Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

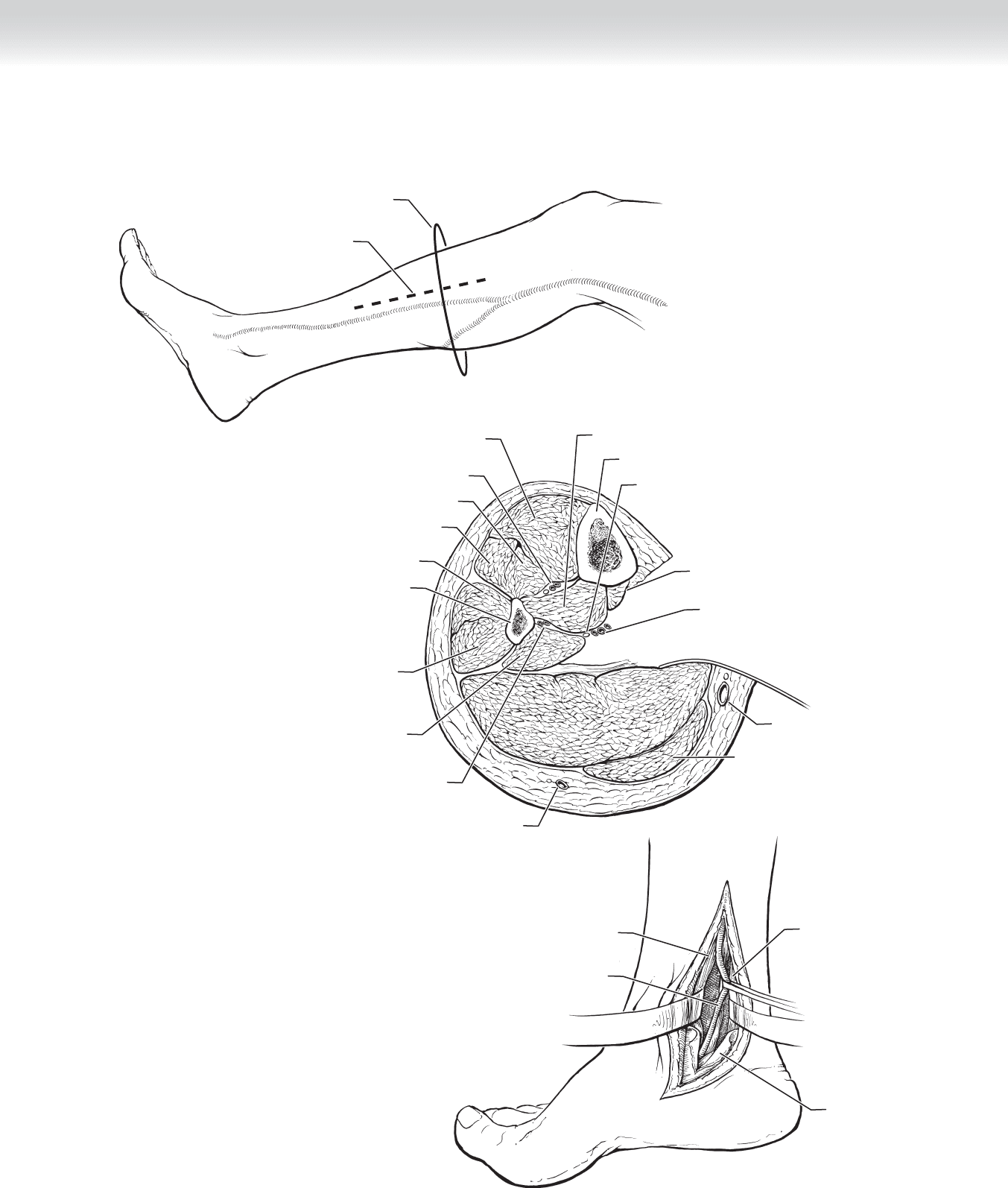
CHAPTER 86 • Femorotibial and Peroneal Bypass 931
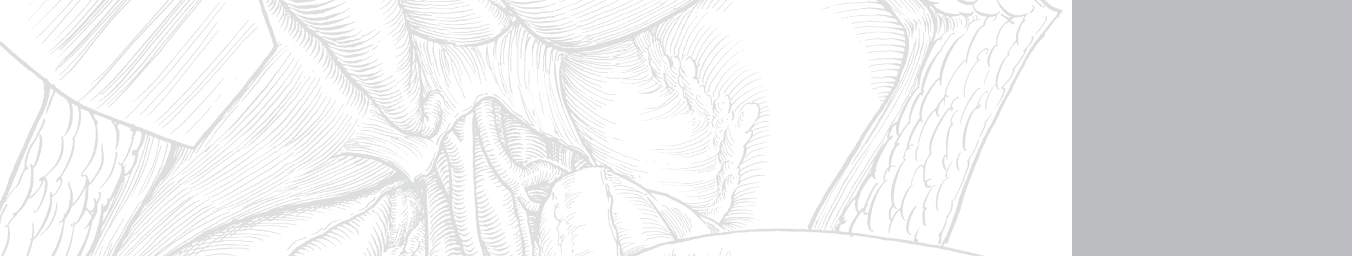
Incision
Posterior Tibial Artery Mid Calf
Cross-section
A
Soleus muscle
Anterior tibial artery and vein,
deep peroneal nerve
Tibialis anterior muscle
Extensor hallucis longus muscle
Extensor digitorum longus muscle
Peroneus brevis muscle
Fibula
Peroneus longus muscle
Flexor hallucis longus muscle
Peroneal artery and vein
Small saphenous vein
Great saphenous vein
Tibia
Tibialis posterior muscle
Tibial nerve
Gastrocnemius muscle
Posterior tibial
artery and veins
Flexor digitorum muscle
B
Soleus muscle
Posterior tibial
artery
Flexor digitorum
longus
Flexor digitorum
brevis
Flexor
retinaculum
C
FIGURE 86–1

932 Section XII • Vascular
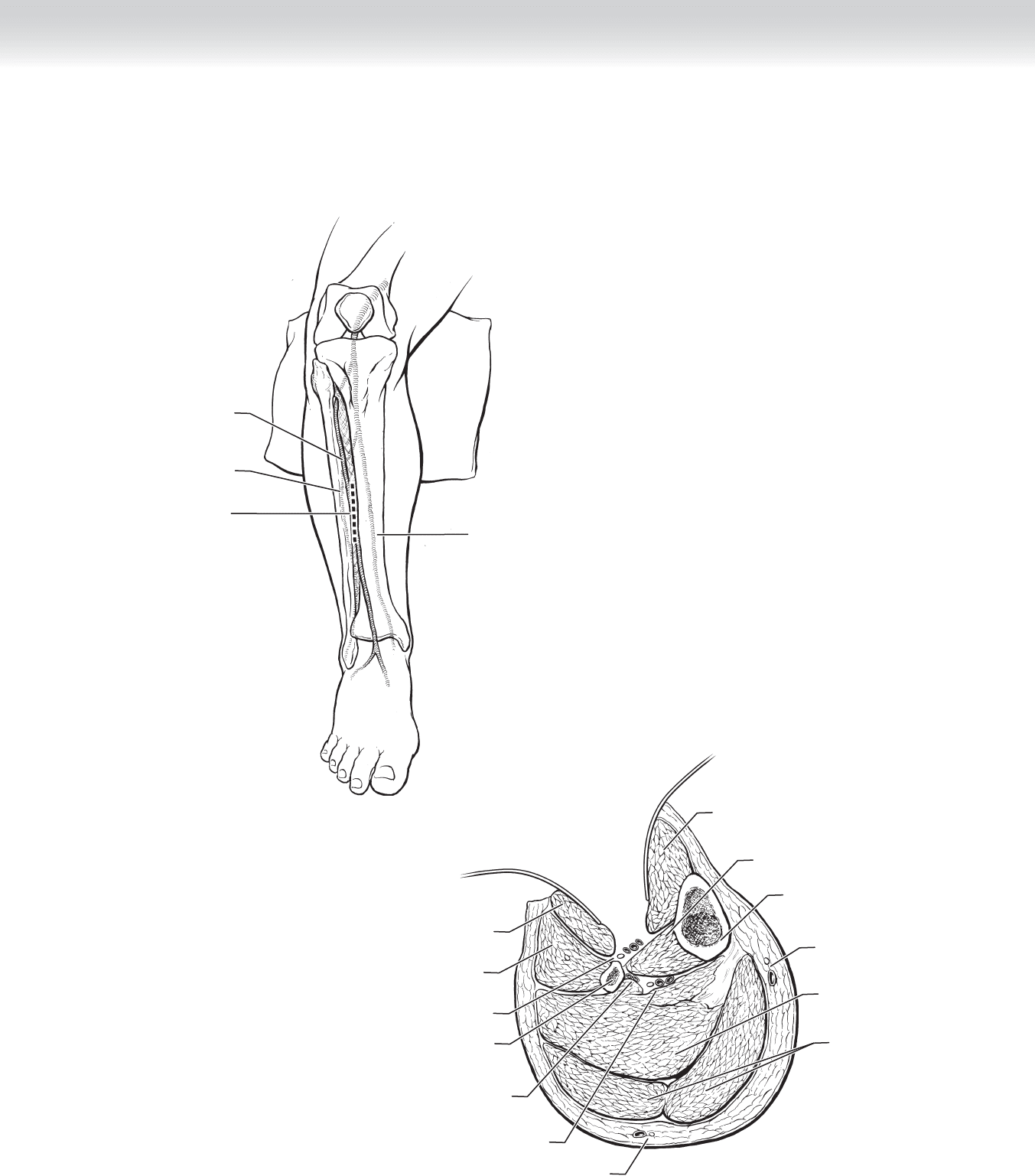
THE ANTERIOR TIBIAL ARTERY
◆ The ATA is isolated through an incision on the lateral calf between the tibia and fi bula
