Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

CHAPTER 85 • Femoropopliteal Bypass (In Situ) 921
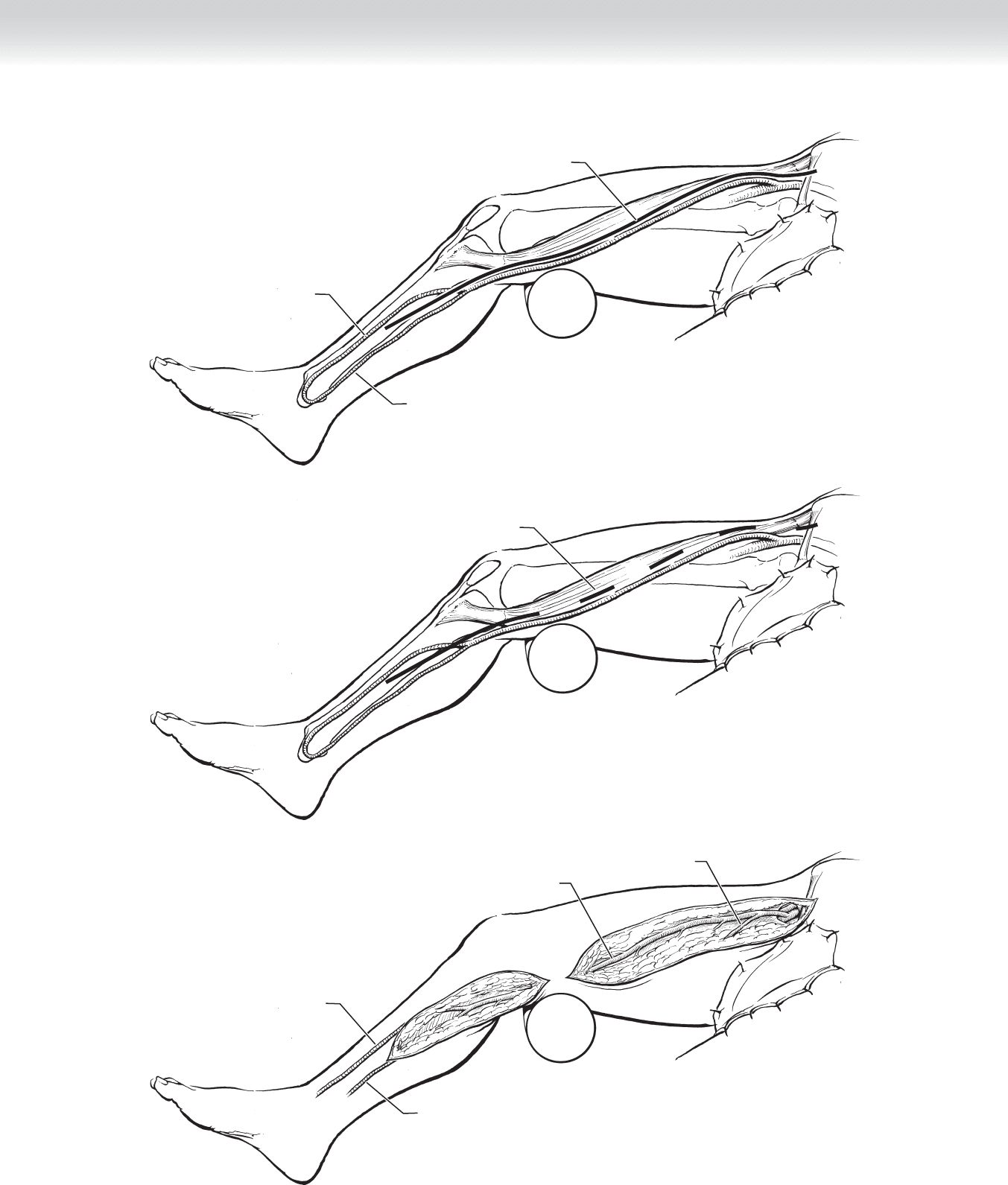
Continuous incision
(solid lines)
True great
saphenous vein
Posterior medial
or posterior arch vein
A
Skip/bridge incision
(dashed lines)
B
Great
saphenous vein
Medial accessory
saphenous vein
C
True great
saphenous vein
Posterior medial
or posterior arch vein
FIGURE 85 –3

922 Section XII • Vascular
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ The standard indication for reconstruction for occlusive disease is limb-threatening isch-
emia. This includes ischemic rest pain, ulceration, and gangrene. There are certain accepted
indications for bypass in the setting of severe claudication that prohibit gainful employment
or maintenance of the activities of daily living.
