Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

492
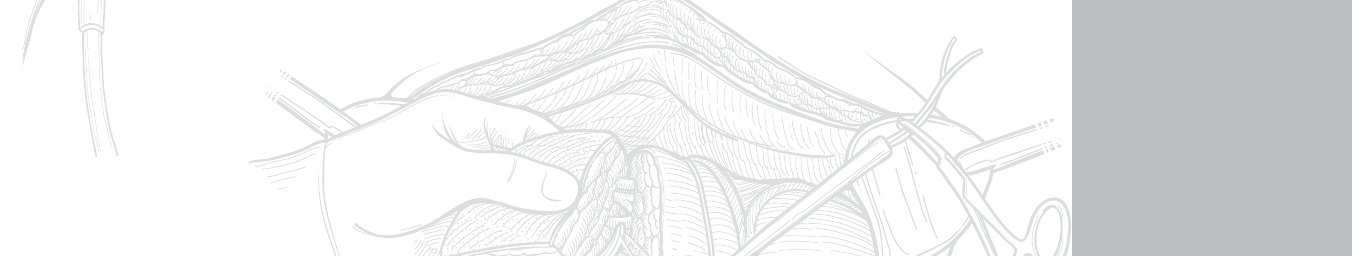
STEP 1: SURGICAL ANATOMY
◆ The liver is suspended in the right upper quadrant by avascular ligamentous attachments. The
falciform ligament is oriented vertically and suspends the liver from the anterior abdominal
wall at its inferior limit to the diaphragm just anterior to the vena cava. The left and right tri-
angular ligaments extend in a transverse direction beginning on the lateral borders of both the
left and right liver, coursing along the diaphragm, and terminating at the vena cava where
they join the superior extent of the falciform ligament. The triangular ligaments are composed
of both anterior and posterior leafl ets.
◆ The liver appears on gross examination to be composed of two discrete lobes. Thus there is a
traditional terminology in which the left and right lobes are defi ned by the falciform ligament.
Resection of one of these is termed a left or right lobectomy. This terminology has largely been
replaced by one based on the intraparenchymal vascular and biliary structures.
◆ Based on the intraparenchymal anatomy, the liver is divided into left and right livers, each
composed of four segments. The line of demarcation is located several centimeters to the
right of the falciform ligament and projects in a line that transects the gallbladder bed from
anterior to posterior (Figures 46-1 and 46-2).
◆ Using the segmental anatomy, the liver is divided into left liver and right liver. The left liver is
served by the left portal vein, left hepatic artery, and left bile duct. It is composed of segments
I, II, III, and IV. Segments II and III represent the traditionally termed left lobe. Segment II is
attached to the left diaphragm, and segment III occupies the inferior aspect of the left lobe.
The boundary between the two extends horizontally approximately midway through the left
lobe. Segment one is also called the caudate lobe. It occupies the posterior aspect of the liver
in the midline. The segment wraps rather like a collar around the vena cava on its left aspect.
This segment is unique for its venous drainage, which is independent of the left or middle
hepatic veins and is composed of multiple tiny tributaries between the vena cava and the seg-
ment. Segment IV is also termed the quadrate lobe, and it occupies the area between the falci-
form ligament medially and the gallbladder bed laterally (see Figure 46-1).
◆ The right liver is composed of segments V, VI, VII, and VIII. These four are oriented around
a horizontal line transecting the right liver at its mid-portion and similarly by a vertical line
that transects the right liver at its mid-portion. Beginning at the inferomedial segment V, the
segments follow a clockwise direction, with VI inferolateral, VII superolateral, and VIII
superomedial (see Figures 46-1 and 46-2).