(Figure 86-2, A). Sometimes in thin legs, you can appreciate the division between the ante-
rior and lateral compartments of the leg and guide your incision more toward the anterior
compartment. In the proximal leg, a plane can be developed between the tibialis anterior
and extensor digitorum longus muscles (Figure 86-2, B). The artery, vein, and nerve
(deep peroneal) will be just anterior to the interosseus membrane. Once again there will be
a rich network of surrounding veins.
◆ By the mid-portion of the leg, the extensor hallucis longus muscle originates and becomes
more prominent, and the plane will be between it and the anterior tibialis muscle.
◆ In the distal third of the leg, the ATA courses much more anteriorly and is found between
the tendon of the tibialis anterior muscle and the extensor hallucis longus muscles.
◆ The challenge with the ATA, however, is how to tunnel the vein graft. The two most popu-
lar options include an anatomic location with it going through the interosseus membrane in
the popliteal space and then laterally in the anterior compartment. The other is to have the
vein in a modifi ed in situ position that courses from a medial to lateral position just below
the skin. If the origin of the bypass is the femoral artery and it courses along the lateral
knee, great care must be taken to account for the knee bending. If the origin of the bypass
is the popliteal, then the options include laying it on top of the tibia or removing a section
of the bone to allow it to sit better. Either way, if this approach is used, extra length of vein,
which may not be available, is required.
CHAPTER 86 • Femorotibial and Peroneal Bypass 933
Tibialis posterior
muscle
Tibia
Saphenous vein
and nerve
Soleus muscle
Gastrocnemius
muscle
Tibialis anterior
muscle
Extensor digitorum
longus muscle
Peroneus longus muscle
Deep peroneus nerve,