◆ The femoropopliteal in situ bypass is one of many open reconstructive options available to
the surgeon. In general, when the vein is to be used for limb salvage, it is customary to use
the below-knee popliteal segment. The above-knee segment may seem like an appropriate
target, but it is known to have a high rate of progression of disease. The in situ technique
offers the advantage of allowing the larger part of the saphenous to be placed on the larger
common femoral artery and the smaller section of vein to be placed on the smaller outfl ow
artery. The alternatives to this include a femoropopliteal bypass with vein that is reversed
and buried in an anatomic tunnel that follows the native superfi cial femoral and popliteal
arteries. A prosthetic infrageniculate (below the knee) graft is reserved for the individual
who has exhausted all autogenous (vein) options in the lower and upper extremities—
including the great and small (also known as the lesser or short) saphenous, as well as the
basilic and cephalic veins. Last, with the endovascular revolution, many catheter-based op-
tions are available, including a percutaneous bypass with covered stent grafts, an atherec-
tomy, or laser treatment, to name a few.
◆ Preoperative venous duplex (a grayscale B-mode ultrasound and doppler waveform analysis)
of the superfi cial veins is very helpful to determine the quality of the vein and to help
choose an operative plan. If the ultrasound can be arranged close to the bypass surgery date,
it is helpful to have the technician mark the course of the vein. Many operative suites have
an ultrasound available, and the vein can be marked before the leg is prepped. This may
help reduce the risk of a fl ap formation.
STEP 3: OPERATIVE STEPS
◆ The patient is placed in a supine position. For occlusive disease, it is a good rule to prepare
more than is needed. In general, both lower extremities should be draped in case further
vein is needed to complete a procedure. The fi rst incision is typically placed in the groin at
the level of the inguinal ligament. The great saphenous vein is identifi ed fi rst at the fossa
ovalis, below Scarpa’s fascia. The femoral sheath is then opened longitudinally to identify
the femoral vessels. The common femoral artery, superfi cial femoral artery (SFA), and pro-
funda femoris artery (PFA) should be isolated. The saphenous vein can then be isolated
either through a continuous incision that “unroofs” the entire vein or through a series of
“skip” incisions, also known as bridge incisions. A continuous incision allows maximal
visualization of all branches but can be associated with greater wound-healing and infection
risks. The bridge technique can heal better but has limited viewing of the vein, which may
result in either vein injury or inadequate ligation of all branches (see Figure 85-3). A third
alternative is a hybrid between a traditional vein harvest and an in situ harvest—an endo-
scopic vein harvest. Some institutions may have a designated individual with extensive
experience, such as a physician’s assistant who harvests for coronary artery bypass grafting.
This technique offers many advantages. There is one incision in the lower thigh that can be
used to harvest the vein to the saphenofemoral junction. The vein can then be placed in
CHAPTER 85 • Femoropopliteal Bypass (In Situ) 923
the harvest tunnel—either reversed or nonreversed. This offers the advantage of an in situ
technique, such as easy graft palpation or duplex surveillance. Additional benefi ts include
fewer incisions at risk for wound dehiscence and graft exposure.