CHAPTER
46
Left Hepatic Lobectomy
William H. Nealon
CHAPTER 46 • Left Hepatic Lobectomy 493
I
Common bile duct
Hepatic artery
Splenic vein
Portal vein
V
VI
IV-B
III
VII
VIII
IV-A
II
FIGURE 46 –1
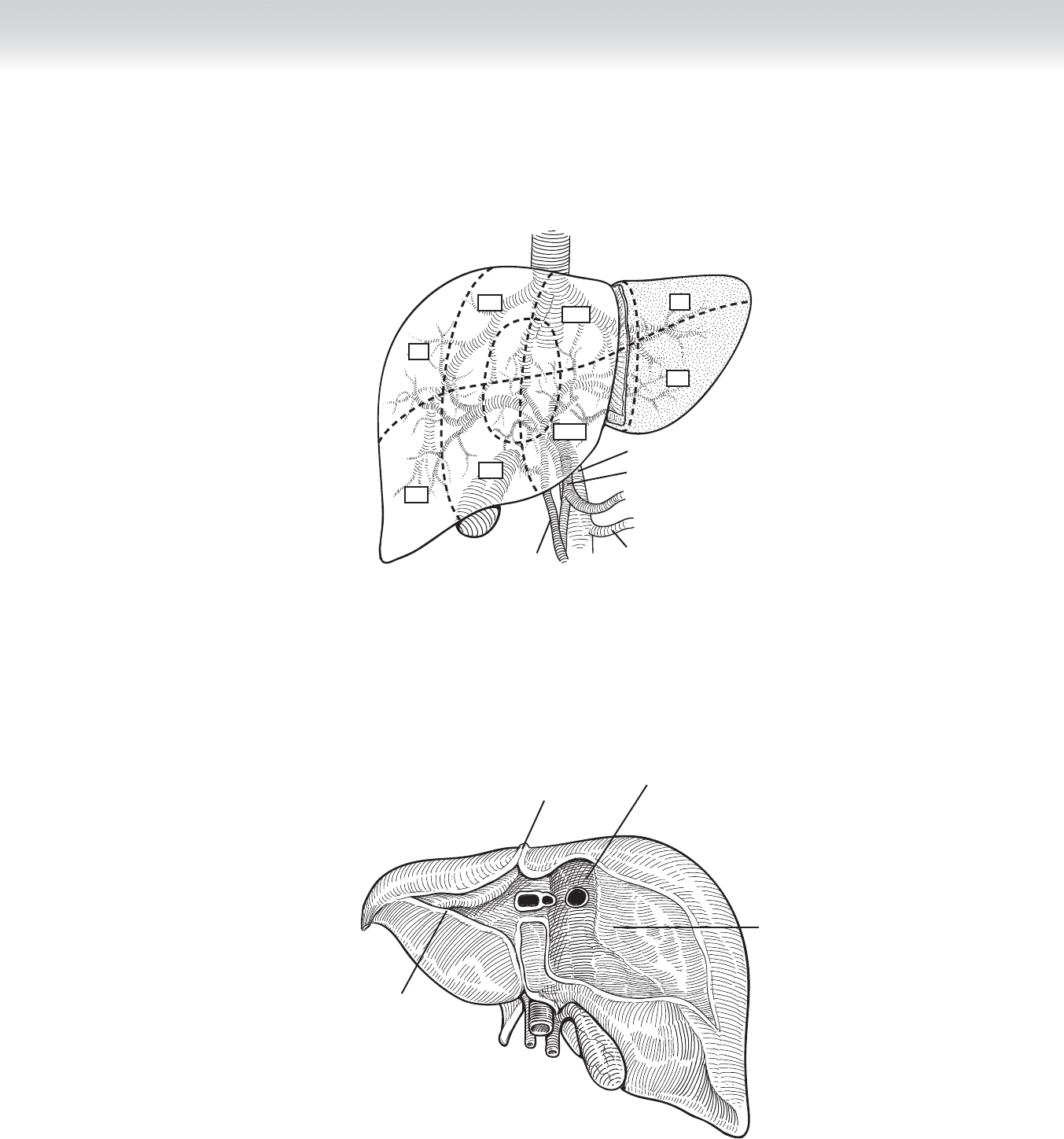
Falciform ligament
Triangular ligament
Bare area
Groove for vena cava
FIGURE 46 –2

494 Section VI • Liver
◆ Lymphovascular and biliary structures enter the liver through the hepatoduodenal ligament
that courses between the duodenum into the base of segments IV and V, which is termed
the porta hepatis. The portal triad of microanatomy is matched by the gross anatomic orien-
tation in the hepatoduodenal ligament—composed of hepatic artery, portal vein, and bile
duct. Each structure divides into a left and right branch and then arborizes within the liver
in a pattern defi ned by the segments (see Figures 46-1 and 46-2).