anterior tibial artery and vein
Peroneal artery and vein
Fibula
Posterior tibial artery and vein,
tibial nerve
Small saphenous vein
B
Tibia
A
Incision
Anterior tibial artery
Fibula
Posterior Tibial Artery Mid Calf
FIGURE 86–2
934 Section XII • Vascular
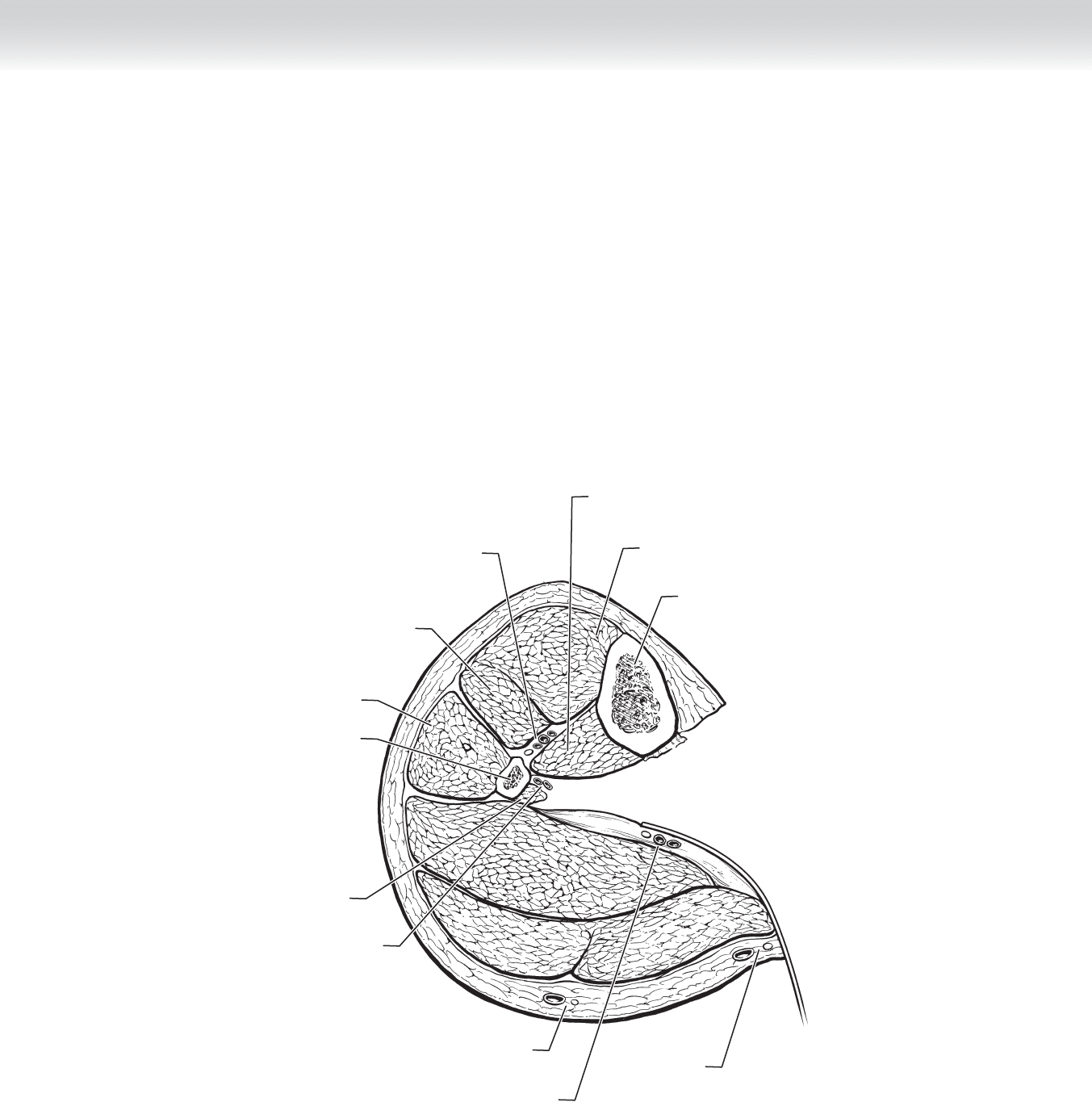
THE PERONEAL ARTERY
◆ The peroneal artery is the most diffi cult tibial artery to work with. It is always much deeper
than expected. In a thin calf, the peroneal artery is generally approached medially. The same
general dissection is used as for the PTA, but you must go deeper for the peroneal artery. The
soleus is again divided and retracted posteriorly toward the OR table (Figure 86-3). The
PTA is left in its loose areolar tissue with the soleus muscle. The peroneal artery will be
located on the anterior surface of the fl exor hallucis longus. This makes sewing the distal
anastomosis more challenging because seeing and sewing in a small deep space is more
diffi cult.
