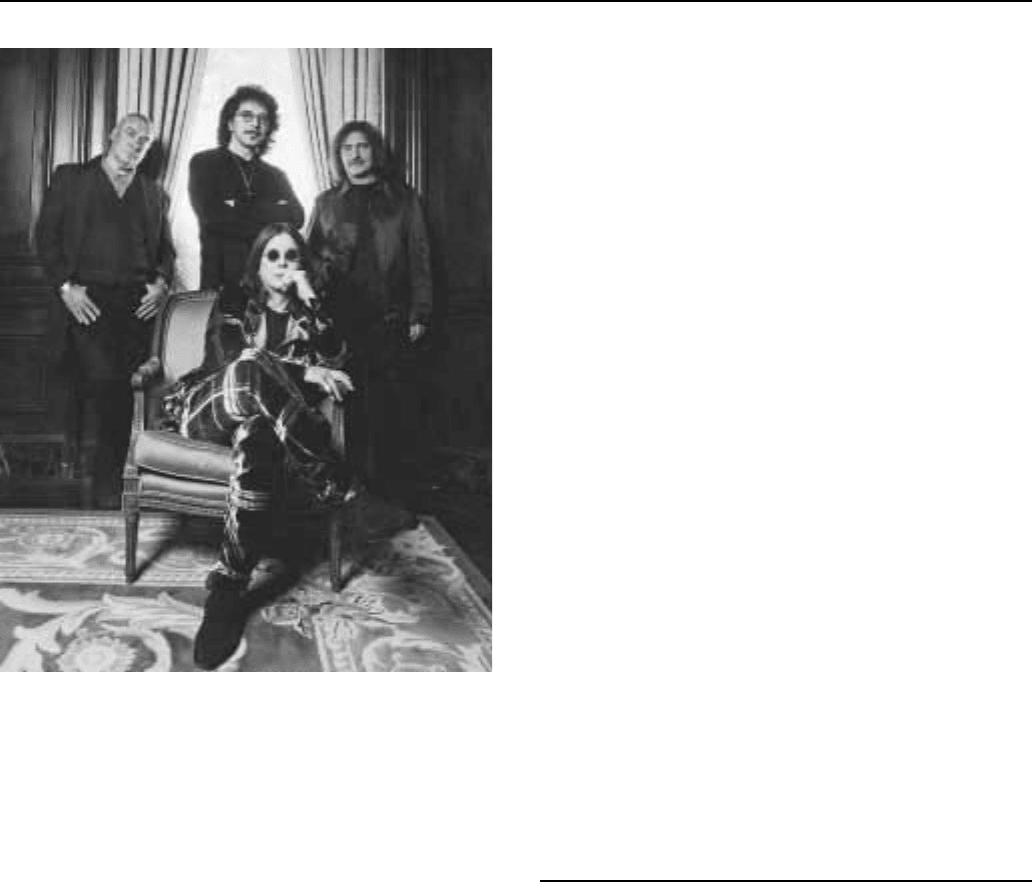
Black Sabbath in 1998: Ozzy Osbourne (seated), (standing from left) Bill
Ward, Tony Iommi, and Geezer Butler.
the group released their self-titled first album in 1970. Black Sabbath
was recorded both quickly and inexpensively—it took only two days
and cost six hundred pounds. In spite of that, the album reached
number 23 on the American charts and would eventually sell over a
million copies. Paranoid was released later the same year and cracked
the top ten in the United States while topping the charts in Britain.
Their third album, Master of Reality, was equally successful and
remained on the Billboard charts in America for almost a year.
Those releases introduced themes which would become staples
for future metal bands: madness, death, and the supernatural. Al-
though some considered the band’s lyrics satanic, there was often an
element of camp present. The group got its name from the title of a
Boris Karloff film, and songs such as ‘‘Fairies Wear Boots’’ are at
least partly tongue-in-cheek. But vocalist John ‘‘Ozzy’’ Osbourne’s
haunting falsetto and Tony Iommi’s simultaneously spare and thun-
dering guitar work would become touchstones for scores of hard
rock bands.
Sabbath released three more albums as well as a greatest hits
collection before Osbourne left the group in 1977, reportedly because
of drug and alcohol problems. He returned in 1978, then left perma-
nently the following year to start his own solo career. Initially, both
Osbourne and the new version of Black Sabbath enjoyed some degree
of commercial success, although many of the Sabbath faithful insisted
the whole greatly exceeded the sum of its parts. During the 1980s the
band would go through an astonishing array of lineup changes and
their popularity plummeted.
In the late 1980s and early 1990s, Soundgarden, Helmet, Nirva-
na, and others in the grunge and resurgent hard rock movements
demonstrated that they had been heavily influenced by the early Black
Sabbath, and this effectively rehabilitated the band’s reputation.