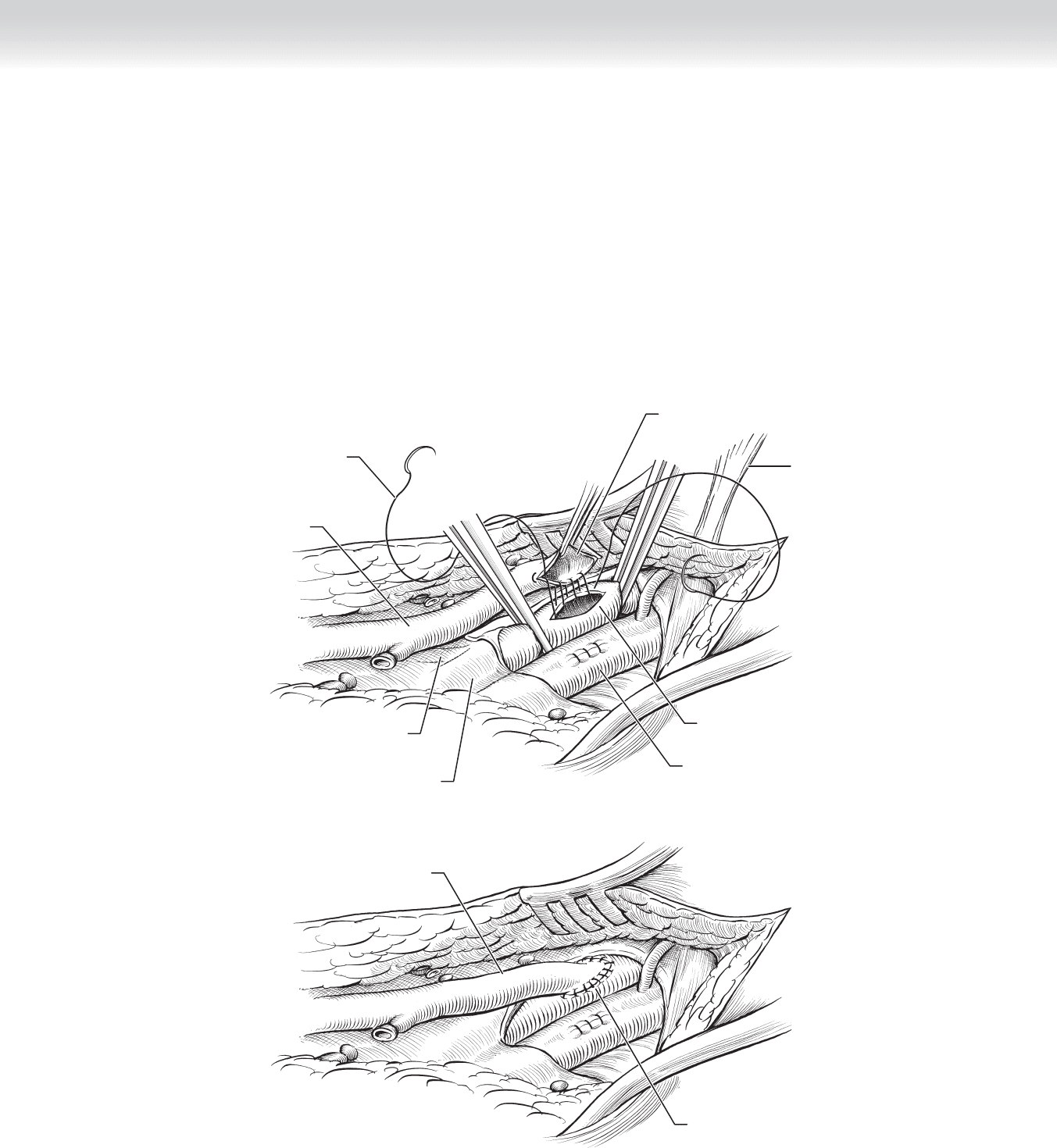
◆ Before the artery is clamped, the patient is given an unfractionated heparin bolus, typically
between 5000 and 10,000 U. The artery is clamped proximally and distally, and an arteriot-
omy is made anteriorly. A standard spatulated end of the vein-to-side of artery anastomosis
is created with Prolene suture, usually a 5-0 or 6-0 stitch (Figure 85-4).