Fibula
Flexor hallucis
longus muscle
Peroneus longus muscle
Tibialis posterior
muscle
Tibia
Tibialis anterior
muscle
Extensor digitorum
longus muscle
Deep peroneal nerve,
anterior tibial artery and vein
Peroneal artery and vein
Posterior tibial artery and vein,
tibial nerve
Saphenous vein
and nerve
Small saphenous vein
Medial Approach Peroneal Artery
Soleus
muscle
Soleus
muscle
Gastrocnemius
muscle
Gastrocnemius
muscle
FIGURE 86–3
CHAPTER 86 • Femorotibial and Peroneal Bypass 935
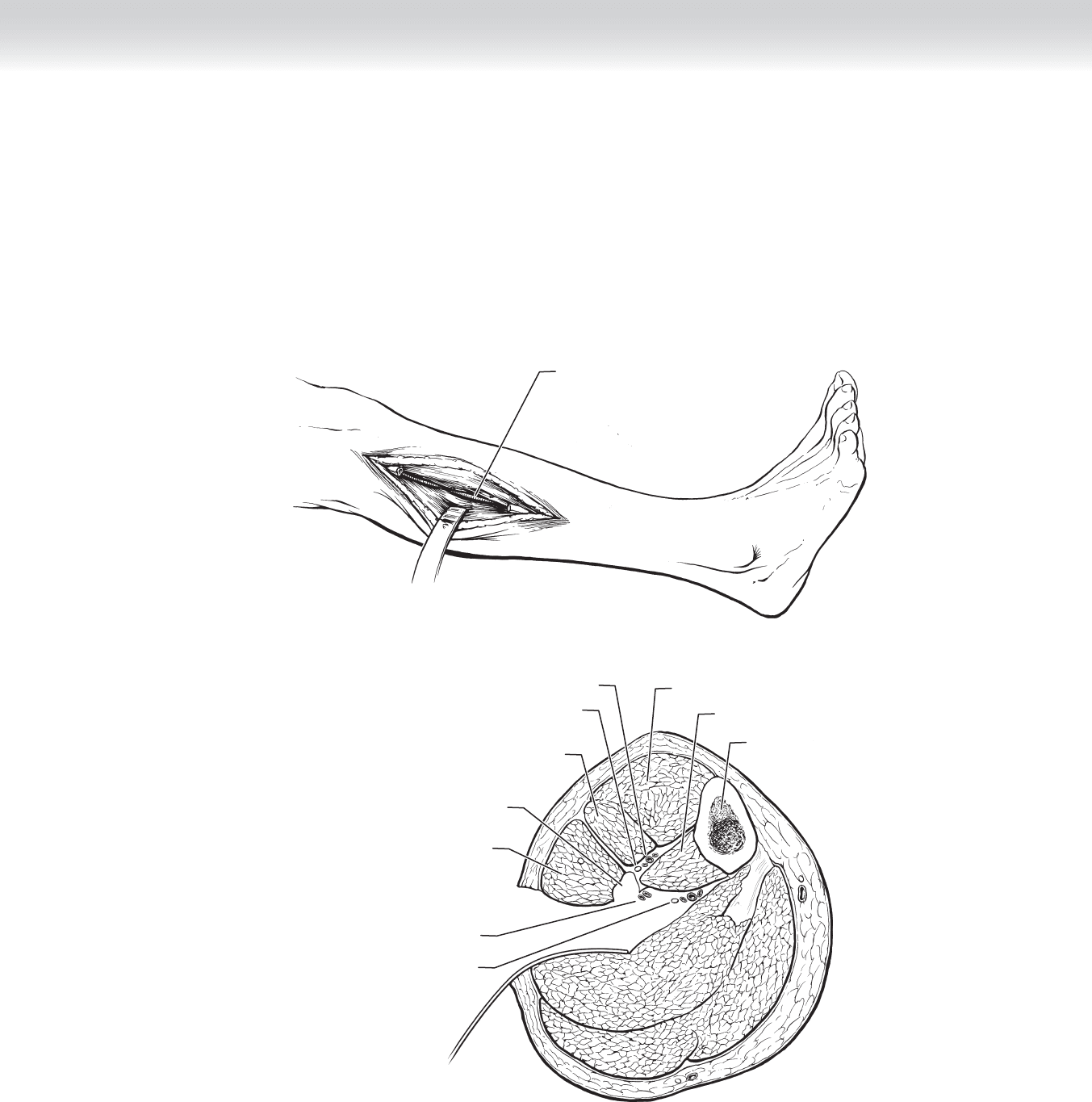
Peroneal artery
A
Lateral Approach Peroneal Artery
Tibialis anterior muscle
Tibia
Soleus
Soleus
muscle
muscle
Soleus
muscle
B
Gastrocnemius
Gastrocnemius
muscle
Gastrocnemius
muscle
Tibialis posterior muscle
Peroneal artery and vein
Peroneus longus muscle
Fibula resected
Extensor digitorum
longus muscle
Deep peroneal nerve
Anterior tibial artery and veins
Posterior tibial artery and veins,
tibial nerve
FIGURE 86–4
◆ If a leg is large or if the peroneal artery is best very distally in the leg, the artery can be approached
laterally with removal of a section of the fi bula (Figure 86-4).