While Sabbath had often been viewed as a dated version of the arena
rock of the 1970s, grunge indicated not only that their music remained
vibrant, but also that it bore many surprising similarities to the Sex
Pistols, Stooges, and other punk and proto-punk bands. Sabbath
became heroes to a new generation of independent and alternative
bands, and the group’s first albums enjoyed an enormous resurgence
in popularity. Their music returned to many radio stations and was
even featured in television commercials. Osbourne organized Ozzfest,
an annual and very successful tour which featured many of the most
prominent heavy metal and hard rock acts, as well as his own band.
Iommi continued to record and tour with Black Sabbath into the late
1990s, although he was the only original member, and listeners and
audiences remained largely unimpressed.
—Bill Freind
F
URTHER READING:
Bashe, Philip. Heavy Metal Thunder: The Music, Its History, Its
Heroes. Garden City, New York, Doubleday, 1985.
Walser, Robert. Running with the Devil: Power, Gender, and Mad-
ness in Heavy Metal Music. Hanover, New Hampshire, University
Press of New England, 1993.
Black, Shirley Temple
See Temple, Shirley
Black Sox Scandal
Although gambling scandals have been a part of professional
baseball since the sport’s beginning, no scandal threatened the game’s
stature as ‘‘the national pastime’’ more than the revelations that eight
members of the Chicago White Sox had conspired to throw the 1919
World Series. Termed the ‘‘Black Sox Scandal,’’ the event will go
down in history as one of the twentieth century’s most notorious
sports debacles.
The Chicago White Sox of the World War I period were one of
the most popular teams in the major leagues. They were led on the
field by ‘‘Shoeless’’ Joe Jackson, an illiterate South Carolinian whose
.356 career batting average is the third highest ever, and pitchers
Eddie Cicotte and Lefty Williams. The Sox were owned by Charles
A. Comiskey, a nineteenth-century ballplayer notorious for paying
his star players as little as possible; Cicotte, who led the American
League with 29 wins in 1919, earned just $5,500 that season.
Comiskey’s stinginess included not paying for the team’s laundry in
1918—the team continued to play in their dirty uniforms, which is
when the sobriquet ‘‘Black Sox’’ originated.
During the 1919 season, the White Sox dominated the American
League standings. Several players on the team demanded that Comiskey
BLACK SOX SCANDALENCYCLOPEDIA OF POPULAR CULTURE
267
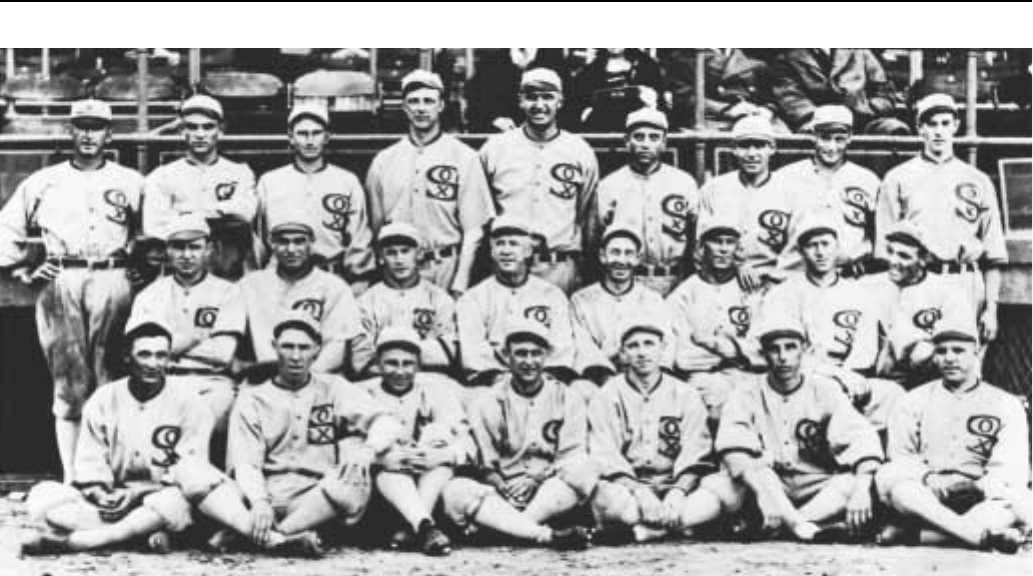
The 1919 Chicago White Sox.
give them raises. He refused. First baseman Chick Gandil began
discussing throwing the World Series with his fellow players. The
eight Sox players who attended meetings on throwing the Series were
Cicotte, Gandil, Williams, Jackson, shortstop Swede Risberg, third
basemen Fred McMullin and Buck Weaver, and outfielder Happy
Felsch. In mid-September, Gandil met with small-time Boston gam-
bler ‘‘Sport’’ Sullivan in New York, telling him his teammates were
interested in throwing the upcoming World Series if Sullivan could
deliver them $80,000. Two more gamblers, ex-major league pitcher
Bill Burns and former boxer Billy Maharg, agreed to contribute
money. These three gamblers contacted New York kingpin Arnold
Rothstein, who agreed to put up the full $80,000.