Great saphenous vein and
common femoral artery anastomosis
Femoral vein
Inguinal ligament
Spatulated end-to-side
Profunda
Superficial
femoral artery
Great
saphenous vein
Monofilament
suture
A
Great saphenous vein and
common femoral artery anastomosis
Great
saphenous vein
B
FIGURE 85 –4

924 Section XII • Vascular
◆ The below-knee popliteal incision on the medial calf typically extends from the tibial tuber-
osity to the midcalf. A general rule for this exposure is to have a bump placed well above
the knee so that the gastrocnemius and soleus muscles hang freely. The fascia is entered,
and an avascular plane is developed by retracting the gastrocnemius and soleus muscles
downward. The popliteal space is then entered, and the vein (anterior to the artery) is dis-
sected free from the popliteal artery. The popliteal vein is commonly duplicated and that
branch is lying posterior to the artery. It can be injured when trying to dissect bluntly with
a right angle. It is best to use sharp dissection in this tight space, because it is much easier
to repair a cut than an avulsed branch (see Figure 85-2).
◆ There are multiple methods for destruction of the valves. A hand-held valvulotome or scis-
sors can be inserted through large side branches. There are also disposable products avail-
able (Figure 85-5). The proximal anastomosis should be created in a standard fashion (see
Figure 85-4). The most proximal fi rst and second valves are removed under direct vision
before this anastomosis is started. It is important to remove the thin valve cusp fl ush with
the vein wall. This will ensure that the cusp remnants do not become involved in the anas-
tomosis, which would severely stenose or occlude the fl ow. Flow should then be established
in the vein graft to identify whether any other valves are intact. There will be a decrease in
pulsatility and fl ow detected by Doppler ultrasound where the valve is still intact.
CHAPTER 85 • Femoropopliteal Bypass (In Situ) 925
Second valve
to be removed
First valve
to be revmoved
A
B
Commerical valvulotome
being advanced through
vein in closed position
Valvulotome opened
C
Valvulotome cutting
through valve while
being withdrawn
through vein
D
Great
saphenous vein
Saline infusion or
blood flow
FIGURE 85 –5

926 Section XII • Vascular
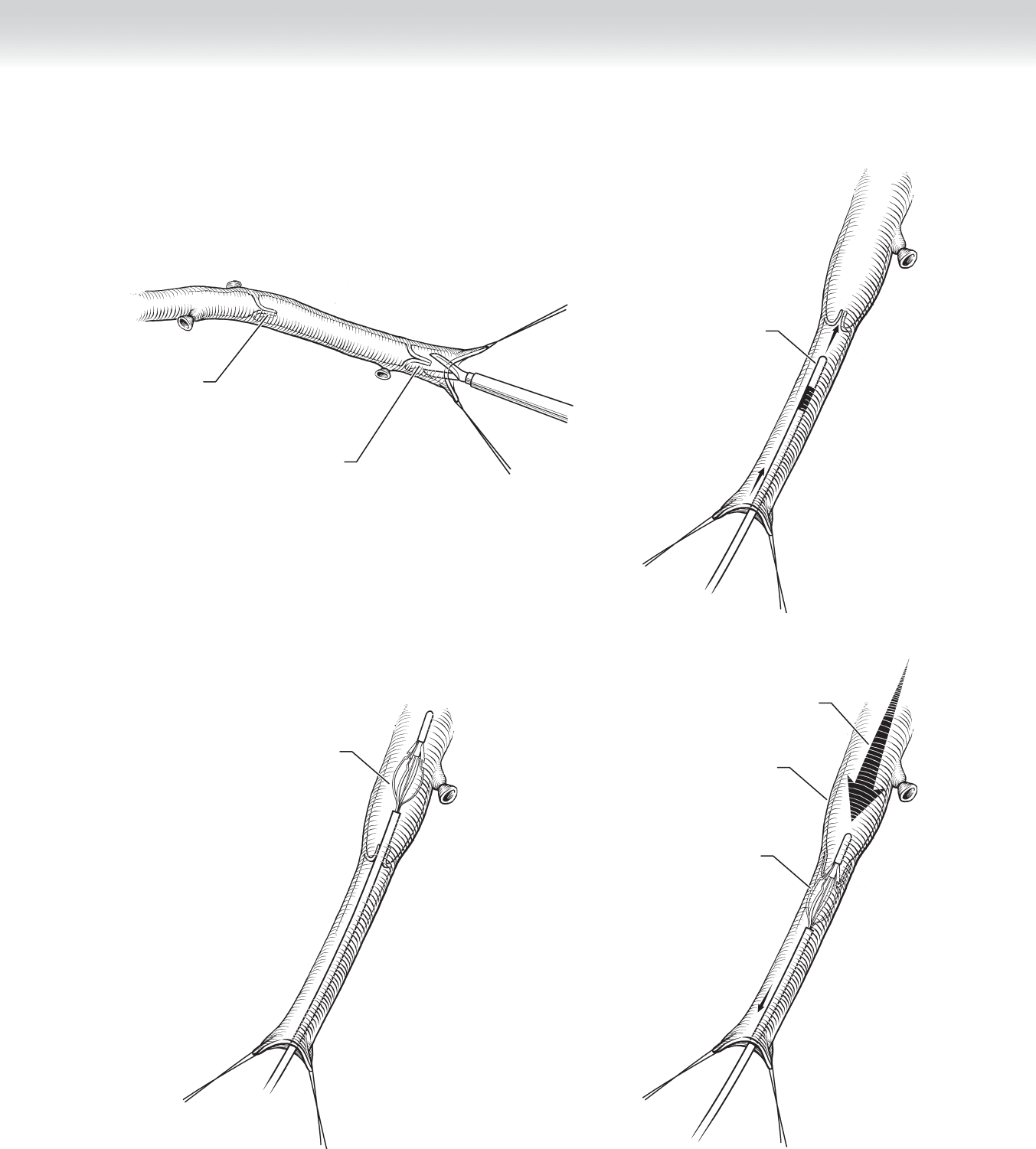