936 Section XII • Vascular
STEP 4: POSTOPERATIVE CARE
◆ Most patients undergoing surgery for peripheral arterial disease have multiple comorbidities
including coronary artery disease. They can be monitored in an intensive care unit, step-down
unit, or specialized fl oor bed depending on the protocols of the institution. Minimum
requirements should include telemetry, and vital signs should be taken every 2 hours, includ-
ing monitoring patency of the graft with Doppler ultrasonography. It is important to educate
staff on the importance of using a quantitative measure, such as a Doppler signal, and not
relying on an individual’s experience at feeling pedal pulses.
◆ If medically stable, the patient should be moved to a fl oor bed as soon as possible. Rehabili-
tation therapy should begin immediately, even if it is as simple as sitting in a chair. Realistic
expectations should be discussed with the family and staff about discharge planning. Many
patients will need transition care either in a rehabilitation facility or a skilled nurse facility
(SNF) before they are independent and can go home by themselves or with a caregiver.
◆ The need for postoperative modulation of the coagulation cascade is greater the longer the
bypass is. Postoperatively, many surgeons prescribe a nonadjusted unfractionated heparin
intravenous drip for 12 to 24 hours. It is common to prescribe either an anticoagulant
(warfarin) or a platelet inhibitor (aspirin or clopidrogel) after that. The decision on which
one to use needs to be individualized based on certain factors. In general, these include
quality of the infl ow, which should be adequate before attempting an infrainguinal proce-
dure. The outfl ow artery may not always be ideal, or a bad vein may convince the surgeon
to use a stronger agent. Most surgeons try to avoid prosthetic conduits (ePTFE) below the
knee, but if it is used, warfarin is generally used.
◆ After discharge, the patient should be seen in the clinic and understand that he or she will
have a relationship with the surgeon for the life of that graft. Routine graft surveillance with
duplex scanning and ankle-brachial indices (ABIs) has been demonstrated to increase the pri-
mary patency of grafts (assisted primary patency). Protocols include a postprocedure baseline
level and close follow-up (every 3 months for a year, then biannually). A drop in the ABI or a
velocity elevation is suggestive of a stenosis in the graft and warrants an arteriogram and pos-
sible intervention.
STEP 5: PEARLS AND PITFALLS
◆ Femorotibial reconstruction is an excellent option for patients with advanced occlusive disease,
most of which present with critical limb ischemia (rest pain or tissue loss). These individuals
have a larger burden of disease and tend to have other serious comorbidities, such as cardiac
disease and long-standing diabetes. They are more likely to have an adverse clinical event in
the perioperative period. Great care must be taken to limit the risk of this, and such treatment
as perioperative beta blockade is essential for this group.
◆ Just as in the in situ femoropopliteal reconstruction, the tibial bypass is also at risk for
wound complication issues. Great care with tissue handling, keeping the graft as deep as
possible, and avoiding a fl ap creation are essential to promote good wound healing.

CHAPTER 86 • Femorotibial and Peroneal Bypass 937
SELECTED REFERENCES
1. Ouriel K, Rutherford R (eds): Atlas of Vascular Surgery: Operative Procedures. Philadelphia, Saunders,
1998.
2. Norgren L, Hiatt WR, Dormandy JA, et al: Inter-Society Consensus for the Management of Peripheral
Arterial Disease (TASC II). J Vasc Surg 2007;45:S5-S6.
3. Valentine RJ, Wind GG: Anatomic Exposures in Vascular Surgery, 2nd ed. Philadelphia, Lippincott
Williams & Wilkins, 2003.