◆ Venous drainage of the liver is primarily located at the superior aspect of the liver in the
midline in short structures between the vena cava and the liver. The left, middle, and right
hepatic veins each enter the vena cava within 2 to 4 cm of one another in a coronal orienta-
tion. One or all of these venous elements may be intrahepatic or may have exceedingly
short extrahepatic components. This anatomic feature raises considerably the risk of uncon-
trolled hemorrhage during dissection and resection (see Figure 46-2). In addition to these
three venous structures, there are between 2 and 20 tiny tributaries between the posterior
surface of the liver and the contiguous vena cava. These must be divided to fully mobilize
the right liver.
INDICATIONS
◆ Left hepatic lobectomy is performed primarily for the treatment of malignant disease, which
includes hepatocellular carcinoma, intrahepatic cholangiocarcinoma, and a variety of meta-
static lesions—most commonly of abdominal origin. The best outcomes are achieved in
patients with metastatic lesions from carcinoma of the colon and rectum.
◆ However, the procedure is also performed for benign diseases, such as cystadenoma of the
liver, giant hemangioma of the liver, and intrahepatic biliary strictures existing primarily
on the left side of the biliary tree, and at times for lesions such as either hepatic adenoma
or focal nodular hyperplasia determined to be clinically signifi cant, perhaps because of
increasing size.
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ Due to the magnitude of hepatic surgery, one fi rst consideration is the medical status of the
patient and likely risk of surgery. Thus one must exclude signifi cant coronary, pulmonary,
or renal disease or age and frailty. Of particular concern in relation to hepatic surgery is the
underlying hepatic function. Because hepatocellular carcinoma is associated with prior hep-
atitis and cirrhosis, one must determine fi rst whether cirrhosis exists and second what level
of function is apparent. Historically, this was measured by examining synthetic and excre-
tory functions and measures of portal hypertension (serum albumin level, coagulation pro-
fi le, serum bilirubin level, ascites, and mental status/serum ammonia). More recently, the
Model for End-Stage Liver Disease (MELD) score was developed as a means of segregating
candidates for liver transplant. This system incorporates prior variables but has added and
places considerable signifi cance to renal function. Particularly when one anticipates a major
resection one must establish that suffi cient liver will remain to support life. Unfortunately,
this estimate of “hepatic reserve” is even today an inexact science.
CHAPTER 46 • Left Hepatic Lobectomy 495
◆ Nutritional status, renal function, degree of ascites, and coagulation abnormalities are all
factors that may be improved by medical management before surgery. Unfortunately, we
have personal experience that such patients may thereby achieve an improved functional
grade but appear to carry a risk that exceeds the risk in patients who have had this
improved functional status without a need for medical manipulation to achieve it.
◆ In the case of malignancy, one must establish that curative resection is clinically achievable.
◆ Routine bowel preparation with both colonic cleansing and antibiotics by the oral route
should be performed. Measures should be taken to have blood transfusions available for the
operation, and on rare occasions platelets should be available.