◆ Once adequate fl ow has been established in the vein, the distal anastomosis can be created
in a similar fashion (Figure 85-6). If the outfl ow artery is calcifi ed, a tourniquet can be
used to occlude the fl ow and avoid placing a clamp on the artery. Before the anastomosis is
completed, it should be appropriately irrigated and fl ushed free of any potential debris or
clot. A completion arteriogram can then be performed, ideally through a large preserved
side branch with a radiopaque marking tape. This is essential if the entire vein had not been
mobilized or if bridge incisions were used so that large branches can be ligated.
STEP 4: POSTOPERATIVE CARE
◆ Most patients undergoing surgery for peripheral arterial disease have multiple comorbidities
including coronary artery disease. They can be monitored in an intensive care unit, step-
down unit, or specialized fl oor bed depending on the protocols of the institution. Minimum
requirements should include telemetry, and vital signs should be taken every 2 hours, in-
cluding monitoring patency of the graft with Doppler ultrasonography. It is important to
educate staff on the importance of using a quantitative measure such as a Doppler signal
and not relying on an individual’s experience at feeling pedal pulses.
◆ If medically stable, the patient should be moved to a fl oor bed as soon as possible. Rehabili-
tation therapy should begin immediately, even if it is as simple as sitting in a chair. Realistic
expectations should be discussed with the family and staff about discharge planning. Many
patients will need transition care either in a rehabilitation facility or by a skilled nurse facility
(SNF) before they are independent and can go home by themselves or with a caregiver.
◆ Postoperatively, many surgeons prescribe a nonadjusted unfractionated heparin intravenous
drip for 12 to 24 hours. It is common for the patient to take either an anticoagulant (warfa-
rin) or a platelet inhibitor (aspirin or clopidrogel) after that. The decision on which to use
needs to be individualized based on certain factors. In general, these include quality of the
infl ow, which should be adequate before attempting an infrainguinal procedure. The out-
fl ow artery may not always be ideal, and a substandard conduit such as ePTFE or a bad
vein may convince the surgeon to use a stronger agent.