4. Rutherford RB: Atlas of Vascular Surgery: Basic Techniques and Exposures. Philadelphia, Saunders, 1993.
938
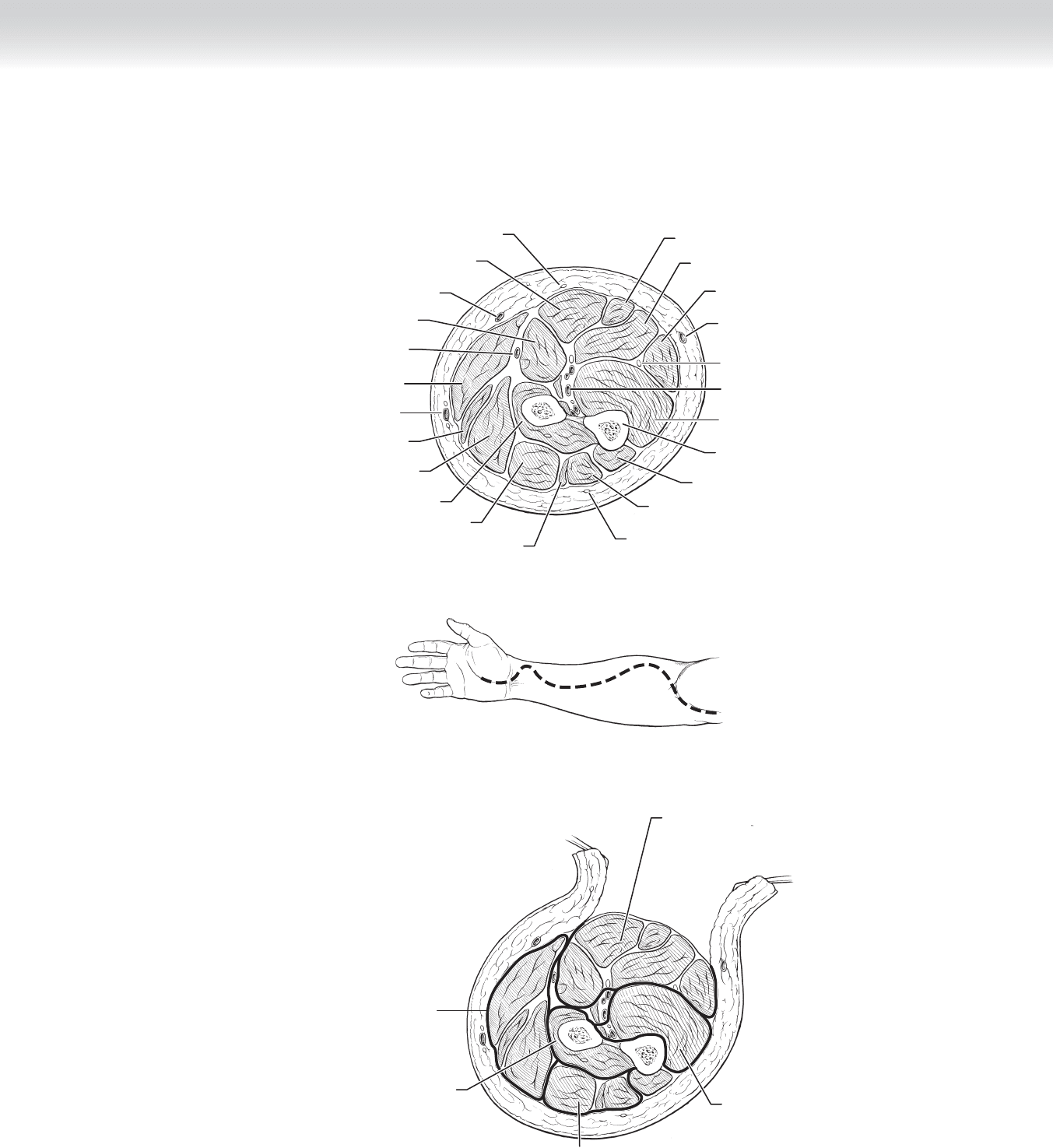
STEP 1: SURGICAL ANATOMY FOR FOREARM
◆ The forearm is divided into multiple fascial compartments, each containing several mus-
cles that are additionally enclosed within individual epimysial envelopes. Three forearm
compartments are usually described: the volar, dorsal, and lateral (mobile wad)
compartments.
◆ The interosseous membrane separates the volar and dorsal compartments from each other,
and the posteriorly and radially located lateral compartment is demarcated by a connective
tissue septum from the antebrachial fascia. In most cases of compartment syndrome, the
volar muscles are the most severely affected, followed in severity by the muscles of the dor-
sal compartment and of the lateral compartment. Some communication exists among the
three main compartments, and release of the volar compartment often relieves elevated tis-
sue pressure in the dorsal compartment. Intraoperative pressure measurements and clinical
fi ndings may preclude the need for a separate dorsal fasciotomy to relieve this extensor
compartment. The lateral compartment musculature is superfi cial and easily decompressed.