STEP 3: OPERATIVE STEPS
1. INCISION
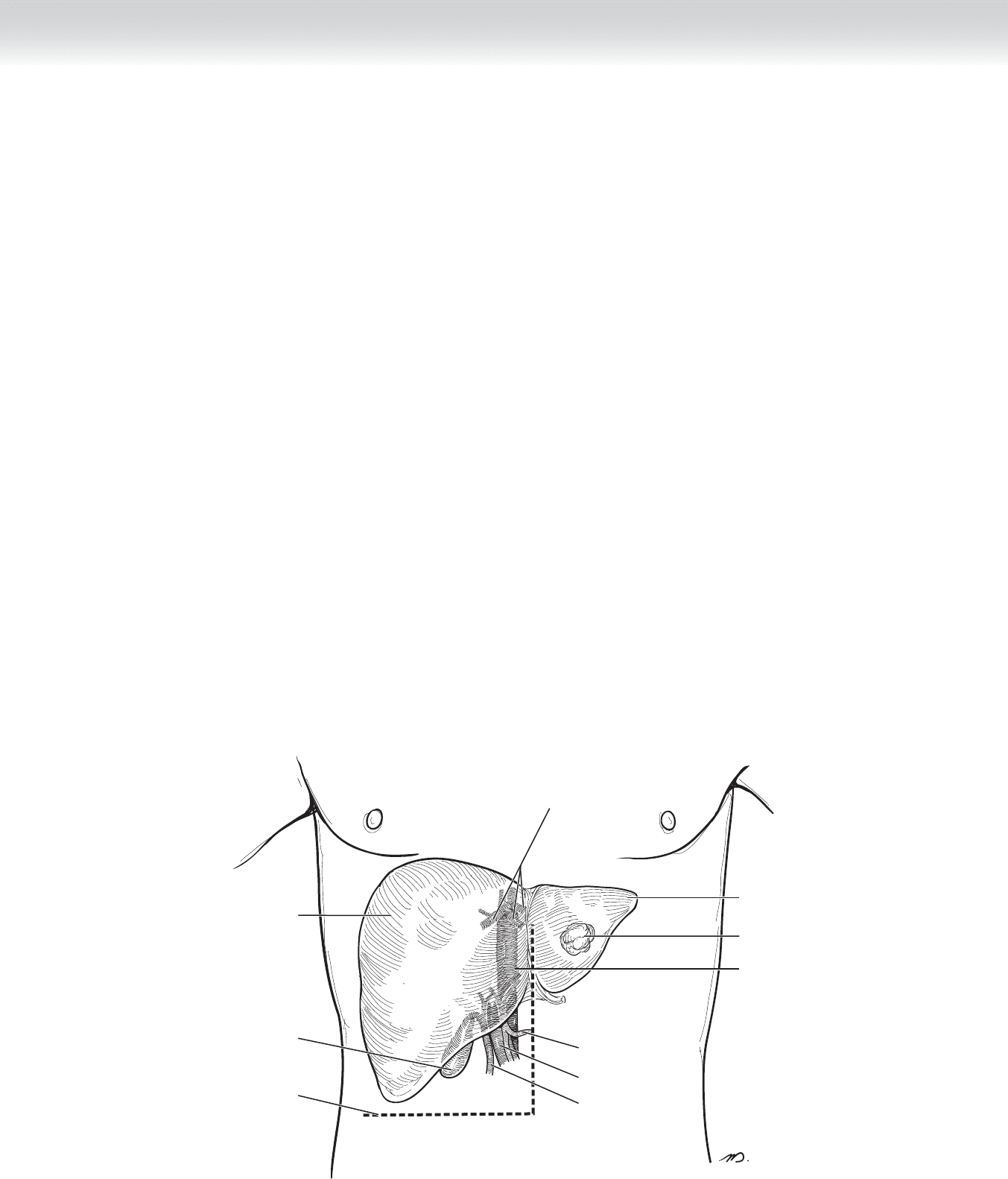
◆ Several incisions can be used with success for the left hepatic resection. We favor the inverted
L incision. Added exposure may be achieved in this incision by extending the incision either
laterally toward the right fl ank along the horizontal component of this incision or medially
across the midline. In addition, one may improve exposure by extending the vertical compo-
nent of the incision toward the xiphoid process (Figure 46-3). Some surgeons prefer the
bilateral subcostal incision with an option to extend the incision in the midline toward the
xiphoid.