Cicotte pitched the Series opener against the Reds. As a sign to
the gamblers that the fix was on, he hit the first batter with a pitch.
Almost instantly, the gambling odds across the country shifted from
the White Sox to the Reds. The Sox fumbled their way to a 9-1 loss in
Game One.
Throughout the Series, the White Sox made glaring mistakes on
the field—fielders threw to the wrong cutoff men, baserunners were
thrown out trying to get an extra base, reliable bunters could not make
sacrifices, and control pitchers such as Williams began walking
batters. Most contemporary sportswriters were convinced something
was corrupt. Chicago sportswriter Hugh Fullerton marked dubious
plays on his scorecard and later discussed them with Hall of Fame
pitcher Christy Mathewson.
The 1919 Series was a best-of-nine affair, and the underdog
Reds led four games to one after five games. When the gamblers’
money had not yet arrived, the frustrated Sox began playing to win,
beating Cincinnati in the sixth and seventh games. Before Williams
started in the eighth game, gamblers approached him and warned him
his wife would be harmed if he made it through the first inning.
Williams was knocked out of the box after allowing three runs in the
first inning. The Cincinnati Reds won the Series with a command-
ing 10-5 win.
After the Series, Gandil, who had pocketed $35,000 of the
$80,000, retired to California. Fullerton wrote columns during the
following year, insisting that gamblers had reached the White Sox; he
was roundly criticized by the baseball establishment and branded
a malcontent.
The fixing of the 1919 Series became public in September 1920,
when Billy Maharg announced that several of the World Series games
had been thrown. Eddie Cicotte broke down and confessed his
involvement in the fixing; he claimed he took part in taking money
‘‘for the wife and kiddies.’’ Joe Jackson, who during the Series batted
a robust .375, signed a confession acknowledging wrongdoing. Upon
leaving the courthouse, legend has it that a tearful boy looked up to
him and pleaded, ‘‘Say it ain’t so, Joe.’’ ‘‘I’m afraid it is,’’ Jackson
allegedly replied.
On September 28, 1920 a Chicago grand jury indicted the eight
players. They were arraigned in early 1921. That summer they were
tried on charges of defrauding the public. The accused were repre-
sented by a team of expensive lawyers paid for by Comiskey. At the
trial it was revealed that the signed confessions of Jackson, Cicotte,
and Williams had been stolen. The defense lawyers maintained that
there were no laws on the books against fixing sporting events.
Following a brief deliberation, the eight were found not guilty on
August 2, 1921. The impact of the allegation, however, was undeni-
able. Kennesaw Mountain Landis, a former Federal judge elected as
organized baseball’s first commissioner in November 1920, declared,
‘‘No player who throws a ball game, no player who undertakes or
promises to throw a ball game, no player who sits in a conference with
a bunch of crooked players and gamblers, where the ways and means
BLACKBOARD JUNGLE ENCYCLOPEDIA OF POPULAR CULTURE
268
of throwing a ball game are planned and discussed and does not
promptly tell his club about it, will ever play professional baseball.’’
The eight Black Sox players spent the rest of their lives in exile.
Jackson played semi-pro baseball under assumed names. Several
appealed to be reinstated, but Landis and his successors invariably
rejected them. Perhaps the saddest story of all was Buck Weaver’s.
While he had attended meetings to fix the Series, he had never
accepted money from the gamblers and had never been accused of
fixing games by the prosecution (in fact, Weaver batted .324 during
the Series). But for not having told Comiskey or baseball officials
about the fix, he was tried with his seven teammates and thrown out of
baseball with them. The last surviving member of the Black Sox,
Swede Risberg, died in October 1975.
Most historians credit baseball’s subsequent survival to two
figures. From on high, Landis ruled major league baseball with an
iron fist until his death in 1944 and gambling scandals decreased
substantially throughout organized baseball. On the field of play,
Babe Ruth’s mythic personality and home run hitting ability brought
back fans disillusioned by the 1919 scandal, while winning the game
millions of new fans.
—Andrew Milner
F
URTHER READING:
Asinof, Eliot. Eight Men Out. New York, Holt, 1963.
Light, Jonathan Frase. The Cultural Encyclopedia of Baseball. Jeffer-
son, North Carolina, McFarland, 1997.
Wallop, Douglass. Baseball: An Informal History. New York, W.W.