◆ After discharge, the patient should be seen in clinic and understand that he or she will have a
relationship with the surgeon for the life of that graft. Routine graft surveillance with duplex
scanning and ankle-brachial indices (ABIs) has been demonstrated to increase the primary
patency of grafts (assisted primary patency). Protocols include a postprocedure baseline level
and close follow-up (every 3 months for a year, then biannually). A drop in the ABI or a
velocity elevation is suggestive of a stenosis in the graft and warrants an arteriogram and
possible intervention.

CHAPTER 85 • Femoropopliteal Bypass (In Situ) 927
Great
saphenous vein
B
A
Popliteal artery
Ink marking anterior
orientation of the vein
Soleus muscle
Gastrocnemius
Great
saphenous vein
C
Anastomosis
Popliteal artery
Ink marking anterior
orientation of the
great saphenous vein
FIGURE 85 –6

928 Section XII • Vascular
STEP 5: PEARLS AND PITFALLS
◆ The in situ bypass technique has been shown to be an excellent choice for infrainguinal
reconstruction for occlusive disease. The location of the graft in the subcutaneous tissues
makes it quite easy to feel and evaluate with duplex ultrasound. There are certain groups of
patients with whom I am very cautious. The diabetic, end-stage renal patient is the classic
individual to have a wound-healing issue. Because the graft is directly under the skin, any
wound dehiscence will result in exposure of the adventitia and graft rupture if it is not dealt
with expediently. One may consider leaving large skin bridges, or I fi nd it preferable to
place the graft in a more anatomic location adjacent to the artery and vein. Thus, when
there are wound-healing issues, it is just a simple superfi cial or deep tissue infection and
not an organ space (i.e., the graft) that is involved.
SELECTED REFERENCES
1. Ouriel K, Rutherford R (eds): Atlas of Vascular Surgery: Operative Procedures. Philadelphia,
Saunders, 1998.
2. Norgren L, Hiatt WR, Dormandy JA, et al: Inter-Society Consensus for the Management of Peripheral
Arterial Disease (TASC II). J Vasc Surg 2007;45:S5-S6.
3. Valentine RJ, Wind GG: Anatomic Exposures in Vascular Surgery, 2nd ed. Philadelphia, Lippincott
Williams & Wilkins, 2003.
4. Rutherford RB: Atlas of Vascular Surgery: Basic Techniques and Exposures. Philadelphia, Saunders, 1993.

929
STEP 1: SURGICAL ANATOMY
◆ A review of the proximal femoral and saphenous vein anatomy has been discussed at length
in Chapter 85. The popliteal artery branches are commonly called the “trifurcation,” denot-
ing its division into three distinct arteries—(1) the anterior tibial artery (ATA), which
crosses the interosseus membrane and runs in the anterior compartment until the ankle
mortise; at that point it is called the dorsalis pedis artery (DPA). It has a large branch that
also may be suitable to receive the bypass is the lateral tarsal artery; (2) the posterior tibial
artery (PTA); and (3) the peroneal artery—which have a common trunk (tibioperoneal
trunk) that courses in the deep posterior compartment. The PTA continues its course on to
the foot at the medial malleous, where it divides into the medial and lateral plantar arteries.
The peroneal artery does not cross the ankle joint, but gives out two consistent branches
that collateralize to the DPA and PTA.
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ The same standard indications for reconstruction are true for tibial bypass as are true for
femoropopliteal reconstructions (see Chapter 85). They include limb-threatening ischemia
(ischemic rest pain, ulceration, and gangrene). Typically the lower in the leg you have to go
to fi nd a suitable target, the greater the burden of disease. There are three basic sections of
the arterial tree below the renal arteries: aortoiliac, femoropopliteal, and tibial (infragenicu-
late). When the disease is confi ned to one segment, then usually the patient will either be
asymptomatic or have claudication. If two or more segments are involved, then the isch-
emia is more profound and the limb can be threatened. So if you are planning a femorotib-
ial bypass, the occlusive lesions would be in two sections, the femoropopliteal and tibial
distribution. It is generally a statement to the overall status of the patient as well, because
these patients tend to have a heavier burden of atherosclerotic disease in other beds also
(coronary and extracranial carotid arteries).