Common
hepatic artery
Portal vein
Inferior vena cava
Hepatic veins
Gallbladder
Common bile duct
Incision
Left lobe
Right lobe
Lesion
FIGURE 46 –3

496 Section VI • Liver
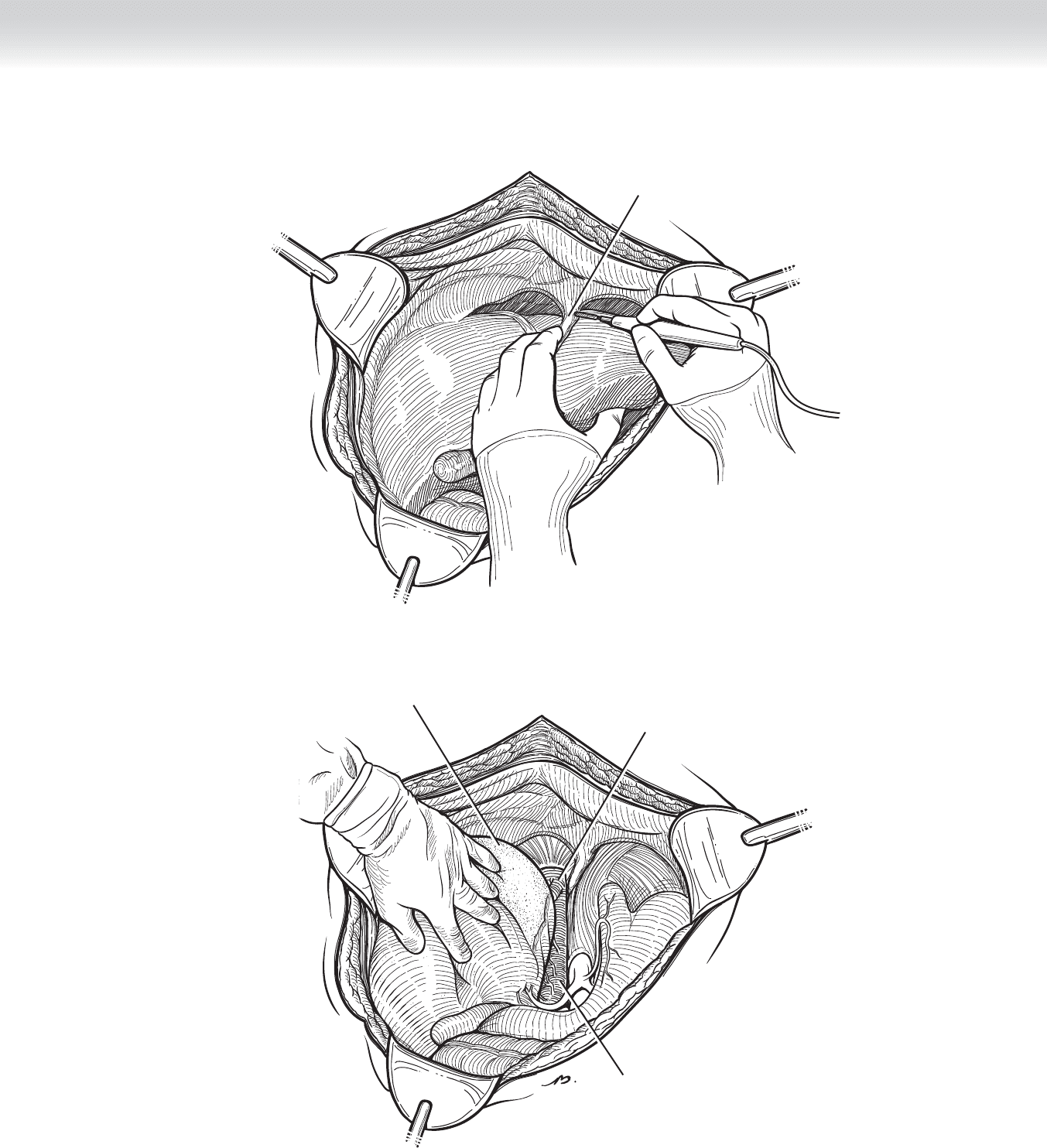
2. DISSECTION
◆ Divide the falciform ligament and leave a 2-0 silk suture as a stay suture, and then place a
hemostat on the silk suture. Carefully incise the avascular plane extending from the falciform
ligament back toward the diaphragm using electrocautery after placing the right hand
beneath the left lobe of the liver (Figure 46-4). In a similar manner under direct vision,
incise the left triangular ligament using electrocautery by fi rst cauterizing the anterior leafl et
of the left triangular ligament. Second, take the posterior leafl et of the left triangular ligament
over toward the vena cava. Anticipate, possibly visualizing, the left hepatic vein as the dissec-
tion carries close to the vena cava and carefully monitor to prevent any injury to the left
hepatic vein. Carefully divide some of the fi ber attachments between the diaphragm and the
superior border of the liver, where the falciform ligament has inserted, and begin to visualize
the vena cava and possibly visualize the middle and left hepatic veins (Figure 46-5).