Norton, 1969.
The Blackboard Jungle
Ten years after the end of World War II, writer-director Richard
Brooks’ film, The Blackboard Jungle (1955) was released. The film
remains as a moody, entertaining potboiler and an early formula for
treating a theme—the rehabilitating education of delinquents and the
inner-city underprivileged—that was still being explored in the
cinema of the 1980s and 1990s. Films as diverse as the serious and
specific Stand and Deliver (1988, Edward James Olmos played the
beleaguered teacher), the comedic Renaissance Man (1994, Danny de
Vito), and the sentimental Dangerous Minds (1995, Michelle Pfeiffer),
can all find their origins in The Blackboard Jungle, which, although
not a particularly masterful film, was unique in its time, and became a
cultural marker in a number of respects. It is popularly remembered as
the first movie ever to feature a rock ’n’ roll song (Bill Haley and the
Comets, ‘‘Rock around the Clock’’), and critically respected for its
then frank treatment of juvenile delinquency and a powerful perform-
ance by actor Glenn Ford. It is notable, too, for establishing the hero
image of African American Sidney Poitier, making him Hollywood’s
first black box-office star, and for its polyglot cast that accurately
reflected the social nature of inner-city ghetto communities.
The Blackboard Jungle, however, accrues greater significance
when set against the cultural climate that produced it. Despite the post
war position of the United States as the world’s leading superpower,
the country still believed itself under the threat of hostile forces.
Public debate was couched exclusively in adversarial terms; under the
constant onslaught, the nation succumbed to the general paranoia that
detected menace in all things from music to motorcyclists, from
people of color and the poor to intellectuals and poets. Even the young
were a menace, a pernicious presence to be controlled, and protected
from the rock ’n’ roll music they listened and danced to, which was
rumored as part of a Communist plot designed to corrupt their morals.
From the mid-1940s on, a stream of novels, articles, sociological
studies and, finally, movies, sought to explain, sensationalize, vilify,
or idealize juvenile delinquency. It was precisely for the dual purpose
of informing and sensationalizing that The Blackboard Jungle was
made, but, like Marlon Brando’s The Wild One (1954), it served to
inflame youthful sentiment, adding tinder to a fire that was already
burning strong.
Adapted from a 1954 novel by Evan Hunter, Brooks’ film tells
the story of Richard Dadier (Ford), a war veteran facing his first
teaching assignment at a tough inner-city high school in an unspeci-
fied northern city. ‘‘This is the garbage can of the educational
system,’’ a veteran teacher tells Dadier. ‘‘Don’t be a hero and never
turn your back on the class.’’ Dadier’s class is the melting pot
incarnate, a mixture of Puerto Ricans, Blacks, Irish, and Italians
controlled by two students—Miller (Poitier) and West (Vic Morrow),
an Irish youth. West is portrayed as an embryo criminal, beyond
redemption, but Miller provides the emotional focus for the movie.
He is intelligent, honest, and diligent, and it becomes Dadier’s
mission to encourage him and develop his potential. However, in its
antagonism to Dadier, the class presents a unified front. They are
hostile to education in general and the teacher’s overtures in particu-
lar, and when he rescues a female teacher from a sexual attack by a
student the hostility becomes a vendetta to force him into quitting.
However, despite being physically attacked, witnessing the victimi-
zation of his colleagues, and withstanding wrongful accusations of
bigotry while worrying about his wife’s difficult pregnancy, Dadier
triumphs over the rebellious students and, by extension, the educa-
tional system. He retains his idealism, and in winning over his
students overcomes his own prejudices.
In setting the film against the background of Dadier’s middle-
class life and its attendant domestic dramas, it was assumed that
audiences would identify with him, the embattled hero, rather than
with the delinquent ghetto kids, but the film’s essentially moral tone is
subverted by the style, the inflections, and exuberance of those kids.
Following an assault by West and his cohorts, Dadier’s faith begins to
waver. He visits a principal at a suburban high school. Over a
soundtrack of students singing the ‘‘Star Spangled Banner’’ Dadier
tours the classrooms filled with clean-cut white students, tractable
and eager to learn. He may yearn for this safe environment, but to the
teenage audiences that flocked to The Blackboard Jungle, it is
Dadier’s inner city charges that seem vital and alive, while the
suburban high school appears as lively as a morgue. The teen
response to The Blackboard Jungle was overwhelming. ‘‘Suddenly,
the festering connections between rock and roll, teenage rebellion,
juvenile delinquency, and other assorted horrors were made explic-
it,’’ writes Greil Marcus. ‘‘Kids poured into the theaters, slashed the
seats, rocked the balcony; they liked it.’’
The instigation of teen rebellion was precisely the opposite
reaction to what the filmmakers had intended. From the opening title