◆ Autogenous vein is clearly the best option for reconstruction below the knee. Similar con-
siderations for vein assessment and procurement exist as for the femoropopliteal, but a lon-
ger section of quality vein is needed. At times, this can be hard to secure, and sections of
different veins can be anastomosed to create a conduit. Always remember that the small
saphenous, cephalic, and basilic veins are wonderful options. They can also be mapped
with ultrasound before the surgery. Again, having to do this raises the degree of complexity
and the possibility for adverse events.
CHAPTER
86
Femorotibial and
Peroneal Bypass
Lori Cindrick Pounds

930 Section XII • Vascular
◆ The decision to leave the vein in situ or bury it anatomically next to the native vessels is the
choice of the surgeon. Each has been shown to be appropriate. A consideration would be
the thin leg of a diabetic patient that has minimal subcutaneous tissue and is at risk for a
wound dehiscence. This would leave the graft easily exposed and at risk for rupture.
STEP 3: OPERATIVE STEPS
◆ The patient is placed supine. For occlusive disease it is a good rule to prepare more than is
needed. In general, both lower extremities should be draped in case further vein is needed to
complete a procedure. The fi rst incision is typically placed in the groin at the level of the ingui-
nal ligament. The great saphenous vein is identifi ed fi rst at the fossa ovalis, below Scarpa’s fas-
cia. The femoral sheath is then opened longitudinally to identify the femoral vessels. The com-
mon femoral artery, superfi cial femoral artery (SFA), and profunda femoris artery (PFA) should
be isolated. The saphenous vein can then be isolated either through a continuous incision that
“unroofs” the entire vein or a series of “skip” incisions, also known as bridge incisions, or if
available, endoscopic vein harvesting (please see Chapter 85 for more detail; see Figure 85-3).
◆ The target vessel has usually been identifi ed on either a preoperative or intraoperative arte-
riogram. It is helpful to use a radiopaque ruler on the skin to show where the tibial vessel is
good, otherwise you can reference a bony landmark (i.e., medial malleolus) and measure
backward. The tibial arteries can be more diffi cult to isolate and work with than the popli-
teal artery. They are found deep in the muscular compartments of the leg and are generally
smaller to sew to.
THE POSTERIOR TIBIAL ARTERY
◆ The PTA is approached through a medial calf incision (Figure 86-1, A) and is generally
combined with the saphenous harvest incision (please see Chapter 85 for more details on a
saphenous vein harvest). When the target is more proximal in the calf, say just past the tib-
ioperoneal trunk, it can be easier to identify the popliteal artery and then divide more of
the soleus muscle off the tibia. Immediately below will be the origin of the ATA and the tib-
ioperoneal trunk. There is typically an extensive network of interconnected veins that will
need to be ligated to allow full exposures. The origin of the PTA is approximately 2 to 3 cm
below the ATA, if that is to be the target.
◆ In the mid to distal leg above the ankle, the PTA remains in the deep posterior compart-
ment, and a thorough knowledge of the anatomy is helpful. The soleus is again removed
from its tibial attachments and retracted toward the OR table (Figure 86-1, B). A plane can
then be developed between the fl exor digitorum longus and the soleus muscles. The artery
will be surrounded again with a complex plexus of veins that need to be divided. In large
muscular legs it can be helpful to use a Doppler pencil to guide the exposure.
◆ At the ankle, the PTA becomes much more superfi cial, allowing an easier dissection, but
also raising the chances of wound complications. A reverse J-shaped incision is made at the
ankle, and the fl exor retinaculum is divided. The neurovascular bundle will be nestled in a
groove between the tendons of the fl exor hallucis longus and fl exor digitorum longus
muscles (Figure 86-1, C).