CHAPTER 46 • Left Hepatic Lobectomy 497
Diaphragm
FIGURE 46 –4
Left hepatic vein
Inferior vena cava
Bare area
FIGURE 46 –5

498 Section VI • Liver
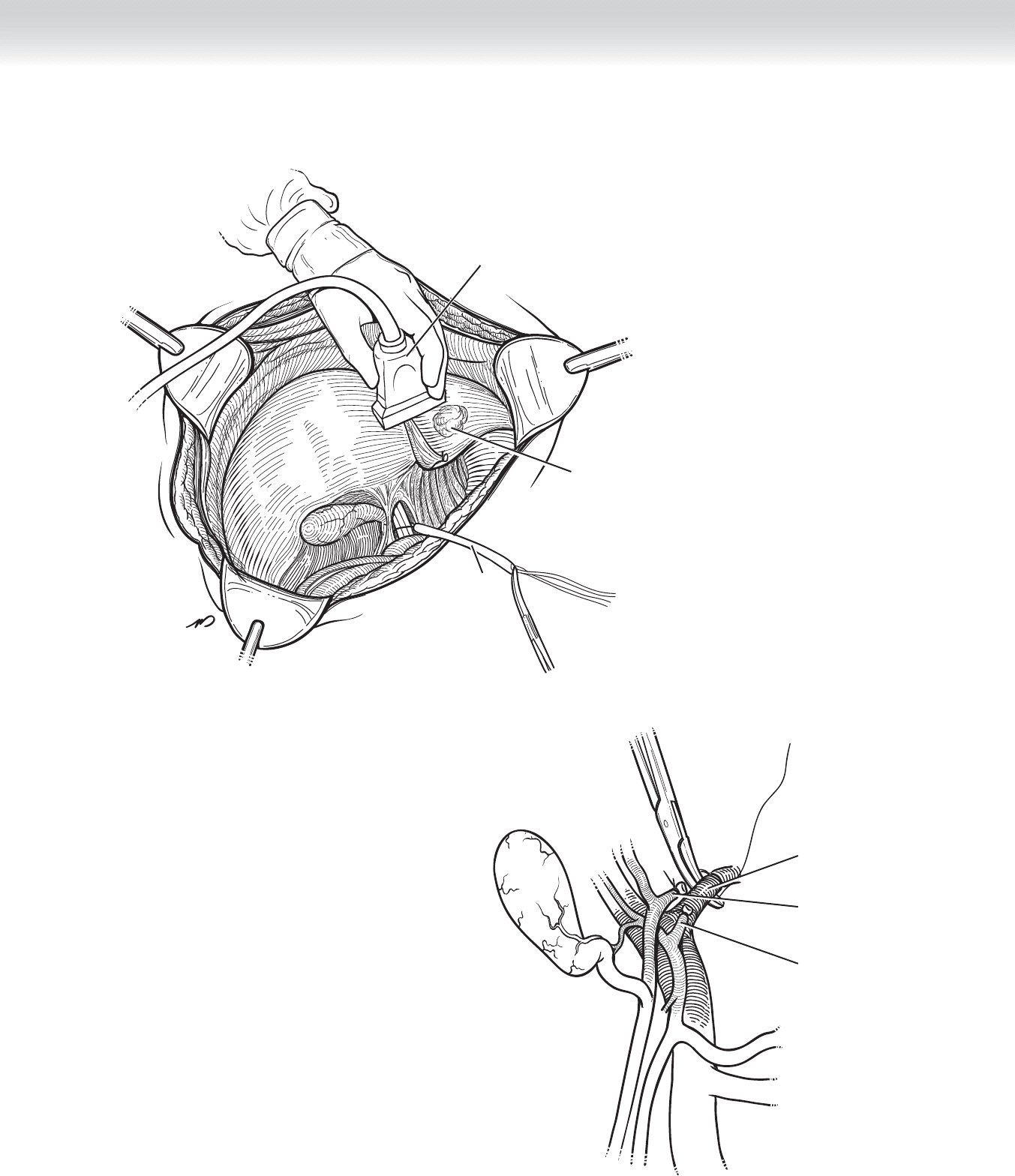
◆ Place a Rummel loop surrounding the portal triad by incising the peritoneum just medial to
the hepatoduodenal ligament. By passing the left hand into the foramen of Winslow, you
pass an umbilical tape. This tape is grasped and placed in the hook device, and the umbili-
cal tape is passed through a section of rubber tubing (Figure 46-6). Use this step in the
event that uncontrolled hemorrhage is encountered during the resection. At this point it is
occasionally necessary to use ultrasound for two reasons:
◆ To establish that the anticipated line of resection includes the lesion you want to resect
◆ To visualize intrahepatic vascular structures, particularly hepatic venous and intrahepatic
portions of the portal venous system (see Figure 46-6)
◆ Next, direct attention to the hepatoduodenal ligament where you must separately identify
each of the three major components of the ligament, which include the following:
◆ Common bile duct
◆ Proper hepatic artery
◆ Portal vein
◆ Encircle the common bile duct with a
1
⁄4-inch Penrose drain. Then encircle the proper
hepatic artery using vessel loops. By placing lateral traction on the bile duct and medial traction
on the artery, you will expose the portal vein, which is situated between these two structures in
a slightly deeper plane. By gently teasing the tissues toward the hilum following a horizontal
plane along the base of segment IV, you will lower the falciform plate. This provides visualiza-
tion of the left structures of the portal, arterial, and biliary systems (Figure 46-7).