◆ Within the volar compartment, additional distinction can be made between the superfi cial
and deep muscles. The superfi cial muscles include the pronator teres, palmaris longus,
fl exor digitorum superfi cialis, fl exor carpi radialis, and fl exor carpi ulnaris. The deep
muscles include the fl exor digitorum profundus, fl exor pollicis longus, and pronator
quadratus. The fl exor digitorum profundus and fl exor pollicis longus are particularly vul-
nerable in compartment syndrome, because they may be compressed against rigid bone and
the unyielding interosseous membrane. Anatomic and clinical reports demonstrate that
release of the superfi cial volar compartments may not be adequate to relieve deep pressures
in these muscles.
◆ The dorsal compartment is also divided into superfi cial and deep muscles. The extensor
digitorum, extensor carpi ulnaris, and extensor digiti minimi are the superfi cial group,
which lie in a plane above the deeper abductor pollicis longus, extensor pollicis brevis, ex-
tensor pollicis longus, extensor indicis, and supinator (Figure 87-1, A).
CHAPTER
87
Fasciotomy—Forearm and Leg
William J. Mileski
CHAPTER 87 • Fasciotomy—Forearm and Leg 939
FIGURE 87 –1
A
MC
Palmaris longus muscle
Flexor digitorum superficialis muscle
Basilic vein
Flexor carpi ulnaris muscle
Ulnar nerve
Flexor digitorum profundus muscle
Common interosseous artery
Ulna bone
Anconeus muscle
Extensor carpi ulnaris muscle
Posterior cutaneous nerve
of forearm from radial nerve
Anterior branch of medial
cutaneous nerve of forearm
Flexor carpi radialis muscle
Pronator teres muscle
Median antebrachial vein
Brachioradialis muscle
Radial artery
Extensor carpi radialis longus muscle
Cephalic vein
Extensor carpi radialis brevis muscle
Supinator muscle
Extensor digitorum muscle
Extensor digiti minimi muscle
Right Forearm
Lateral
Right Forearm
Medial
Volar incision
B
C
Superficial volar
compartment
Deep volar
compartment
Superficial
dorsal compartment
Lateral compartment
Deep dorsal
compartment

940 Section XII • Vascular
STEP 2: PREOPERATIVE CONSIDERATIONS FOR FOREARM
◆ Compartment syndrome is a surgical emergency that usually requires release of the superfi -
cial muscle compartments. In some clinical situations, it is imperative to also explore the
deep muscle compartments.
◆ Forearm compartment syndrome requires immediate evaluation and treatment. The need
for operation is established by careful review of the patient’s history; the presence of physi-
cal signs and symptoms, such as pain with passive stretching, paresthesias, paresis, and
palpably tense compartments; and, if needed, the measurement of elevated compartment
pressures (⬎30 cm H
2
O).
◆ The treatment of compartment syndrome requires expedient fasciotomy when nonoperative
maneuvers such as cast removal are unsuccessful. If left untreated, elevated tissue pressure
within the fascial confi nes decreases capillary blood perfusion below a level necessary for
soft tissue viability. Most patients ultimately have minimal limb dysfunction when fasciot-
omy has been performed promptly and to an adequate depth. Postoperative loss of function
may be caused by several factors, including damage from the initial injury, ischemia caused
by elevated tissue pressure before fasciotomy, inadequate fasciotomy, and iatrogenic surgical
injury.
◆ Mandatory exploration of deep muscle compartments is indicated in situations in which the
deep muscles are preferentially injured, such as in cases of high-voltage electrical injury.
The high electrical resistance of bone transmits a signifi cant thermal injury to the adjacent
muscles of the deep compartment. Other conditions that require exploration of the deep
spaces include severe crush injuries; situations involving extended pressure, such as an
unconscious patient lying on the limb; and when there is ongoing sepsis or suspicion of
necrotic muscle, despite previous fasciotomy. If epimysiotomies of the deep muscles are not
performed in these situations, necrosis and contracture may result.
◆ Limited incisions to minimize collateral morbidity from fasciotomy do not offer access to all
components and increase the potential for missing an ischemic or necrotic muscle group.
STEP 3: OPERATIVE STEPS FOR FOREARM
1. INCISION
◆ A commonly used approach, begins 1 cm proximal and 2 cm lateral to the medial epicon-
dyle. The incision is carried obliquely across the antecubital fossa and over the volar aspect
of the mobile wad and is then curved medially to reach the midline of the forearm at the
junction of its middle and distal thirds. The incision is continued straight distally to the
proximal wrist crease ulnar to the tendon of the palmaris longus and is fi nally curved across
to the midpalm (Figure 87-1, B).