◆ Establish an acceptable length on each of these structures to ensure careful and safe division.
◆ Divide the left hilar structures sequentially. Divide the left hepatic duct. You must use nonab-
sorbable suture, either 3-0 or 4-0 Vicryl or polydioxanone (PDS). Divide the left hepatic
artery between clamps and suture ligate using 3-0 silk suture ligature. Divide the portal vein
between clamps. Sew the stump of the left portal vein with a continuous running 4-0
Prolene suture (see Figure 46-7).
◆ After division of all of the left hilar structures, a clear line of demarcation will be seen with
purple discoloration of the anatomic left liver. The demarcation crosses the gallbladder bed
from anterior to posterior.
◆ In patients who still have a gallbladder, perform a cholecystectomy in the normal fashion.
◆ Encircle the left hepatic vein with a vessel loop. It is important to note that at times, with
varying sizes of the liver, the left hepatic vein may be situated in a more lateral and inferior
location than you might anticipate, and it is vital to establish whether the vein that is fi rst
seen in the dissection along the diaphragm is not the middle hepatic vein. It is also vital
that you not sacrifi ce the middle hepatic vein if it is not necessary to do so. Do not divide
the hepatic veins until you complete the dissection. However, establish some control of the
vein by encircling it.
CHAPTER 46 • Left Hepatic Lobectomy 499
Tumor
Rummel loop
Intraoperative
ultrasound
FIGURE 46 –6
Left portal vein
being divided
Left hepatic duct
Left hepatic artery
(divided)
FIGURE 46 –7

500 Section VI • Liver
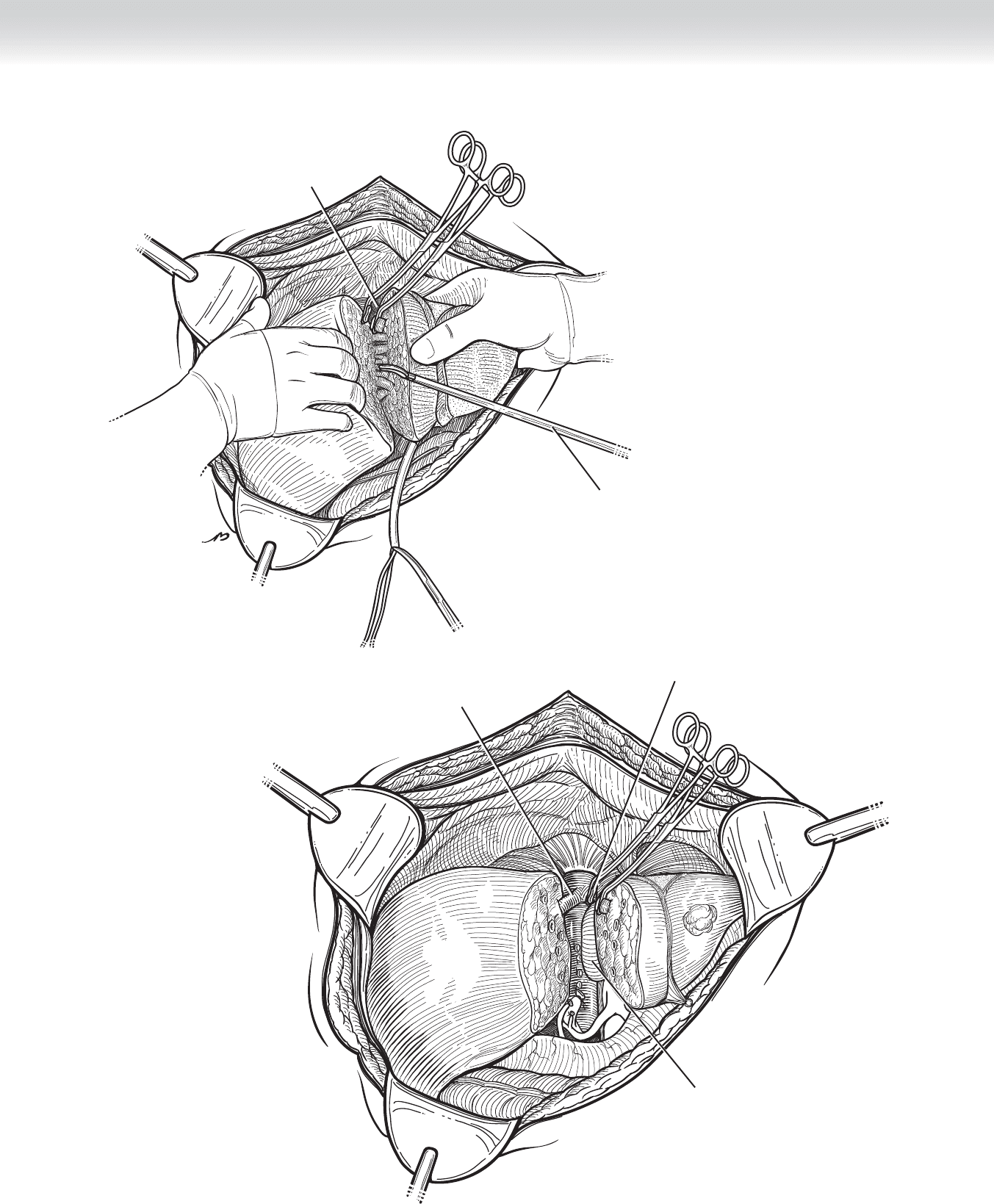
◆ Once you establish safety, proceed with the resection. The Habib radio-frequency device
may be used for division of parenchyma that is remote from major structures. During divi-
sion of the parenchyma, you will visualize vascular and biliary structures. When size dic-
tates, these may be divided between clamps and tied (Figure 46-8).
◆ Along the line of demarcation, score the capsule of the liver anteriorly, using electrocautery.
Then use a harmonic scalpel to carefully and sequentially divide the liver by layers. Do not
permit yourself to establish a deep hole in the liver where control of hemorrhage will be
greatly compromised.
◆ During this dissection, divide major portal, arterial, and biliary structures between clamps
and suture ligate using 3-0 silk suture ligatures. Slightly blunt clearing of surrounding fl aky
parenchyma may be achieved using a metal-tipped fi ne-tip suction apparatus, such as the
Frazier tip instrument. As the dissection is carried toward the hilar structures, it is vital to
recognize and avoid injury to the right hepatic vessels; failure to do so can result in isch-
emia of the right liver (see Figure 46-8).
◆ At this point, no more than 0.5 to 2 cm depth of liver remains before you encounter the
vena cava. Carry the dissection down to the vena cava, beginning in the inferior border of
the liver. The left hepatic vein is typically situated at the diaphragmatic surface of the supe-
rior border of the left liver. Once again, note that at times the liver may be rotated, and
what appears to be the left hepatic vein may be the middle hepatic vein. Do not divide the
vein until all infl ow has been reliably interrupted. Typically, the hepatic veins are not
divided until the completion of the dissection. Thus stay alert for the identifi cation of the
left hepatic vein as the dissection is carried superiorly for the fi nal 0.5 to 2 cm thickness of
remaining left liver attached to the right liver (Figure 46-9).
CHAPTER 46 • Left Hepatic Lobectomy 501
Left hepatic vein
Harmonic
FIGURE 46 –8
Left hepatic vein
Middle hepatic vein
Segment I
FIGURE 46 –9
